Liquorrhoea associated with intrapelvic meningocele resection successfully treated by conservative therapy: a case report
2013-12-23XijuXie荭XiodongYng荭HoXuFengWngYoufngHuDeprtmentofGenerlSurgerytheFirstAffilitedHospitlNnjingMediclUniversityNnjingJingsu210029ChinDeprtmentofChildrenHelththeFirstAffilitedHospitlNnjingMediclUniversityNnjingJingsu21002
Xiju Xie荭, Xiodong Yng荭, Ho Xu Feng Wng , Youfng Hu,Deprtment of Generl Surgery, the First Affilited Hospitl, Nnjing Medicl University, Nnjing, Jingsu 210029, Chin;Deprtment of Children's Helth, the First Affilited Hospitl, Nnjing Medicl University, Nnjing, Jingsu 210029, Chin.
INTRODUCTION
Spinal meningocele is associated with spina bifida cysts and may occur at any age[1]. However, intrapelvic meningocele is rare and, without spinal compression, this type of meningocele does not cause any discomfort. For this reason, intrapelvic meningocele has not attracted much attention for a long time. Here, we report a case of an asymptomatic intrapelvic meningocele found incidentally during a sigmoidectomy due to megacolon in a 30-year old male patient.
CASE REPORT
A 30-year-old male, admitted because of constipation, was scheduled to undergo sigmoidectomy. Preoperative magnetic resonance (MR) scan indicated that a cyst was in front of the third sacral vertebrae (S3) (Fig. 1A and 1B). After sigmoidectomy, this cyst was resected. However, on the first postoperative day, 150 mL of amber liquid was drained from pelvic drainage tube. Over the following several days, the volume of this amber liquid had not reduced, but increased. Liquorrhoea was considered and Pandy test showed a negative result. Histological examination of the resected cyst confirmed the diagnosis of liquorrhoea (Fig. 1C and 1D). Because the patient had just undergone sigmoidectomy, conservative treatment consisting of three main steps was considered: drainage, anti-infection therapy (cefpiramide combined with tinidazole) and posturing by raising the position of the 荭These authors contributed equally to this work.
The authors reported no conflict of interests.
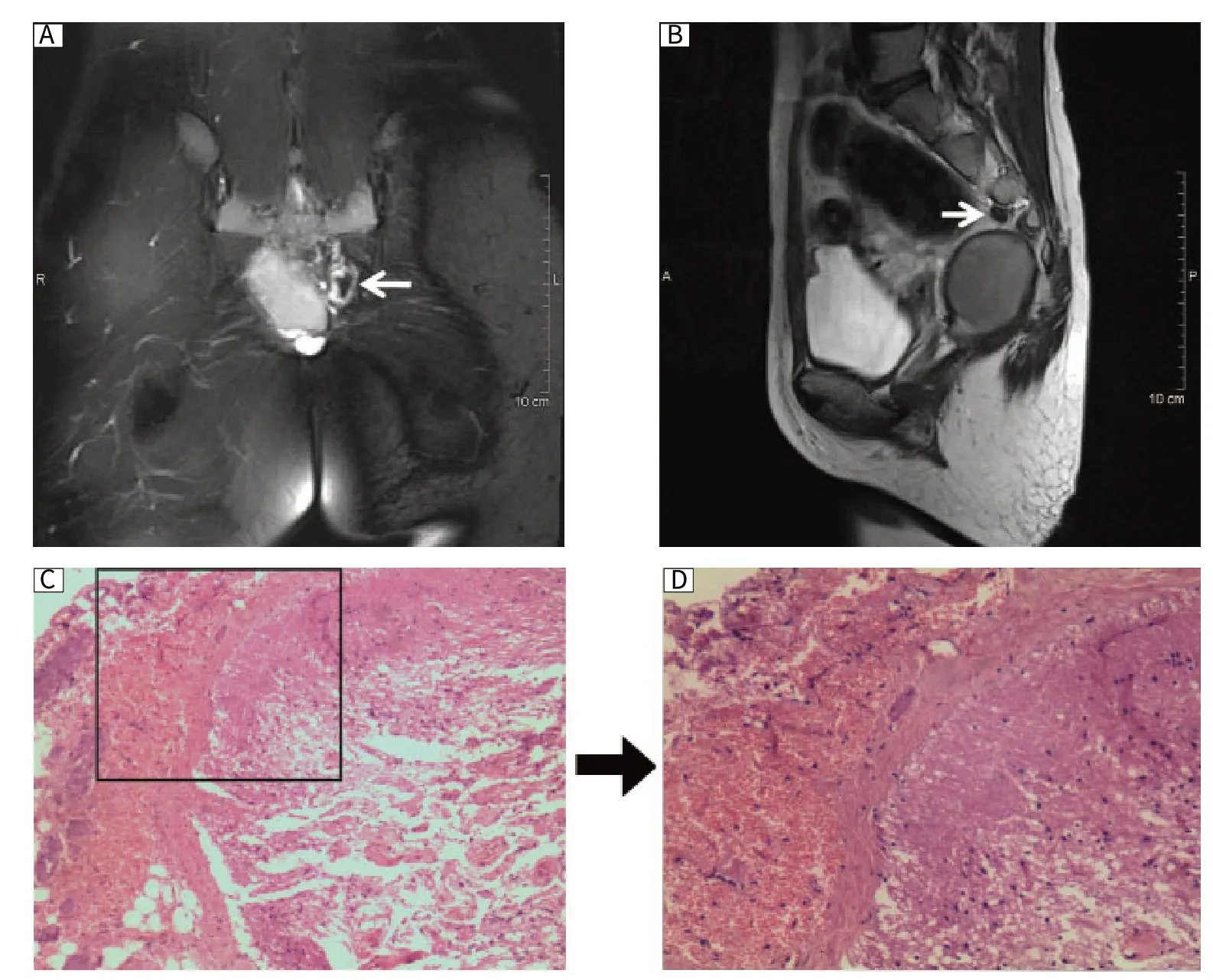
Fig. 1 Liquorrhoea associated with intrapelvic meningocele resection. MR scan reveals the presence of a cyst 3 cm in diameter (arrow) in front of S3 in a 30-year-old male patient (A: coronal section; B: median sagittal section). Histological examination (C: ×40; D: ×100) showed that the cyst was mixed with nerve collagen tissue (H&E).
DISCUSSION
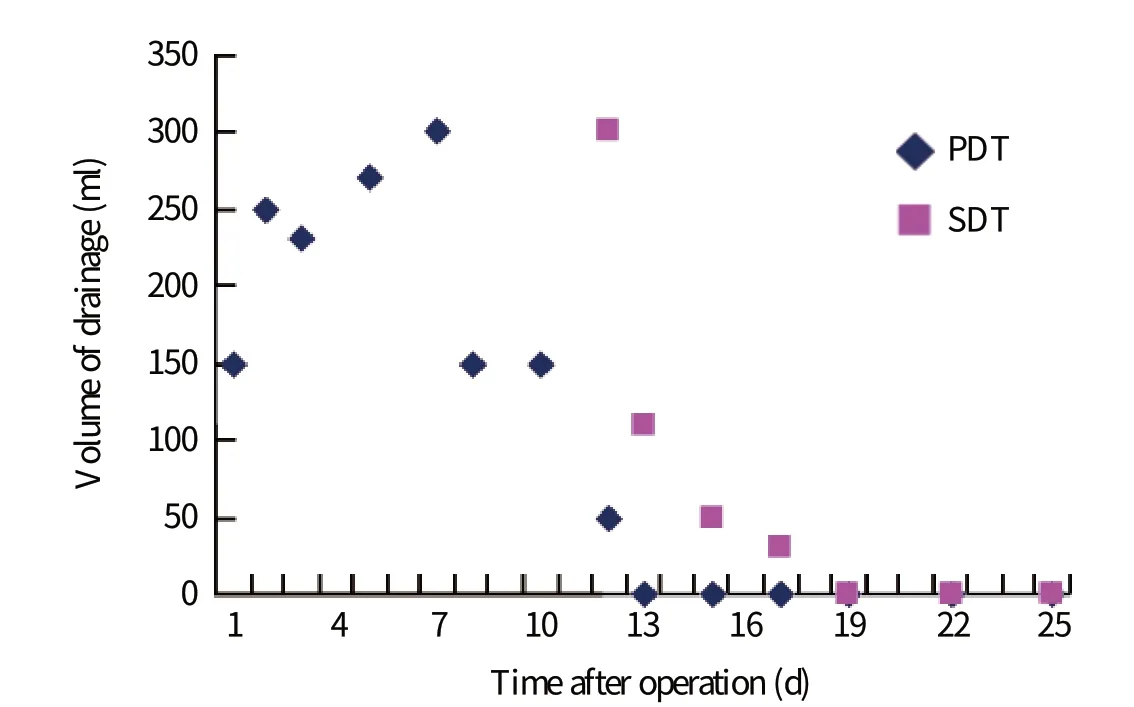
Fig. 2 The drainage volume after operation. PDT: pelvic drainage tube; SDT: subarachnoid drainage tube.
Intrapelvic meningocele is defined as a CSF-filled sac within the spinal meningeal wall which protrudes into the intrapelvic cavity through an enlarged intervertebral foramen or bone defect. Acquired meningocele is relatively common as a laminectomy complication, while congenital meningocele is commonly associated with neurofibromatosis[2,3]. Isolated intrapelvic meningoceles without neurofibromatosis are uncommon. The clinical manifestation of an intrapelvic meningocele is closely related to its size and relationship with surrounding structures. It may include back pain, urinary and fecal incontinence, and lower limbs weakness or paralysis. A small lesion may be asymptomatic and discovered incidentally, as it was in our case. For small- and medium-sized lesions, the most common surgical management is resection of the meningocele and repair of the dural defect through laminectomy[4,5]. In this case, surgery was performed with removal of the meningocele pouches and shunting of the cyst to the subarachnoid region. However, liquorrhoea occurred after the op-eration. Although liquorrhoea is a common occur-ance with cystectomy, it may result in infection of the central nervous system.
The most important consideration in treating liquorrhoea is preventing infection. Incontrovertibly, surgery is an effective way to treat liquorrhoea. In this case, specific posture and drainage in combination with anti-infection therapy were performed instead of surgery. This conservative method can also treat liquorrhoea effectively and at the same time help patients avoid a second operation.
[1] Bassiouni H, Hunold A, Asgari S, Hubschen U, Konig HJ, Stolke D. Spinal intradural juxtamedullary cysts in the adult: surgical management and outcome. Neurosurgery 2004; 55: 1352-9; discussion 9-60.
[2] de Andrade GC, Braga OP, Hisatugo MK, de Paiva Neto MA, Succi E, Braga FM. Giant intrathoracic meningoceles associated with cutaneous neurofibromatosis type I: case report. Arq Neuropsiquiatr 2003; 61: 677-81.
[3] Ebara S, Yuzawa Y, Kinoshita T, Takahashi J, Nakamura I, Hirabayashi H, et al. A neurofibromatosis type 1 patient with severe kyphoscoliosis and intrathoracic meningocele. J Clin Neurosci 2003; 10: 268-72.
[4] Chee CP. Lateral thoracic meningocele associated with neurofibromatosis: total excision by posterolateral extradural approach. A case report. Spine (Phila Pa 1976) 1989; 14: 129-31.
[5] Zamponi C, Cervoni L, Caruso R. Large intrathoracic meningocele in a patient with neurofibromatosis: technical report. Neurosurg Rev 1996; 19: 275-7.
杂志排行
THE JOURNAL OF BIOMEDICAL RESEARCH的其它文章
- Prognostic assessment of apoptotic gene polymorphisms in nonsmall cell lung cancer in Chinese
- Expression of cytochrome P450 2A13 in human non-small cell lung cancer and its clinical significance
- Genetic variants in pseudogene E2F3P1 confer risk for HBV-related hepatocellular carcinoma in a Chinese population
