The incidence of oxygen desaturation during rapid sequence induction and intubation
2014-03-20
Department of Anesthesia, School of Medicine, Gondar College of Medicine and Health Sciences, University of Gondar, Gondar 196, Ethiopia
Corresponding Author:Endale Gebreegziabher Gebremedhn, Email: endalege@yahoo.com
The incidence of oxygen desaturation during rapid sequence induction and intubation
Endale Gebreegziabher Gebremedhn, Desta Mesele, Derso Aemero, Ehtemariam Alemu
Department of Anesthesia, School of Medicine, Gondar College of Medicine and Health Sciences, University of Gondar, Gondar 196, Ethiopia
Corresponding Author:Endale Gebreegziabher Gebremedhn, Email: endalege@yahoo.com
BACKGROUND:Rapid sequence induction and intubation (RSII) is an emergency airway management technique for patients with a risk of pulmonary aspiration. It involves preoxygenation, administration of predetermined doses of induction and paralytic drugs, avoidance of mask ventilation, and laryngoscopy followed by tracheal intubation and keeping cricoid pressure applied till endotracheal tube cuff be inflated. Oxygen desaturation has been seen during RSII. We assessed the incidence of oxygen desaturation during RSII.
METHODS:An institution-based observational study was conducted from March 3 to May 4, 2014 in our hospital. All patients who were operated upon under general anesthesia with RSII during the study period were included. A checklist was prepared for data collection.
RESULTS:A total of 153 patients were included in this study with a response rate of 91.6%. Appropriate drugs for RSII, equipments for RSII, equipments for dif fi cult intubation, suction machine with a catheter, a monitor and an oxygen backup such as ambu bag were not prepared for 41 (26.8%), 50 (32.7%), 51 (33.3%), 38 (24.8%) and 25 (16.3%) patients respectively. Cricoid pressure was not applied at all for 17 (11.1%) patients and 53 (34.6%) patients were ventilated after induction of anesthesia but before intubation and endotracheal cuff inflation. A total of 55 (35.9%) patients desaturated during RSII (SPO2<95%). The minimum, maximum and mean oxygen desaturations were 26%, 94% and 70.9% respectively. The oxygen desaturation was in the range of <50%, 50%–64%, 65%–74%, 75%–84%, 85%–89 % and 90%–94% for 6 (3.9%), 7 (4.6%), 5 (3.3%), 10 (6.5%), 13 (8.5%) and 14 (9.2%) patients respectively.
CONCLUSION:The incidence of oxygen desaturation during RSII was high in our hospital. Preoperative patient optimization and training about the techniques of RSII should be emphasized.
General anesthesia; Rapid sequence induction and intubation; Oxygen desaturation
INTRODUCTION
Rapid sequence induction and intubation (RSII) is the administration of a potent induction agent followed by a rapidly acting neuromuscular blocking agent to induce unconsciousness and motor paralysis for tracheal intubation for patients with the risk of pulmonary aspiration.[1]Cricoids pressure is applied from the moment the patient loses consciousness until the endotracheal cuff is in fl ated.[2]
Desaturation is defined as oxygen saturation < 90% from the initial SPO2of >90% or a decrease from a baseline of less than 90%.[3]The rate of oxygen desaturation during apnea is affected by body hemoglobin concentration and oxygen consumption.[4]Desaturation <70% puts patients at risk for dysrhythmias, hemodynamic decompositions, hypoxic brain injury, and death.[5]Desaturation <90% developed during rapid sequence intubation in 15 (15%) of 101 patients with trauma managed by anesthesiologists and in 19 (18%) of 99 patients managed by emergency physicians.[6]Suxamethonium was recognized the muscle relaxant of choice for RSII because of its fast onset of action.[7]RSII could be performed when there was an increased risk of pulmonary aspiration of gastric content.[8]
In a study,[9]the administration of thiopental and suxamethonium 1.0 mg/kg, without assisted ventilation but close monitoring of oxygen saturation levels, patients showed desaturation to SPO2<80%. Another study[10]found that the reduction of suxamethonium dose from 1.0 mg/kg to 0.6 mg/kg slightly lowered the incidence of oxygen desaturation <90% (from 85% to 65%).
An American study[11]revealed that after 3 minutes of preoxygenation, the patients were given sedatives and muscle relaxants to decrease their saturation from 100% to 95%. Desaturation of less than 90% appeared during rapid sequence intubation in 15 (15%) of 101 patients with trauma managed by anesthesiologists and in 19 (18%) of 99 patients managed by emergency physicians.[12]
The mean recovery time was 43 (39–48) seconds in succinylcholine vs. 36 (33–38) seconds in rocuronium.[13]Desaturation to below 70% puts patients at risk for dysrhythmia, hemodynamic decomposition, hypoxic brain injury, and death.[14]
A study[15]from China showed that apnea was always present during rapid sequence induction of general anesthesia in obese patients. Patients might have an increased risk of hypoxia due to the diminished oxygen reserve during the induction of general anesthesia whose body mass index was >26 kg/m2.[16]Preoxygenation provides an oxygen reservoir that will delay the depletion of oxygen in the absence of ventilation (after paralysis) for up to 8 minutes in healthy adults.[17]
Many patients with the risk of pulmonary aspiration have been operated on under general anesthesia with RSII in our hospital. Oxygen desaturation has been seen during RSII. The present study was to assess the incidence of oxygen desaturation during RSII.
METHODS
Patients
An institution-based observation study was conducted from March 3 to May 4, 2014.
All (elective, emergency, major, minor, obstetrics, gynecological and surgical) patients who were operated upon under general anesthesia with RSII at our hospital were included.
Patients who were below 18 years old, contraindicated for succinylcholine, had difficult intubation warranting awake fiberoptic intubation, absence of a qualified anesthetist, and those who were operated on under spinal anesthesia, general anesthesia with sedation and laryngeal mask airway were excluded.
Variables
Socio-demographic variables included sex, age, ASA status, type of operation, surgical subspecialty, presence of respiratory disease, history of cigarette smoking, preoperative alcohol intake, seniority of anesthetist, service year of anesthetists, RSII training after graduation, prophylactic agents for pulmonary aspiration, pre-induction desaturation, pre-induction vital signs (before 5 minutes), and patient position during induction of anesthesia.
Preoperative airway was assessed in terms of OPV status, airway deformity, preoperative airway obstruction, and preoperative oxygen desaturation.
Before operation, equipments for RSII, equipments for difficult intubation, suction machines, monitoring devices, oxygen, and oxygen backup.
In prevention of pulmonary aspiration, cimetidine, sodium citrate, and metoclopramide were administered before anesthesia.
Intubation agents included thiopental, ketamine, propofol, succinylcholine, vecuronium, and pancuronium.
Monitoring equipments included ECG, pulseoximeter, capnograph, thermometer, glucometer, etc.
Factors related with techniques of RSII
Preoxygenation, suction machine connected with a suction catheter connected and turned on (before induction, after induction, not done), type of induction drugs used, landmark identification for cricoid pressure (before induction of anesthesia, after induction of anesthesia but before loss of consciousness, both after induction of anesthesia and loss of consciousness, not done), qualification of assistant who applied cricoid pressure, number of laryngoscopy attempts during RSII, oxygen desaturation during RSII and dif fi cult intubation during RSII (type, measure).
Complications of RSII included hypertension, hypotension, tachycardia, bradycardia, bronchospasm, laryngospasm, pulmonary aspiration, and cardiopulmonary arrest.
Operational de fi nitions
According to the WHO definition, the patients were classified as having desaturated if the oxygen saturation was <95%.[21]A decrease in oxygen saturation was foundby continuous monitoring with pulseoximetry at any time between the start of induction of anesthesia and the completion of the intubation. Recovery period: The time lasted from the initiation of ventilation after desaturation during RSII to the time when the oxygen saturation returned to >95%.
Definition of RSII: A technique used by a practising anesthetist consisted of preoxygenation, rapid administration of predetermined doses of both induction and paralytic drugs with rapid onset and offset of actions, concurrent application of cricoid pressure, avoidance of bag and mask ventilation, and direct laryngoscopy followed by tracheal intubation using a suction machine with a suction catheter and cricoid pressure applied till the in fl ation of endotracheal tube cuff.
Time of cricoid pressure application: The anatomic landmark for cricoid pressure was identified before induction and application of cricoid pressure after loss of consciousness or anatomic landmark or both anatomic landmark identi fi cation and cricoid pressure application were done after induction and loss of consciousness.
If anatomic landmark is identi fi ed before the induction of anesthesia, 10 N can be applied and continues with 20–30 N after induction till the endotracheal tube cuff is being inflated. Since it is a critical and life-saving technique, it should be applied for every patient with risk of aspiration unless there is a special consideration.
Data processing and analysis
The checklist was checked for completeness, cleaned manually, entered and analyzed using SPSS version 20.0 for windows. Frequencies and cross tabulations were used to summarize the descriptive statistics of the data, and tables were used for data presentation.
Ethical approval was obtained from the Ethical Review Committee of School of Medicine, Gondar College of Medicine and Health Sciences, University of Gondar. Con fi dentiality was ensured using an anonymous checklist and keeping the checklist locked.
RESULTS
Socio-demographic characteristics of the participants
A total of 286 patients were operated upon under general anesthesia during the study period. One hundred and sixty-seven of the 286 patients were operated on under general anesthesia with rapid sequence induction and intubation. Fourteen of the 167 patients were excluded from the study due to incomplete filling of the checklist. A total of 153 patients were included in this study with a response rate of 91.6%. Males accounted for 54.2% of the participants. The minimum, maximum and median ages of the patients were 18, 75 and 28 years respectively. The ages of 45 (29.4%) patients were in the range of 18–24, 36 (23.5%) in the range of 25–29, 36 (23.5%) in the range of 30–39, 23 (15%) in the range of 40–49, 7 (4.6%) in the range of 50–59, 2 (1.3%) in the range of 60–65 and 4 (2.6%) in the range of > 65 years old respectively.
Most of operations 87 (56.9%) were done by anesthetists with less than one-year services, 21 (13.7%) with 1–2 years of services, 29 (18.9%) with 3–5 years of services, and 16 (10.5%) with more than 5 years of services. The majority of 137 (89.5%) patients were emergency patients, whereas 14 (9.5%) were elective patients (Table 1).
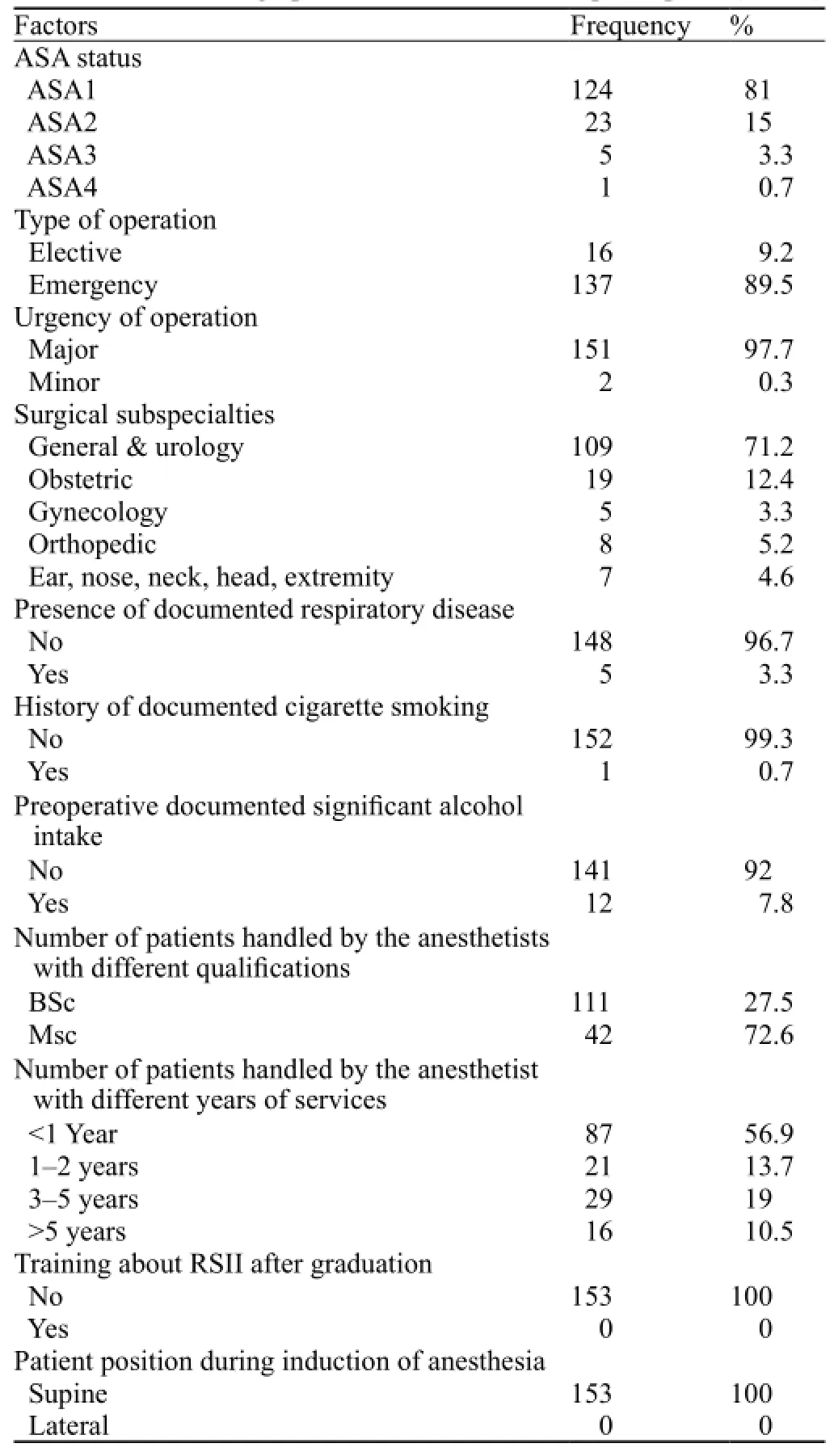
Table 1. Socio-demographic characteristics of the participants (n=153)
Preoperative patient status and preparation for rapid sequence induction and intubation
No patient had a history of respiratory disease, cigarette smoking and significant alcohol intake. The preoperative vital signs of the patients were (5–10 minutes before the induction of anesthesia): BP=118±15.9/78 (78–70) mmHg [(mean±SD/mean (IQR)], PR=91.9±17.55 beats/minute (mean±SD), RR=22 (24–20) beats/minute and SPO2=94.2%±10.12% respectively. Nine patients desaturated before anesthesia and surgery. The oxygen saturation of 4 (2.6%) patients was in the range of 85%–89%, 3 (2.0%) patients in the range of 74%–85%, 1 (0.7%) patient in the range of 65%–74% and 1 (0.7%) patient less than 50% respectively.
One hundred and sixteen patients were not subjected to prophylaxis for pulmonary aspiration. Fifteen (9.8%) patients were given cimetidine, 10 (6.5%) dexamethohasone, 6 (3.9%) metoclorpromide, 5 (3.3%) cimetidine and dexamethasone, and 1 (0.7%) was given cimetidine and metoclorpromide respectively. Of these patients, 34 (22.2%) were given prophylaxis drugs before 30 minutes and 3 (1.9%) patients within 30 minutes before induction of anesthesia respectively.
Appropriate drugs for RSII, equipments for RSII, equipments for dif fi cult intubation, suction machine with catheters, monitorings and oxygen backup such as ambu bag were not prepared for 41 (26.8%), 50 (32.7%), 51 (33.3%), 38 (24.8%) and 25 (16.3%) patients respectively (Table 2).
The techniques of rapid sequence induction and intubation
Patients were monitored with 3 lead ECG, pulseoximeter and NIBP during operation. Monitorings were used before induction of anesthesia in 129 (77.2%) patients, and after induction of anesthesia in 26 (15.6%) and 12 (7.2%) patients who were operated on without monitoring.
All patients were preoxygenated with 100% oxygen for 3–5 minutes before induction of anesthesia. One hundered and two (66.7%) patients were anesthetized with ketamine, 16 (10.5%) with propofol, 3 (1.9%) with ketamine and halothane, 1 (0.6%) with ketamine and thiopentone, 1 (0.6%) with thiopentone and halothane, and 3 (1.9%) with thiopentone respectively. All patients were paralyzed with suxamethonium. In all the patients, 140 (91.5%), 10 (6.5%) and 3 (2.0%) patients were intubated with the first, second and third laryngoscopy attempts respectively. Analgesic drugs were used asfollows: fentanyl in 88 (57%) patients, tramadol in 17 (11.5%), pethidine in 3 (1.9%), fentanyl and tramadol in 13 (8.5%), diclofenac and fentanyl in 8 (5.2%) and pethidine and fentanyl in 2 (1.3%) during the operation.

Table 2. Preoperative patient status and preparation for rapid sequence induction and intubation (n=153)
Suction machine with a catheter before induction of anesthesia was used in 118 (77.1%) patients and after induction in 18 (11.8%); but it was not used in 17 (11.1%) patients. The patients were ventilated by anesthetists after induction of anesthesia, but 53 (34.6%) of the patients were ventilated before intubation and endotracheal tube cuff in fl ation (Table 3).
The experiences of anesthetists markedly affected their techniques about RSII. Suction machine which was not connected with a catheter and was not turned on before induction of anesthesia in 7 (4.6%), 5 (3.3%), 3 (1.9%) and 2 (1.3%) patients by the anesthetists with services of <1 year, 1–2 years, 3–5 years and > 5 years respectively. Cricoid pressure was not used in7 (4.6%), 5 (3.3%), 3 (1.9%) and 2 (1.3%) patients by the anesthetists with services of <1 year, 1–2 years, 3–5 years and >5 years respectively.
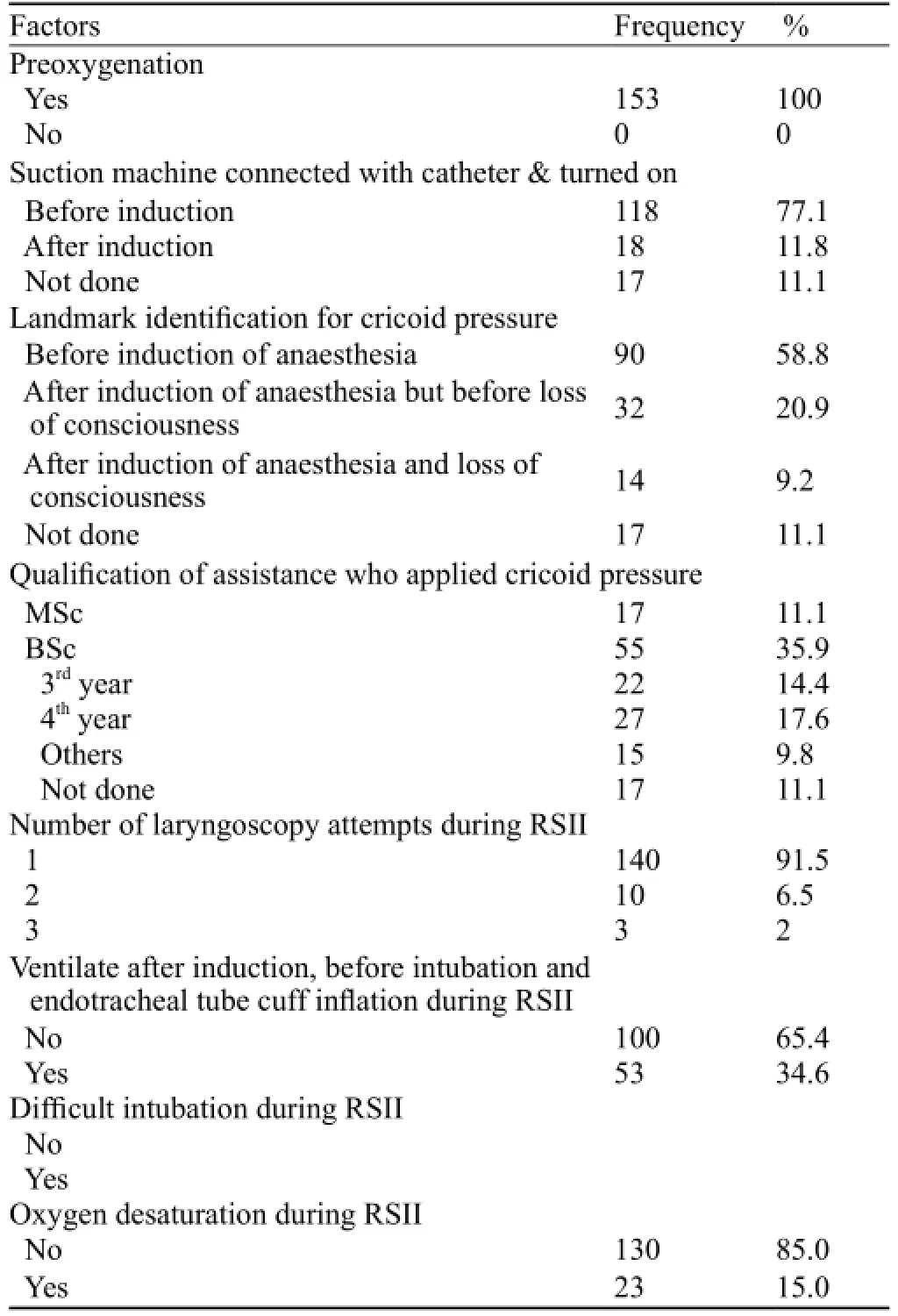
Table 3. Techniques of rapid sequence induction and intubation (n=153)
The incidence of oxygen desaturation during RSII and other immediate complications
A total of 55 (35.9%) patients were desaturated during RSII (SPO2<95%). The minimum, maximum and mean oxygen desaturations were 26%, 94% and 70.9% respectively.
The range of oxygen desaturation was <50%, 50%–64%, 65%–74%, 75%–84%, 85%–89% and 90%–94% in 6 (3.9%), 7 (4.6%), 5 (3.3%), 10 (6.5%), 13 (8.5%) and 14 (9.2%) patients respectively. The minimum, maximum and mean oxygen desaturation periods during RSII were 1, 10 and 4.27 minutes respectively. Of the 55 patients, 6 had difficult airway. Only 18 of the 55 patients were ventilated with a facemask during desaturation till they recovered from hypoxia before intubation, and the rest 37patients were ventilated after intubation. The urgency of operation, type of operation, quali fi cations of anesthetists, and years of services of anesthetists markedly affected the occurrence of oxygen desaturation during RSII (Table 4).

Table 4. Effect of different factors on the occurrence of oxygen desaturation during RSII (n=153)
Difficult airway also occurred during RSII in 23 (15%) patients. Difficult laryngoscopy was oberved in 13 (8.5%) patients and difficult mask ventilation in 10 (6.5%) patients. The occurrence of dif fi cult airway during RSII was also markedly affected by the urgency of operation, qualification and experiences of anesthetists. Of the 23 patients with dif fi cult airway, 21 (13.7%) were emergency patients and 2 (1.3%) were elective patients. Sixteen of the 23 (10.5%) patients with difficult airway were seen in the patients handled by BSc anesthetists whereas 7 (4.6%) in those handled by MSc anesthetists. Of the 23 patients with difficult airway, 15 (9.8%), 3 (1.9%), 2 (1.3%) and 3 (1.9%) were encountered by the anesthetists with services of <1 year, 1–2 years, 3–5 years and > 5 years respectively.
Of the 23 patients with difficult airway, 4 (2.6%), 6 (3.9%), and 13 (8.5%) patients were intubated using pillow, stylet and bougie respectively. Other immediate complications occurred during RSII were hypertension in 20 (13.1%) patients, hypotension in 23(15%), tachycardia in 50 (32.7%) and bradycardia in 8 (5.2%). No perioperative death occurred.
DISCUSSION
In the present study, the incidence of oxygen desaturation during rapid sequence induction and intubation was high (55, 35.9%). This fi nding was similar to a study conducted in Switzerland where oxygen desaturation was 34%.[9]This might be due to inadequate preoxygenation and lack of updating training about the techniques of RSII.
In this study, 116 patients were not given prophylaxis for pulmonary aspiration, appropriate drugs for RSII, equipments for RSII, and equipments for difficult intubation. Suction machine with a catheter, a monitor and an oxygen backup such as ambu bag was not prepared for 41 (26.8%), 50 (32.7%), 51 (33.3%), 38 (24.8%) and 25 (16.3%) patients respectively. These rates were lower than those reported in a study from North Carolina.[18]The difference could be due to the difference in the techniques of RSII used by anesthetists.
Moreover, anesthetists identified the anatomic landmark for cricoid pressure before and after induction of anesthesia but before loss of consciousness, or both after induction of anesthesia and loss of consciousness in 90 (58.8%), 32 (20.9%), and 14 (9.2%) patients respectively. Cricoid pressure was not applied in 17 (11.1%) patients, which was lower than that reported elsewhere.[18]This discrepancy could be due to the difference in the training of anesthetists about the techniques of RSII.
In the present study, anesthetists ventilated the patients after induction of anesthesia but before intubation. Endotracheal tube cuff inflation was done in 53 (34.6%) patients, without connecting a suction machine with a catheter. The suction machine was turned on in 17 (11.1%) patients during RSII. This fi nding was similar to that reported in a study conducted in Boston where the patients were ventilated after induction of anesthesia but before (41%) and after administration of muscle relaxant (35%).[19]The result might be due to the nature of study design (modified rapid sequence induction) and the different techniques of RSII used in different countries.
In this study, most patients (102, 66.7%) were anesthestized with ketamine and were paralyzed with suxamethonium. This rate was higher than that reported in a survey conducted in UK (ketamine use, 8%).[20]This could be due to optimization of preoperative patients and ketamine use in our hospital, which attributed to its sympathomimetic effects. In conclusion, the incidence of oxygen desaturation during RSII was high in our hospital. Optimization of preoperative patients and training of anesthestists in using the techniques of rapid sequence induction and intubation should be emphasized.
Funding:None.
Ethical approval:This study was approved by the Ethical Committee of School of Medicine, Gondar College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia.
Conflicts of interest:The authors do not have any conflict of interest.
Contributors:Endale Gebreegziabher conceived the study. All authors involved in proposal development, data collection, data analysis, paper writing and manuscript preparation. We authors approved the fi nal manuscript and agreed to publish in WJEM.
REFERENCES
1 Dufour DG, Larose DL, Clement SC. Rapid sequence intubation in the emergency department. J Emerg Med 1995; 13: 705–710.
2 Koziol CA, Cuddeford JD, Moos DD. Assessing the force generated with application of cricoid pressure. AORN J 2000; 72: 1018–1028, 1030.
3 Dunford JV, Davis DP, Ochs M, Doney M, Hoyt DB. Incidence of transient hypoxia and pulse rate reactivity during paramedic rapid sequence intubation. Ann Emerg Med 2003; 42: 721–728.
4 Farmery AD, Roe PG. A model to describe the rate of oxyhaemoglobin desaturation during apnoea. Br J Anaesth 1996; 76: 284–291.
5 Davis DP, Hwang JQ, Dunford JV. Rate of decline in oxygensaturation at various pulse oximetry values with prehospital rapid sequence intubation. Prehosp Emerg Care 2008; 2: 46–51.
6 Marsch CS, Steiner L, Bucher E, Pargger H, Schumann M, Aebi T, et al. Succinylcholine versus rocuronium for rapid sequence intubation in intensive care a prospective randomized controlled trial. Critical Care 2011; 15: 199.
7 Rofperry JJ, Sillberg VA, Well A. Rocuronium vs. succinylcholine for RSII. Coohrane Data Base Syst Reu 2008; 278.
8 El-Orbany M, Connolly LA. Rapid sequence induction and intubation current controversy. Anesth Analg 2010; 110: 1318–1325.
9 Heier T, Feiner JR, Lin J, Brown R, Caldwell JE. Hemoglobin desaturation after succinylcholine-induced apnea. Anesthesiology 2001; 94: 754–759.
10 Neguib M, Samarkandi AH, Abdullah K, Riad W, Alharby SW. Succinylcholine dosage and apnea-induced haemoglobin desaturation in patients. Anesthesiology 2005; 102: 35–40.
11 Lane S, Saunders D, Scho fi eld A, Padmanabhan R, Hildreth A, Laws D. A prospective, randomised controlled trial comparing the efficacy of preoxygenation in the 20 degrees head-up vs supine position. Anaesthesia 2005; 60: 1064–1067.
12 Laurel O, Woodrow Y, Stan M, Jack P. Role of the emergency medicine physician in airway management of the trauma patient. J Trauma 2001; 51: 1065–1068.
13 Tang L, Li S, Huang S, Ma H, Wang Z. Desaturation following rapid sequence induction using succinylcholine vs. rocuroniumin overweight patients. Acta Anaesthesiol Scand 2011; 55: 203–208.
14 Mort CT. The incidence and risk factors for cardiac arrest during emergency tracheal intubation and justi fi cation for incorporating the ASA guidelines in the remote location. J Clin Anesth 2004; 16: 508–516.
15 Herriger A, Frascarolo P, Spahn DR, Magnusson L. The effect of positive airway pressure during pre-oxygenation and induction of anaesthesia upon duration of non hypoxic apnoea. Anaesthesia 2004; 59: 243–247.
16 Gander S, Frascarolo P, Suter M, Spahn DR, Magnusson L. Positive end-expiratory pressure during induction of general anesthesia increases duration of nonhypoxic apnea in morbidly obese patients. Anesth Analg 2005; 100: 580–584.
17 Benumof JL, Dagg R, Benumof R. Critical hemoglobin desaturation will occur before return to an unparalyzed state following 1 mg/kg intravenous succinylcholine. Anesthesiology 1997; 87: 979–982.
18 Schelesinger S, Blanchfield D. Modified rapid-sequence induction of anesthesia: a survey of current clinical practice. AANA J 2001; 69: 291–298.
19 Ehrenfeld JM, Cassedy EA, Forbes VE, Mercaldo ND, Sandberg WS. Modi fi ed rapid sequence induction and intubation: a survey of United States current practice. Anesth Analg 2012; 115: 95–101.
20 Morris J, Cook TM. Rapid sequence induction: a national survey of practice. Anaesthesia 2001; 56: 1090–1097.
21 Using the WHO pulseoximeter. Tutorial 1: The basics 2010, WHO.
Received May 25, 2014
Accepted after revision October 9, 2014
World J Emerg Med 2014;5(4):279–285
10.5847/wjem.j.issn.1920–8642.2014.04.007
杂志排行
World journal of emergency medicine的其它文章
- Current pre-hospital traumatic brain injury management in China
- Emergency bedside ultrasound for the diagnosis of pediatric intussusception: a retrospective review
- How to secure the connection between thoracostomy tube and drainage system?
- Clinical probability and risk analysis of patients with suspected pulmonary embolism
- Thyroid hormone alterations in trauma patients requiring massive transfusion: An observational study
- A single subcutaneous dose of tramadol for mild to moderate musculoskeletal trauma in the emergency department
