Clinical Observation on Acupuncture Plus Acupoint Sticking for Bronchial Asthma in Remissive State
2013-07-18XuSiweiZhangBimengZhouJunmeiHuZhihaiPanChaoanWangYiShouYinYangYangLiuMiaomiao
Xu Si-wei, Zhang Bi-meng, Zhou Jun-mei, Hu Zhi-hai, Pan Chao-an, Wang Yi, Shou Yin, Yang Yang, Liu Miao-miao
1 Shanghai University of Traditional Chinese Medicine, Shanghai 201203, China
2 The First People’s Hospital Affiliated to Shanghai Jiaotong University, Shanghai 200080, China
3 Shanghai Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai 200082, China
4 Ledu Hospital of Songjiang District, Shanghai 201600, China
Clinical Observation on Acupuncture Plus Acupoint Sticking for Bronchial Asthma in Remissive State
Xu Si-wei1,2, Zhang Bi-meng2, Zhou Jun-mei2, Hu Zhi-hai3, Pan Chao-an4, Wang Yi3, Shou Yin2, Yang Yang2, Liu Miao-miao2
1 Shanghai University of Traditional Chinese Medicine, Shanghai 201203, China
2 The First People’s Hospital Affiliated to Shanghai Jiaotong University, Shanghai 200080, China
3 Shanghai Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai 200082, China
4 Ledu Hospital of Songjiang District, Shanghai 201600, China
Objective: To observe the clinical efficacy of acupuncture plus acupoint sticking for bronchial asthma in remissive state.
Methods: A total of 210 cases with asthma at remissive state were randomly allocated into an acupuncture group of 100 cases and a comprehensive therapy group of 110 cases. Cases in the acupuncture group were treated with acupuncture alone, and cases in the comprehensive therapy group were treated with acupuncture plus acupoint sticking therapy. Then the therapeutic efficacies were compared using observation indexes including wheezing, cough and coughing up phlegm, peak expiratory flow (PEF) and forced expiratory volume in one second (FEV1). In addition, the overall therapeutic efficacies were also analyzed on different traditional Chinese medicine (TCM) patterns.
Results: The comprehensive therapy obtained better effects than acupuncture alone in alleviating cough and coughing up phlegm and improving PEF and FEV1; the overall efficacies on asthma due to lung-qi deficiency and spleen-qi deficiency were better than those on asthma due to kidney-qi deficiency.
Conclusion: Acupuncture plus acupoint sticking is a convenient and effective therapy for asthma at remissive state and therefore worthy of being popularized.
Acupuncture Therapy; Acupuncture Medication Combined; Acupoint Therapy; Acupoint Sticking Therapy; Asthma
Bronchial asthma is a common chronic pulmonary condition that endangers public health and attacks all age groups. It is characterized by recurrent attacks of wheezing, shortness of breath, chest tightness and coughing. Symptoms are usually worse at night and in the early morning. Some people may have marked and persistent symptoms or even developed into status asthmaticus. This condition can greatly impair the patients’ quality of life and cause severe social and economic burden. Over the recent years, the incidence of asthma has been raised, especially in children. However, asthma cannot be well managed by Western medicine. Based on the theory of‘treating problems before onset’, ‘man-nature harmony’ and ‘nourishing yang in spring and summer’, this study employed acupuncture plus acupoint sticking in the hottest summer days for asthma at remissive state. The report is now summarized as follows.
1 Clinical Materials
1.1 Diagnostic criteria
This was made according to the diagnostic criteria for asthma in remissivestate revised in theGuidelines for Asthma Prevention and Management[1]by Chinese Society of Respiratory Disease Asthma Study Group.
This includes recurrent episodes of wheezing, shortness of breath, chest tightness and coughing that are often triggered by exposure to allergens or cold air, viral infection of the upper respiratory tract and physical exercise; audible scattered or diffuse expiratory wheezes and prolonged expiratory phase; above signs and symptoms can spontaneously alleviate or be alleviated in response to treatment; atypical bronchial asthma (no wheezing) needs to be confirmed with at least one of the following three items: positive results of bronchial provocation test or exercise challenge test; a positive result of bronchial relaxation test, forced expiratory volume in one second (FEV1) ≥12%, and the absolute value of FEV1increase >200 mL; the daily aberration rate of peak expiratory flow (PEF) ≥20%; excluding wheezing, shortness of breath, chest tightness and coughing occurred in other medical conditions.
Staging criteria: By clinical manifestations, bronchial asthma can be classified into three states, namely acute asthmatic episodes, chronic persistent state and clinical remissive state. All cases included in this study were in remissive state.
Definition of clinical remissive state: Almost no signs and symptoms with or without treatment, basic recovery of the pulmonary function maintaining for at least 3 months.
1.2 Traditional Chinese medicine (TCM) patterns[2]
According to the pattern identification of ‘wheezing syndrome’ in theShanghai Diagnostic and Therapeutic Guidelines of Traditional Chinese Medicine, this condition can be classified into three patterns: lung-qi deficiency, spleen-qi deficiency and kidney-qi deficiency.
1.2.1 Lung-qi deficiency
Patients may present with spontaneous sweating, intolerance of wind, frequent common colds, asthmatic episodes triggered by weather changes, frequent sneezing before onset, stuffy or runny nose, a thin white tongue coating and a soft pulse.
1.2.2 Spleen-qi deficiency
Patients may present with excessive phlegm, lassitude, poor appetite, loose stools, asthmatic episodes triggered by improper diet, a thin white tongue coating and a thready moderate pulse.
1.2.3 Kidney-qi deficiency
Patients may present with shortness of breath, especially upon physical exertion, soreness and weakness of the low back and knee joints, dizziness, tinnitus, fatigue, cold (lower) limbs, clear profuse urine, a pale tongue and a deep thready pulse.
1.3 Inclusion criteria
Those with asthma in remissive state and met the above diagnostic criteria for bronchial asthma and TCM wheezing syndrome; men or women aged between 10 and 60 years; having discontinued other therapies during the study; willing to participate in the trial and signed the informed consent.
1.4 Exclusion criteria
Those during acute asthmatic episodes or severe persistent non-acute bronchial asthma; having complications of wheezing and difficult breathing coupled with other medical conditions [such as tuberculosis (TB), bronchiectasis and tumor]; having chronic pulmonary heart disease; women during pregnancy or lactation; reluctant to participate in the study, dropped out or lost follow-up; having persistent deterioration or severe complications during the clinical trial.
1.5 General data
The 210 cases included in the study were all treated in acupuncture departments of the First People’s Hospital Affiliated to Shanghai Jiaotong University or Shanghai Hospital of Integrated Traditional Chinese and Western Medicine between July 2010 and October 2012. These cases were randomly allocated into an acupuncture group of 100 cases and a comprehensive therapy group of 110 cases. There were no betweengroup statistical differences in general data, indicating that the two groups were comparable (table 1).
During the study, 1 case in the acupuncture group dropped out and 2 cases lost follow-up; 2 cases in the comprehensive therapy group dropped out and 2 cases lost follow-up. Clinical procedure flow chart in the two groups is shown in Fig.1.
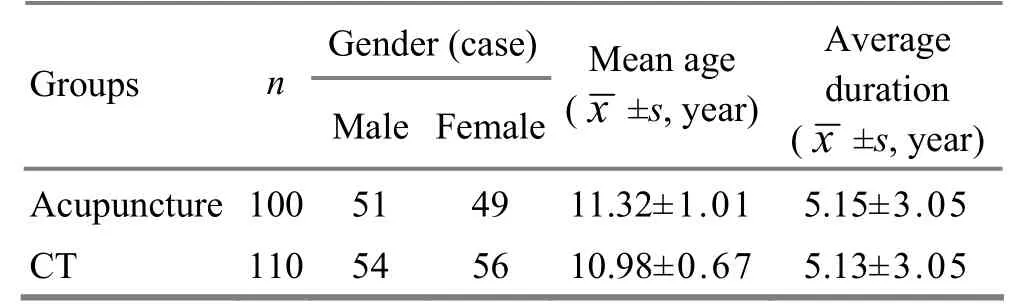
Table 1. Between-group comparison in general data
2 Treatment Methods
2.1 Acupuncture group
Acupoints: Dingchuan (EX-B 1) and bilateral Feishu (BL 13), Zusanli (ST 36) and Fenglong (ST 40).
Method: After disinfection, puncture the above acupoints by 0.5-1.2 cun perpendicularly. A better effect can be achieved with local soreness and distension in Feishu (BL 13) and Dingchuan (EX-B 1),along with an electric shock sensation in Zusanli (ST 36) and Fenglong (ST 40) radiating towards the dorsum of the feet. The needles were retained for 20 min. All patients were treated once every other day during the hottest summer days, 5 times constituted a course of treatment. There was a 2-day interval between two courses. The therapeutic efficacy was observed after three courses of treatment.
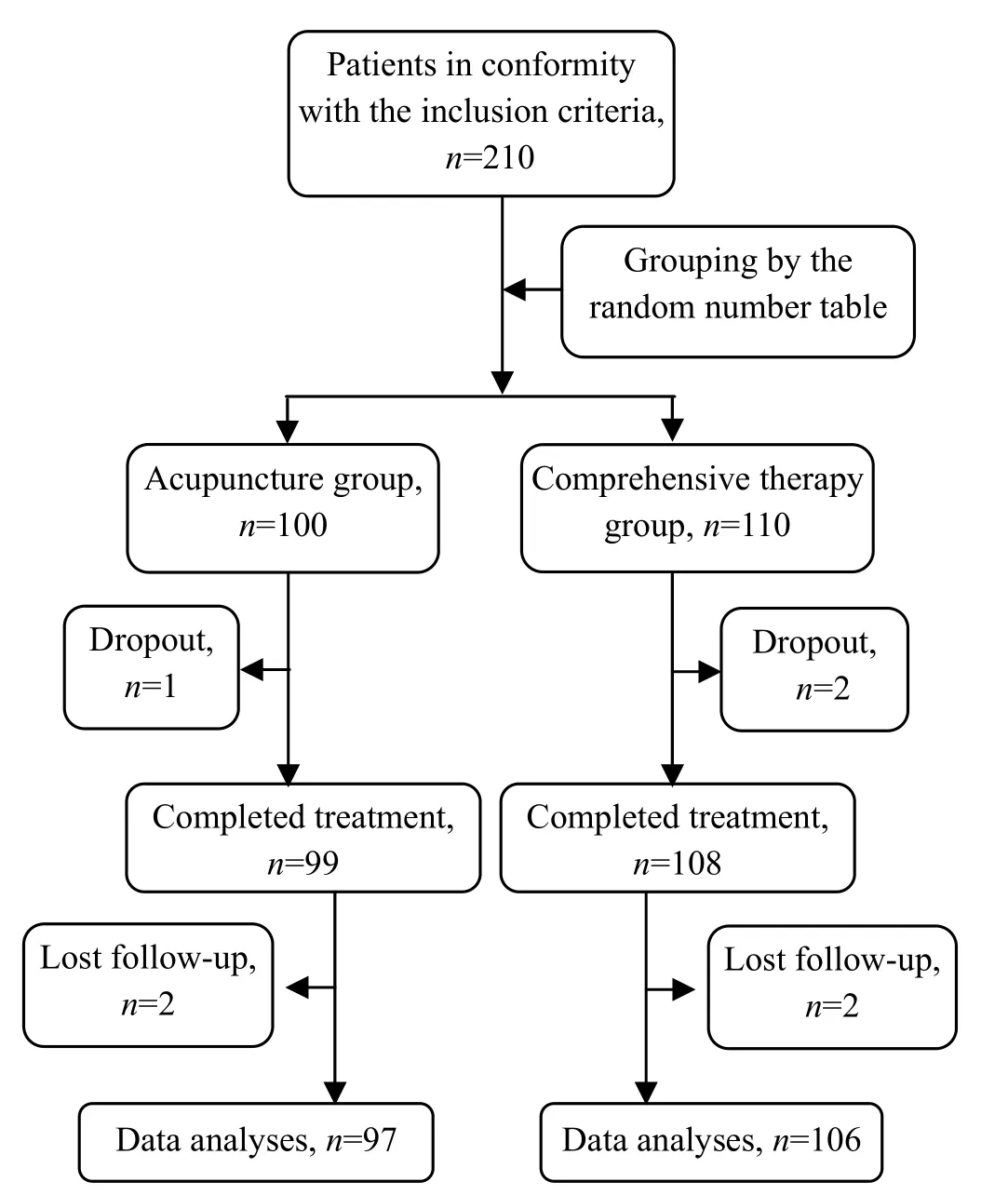
Fig.1 Procedure of clinical management
2.2 Comprehensive therapy group
In addition to same acupuncture therapy as the acupuncture group, patients in this group received acupoint sticking therapy.
Ingredients:Rou Gui(Cortex Cinnamomi),Ma Huang(Herba Ephedrae),Gan Sui(Radix Kansui),Ding Xiang(Flos Caryophylli),Xi Xin(Radix et Rhizoma Asari),Yan Hu Suo(Rhizoma Corydalis) andBai Jie Zi(Semen Sinapis).
Acupoints: Dingchuan (EX-B1), Dazhui (GV 14), Tiantu (CV 22) and bilateral Feishu (BL 13).
Time of acupoint sticking: The first three days of the three hottest summer periods respectively, i.e., first acupoint sticking within the first three days of the first hottest period, the second acupoint sticking within the first three days of the second hottest period and the third acupoint sticking within the first three days of the third hottest period, a total of three times (Note: In 2010, the three hottest periods were July 19, July 29 and August 8 respectively; in 2011, the three hottest periods were July 14, July 24 and August 13 respectively; and in 2012, the three hottest periods were July 18, July 28 and August 7 respectively).
Method: Made above medicinal powder into herbal cakes, mixed with fresh ginger juice, applied to aforementioned points and covered by paper adhesive tapes. The application lasted no more than 4 h for adults and no more than 2 h for children. The patients should have a tolerable burning sensation in the localized area. The therapeutic efficacy was observed after three times of treatment.
3 Therapeutic Efficacy Observation
3.1 Observation indexes and therapeutic efficacy criteria
Pulmonary function markers PEF and FEV1were determined before and after treatment.
A comprehensive evaluation was made according to the criteria of therapeutic efficacy for wheezing syndrome in theGuiding Principles for Clinical Study of New Chinese Medicines[3], coupled with scoring of signs and symptoms.
Efficacy index = (Total scores of pre-treatment symptoms – Total scores of post-treatment scores) ÷ Total scores of pre-treatment symptoms × 100%.
Recovery: Absence or almost absence of clinical signs and symptoms, the efficacy index ≥90%.
Marked effect: Substantial improvement of clinical signs and symptoms, the efficacy index≥70% but<90%.
Improvement: Alleviation of clinical signs and symptoms, the efficacy index ≥30% but <70%.
Failure: Clinical signs and symptoms remained unchanged or became worse, the efficacy index <30%.
3.2 Statistical management
The SPSS 16.0 version software was used for all data analysis,Riditanalysis for ranked data, one-factor analysis of variance for measurement data, andP<0.05 indicates a statistical significance.
3.3 Study results
3.3.1 Clinical efficacy analysis
After three courses of treatment, the total effective rate in the comprehensive therapy group was 83.0%, versus 67.0% in the acupuncture group, showing a statistical difference (P<0.05) and indicating a better effect in the comprehensive therapy group (table 2).
3.3.2 Improvement analysis of major symptoms
The major symptoms (wheezing, cough and coughing up phlegm) in the two groups were scored before and after treatment. Before treatment, there was no between-group significant difference in symptom scoring (P>0.05). After treatment, scores of major symptoms in both groups were significantly reduced(P<0.05), indicating that both treatment protocols could alleviate major symptoms. After treatment, there were between-group significant difference in scores of cough and coughing up phlegm (bothP<0.05), indicating a better effect in the comprehensive therapy group than that in the acupuncture group (table 3).
3.3.3 Improvement analysis of pulmonary function
Before treatment, there were no between-group significant differences in FEV1and PEF (P>0.05). After treatment, the FEV1and PEF in both groups were significantly increased (P<0.05), indicating that both treatment protocols could improve the patients’pulmonary functions. After treatment, there were between-group significant differences in FEV1and PEF (P<0.05), indicating a better effect in the comprehensive therapy group than that in the acupuncture group (table 4).
3.3.4 Therapeutic efficacies on TCM patterns
Therapeutic efficacy analysis has shown the best effect for spleen-qi deficiency, second for lung-qi deficiency and poorest for kidney-qi deficiency. There were between-group statistical differences in total effective rates of same patterns (P<0.05), indicating that acupuncture plus acupoint sticking worked better than acupuncture alone for all three patterns (table 5).
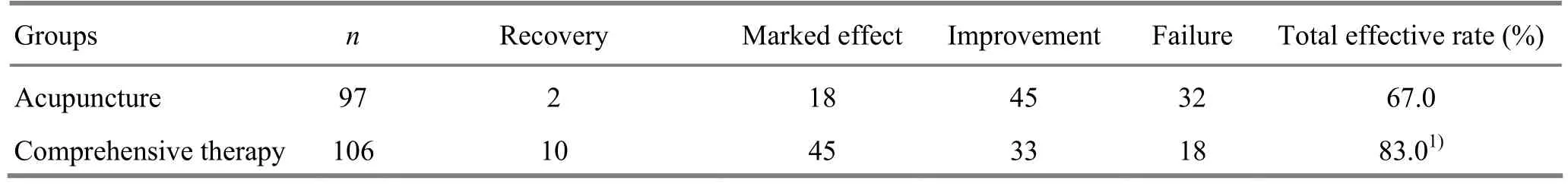
Table 2. Between-group comparison of clinical efficacies (case)
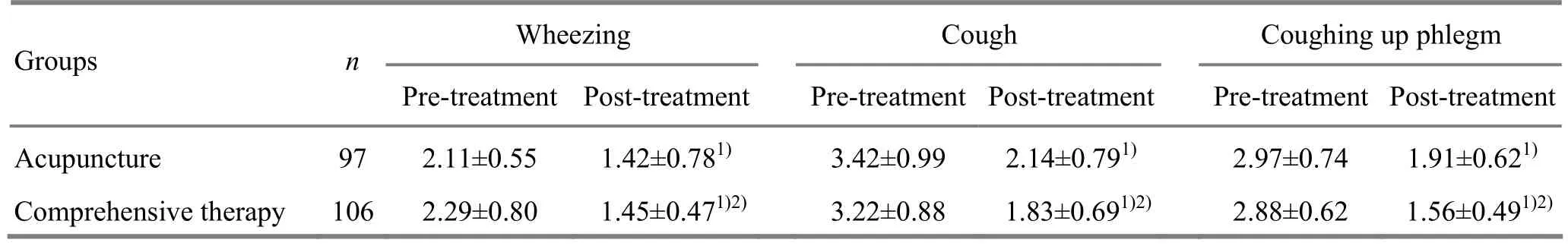
Table 3. Therapeutic efficacy analysis of different patterns in acupuncture group (case)
Table 4. Between-group comparison in pulmonary function improvement before and after treatment ()
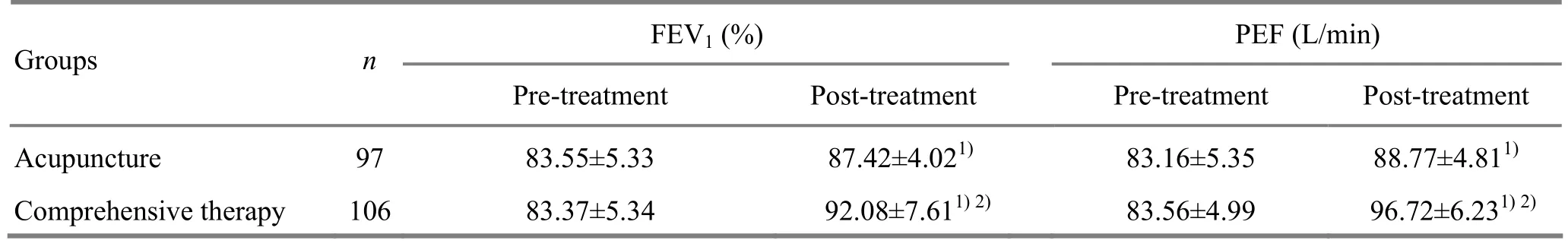
Table 4. Between-group comparison in pulmonary function improvement before and after treatment ()
Note: Compared with intra-group results pre-treatment, 1)P<0.05; compared with the acupuncture group, 2)P<0.05
GroupsnFEV1(%) PEF (L/min) Pre-treatment Post-treatment Pre-treatment Post-treatment Acupuncture 97 83.55±5.33 87.42±4.021)83.16±5.35 88.77±4.811)Comprehensive therapy 106 83.37±5.34 92.08±7.611)2)83.56±4.99 96.72±6.231)2)
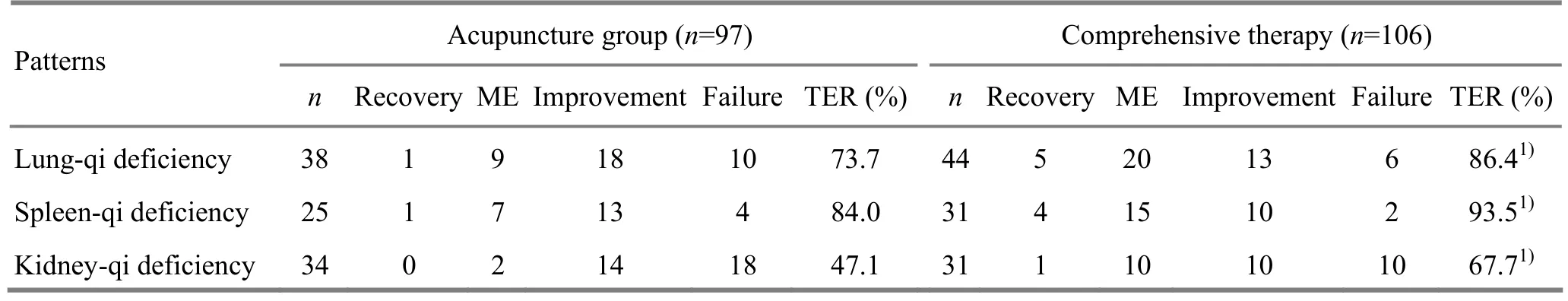
Table 5. Therapeutic efficacy analysis of different patterns in acupuncture group (case)
4 Analysis and Discussion
In Chinese medicine, the onset and progression of bronchial asthma are closely associated with phlegm, stasis[4-7], dysfunctions of the lung, spleen, kidney and liver[8-11], exogenous pathogens, emotional disturbance, improper diet, overexertion or chronic conditions. In remission stage, asthma mainly manifests as deficiency in the root cause, whereas acute asthmatic episodes often manifest excess in symptoms. Over time, repeatedasthma attacks may impair the kidney, spleen and lung, manifesting a combined deficiency and excess syndrome.
The multi-link and multi-target actions of acupuncture aim to treat both the symptoms and root cause of asthma. Needling Feishu (BL 13), Dingchuan (EX-B 1), Zusanli (ST 36) and Fenglong (ST 40) can regulate the spleen and stomach, supplement anti-pathogenic qi, strengthen the spleen, resolve phlegm, harmonize the stomach and regulate lung-qi. Acupoint sticking is an important Chinese external therapy and considered to be quintessence of acupuncture. During the hottest summer days, external flourishing of yang qi, opening of the bodily striae and fast metabolism all contribute to a good transcutaneous herbal absorption. Thanks to the dual effects from point stimulation and herbal absorption, acupoint sticking to Dazhu (GV 14), Feishu (BL 13), Dingchuan (EX-B 1) and Tiantu (CV 22) can warm yang and dissipate cold and therefore obtain satisfactory treatment effects[12-14]. This study has proven that acupuncture could improve the patient’s PEF and FEV1, relieve airway obstruction, improve ventilation function and thus alleviate cough, coughing up phlegm and wheezing, so obtained better effects than acupuncture alone. This study has also suggested that acupuncture works better for bronchial asthma (in remission state) due to lung-qi deficiency and spleen-qi deficiency than that due to kidney-qi deficiency. This might be related to the fact that, in addition to lung deficiency, chronic asthma may affect the kidney and result in kidney-qi deficiency and kidney failing to absorb qi.
The non-invasive pain-free acupoint sticking is easy to be accepted by patients. Combining acupoint sticking and traditional acupuncture can substantially boost the pulmonary function of asthma patients in remission stage, improve the clinical efficacy and is therefore worthy of being popularized in clinical practice.
[1] Chinese Society of Respiratory Disease Asthma Study Group. Guidelines for asthma prevention and management (definition, diagnosis, treatment and management protocol). Zhonghua Jiehe He Huxi Zazhi, 2008, 31(3): 177-185.
[2] Shanghai Municipal Health Bureau. Shanghai Diagnostic and Therapeutic Guidelines of Traditional Chinese Medicine. 2nd Edition. Shanghai: Publishing House of Shanghai University of Traditional Chinese Medicine, 2003: 14.
[3] Ministry of Health of the People’s Republic of China. Guiding Principles for Clinical Study of New Chinese Medicines. Beijing: China Medico-Pharmaceutical Science & Technology Publishing House, 2002: 60-66.
[4] Gao GQ. Clinical study on treating pediatric bronchial asthma with liver-soothing and blood-activating method. Shandong Zhongyiyao Daxue Xuebao, 2006, 30(3): 221-224, 232.
[5] Luo SJ, Fu QP, He GP, Du HH. Exploration on blood stasis and pediatric asthma. Zhongguo Zhongyi Jichu Yixue Zazhi, 2012, 18(2): 142,144.
[6] Wu QF, Lu QR, Zhang YM, Gong HD. Observations on the efficacy of acupoint application in treating bronchial asthma. Shanghai Zhenjiu Zazhi, 2009, 28(11): 626-628.
[7] Zhang AG. Phlegm-stasis and bronchial asthma. Shandong Zhongyi Zazhi, 2002, 21(10): 632-633.
[8] Zhao LQ. Prof. Zhu Zhen-duo’s experience in the treatment of senile asthma. Zhongguo Zhongyiyao, 2005, 3(6):12-13.
[9] Liu X, Dai AG, Zhou JP, Zhou JJ, Zhao Q, Fan TH. Effect of acupuncture on apoptosis of pulmonary eosinophils in asthmatic guinea-pigs. Shanghai Zhenjiu Zazhi, 2003, 22(7): 3-5.
[10] Cui LP, Yang YQ, Chen HP, Zhang YY, Ma SL. Effects of acupuncture on allergic asthma in SD rats. Shanghai Zhenjiu Zazhi, 1999, 18(3): 35-37.
[11] Tong Q, Liang YP, Zheng ZT. Influence of acupoint application therapy on biochemical indexes of asthma patients in remission period. J Acupunct Tuina Sci, 2010, 8(3): 184-188.
[12] Liu YY, Ai Z, Zou T, Zhang QR, Yang L. Comparative study of dog days versus non-dog days moxibustion for treatment of chronic bronchitis. Shanghai Zhenjiu Zazhi, 2013, 32(4): 268-269.
[13] Xu SW. Observations on therapeutic effect of Back-Shu acupoint in treatment of asthma. J Acupunct Tuina Science, 2008, 6(1): 32-35.
[14] Zhu XM. Exploring time factors in treating winter diseases in summer and reckoning the dates of dog days. Shanghai Zhenjiu Zazhi, 2013, 32(3): 224-226.
Translator: Han Chou-ping
R246.1
A
Date: May 18, 2013
Author: Xu Si-wei, associate chief physician
Zhang Bi-meng, M.D., associate chief physician, associate professor, master tutor.
E-mail: pjzhtiger08@aliyun.com
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Therapeutic Efficacy Observation on Combining Acupuncture and Chinese Herbal Fumigation for Cervical Radiculopathy
- Clinical Study on Moxibustion at Shenque (CV 8) for Chronic Urticaria
- Clinical Research Progress of Acupuncture-moxibustion for Chronic Urticaria
- Clinical Observation on Dong’s Extraordinary Points for Tinnitus Due to Cervical Spondylosis
- Therapeutic Efficacy Observation on Point-toward-point Acupuncture Combined with Herbs Iontophoresis for Knee Osteoarthritis
- Observation on Clinical Effect of Superficial Needling for Intractable Humeral Epicondylitis
