Morbidity, surveillance and epidemiology of scorpion sting, cutaneous leishmaniasis and pediculosis capitis in Bandar-mahshahr County, Southwestern Iran
2014-03-22HamidKassiriMohammadHosseinFeizhaddadMohammadAbdehpanah
Hamid Kassiri, Mohammad-Hossein Feizhaddad, Mohammad Abdehpanah
1School of Health, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
2School of Medicine, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
Morbidity, surveillance and epidemiology of scorpion sting, cutaneous leishmaniasis and pediculosis capitis in Bandar-mahshahr County, Southwestern Iran
Hamid Kassiri1*, Mohammad-Hossein Feizhaddad2*, Mohammad Abdehpanah1
1School of Health, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
2School of Medicine, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran
Objective: To study epidemiologic features of scorpion stings, patients with cutaneous leishmaniasis and pediculosis capitis cases in Bandar-mahshahr County, Southwestern Iran, during 2008-2009. Methods: A descriptive study was conducted on the referred individuals with stung scorpions, pediculosis capitis and cutaneous leishmaniasis attending health centers from Bandar-mahshahr County in 2008. The patients' medical records with epidemiologic and demographic data were collected. Using SPSS, we have attempted to summarize statistics, namely frequencies and percentages. Results: A total of 135 scorpion stings patients were studied. Of these, 34.8% were female and 65.2% male. Most of the Scorpion stings were recorded in the 21-30 year age group (37.8%). A total of 82 cases of cutaneous leishmaniasis were studied in this assignment that all cases have been reported from urban health centers. Considering number of wounds on the body the maximum of the patients (37.6%) had only one lesion. In this study, 12 referred patients from the health centers were studied for pediculosis capitis. According to obtained information one of the patients was male and 11 patients were female. Conclusions: Some important measures, such as education, health promotion and public participation should be implemented for preventing of these diseases.
ARTICLE INFO
Article history:
Received 8 August 2013
Received in revised form 15 September 2013
Accepted 24 September 2013
Available online 20 November 2014
Epidemiology
Scorpion sting
Cutaneous leishmaniasis
Pediculosis capitis
Iran
1. Introduction
Scorpion sting is one of the most important health problems in developing countries and world tropical and subtropical areas. Every year thousands will face the risk of death due to scorpion stings. Currently, scorpion sting in some parts of the world is counted as the important health problems for Southern parts of Africa, Middle East, Southern states of America, Mexico, South America and the Indian subcontinent. Although, world statistics are estimated for 1 million scorpion stings annually, in Mexico alone, 250 000 cases are occurred and in Tunisia 40 000 cases with 100 deaths. Scorpion sting is the most important health problems in Brazil with 50 deaths from 37 000 cases. In the world, more than 1 500 species of scorpion reported that approximately stings of 50 species are semi-dangerous to very dangerous for human health[1].
In Iran, scorpions and scorpion stings was considered as one of the major health problems. This problem, in addition to stress and induced anxiety by high medical costs exposes the risk of death for a large number of people lives annually[2-4]. In Iran, more than 100 000 people are struck by scorpions annually of which more than 75% of them are children however, only about 36 000 cases are reported and a minimum of 7 to 60 cases per year resulting in death[5]. Despite the fact that approximately 10 000 to 13 000 scorpion stings are reported in the United States, only 4 deaths occur every 11 years[6].
Depending on the climate and weather in Iran, and diversity for species scorpions, the stings in different parts of the country, especially in the warm months are reported every year. According to the Director General of the Ministry of Health for Prevent and Combat against Diseases in 1997,33 731 cases of scorpion stings occurred of which, 39 cases have been fatal. Of 33 731 cases, 23 437 stings have been happened in Khuzestan Province with 32 deaths, i.e. 82% of deaths occurred in Khuzestan. This means that the lethality of Khuzestan Province’s scorpions is more than the others part of the countr[7]. In 2005, 42 850 cases of scorpion stings with 14 deaths and in 2006 the numbers of 45 950 cases with 18 deaths have been reported[8]. Hormozgan and Khuzestan provinces are important foci for the scorpion stings in Iran and tens of thousands of cases with tens deaths are reported, annually[7].
In Khuzestan Province the most dangerous scorpion sting is attributed toHemiscorpius lepturus(H. lepturus). The venom of the scorpion could effect on the most vital organs and lead to the fatal outcome[9]. Considering that most deaths in Iran due to scorpion stings occurring in Khuzestan Province are owing toH. lepturussting thus, it can be said that this species is the most dangerous scorpion in Iran which is found in abundance in Khuzestan Province, particularly in East province[10]. This scorpion venom has hemotoxic and cytotoxic properties. The majority of struck victims are children in Iran. The most important scorpion sting symptoms in the human repercussions locally included; necrosis, swelling, erythema, ecchymosis and systemic; severe hemolysis, hematuria (blood in urine) and kidney failure[11,12].
Leishmaniasis is one of the common diseases among humans and animals which occurs in three forms of cutaneous leishmaniasis, visceral leishmaniasis (kalaazar) and cutaneous-mucosa leishmaniasis. Agent of cutaneous leishmaniasis is a protozoan from flagellate groups, Trypanozomatidae family and Leishmania genus. Leishmania is transferred by the bite of mosquitoes belong to the Psychodidae family, subfamily of Phlebotominae from animal reservoir (mostly rodents and domestic and wild carnivores) and infected human to healthy individuals. Symptoms include ulcers which may remain on the body (face, hands, feet, etc.) by one year[13,14].
Leishmania tropica(L. tropica) cause urban cutaneous leishmaniasis andL. majorcause rural cutaneous leishmaniasis which they have been isolated from patients in Iran. The parasite life cycle is as Phlebotmus female sandflies bite the infected host and the amastigotes enter into the insect gut. Then, the forms of Leptomonad in sandflies are inoculated into a new vertebrate host body and are transformed into the Leishman bodies in skin macrophages. The reservoirs of urban cutaneous leishmaniasis are humans and dogs while, the reservoirs of rural cutaneous leishmaniasis are rodents the Gerbillidae family. The cutaneous lesions are usually raised volcanoshaped ulcers with depressed center covered by granulation tissue and rigid edges. After a periodical phase the lesion healed spontaneously and subsequently recovered the scars remain permanently. The rural cutaneous lesion is wet and the lesion size is larger than the urban cutaneous lesion[15-18].
Cutaneous leishmaniasis is one of the ten most important parasitic diseases in the world tropical areas that the World Health Organization advises and supports the study and research on various aspects of the disease. Extent of the disease is evident on every continent except Australia and this disease is seen in 88 countries of which, 72 countries (82%) are in developing countries. Annually, 1.0-1.5 million of cutaneous leishmaniasis cases and 500 000 visceral leishmaniasis cases are reported due to this parasite. It is estimated that a population of about 350 million people worldwide are at risk of involving the disease. About 90% of cutaneous leishmaniasis is reported in the world from Afghanistan, Algeria, Brazil, Iran, Peru, Saudi Arabia and Syria among which, Iran and Saudi Arabia are the most prevalent[19-22].
Cutaneous leishmaniasis was existed in Iran for a very long time and today Iran is one of the most important disease foci in the world. Iran is among the countries with the highest incidence of ZCL infection withL. majorwhich is observed in the form of endemic in some parts[23]. Each year approximately 20 thousands cases of cutaneous leishmaniasis were reported from different parts of the country, although the actual amount multiply the estimate reported[24,25]. The incidence of cutaneous leishmaniasis in Iran has increased, so that the number of positive cases in 2005 compared to 2001 increased by about 105 percent. The prevalence of the disease in the provinces of Khorassan, Fars, Khuzestan, and Kerman was high and the provinces of Ilam, Yazd and Bushehr had the highest rate of new cases. The provinces of Yazd, Busher, Khorassan, Fars, Ilam, Khuzestan and Esfahan with average of 166 cases per 100 000 people in Iran, have the highest incidence rates. However, the western and the western north provinces of the country with less than 10 cases per 100 000 have the lowest incidence of cutaneous leishmaniasis in the country[26-30].
Pediculosis capitis infestation is a parasitic disease caused by an external and obligatory parasite; called louse; in humans. So far, three species, includingPediculus humanus(P. humanus) (body louse),Pediculus capitis(P. capitis) (head louse) andPhtirus pubis(P. pubis) (pubic louse) have been identified as parasites in humans[31]. Human lice are belonging to the Anoplura order and composed of 490 bloodfed species. They are mammals’ obligatory ectoparasites which cannot live away from host, except for a short time[32]. Pediculosis in primary school students is among the most common diseases. At present, in many countries, especially in developing countries wide campaign was begun to control lice infestation and preventing the spread of the disease.However, despite enormous efforts and costs the disease fully controls have not yet managed[33]. Pediculosis is an endemic parasitic infestation in many countries of the world[34]. In people with pediculosis the direct effects of lice bites cause the injection of foreign protein from the insect saliva into the host body that associated with stimulation of host susceptibility and fatigue. Repeated injections of lice saliva may be cause acute allergic such as itching. If stools dust is inhaled may appear similar symptoms to hay fever[35]. A total number of 6 to 12 million people worldwide are infested, annually. This disease is one of the most common contagious diseases in the community[36]. According to WHO statistics, Iran is one of the most infested regions for this insect in the world. Infestations are mainly among elementary school students[37] and studies on children around the world shows that the prevalence of louse infestation is less than 10% for which sometimes this rate reaches 40% or more. The incidence of pediculosis was found to be 5.1% by a survey conducted in Rasht County (northern Iran) in 2003[38]. Another study was performed in the County of Sari (northern Iran) on 10 991 elementary school students in 2001-2002. Number of 215 (1.9%) cases was infested with pediculosis. The prevalence in primary schools was 3.7% for girls and 0.5% for boys. In this study, a statistically significant association was found between infestation and occupation, parent education level, and common tools use. However, in other studied variables (father’s educational level, father’s income, and father’s occupation) statistic correlation was not observed[39]. The most effective ways to combat the disease are, patients treated with drugs including Lindane, Permethrin 1%, Crotamiton 10%, Malathion 0.5%, ointment Sulphur 6%-12% and public education and health promotion in infested communities[40].
This study was conducted to determine the epidemiology of scorpion stings, cutaneous leishmaniasis and pediculosis capitis in Bandar-mahshahr County, southwestern Iran, during 2008-2009. This information is important for the control of these problems.
2. Materials and methods
This was a descriptive cross-sectional study of the medical records of all people diagnosed with scorpion envenomation, cutaneous leishmaniasis or pediculosis capitis who were admitted to Bandar-mahshahr health services centers over 2008-2009. The cases were monitored after their physical, laboratory and history examination. Three special scorpion sting, cutaneous leishmaniasis and pediculosis capitis sheets were prepared. These sheets contained information about demographic and epidemiologic characters. The frequencies of epidemiological features were changed to the percentage basis. Data were analyzed using a SPSS computer package by using descriptive statistics.
3. Results
A total of 135 scorpion stings patients were studied. Of these, 34.8% were female and 65.2% male. Most of the Scorpion stings were recorded in the 21-30 year age group (37.8%) and the lowest for those aged less than 11 years (8.9%) (Table 1). Stings occurred throughout the year, however, the highest frequency happened in October (24.4%) (Table 2). Most of the scorpion stings occurred in summer (45.2%) and fall (39.5%) (Table 3). The maximum hits of scorpions were in housewives (28.1%) and the lowest was in the employees (10.4%) (Table 4).

Table 2. Distribution of scorpion sting cases by month in Bandar-mahshahr County, Southwestern Iran (2008-2009).

Table 3. Distribution of scorpion sting cases by season in Bandar-mahshahr County, Southwestern Iran (2008-2009).

Table 1. Distribution of scorpion sting cases by age group in Bandar-mahshahr County, Southwestern Iran (2008-2009).
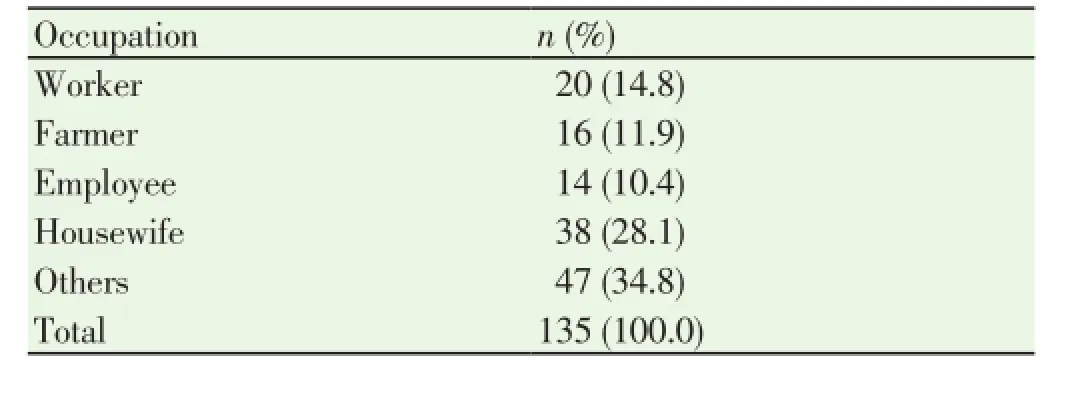
Table 4. Distribution of scorpion sting cases by occupation in Bandarmahshahr County, Southwestern Iran (2008-2009).
A total of 82 cases of cutaneous leishmaniasis were studied in this assignment that all cases have been reported from urban health centers. Considering number of lesions on the body the maximum of the patients (37.8%) had only one lesion (Table 5). From the point of lesion site view on the patient’s body, the feet and hands (31.6%, 29.3%, respectively) were the most (Table 6). Cutaneous leishmaniasis cases occurred throughout the year, however, the highest frequency happened in October (15.8%) (Table 7). The most cases documented in autumn (35.4%) and winter (25.6%) (Table 8).
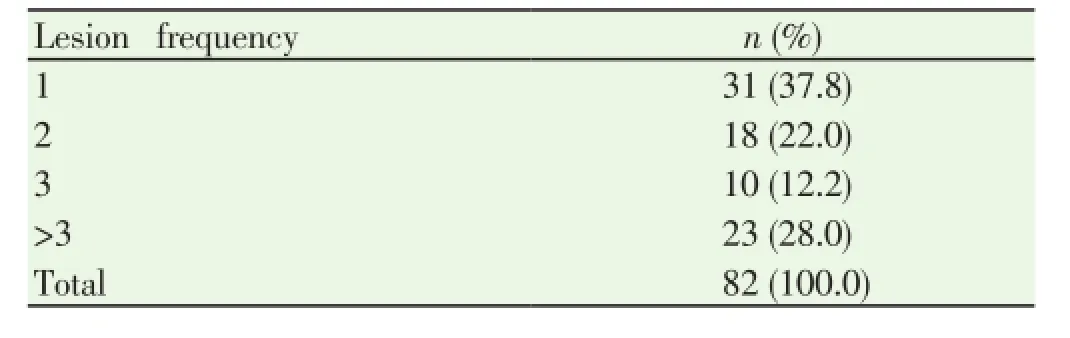
Table 5. Distribution of cutaneous leishmaniasis cases by lesion frequency in Bandar-mahshahr County, Southwestern Iran (2008-2009).

Table 6. Distribution of cutaneous leishmaniasis cases by lesion site on the body in Bandar-mahshahr County, Southwestern Iran (2008-2009).
In this study, 12 referred patients from the health centers were studied for pediculosis capitis in Bandar-mahshahr County. According to obtained information one of the patients was male (8.3%) and 11 patients (91.7%) were female. The least of pediculosis capitis cases was observed in the age group above 17 years (33.3%) and the large number of cases in the age group 11 to 17 years (66.7%). Furthermore, all cases were living in rural areas of Bandar-mahshahr County. TheP. capitiswas diagnosed for all infested patients with pediculosis and none had a history of previous infestation. In addition, the most was observed in the summer season (66.7%) and the least in autumn (33.4%).
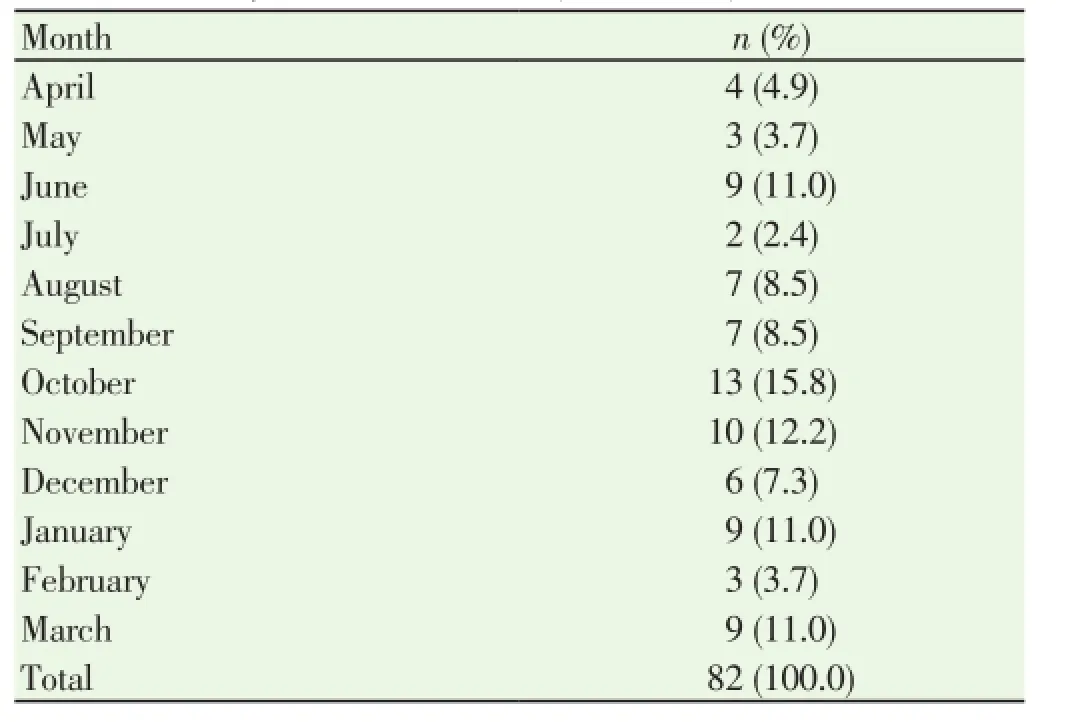
Table 7. Distribution of cutaneous leishmaniasis cases by month in Bandarmahshahr County, Southwestern Iran (2008-2009).

Table 8. Distribution of cutaneous leishmaniasis cases by season in Bandarmahshahr County, Southwestern Iran (2008-2009).
4. Discussion
Depending on the climate and weather diversity and scorpion species, stings were reported from different parts of Iran every year, especially in the warm months. The lethality of Khuzestan province’s scorpions is more than the others part of the country[7]. Evaluation of scorpion stings in referred individuals to health centers from Bandarmahshahr County and demographic and epidemiological parameters studies of 135 patients were recorded, of which 65.2% were male. The most scorpion stinging cases were reported for the range of more than 20 years of age (74.8%). In addition, from point of the job view, housewives struck the most of the patients (28.1%) for scorpion stinging. Evaluation of the scorpion stings based on the months showed that most cases have happened in the warm months (July, August, September and October) which this could be due to the increased activity of scorpions in the warm months. Investigations carried out on scorpion stings based on season indicated that most cases occurred in summer and autumn. However, the scorpion sting has not been reported in winter due to reduced activity of scorpions in this season.
Leishmaniasis is a disease that factors such as environmental changes, immigration and non-proceduralurbanization have considerable effects on the disease epidemiological aspects[41]. In addition, the natural and man-made disasters (such as earthquakes and wars) can change the face of the disease epidemiology. Among the factors that could affect the incidence of disease and change the annual incidence of cutaneous leishmaniasis can be traced in the following factors: ecological factors, abundance of vectors and reservoirs of disease, annual changes in weather and climatic conditions, the health authorities regards to the prevention and control, health education to the people, personal protection and environmental health, population immunity level, creating new foci of disease, residual spraying especially in rural regions and surveillance programs. Regardless of the reasons stated above, it seems that in some of rural cutaneous leishmaniasis foci, abundance of disease is decreased due to programs to combat malaria. However, during these years the sensitive and non-immune population increased and after discontinuation of the spraying insecticides the disease epidemics have shown itself and later reverted back to its normal level[42,43].
One of the aims of this project was to investigate cutaneous leishmaniasis in patients referred to health centers in the Bandar-mahshahr County and study of demographic and epidemiological parameters. A total of 82 patients for cutaneous leishmaniasis were studied, all which have been reported from urban health centers. The present survey, based on the number of lesions on the body, showed that the patients often had one lesion on their body. Results of an epidemiological study on 5 139 school children in the area of Isfahan’s Borkhar by Ebadi and Hejazi showed that the lesion of cutaneous leishmaniasis was revealed in the most frequent of 1 212 cases (43.9%) with one lesion[44].
According to obtained results of this study, based on the lesion on the body of patients, most of lesions were on the feet, hands and faces, respectively. Doroodgar and colleagues in their study on 5 098 rural and urban residences based on lesion location on the patients’ body, most of the ulcers were on the hands (46.6%) and then feet, faces and other parts of the body, respectively[45]. The results of the present survey on cases of cutaneous leishmaniasis by months showed that the most cases documented in October and November, respectively. This is due to the fact that sand fly’s activities are more during the wet seasons. In another study by Talari and colleagues on cutaneous leishmaniasis from Kashan County in a 7 year period, 3 028 patients were studied and the highest infection rates were documented for November and December (20% and 26%) and the lowest was in July (2.5%)[46].
The results obtained from the cutaneous leishmaniasis study by seasons showed that the lowest number of cases were observed in the spring with 16 cases (19.5%) and summer with 16 cases (19.5%) while, the most cases have been reported in fall for 29 cases (35.4%) and winter with 21 cases (25.6%), respectively. Results of an epidemiological study on cutaneous leishmaniasis for 5 139 school children in the region of Borkhar of Esfahan by Ebadi and Hijazi showed that 33.1% of the patients had scar and 6.2% had active ulcer. Having a scar or active ulcer had a significant association with age, sex and parental education however; there was not a significant relationship with residential areas. From lesion site point of view on the patient body, 35.3% lesions were on faces, 29.2% on hands, 27% on feet, 6.7% on trunk and 1.8% in the neck, respectively[44].
The public’s general health is very important so that, the society progress is depending on the individual’s general health. Among the threats to public health, insect infestation, especially ectoparasites are the most important agents that despite health promotion and advancement of medical science, it is still considered to be a health problem[32]. Human sucking lice can transmit diseases such as epidemic typhus and epidemic relapsing fever and has long been considered by various researchers. Head lice infestation can be seen in abundance in all parts of the world including Iran, especially in areas with high population density and combined with poverty and lack of personal hygiene principles. This is a common infestation among children, especially in rural areas. Head lice infestation in patients leads to feelings of inferiority and inadequacy, creating mental stimulation, depression and insomnia[31].
The other objective of this project was to investigate pediculosis capitis in referrals to health centers from Bandar-mahshahr County and the study of demographic and epidemiological indices. In this study, 12 referred pediculosis patients to the health centers from Bandarmahshahr County were studied with regard to the information obtained. Among the reported pediculosis cases in 2008-2009, 91.7% were women. The survey also revealed that most infested individuals from pediculosis based on the age group were reported in younger than 17 years. This could possibly be due to their self-sufficient inattention to personal hygiene. The patients with pediculosis were also studied from the point of residential view. All pediculosis cases in 2008-2009 were residents of the city regions. In addition, the study was carried out on the lice type and the history of the infested individuals based. It was cleared that all cases have been infested with P. capitis and none of them have been previously infested. Investigations on pediculosis cases based on month showed that all reported cases by health centers were in August, September and October and in the remaining months of the year no cases have been reported. Furthermore, the survey according to season revealed that8 cases of the disease have been occurred in summer and 4 cases in autumn.
The highest scorpion stings and its mortality rate in the southern provinces; south-west and south-east of the country make double the importance for prevention and control. Currently, with regard to the socio-economic and climate condition of provinces, 80% of scorpion stings were occurred in the southern provinces, the south- east and south-west and the Khuzestan Province allocated the first rank of scorpion stings among other provinces.
Scorpion fauna distribution with biological diversity, behavior properties and lack of information in this field are other confronting challenges that multiply the problem for scorpion stings. The venom of some dangerous species of scorpion causes lysis of red blood cells, and venom of some species of scorpions is more lethal that its effects are in the form of nervous system symptoms. It seems that some preventive actions such as repairing cracks and crevices of buildings keep away logs and twigs from the living area and not sleeping in the open air outside the building, reduce the number of scorpion stings.
Some important measures that should be implemented including; homes protection, prevent the increase of scorpions population, protection of victims before transmitting the casualty to medical centers, applying single protocol at different levels for the treatment of scorpion stings, trying to improve reporting and information system, education and public participation, strengthen inter-sectoral coordination, execution of useful researches and strengthen and resources development.
Epidemiologic factors such as age, gender, season and travel to endemic areas effect on the prevalence of cutaneous leishmaniasis. These factors can be used to design and evaluate effective prevention and control programs. The appropriate information should be made to public about the disease and ways of transmission and prevention through mass media, schools and health centers, and even country points out. In addition, members of society in case of feeling the bite of insects and observation the skin lesions such as papules must see a doctor as soon as possible to prevent the lesions spread and transmission of the disease to others through a timely and quick diagnosis of disease. Moreover, it seems that if the reporting system for insect transmitted diseases (including cutaneous leishmaniasis) taken seriously and act quickly in infected areas; by insecticides spraying, the local transmission of the disease can be significantly reduced.
As the study’s results show the head lice infestation still is a major problem in countries with poor hygiene and deprived living facilities as well as the bad economic situation. The infestation does not depend only on one factor but several factors such as; families’ socio-economic status, health education and culture, raising the families education level, family planning and reducing family size, and the welfare facilities.
The solution for this and many other problems that are related to the cultural, economic and social, needs the participation of various parts of government such as the Ministry of Education, the Ministry of Health and Medical Education, Welfare Organization, Imam Khomeini Relief Committee, students and their families, and even institutions like the City Council, parents and teachers society.
Conflict of interest
The authors declare that there is no conflict of interest.
Acknowledgements
The authors are grateful to staffs of Bandar-mahshahr health services centers for their contribution and help. This research was supported by the project No. 88S.96 Ahvaz Jundishapur University of Medical sciences Vice-Chancellor for Research affairs.
[1] WHO. Rabies and envenoming. Report of consultative meeting. Geneva: World health organization; 2007.
[2] Farzanpay R. Scorpion Knowledge. Tehran: Academic press; 1987, p. 284[In Persian].
[3] Zargani J. Reproductive biology and comparative study on effects telson cut in affair behavior of three species of scorpions in Iran. MSPH Thesis. Tehran: Tehran Univ Med Sci 1998, p. 194[In Persian].
[4] Kamali K. Scorpions of Khuzestan, treatment of scorpion sting and how to control them. J Elmi Keshavarzi 1984; 1: 1-31[In Persian].
[5] Chaichi M. Iran is the most important country about scorpionism in the world. J Salamat 2006[In Persian].
[6] Harrison TR, Fauci AS, Braunwald E. Harrison’s principles of internal medicine. New York: MC Craw Hill Co; 2005, p. 2604.
[7] Labafgahsemi R. Status of scorpion sting in Iran and its prevention. J Behvarz 1999; 2(10): 32-35[In Persian].
[8] Iranian Ministry of Health and Medical Education. Annual report of center for diseases control. 2005-2006. Tehran: Iranian Ministry of Health and Medical Education [In Persian].
[9] Afzali N, Pezeshki N. Surveying of kidney acute dysfunction following Hemiscorpius lepturus sting in children. J Med Sci Ahwaz Jundishapour Univ Med Sci 1998; 25: 42-48[In Persian].
[10] Akbari A, Tabatabai M, Hedayat A, Modir-Rosta H, Alizadeh M, Kamal-Zareh M. Study of the geographical distribution of scorpions in the south of Iran. J Pajohesh Va Sazandegi 1997; 34: 112-115[In Persian].
[11] Radmanesh M. Survey of scorpionism. J Daru va Darman 1990; 7(76): 26-30[In Persian].
[12] Chitnis PA, Maraghi S, Vazirianzadeh B. Epidemiological and laboratory study on scorpion stings in Khuzestan province. J Med Fac Guilan Univ Med Sci 1993; 2: 5-12[ In Prsian].
[13] Iranian Ministry of Health and Medical Education, Center for disease control. Instruction of Leishmaniasis Control. Tehran: Iranian Ministry of Health and Medical Education; 1999, p. 68[In Persian].
[14] Markele WH, Khaldoun MMO. Cutaneous Leishmaniasis, recognition and treatment. Am Fam Physic 2004; 69: 455-460.
[15] Ghorori MJ. Medical Protozoology. Publishing tabib: The Cultural Institute Tymorzadeh publishing; 1999, p. 160-178[In Persian].
[16] Iranian Ministry of Health and Medical Education. Offic of Disease Prevention and Care. Statistics on the incidence of cutaneous leishmaniasis. Tehran: Iranian Ministry of Health and Medical Education; 1999[In Persian].
[17] Iranian Ministry of Health and Medical Education. Office of Disease Prevention and Care. Guidelines on lesihmaniasis control. Tehran: Iranian Ministry of Health and Medical Education; 1999[In Persian].
[18] Brown HW, Neva FA. Basic clinical parasitology. 5th Edition. New York: Appleton Century Crofts; 1983, p. 62-72.
[19] World Health Organization. The leishmaniasis. WHO Tech Rep Ser No. 701. Geneva: World health organization; 1984, p. 2-4.
[20] World Health Organization. WHO Tech Rep Ser No. 793. Expert committee: Epidemiological aspects, Control of the leishmaniasis. Geneva: World health organization; 1990, p. 41-46.
[21] Ashford RW. Leishmaniasis reservoirs and their significance in control. Clin Dermatol 1996; 14(5): 523-532.
[22] Desjeux P. Disease watch focus, Leishmaniasis. Nature Rev Microbiol 2004; 2: 692-693.
[23] Mohebali M, Yaghoobi P, Hooshmand B, Khamesipour A. Efficacy of Paromomycin ointment prepared in Iran (Paromo-U) against cutaneous Leishmaniasis caused by Leishmania major in mouse model. Iranian J Dermato 2004; 26: 88-94[In Persian].
[24] WHO. Leishmaniasis and leishmania/HIV co-infection. In: WHO report on global surveillance of epidemic-prone ifectious diseases. Geneva: WHO; 2000, p.121-127.
[25] Yaghoobi-Ershadi MR, Zahraei-Ramezani AR, Akhavan AA, Jalali-Zand AR. Rodent control operations against zoonotic cutaneous leishmaniasis in Iran. Ann Saudi Med 2005; 25(4): 309-312.
[26] Athari A, Jalallu N. Epidemiological survey of cutaneous leishmaniasis in Iran 2001-2005. Sci J Isfahan Univ Med Sci 2006; 24(82): 8-13[In Persian].
[27] Javadian E, Nadim A, Tahvildari A, Assefi V. Epidemiology of cutaneous leishmaniasis in Korassan Privince, Iran. Bull Soc Pathol Exot Filiales 1976; 69(2): 140-143.
[28] Moaddeb A, Gettner S, Ardehali S. Studies on the causative agent of cutaneous leishmaniasis in Shiraz, Iran. Iran J Med Sci 1993; 18(1,2): 28-33.
[29] Salimi MA. Clinical and epidemiological comparison on the cutaneous leishmaniasis in the city and villages of Isfahan. Iran J Public Health 2000; 2(4): 214-219[In Persian].
[30] Nadim A, Seyedi - Rashti MA. A brief review of the epidemiology of various types of leishmaniasis in Iran. Acta Med Iran 1971; 8(4): 99-106.
[31] Zaim M, Seyedi Rashti MA, Saebi MA. A textbook on Medical Entomology. Tehran: Tehran University Press; 2004, p. 297-308[In Persian].
[32] Safi MH. Prevalence of Pediculus capitis infestation and related factors in infestation in children of elementary schools in Islamshahr County. Tehran. MSPH Thesis. Tehran University of Medical Sciences. 1996[In Persian].
[33] Golchai J, Ahmadi - Ghajari M. Study on the prevalence of Pediculus capitis among children aged 3-7 years in nursery schools of Rasht. J Med School, Guilan Univ Med Sci 2002; 11(41): 21-24[In Persian]
[34] Kokturk A, Baz K, Bugdayci R, Sasmaz T, Tursen U, Kaya TI, et al. The prevalence of pediculosis capitis in school children in Mersin. Turkey Int J Dermatol 2003; 42(9): 694-698.
[35] Ghavami MB. Medical Entomology. 1st ed. Zangan Publication. 1998, p. 243.
[36] Mnosen K, Olson L. A population base approach to pediculosis management. Publ Health Nurse 2002; 19(3): 201-208.
[37] Hensel P. The challenge of choosing a pediculicide. Publ Health Nurse 2000; 17(4): 1-2.
[38] Koch T, Brown M, Selim P, Isam C. Towards the eradication of head lice: literature review and research agenda. J Clin Nura 2001; 10: 364-377.
[39] Motavalli-Haghi F, Sharif M, Sedaghat MM, Gholami S. Head louse infestation rate in primary school students town-ship Sari in 1997-1998. J Mazandaran Univ Med Sci 1999; 9(24): 44-48[In Persian].
[40] Schenone H, Wiedmaier G , Contreras L . Treatment of pediculosis capitis in children with permethrin shampoo or lotion. Bol child parasitol 1994, 49(3-4): 49-52.
[41] Aflatonian MR, Sharifi I. The frequency of cutaneous leishmaniasis in people referred to health centers of bam County during 2000-2004. J Rafsanjan Univ Med Sci 2006; 5(2): 123-128[In Persian].
[42] WHO. Studies of leishmaniasis vectors/reservoirs and their control in the world, part 2, WHO/VBC/80. No.779. Geneva: WHO; 1980, p. 34.
[43] Vatandoost H, Hanafi-Bojd AA. Medical and veterinary ectoparasites. 1st ed. Tehran: Tehran University of medical sciences publication; 2002, p. 103-107[In Persian].
[44] Ebadi M, Hejazi SH. Epidemiology of cutaneous leishmaniases in the students of primary schools in Borkhar region, Isfahan. J Kerman Uni Med Sci 2003; 10(2): 92-98[In Persian].
[45] Doroodgar A, Mahboubi S, Nematyan M, Sayyah M, Doroodgar M. Epidemiology of Cutaneous Leishmaniasis in Kashan County in 2007-2008. J Semnan Univ Med Sci 2009; 10(3): 177-184[In Persian].
[46] Talari SA, Vakili Z, Moshtaghi S. A survey of cutaneous leishmaniasis in Kashan County during 1994-2000. J Feyz 2003; 26: 71-76[In Persian].
ment heading
10.1016/S2221-6189(14)60043-3
*Corresponding author: Mohammad-Hossein Feizhaddad and Hamid Kassiri, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
Tel: +986113738269
Fax: +986113738282
E-mail: Hfeizhaddad@yahoo.com; Hamid.kassiri@yahoo.com
杂志排行
Journal of Acute Disease的其它文章
- Posterior reversible leukoencephalopathy syndrome presenting in a post-partum, 25-year-old-female with concomitant subarachnoid hemorrhage
- Cardioprotective potential of hydro-alcoholic fruit extract of Ananas comosus against isoproterenol induced myocardial infraction in Wistar Albino rats.
- Patients with the tako-tsubo cardiomyopathy-clinical evaluation and outcome
- Acute brain hemorrhage in dengue
- The epidemiology of tick-borne relapsing fever in Bijar County, North-Western Iran
- Heart, tracheo-bronchial and thoracic spine trauma. Succesful multidisciplinary management: a challenging thoracic politrauma
