A minimally invasive multiple percutaneous drainage technique for acute necrotizing pancreatitis
2014-03-20TakeroTerayamaToruHifumiNobuakiKiriuHiroshiKatoYuichiKoidoYoshiakiIchinoseKoheiMorimotoKurodaYasuhiro
Takero Terayama, Toru Hifumi, Nobuaki Kiriu, Hiroshi Kato, Yuichi Koido, Yoshiaki Ichinose, Kohei Morimoto, Kuroda Yasuhiro
1Division of Critical Care Medicine and Trauma, National Hospital Organization Disaster Medical Center, Tachikawa, Tokyo 190-0014, Japan
2Emergency Medical Center, Kagawa University Hospital, Miki, Kita, Kagawa 761-0793, Japan
3Division of Radiology, National Hospital Organization Disaster Medical Center, Tachikawa, Tokyo 190-0014, Japan
Corresponding Author:Toru Hifumi, Email: hifumitoru@gmail.com
A minimally invasive multiple percutaneous drainage technique for acute necrotizing pancreatitis
Takero Terayama1, Toru Hifumi2, Nobuaki Kiriu1, Hiroshi Kato1, Yuichi Koido1, Yoshiaki Ichinose3, Kohei Morimoto3, Kuroda Yasuhiro1
1Division of Critical Care Medicine and Trauma, National Hospital Organization Disaster Medical Center, Tachikawa, Tokyo 190-0014, Japan
2Emergency Medical Center, Kagawa University Hospital, Miki, Kita, Kagawa 761-0793, Japan
3Division of Radiology, National Hospital Organization Disaster Medical Center, Tachikawa, Tokyo 190-0014, Japan
Corresponding Author:Toru Hifumi, Email: hifumitoru@gmail.com
BACKGROUND:In approximately 20% of patients, necrotizing pancreatitis is complicated with severe acute pancreatitis, with high morbidity and mortality rates. Minimally invasive step-up approach is both safe and effective, but sometimes requires multiple access sites.
METHODS:A 62-year-old woman was admitted with diabetic ketoacidosis, and initial computed tomography (CT) revealed no evidence of acute pancreatitis. She was clinically improved with insulin therapy, fl uid administration, and electrolyte replacement. However, on the 14thday of admission, she developed a high-grade fever, and CT demonstrated evidence of acute necrotizing pancreatitis with a large collection of peripancreatic fl uid. Percutaneous transgastric drainage was performed and a 14 French gauge (Fr) pigtail catheter was placed 1 week later, which drained copious pus. Because of persistent high-grade fever and poor clinical improvement, multiple 8 and 10 Fr pigtail catheters were placed via the initial drainage route, allowing the safe and effective drainage of the extensive necrotic tissue that was occupying the bilateral anterior pararenal space.
RESULTS:After drainage, the patient recovered well and the last catheter was removed on day 123 of admission.
CONCLUSIONS:Multiple percutaneous drainage requires both careful judgment and specialist skills. The perforation of the colon and small bowel as well as the injury of the kidney and major vessels can occur. The current technique appears to be safe and minimally invasive compared with other drainage methods in patients with extended, infected necrotic pancreatic pseudocysts.
Percutaneous drainage; Acute necrotizing pancreatitis; Minimally invasive technique
INTRODUCTION
In approximately 20% of patients, necrotizing pancreatitis complicates severe acute pancreatitis, and is associated with a mortality rate of 8%–39%.[1]Secondary infection of necrotic tissue is an indication for intervention;[2]however, the traditional approach of open necrosectomy to completely remove the infected necrotic tissue is highly invasive with high morbidity and mortality.[3–5]Alternative less invasive techniques include percutaneous drainage,[6]endoscopic (transgastric) drainage,[7]and minimally invasive retroperitoneal necrosectomy.[8]These therapies are associated with fewer complications but often require repeat procedures from multiple sites to achieve adequate drainage of all the necrotic tissue, which can cause major bleeding and/or perforation of visceral organs.[9–11]We report the first case of acute necrotizing pancreatitis that was successfully treated with minimally invasive multiplepercutaneous drainage using pre-exiting access site of percutaneous transgastric drainage.
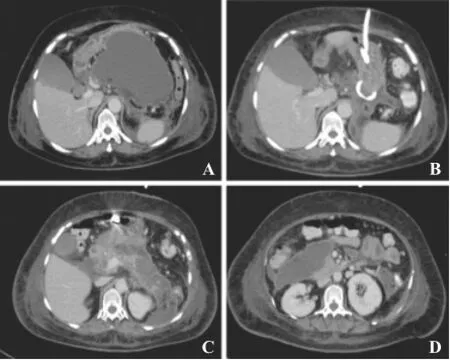
Figure 1. Abdominal computed tomography images. Pseudocyst in the omental bursa on computed tomography (CT) scan on the 22ndday of admission (A). CT scan on the 29thday of admission revealed remarkable progress with percutaneous transgastric drainage tube placed in the omental bursa (B). There was no notable change to the pseudocyst in bilateral anterior pararenal space (C, D).
CASE REPORT
A 62-year-old woman was admitted with diabetic ketoacidosis (pH 7.222; blood glucose, 1 570 mg/dL; positive urine ketones). Initial whole body computed tomography (CT) scan was performed but found no evidence of acute pancreatitis. She was clinically improved with insulin therapy, fluid administration, and electrolyte replacement. However, on the 14thday of admission, she developed a high-grade fever, and CT demonstrated a large peripancreatic fl uid collection associated with acute necrotizing pancreatitis (Figure 1A). Intravenous antibiotic treatment with tazobactam and piperacillin was initiated. Percutaneous transgastric drainage was performed and a 14 French (Fr)-gauge pigtail catheter was placed 1 week later, and a copious amount of thick pus was drained.
However, there was little clinical improvement and another percutaneous drainage was planned after a repeat CT demonstrated progressing fluid collections in the bilateral pararenal spaces (Figure 1B-D). Because surgical procedures were considered too invasive in this patient, multiple 8 and 10 Fr-gauge pigtail catheters were placed using the initial drainage route via guide wires (Figure 2 and Figure 3A-D). Because of daily drainage and lavage using a saline solution, hematological evidence of in fl ammation gradually improved; C-reactive protein (CRP) improved from 19 to 1 mg/dL.The catheter in the omental bursa was removed on day 107 of admission, with the remainder being removed on day 122. She was mobile with a stick by day 160 and was discharged on day 193. After removal of the catheters, there was no recurrence and the CRP remained below 2.0 mg/dL.

Figure 2. Percutaneous drainage tubes using the initial percutaneous transgastric drainage access site. Three drainage tubes were placed using initial percutaneous transgastric drainage route.

Figure 3. Computed tomography scan on the 50thday of admission after minimally invasive multiple percutaneous drainage. Three catheters were placed: catheter A (⌂) (patient's left side), catheter B (Δ) (center), and catheter C (↑) (right). Each catheter passed through the abdominal skin, the anterior wall of the stomach and the posterior wall, before reaching their fi nal placement. Catheter A (⌂) was placed in the left pararenal space, catheter B (Δ) in the omental bursa, and catheter C (↑) in the right pararenal space. The jejunal tube () was placed for enteral feeding.
DISCUSSION
We report a new technique that safely and effectively controlled infection associated with extensive necrotic tissue in acute necrotizing pancreatitis. Van Santvoort etal[9]conducted a multicenter trial comparing a minimally invasive step-up approach with open necrosectomy for necrotizing pancreatitis, and concluded that minimally invasive percutaneous or endoscopic transgastric drainage is the preferred treatment strategy for patients with necrotizing pancreatitis. If necessary, they stated that it could be followed up with minimally invasive retroperitoneal necrosectomy. However, percutaneous drainage requires repeated procedures, which limit its implementation in clinical practice. Freeny et al[6]first described successful percutaneous drainage of infected pancreatic necrosis. In this report of 34 patients with infected necrosis, each patient required 3 separate catheter sites and 4 exchanges for removal of necrotic material. Bakker et al[12]conducted a randomized control study in which they compared endoscopic transgastric necrosectomy with surgical necrosectomy for infected necrotizing pancreatitis, and they concluded that endoscopic necrosectomy demonstrated a significantly lower rate of major complications and death. However, this technique also requires repeated procedures to remove a majority of the necrotic materials. Moreover, because it requires both advanced skill and medical equipment, this technique cannot be effectively performed at all institutions in clinical practice, despite strong clinical evidence.[12,13]Extension into the paracolic gutters may require adjuvant percutaneous/retroperitoneal techniques. Both proposed techniques could require multiple approach sites to drain all necrotic tissue, and therefore could pose a major risk of complication, including major bleeding and/ or perforation of visceral organs.
Our technique required only one access site and was therefore less invasive and safer than conventional techniques. The management of acute necrotizing pancreatitis should be tailored according to needs of individual patients, and this new technique may have a broad range of applicability.
In conclusion, the current technique appears to be safe and minimally invasive compared with other drainage methods in patients with extended, infected necrotic pancreatic pseudocysts.
ACKNOWLEDGMENTS
The authors thank the ICU staff and the laboratory team of the National Hospital Organization Disaster Medical Center.
Funding:None.
Ethical approval:The study was approved by the Ethical Committee of the National Hospital Organization Disaster Medical Center, Tokyo 190–0014, Japan.
Con fl icts of interest:The authors declare that they have no competing interests.
Contributors:TT, TH, NK, YI and KM treated patients. TT and TH wrote the manuscript. NK, HK, and YK revised and edited the manuscript. All authors read and approved the fi nal manuscript.
REFERENCES
1 Banks PA, Freeman ML. Practice guidelines in acute pancreatitis. Am J Gastroenterol 2006; 101: 2379–2400.
2 Nathens AB, Curtis JR, Beale RJ, Cook DJ, Moreno RP, Romand JA, et al. Management of the critically ill patient with severe acute pancreatitis. Crit Care Med 2004; 32: 2524–2536.
3 Traverso LW, Kozarek RA. Pancreatic necrosectomy: de fi nitions and technique. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract 2005; 9: 436–439.
4 Rau B, Bothe A, Beger HG. Surgical treatment of necrotizing pancreatitis by necrosectomy and closed lavage: changing patient characteristics and outcome in a 19-year, single-center series. Surgery 2005; 138: 28–39.
5 Rodriguez JR1, Razo AO, Targarona J, Thayer SP, Rattner DW, Warshaw AL, et al. Debridement and closed packing for sterile or infected necrotizing pancreatitis: insights into indications and outcomes in 167 patients. Annals of surgery 2008; 247: 294–299.
6 Freeny PC, Hauptmann E, Althaus SJ, et al. Percutaneous CT-guided catheter drainage of infected acute necrotizing pancreatitis: techniques and results. AJR Am J Roentgenol 1998; 170: 969–975.
7 Papachristou GI1, Takahashi N, Chahal P, Sarr MG, Baron TH. Peroral endoscopic drainage/debridement of walled-off pancreatic necrosis. Ann Surg 2007; 245: 943–951.
8 Connor S, Alexakis N, Raraty MG, Ghaneh P, Evans J, Hughes M, et al. Early and late complications after pancreatic necrosectomy. Surgery 2005; 137: 499–505.
9 van Santvoort HC, Besselink MG, Bakker OJ, Hofker HS, Boermeester MA, Dejong CH, et al. A step-up approach or open necrosectomy for necrotizing pancreatitis. N Engl J Med 2010; 362: 1491–1502.
10 Charnley RM, Lochan R, Gray H, O'Sullivan CB, Scott J, Oppong KE. Endoscopic necrosectomy as primary therapy in the management of infected pancreatic necrosis. Endoscopy 2006; 38: 925–928.
11 Carter R. Management of infected necrosis secondary to acute pancreatitis: a balanced role for minimal access techniques. Pancreatology 2003; 3: 133–138.
12 Bakker OJ, van Santvoort HC, van Brunschot S, Geskus RB, Besselink MG, Bollen TL, et al. Endoscopic transgastric vs surgical necrosectomy for infected necrotizing pancreatitis: a randomized trial. JAMA 2012; 307: 1053–1061.
13 Varadarajulu S, Bang JY, Sutton BS, Trevino JM, Christein JD, Wilcox CM. Equal efficacy of endoscopic and surgical cystogastrostomy for pancreatic pseudocyst drainage in a randomized trial. Gastroenterology 2013; 145: 583–590 e581.
Received May 12, 2014
Accepted after revision September 25, 2014
World J Emerg Med 2014;5(4):310–312
10.5847/wjem.j.issn.1920–8642.2014.04.012
杂志排行
World journal of emergency medicine的其它文章
- Current pre-hospital traumatic brain injury management in China
- Emergency bedside ultrasound for the diagnosis of pediatric intussusception: a retrospective review
- How to secure the connection between thoracostomy tube and drainage system?
- Clinical probability and risk analysis of patients with suspected pulmonary embolism
- Thyroid hormone alterations in trauma patients requiring massive transfusion: An observational study
- The incidence of oxygen desaturation during rapid sequence induction and intubation
