Therapeutic Efficacy Observation on Combining Acupuncture and Chinese Herbal Fumigation for Cervical Radiculopathy
2013-07-18JingLeiDengHongyongWangWenliLiYue
Jing Lei, Deng Hong-yong, Wang Wen-li, Li Yue
Dongnan Hospital of Huangpu District, Shanghai 200023, China
Therapeutic Efficacy Observation on Combining Acupuncture and Chinese Herbal Fumigation for Cervical Radiculopathy
Jing Lei, Deng Hong-yong, Wang Wen-li, Li Yue
Dongnan Hospital of Huangpu District, Shanghai 200023, China
Objective: To observe the clinical effect of needling eight neck points and Chinese herbal fumigation for cervical radiculopathy.
Methods: A total of 85 cases who met the inclusion criteria of cervical radiculopathy were allocated into a Jiaji (EX-B 2) points group, an eight neck points group and a comprehensive therapy group according to single-blind randomized controlled trial design. The 27 cases in the Jiaji (EX-B 2) points group were treated with needling cervical Jiaji (EX-B 2) points. The 28 cases in the eight neck points group were treated with needling the eight neck points. The 30 cases in the comprehensive therapy group were treated with needling the eight neck points coupled with Chinese herbal fumigation over the affected area. Before and after treatment, the symptoms of traditional Chinese medicine (TCM) were graded and the short-form McGill pain questionnaire (SF-MQP) was employed to test pain rating index (PRI), visual analogue scale (VAS) and present pain intensity (PPI). In addition, therapeutic efficacies were compared among three groups.
Results: After treatment, all SF-MPQ scores in three groups were significantly reduced, and there were inter-group statistical significant in comparison of scores differences between before and after treatment (P<0.01); there were inter-group statistical differences in the total effective rate (P<0.05).
Conclusion: Needling the cervical Jiaji (EX-B 2) points and eight neck points can both alleviate pain in cervical radiculopathy patient. However, combining needling the eight neck points and Chinese herbal fumigation can obtain the better effect.
Acupuncture Therapy; Acupuncture Medication Combined; Spondylosis; Neck Pain
Cervical radiculopathy is caused by chronic degenerative changes of the cervical spine, such as bone spurs on the cervical vertebrae, calcification of the cervical ligament and hypertrophy of the joint capsule. These changes can, over time, compress one or more of the nerve roots, causing a series of symptoms. As the most common cervical spondylosis, cervical radiculopathy is clinically characterized by pain and numbness on the neck, shoulder and arms, and tender, and radiating pain on the nape[1]. We’ve observed the therapeutic efficacy differences in clinical improvement and pain alleviation between needling different points and combining needling with Chinese herbal fumigation. The results are now summarized as follows.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria in Western medicine
This is made according to the diagnostic basis for cervical radiculopathy stipulated in the Second National Symposium on Cervical Spondylosis[2]. Typical radicular symptoms (numbness, pain) in the area where the nerve that is irritated travels; positive Spurling sign and brachial plexus tension test; confirmation by images (cervical X-ray suggests: vertebral bone hyperplasia, visible hyperplasia of uncovertebral joint, narrowing of intervertebral spaces and smaller intervertebral foramen; CT or MRI scan shows: vertebral outgrowth and nerve root canal stenosis); no marked effect from a local anesthetic nerve block (unnecessary for those with a clear diagnosis); exclusion of pain in the upper limbs due to other conditions (for example, thoracic outlet syndrome, tennis elbow, carpal-tunnel syndrome, cubital-tunnel syndrome, adhesive capsulitis and bicipital tenosynovitis).
1.1.2 Diagnostic criteria (pattern identification) in Chinese medicine
According to the diagnostic basis for cervical spondylosis in theGuiding Principles for Clinical Study of New Chinese Medicines[3], this condition can be differentiated into the following two patterns.
Wind-cold blocking the meridians: Major symptoms include a history of extracting wind-cold, sore and cold limbs and the symptoms become better with warmth; minor symptoms include neck stiffness/pain, impaired movement, numbness/pain in the extremities, limb spasticity, muscular atrophy, and finger/toe numbness. The tongue is dark with a thin white coating. The pulse is deep wiry or deep slow.
Qi stagnation and blood stasis: Major symptoms include a history of cervical trauma or injury, neck stiffness/pain in a fixed location and the pain aggravates upon physical exertions. Minor symptom is limb numbness. The tongue is pale-red or dark-purple with stasis spots. The pulse is wiry or hesitant.
1.2 Inclusion criteria
Those who met the above criteria; men or women aged between 22 and 65 years; those who were willing to sign the informed consent and finish the required examinations and investigation.
1.3 Exclusion criteria
Those who failed to meet the above criteria; aged under 22 or above 65 years; having severe heart diseases or implanted a pacemaker; having coagulation disorders; having an allergic constitution or women during pregnancy or lactation; having complications of mental disorders or senile dementia; and those who received other clinical trials over the past 4 weeks.
1.4 General data
The 90 cases who met the inclusion criteria were outpatients and inpatients in Rehabilitation and Traumatology Departments of Dongnan Hospital of Huangpu District, Shanghai, between January 2011 and July 2012. They were allocated into three groups by single-blind randomized controlled clinical trial design. The three groups were the Jiaji (EX-B 2) points group, the eight neck points group and the comprehensive therapy group. Originally there were 30 cases in each group; however, 27, 28 and 30 cases were collected respectively due to multiple reasons (faint or left Shanghai during the treatment). The flow chart of clinical procedures in three groups was shown in Fig.1. There were no inter-group statistical differences in age, gender and duration (P>0.05), indicating that these three groups were comparable (table 1).
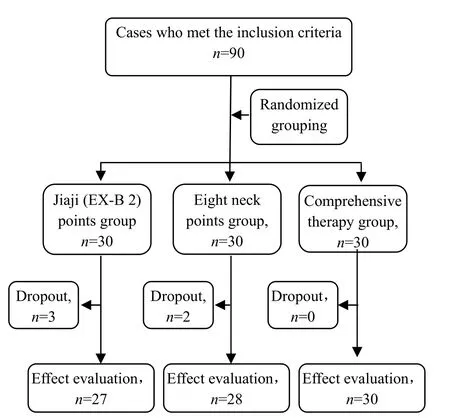
Fig.1 Flow chart of clinical procedure
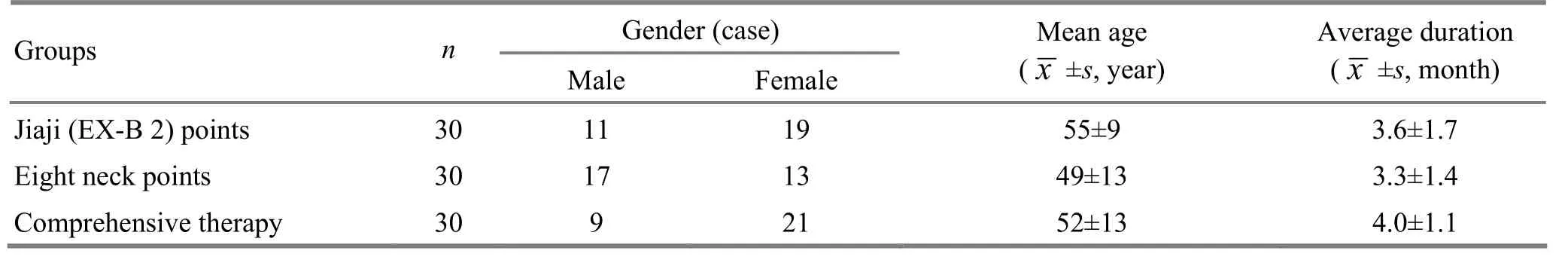
Table 1. Comparison of general data among three groups
2 Treatment Methods
2.1 Jiaji (EX-B 2) points group
Points: Bilateral cervical Jiaji (EX-B 2) points at the levels from C3-7.
Method: With a sitting or prone position of the patient, after sterilizing the local skin, punctured above Jiaji (EX-B 2) points 1.5 cun perpendicularly using disposable aseptic filiform needles of 0.25 mm in diameter and 40 mm in length. Retained the needles for 20 min upon arrival of qi. The treatment was conducted once a day, 5 times a week and 10 times for a course of treatment. The patients were treated for two consecutive courses (4 weeks).
2.2 Eight neck points group
Points: Jingbailao (EX-HN15), Dazhui (GV 14) and bilateral Fengchi (GB 20), Fengfu (GV 16) and Tianzhu (BL 10).
Method: With a sitting or prone position of the patient, after sterilizing the local skin, punctured above points 0.5-0.8 cun using disposable aseptic filiform needles of 0.25 mm in diameter and 40 mm in length. Followed with even reinforcing-reducing manipulation by rotating upon arrival of qi. Retained the needles for 20 min. The courses of treatment were same as the Jiaji (EX-B 2) points group.
2.3 Comprehensive therapy group
2.3.1 Needling the eight neck points
The points, needling methods and courses of treatment were same as the eight neck points group. 2.3.2 Chinese herbal fumigation
Formula ingredients:Zi Jing Pi(Cortex Cercis Chinensis) 30 g,Huang Jing Zi(Fructus Viticis Negundo) 20 g,Luo Shi Teng(Caulis Trachelospermi) 20 g,Qian Qian Huo(Sambucus Williamsii Hance) 30 g,Dang Gui(Radix Angelicae Sinensis) 10 g,Dan Shen(Radix et Rhizoma Salviae Miltiorrhizae) 20 g,Ji Xue Teng(Caulis Spatholobi) 30 g,Niu Xi(Radix Achyranthis Bidentatae) 20 g,Nan Xing(Arisaema cum Bile) 20 g,Hu Zhang(Rhizoma PolygoniCuspidati) 20 g,Bai Zhi(Radix Angelicae Dahuricae) 20 g,Jiang Huang(Rhizoma Curcumae Longae) 10 g,Gui Zhi(Ramulus Cinnamomi) 10 g,Chuan Wu(Radix Aconiti) 15 g,Cao Wu(Radix Aconiti Kusnezoffii) 15 g,Qiang Huo(Rhizoma et Radix Notopterygii) 10 g,Du Huo(Radix Angelicae Pubescentis) 10 g andXian Ling Pi(Epimedium davidii Franch) 20 g.
Method: The herbal fumigation was conducted after acupuncture using the self-controlled fumigation treatment device (manufactured by Sanzhou Medical Equipment Co. Ltd., Shanghai, China). Placed 800 mL of the herbal decoction into the treatment device and made the vapor exit aim at the affected area. Then turned the device on to emit the herbal steam (Fig.2). The fumigation lasted 20 min, once a day, and 10 times for a course of treatment. The patients were treated for two consecutive courses.

Fig.2 Chinese herbal fumigation
3 Therapeutic Efficacy Observation
3.1 Observation indexes
3.1.1 Traditional Chinese medicine symptom (TCM) scoring[3]
The TCM symptom scoring was performed before and after treatment according to theGuiding Principles for Clinical Study of New Chinese Medicines.
Recovery: Absence of clinical signs and symptoms, functional recovery and the decrease in scores of signs and symptoms was ≥95%.
Marked effect: Absence or substantial alleviation of clinical symptoms, remarkable improvement of clinical signs, basic functional recovery and the decrease in scores of signs and symptoms was ≥70% but <95%.
Improvement: Some alleviation of clinical signs and symptoms and the decrease in scores of signs and symptoms was ≥30% but <70%.
Failure: The signs and symptoms remain unchanged or aggravated after treatment, the decrease in scores of signs and symptoms was <30%.
3.1.2 Short-form McGill pain questionnaire (SF-MPQ)
The SF-MPQ was used to evaluate the pain rating index (PRI), visual analogue scale (VAS) and present pain intensity (PPI)[4].
3.2 Criteria of therapeutic efficacy
This was conducted according to the criteria of therapeutic efficacy for cervical spondylosis in theGuiding Principles for Clinical Study of New Chinese Medicines.
Recovery: Absence of clinical signs and symptoms, functional recovery, the decrease in scores of signs and symptoms was ≥95% and normal X-ray findings.
Marked effect: Absence or substantial alleviation of clinical symptoms, remarkable improvement of clinical signs, basic functional recovery and the decrease in scores of signs and symptoms was ≥70 but <95%.
Improvement: Some alleviation of clinical signs and symptoms and the decrease in scores of signs and symptoms was ≥30% but <70%.
Failure: The signs and symptoms remain unchanged or aggravated after treatment, the decrease in scores of signs and symptoms was <30%.
3.3 Statistical method
The SPSS 18.0 version software was used for statistical analysis, Chi-square test for numeration data, and analysis of variance andt-test for measurement data. A statistical significance is indicated byP<0.05.
3.4 Treatment results
3.4.1 Inter-group comparison of SF-MQP scores before and after treatment
After treatment, the PPI, VAS and PRI scores in three groups were all significantly reduced (P<0.01), and there were statistical differences in before-after PPI, VAS and PRI score differences among three groups (P<0.01), (table 2).
3.4.2 Inter-group comparison of clinical effects
The total effective rate in the comprehensive therapy group was higher than those in the other two groups (P<0.05), (table 3).
Table 2. Inter-group comparison of SF-MPQ scores before and after treatment (, point)
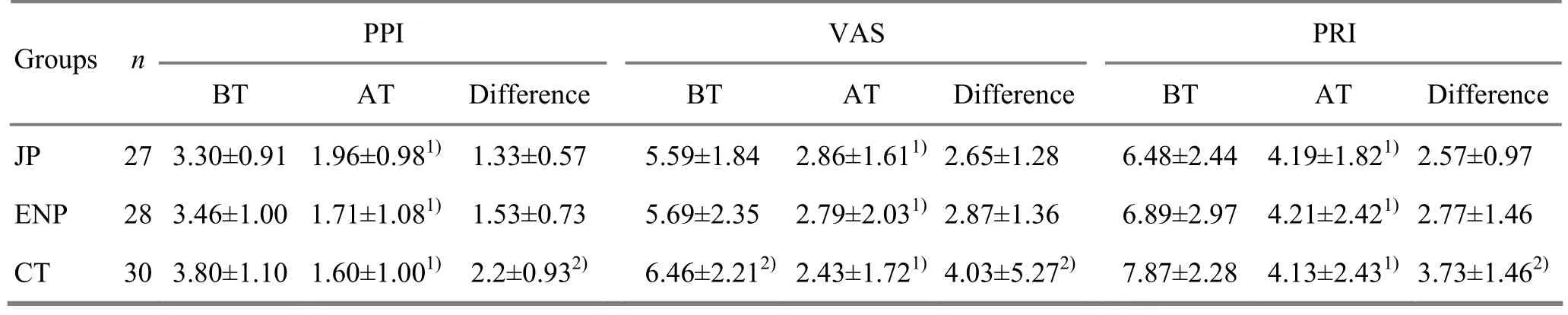
Table 2. Inter-group comparison of SF-MPQ scores before and after treatment (, point)
Note: JP=Jiaji (EX-B 2) point group; ENP=Eight neck points group; CT=Comprehensive therapy group; BT=Before treatment; AT=After treatment; compared with the intra-group results before treatment, 1)P<0.01; compared with the Jiaji (EX-B 2) points group and the eight neck points group, 2)P<0.01
GroupsnPPI VAS PRI BT AT Difference BT AT DifferenceBT AT Difference JP 27 3.30±0.91 1.96±0.981)1.33±0.57 5.59±1.842.86±1.611)2.65±1.286.48±2.44 4.19±1.821)2.57±0.97 ENP 28 3.46±1.00 1.71±1.081)1.53±0.73 5.69±2.352.79±2.031)2.87±1.366.89±2.97 4.21±2.421)2.77±1.46 CT 30 3.80±1.10 1.60±1.001)2.2±0.932)6.46±2.212)2.43±1.721)4.03±5.272)7.87±2.28 4.13±2.431)3.73±1.462)
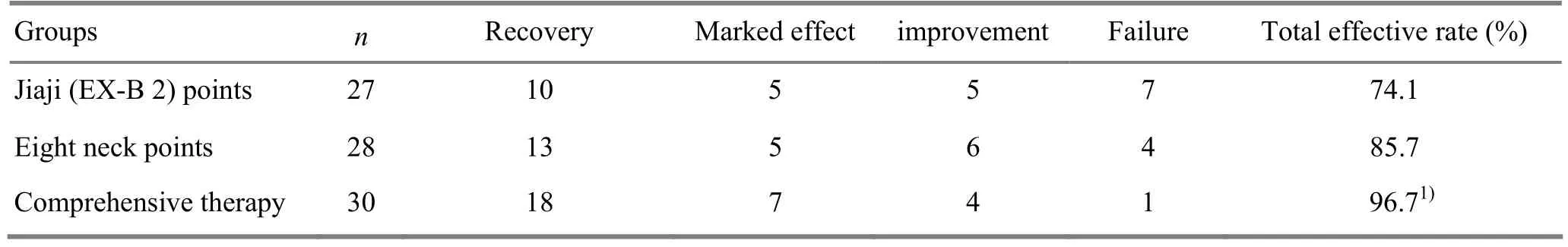
Table 3. Inter-group comparison of clinical effects (case)
4 Discussion
In Chinese medicine, cervical radiculopathy falls under the category of bone Bi-Impediment and neck-shoulder pain. Contributing factors include contraction of wind, cold and dampness, strain, improper neck postures, trauma or neck muscle spasm. This condition can be managed by many TCM therapies, including two common methods: acupuncture and Chinese herbal fumigation[5-10]. In the eight neck points group in this study, patients were treated with eight neck points. Specifically, Fengchi (GB 20) and Fengfu (GV 16) dissipate or subdue wind, unblock and open up orifices. Tianzhu (BL 10) and Dazhui (GV 14) regulate all yang meridians, circulate blood and unblock collaterals. Jingbailao (EX-HN 15) relieves spasm and alleviates pain. The study findings have shown that needling the eight neck points could obtain better effects than cervical Jiaji (EX-B 2) points.
Since cervical spondylosis is often closely associated with factors such as cold retention, blood stasis and kidney deficiency, acupuncture alone may not be sufficient enough to warm the local meridians and dissipate cold. Chinese herbal fumigation can directly work on the affected area to reinforce the actions of warming meridians, dissipate cold and circulate blood. This method is based on the principle of ‘treating cold syndrome with heat therapy’. In terms of total effective rate, combining needling eight neck points with Chinese herbal fumigation obtained better effect than the other two groups (P<0.05).
In conclusion, combining acupuncture and Chinese herbal fumigation has exact efficacy for cervical radiculopathy and is worthy of being popularized in clinical treatment.
[1] Zhao DL. Modern Diagnosis and Treatment of Cervical Spondylosis. Beijing: People's Military Medical Press, 2001: 72.
[2] Sun Y, Li GC. Memoir of the second symposium on cervical spondylosis. Jiefangjun Yixue Zazhi, 1994, 19(2): 156-158.
[3] Ministry of Health of the People’s Republic of China. Guiding Principles for Clinical Study of New Chinese Medicines. Beijing: China Medico-Pharmaceutical Science & Technology Publishing House, 2002: 138-140.
[4] Melzack R. The McGill pain questionnaire: major properties and scoring methods. Pain, 1975, 1(3): 277-299.
[5] Liu JQ, Zhuang SM, Lǚ HB, Liu J. Clinical observation on treatment of cervical vertigo by main selection of acupuncture. Shanghai Zhenjiu Zazhi, 2011, 30(1): 14-15.
[6] Yue JH, Zhang QH, Wang SL, Gao WB. Research progress of electroacupuncture treatment on cervical spondylosis radiculopathy in recent ten years. J Acupunct Tuina Sci, 2011, 9(2): 127-132.
[7] Luo KT, Luo AL, Shen ZF, Liu XL, Shen QH. Observation on the efficacy of warm needling plus acupoint application in treating cervical spondylotic radiculopathy. Shanghai Zhenjiu Zazhi, 2011, 30(8): 558-559.
[8] Zhang HK. Clinical observation on needling tendon for cervical spondylosis causing vertebral artery insufficiency. J Acupunct Tuina Sci, 2011, 9(1): 55-57.
[9] Sun DL, Chen DL, Ni CH, Zahng Y, Wang XF, Ma HF, Jiang HX. Randomized controlled trial of acupuncture plus behavior therapy for cervical spondylosis and cervical spondylotic radiculopathy. Shanghai Zhenjiu Zazhi, 2011, 30(6): 399-402.
[10] Liu HB. Therapeutic effect observation on combined tuina and Chinese medicinal fu migation for knee osteoarthritis. J Acupunct Tuina Sci, 2011, 9(3): 173-176.
Translator: Han Chou-ping
R246.2
A
date: June 15, 2013
Author: Jing Lei, attending physician.
E-mail: jinlei2001@163.com
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Therapeutic Efficacy Observation on Combining Acupuncture, Tuina and Functional Exercise for Transverse Process Syndrome of the Third Lumbar Vertebra
- Clinical Study on Moxibustion at Shenque (CV 8) for Chronic Urticaria
- Clinical Research Progress of Acupuncture-moxibustion for Chronic Urticaria
- Clinical Observation on Dong’s Extraordinary Points for Tinnitus Due to Cervical Spondylosis
- Observation on Clinical Effect of Superficial Needling for Intractable Humeral Epicondylitis
- Clinical Observation on Acupuncture Plus Acupoint Sticking for Bronchial Asthma in Remissive State
