Risk factors of poor prognosis and portal vein tumor thrombosis after curative resection of solitary hepatocellular carcinoma
2013-05-22
Beijing, China
Risk factors of poor prognosis and portal vein tumor thrombosis after curative resection of solitary hepatocellular carcinoma
Li Zhou, Jing-An Rui, Shao-Bin Wang, Shu-Guang Chen and Qiang Qu
Beijing, China
BACKGROUND:Predictors of poor prognosis of solitary hepatocellular carcinoma (SHCC), a subgroup encompassing most patients with the malignancy, are still controversial. Hence, risk factors for portal vein tumor thrombosis (PVTT) in SHCC are obscure. The present study was designed to address this issue.
METHOD:Clinicopathological and follow-up data for 156 consecutive patients with SHCC following curative hepatic resection were analyzed using uni- and multi-variate analyses.
RESULTS:Univariate analysis showed that PVTT, tumornode-metastasis (TNM) stage, Edmondson-Steiner grade and preoperative serum alpha-fetoprotein (AFP) level were associated with the overall and disease-free survival, whereas tumor size only inf l uenced the overall survival. In multivariate Cox regression tests, Edmondson-Steiner grade and TNM stage were independent prognostic markers for both overall and diseasefree survival. In addition, the Chi-square test showed that AFP level and Edmondson-Steiner grade were correlated with PVTT. Among them, only Edmondson-Steiner grade was shown to be of independent signif i cance for PVTT in multi-variate logistic regression analysis. Additionally, AFP, the sole preoperative factor for PVTT, was not adequately sensitive and specif i c.
CONCLUSIONS:Factors relating to post-surgical prognosis and PVTT in SHCC are all tumor-related. Of these, Edmondson-Steiner grade and TNM stage might be of particular importance in survival analysis. In addition, accurate prediction of PVTT by clinicopathological parameters before surgery remains diff i cult.
(Hepatobiliary Pancreat Dis Int 2013;12:68-73)
solitary hepatocellular carcinoma; curative resection; prognosis; portal vein tumor thrombosis
Introduction
Hepatocellular carcinoma (HCC) is life-threatening because of its high incidence and mortality.[1-3]So far, the overall clinical outcome of HCC remains unsatisfactory, although some improvements have been achieved in many curative and palliative modalities, such as hepatic resection, liver transplantation, radiofrequency ablation and transcatheter arterial chemoembolization (TACE).[4]Therefore, much attention has been paid to identify factors affecting the survival of HCC patients, including conventional clinicopathological variables and novel molecular markers.[5]Among them, tumor number was shown to be an important determinant of prognosis of HCC in patients undergoing several kinds of treatments.[6-10]Obviously, individuals with solitary HCC (SHCC) had relatively better survival than those with multi-nodular tumor. However, prognostic predictors of SHCC, the main subgroup of HCC according to tumor number,[7]are still controversial.[11,12]Thus, further accumulation of more relevant data is required.
Portal vein tumor thrombosis (PVTT), a unique disseminating manner of HCC, was found to be associated with poor prognosis of HCC.[13-15]Currently, imaging examinations including computed tomography (CT) are the main approaches for detection of PVTT, but their sensitivity and specif i city are unsatisfactory, especially for small-sized HCC.[16]Therefore, it is considered whether clinicopathological variables could be helpful in predicting PVTT. To the present, only preliminary of such method has been reported in patients with HCC.[17]The present study was designed to address the mentioned issue in a cohort of Chinese patients with SHCC who had undergone curative resection of the tumor.
Methods
Patients
The medical records of 156 patients with SHCC (def i ned as single nodular HCC without satellite lesion at the time of diagnosis), who had undergone curative hepatic resection from 1995 to 2002, were reviewed retrospectively. These patients consisted of 137 males and 19 females, with a median age of 47 years (range 15-77). Tumor size was def i ned as the largest dimension of the tumor mass. PVTT, based on fi ndings in imaging, operation and postoperative examination, indicated gross tumor invasion in the main branches of the portal vein. Tumor-nodemetastasis (TNM) staging and Edmondson-Steiner grading were carried out according to the conventional criteria.[18,19]Written informed consent was obtained from all patients.
Criteria of curative resection and determination of variables
The criteria of curative resection for patients with HCC were as follows: (1) Tumors (no more than three) were limited with at least two segments free of lesion; (2) No evidence of tumor thrombus in the trunks of the portal vein, hepatic vein and bile duct; (3) Child-Pugh grading was not worse than class B. Ten host and tumorrelated variables were evaluated by survival analyses: age, gender, hepatitis B surface antigen (HBsAg), hepatitis C virus C virus (HCV), Child-Pugh grade, preoperative alpha-fetoprotein (AFP) level, tumor size, PVTT, TNM stage and Edmondson-Steiner grade. For PVTT, TNM stage was excluded from the analyses, because PVTT was involved in the system.[18]
Adjuvant therapy and follow-up

Fig. 1.Imaging examinations of recurrent tumors (arrows) in patients with SHCC after curative resection.A: angiography;B: enhanced computed tomography. SHCC: solitary hepatocellular carcinoma.
After the resection, the patients, especially those with recurrent tumors, received multi-modal serial therapies including TACE, local ablation therapy and biological therapy. These patients were followed up every one month up to three months. Regular imaging (Fig. 1) and testing of serum AFP levels were performed to detect tumor recurrence and metastasis. Later, the patients were followed up from 3 to 108 months (median 19).
Statistical analysis
A statistical software package, SPSS11.5 (SPSS Inc., Chicago, IL., USA) was used for all analyses. The survival rate of the patients was calculated by the Kaplan-Meier method and compared with the log-rank test. Multivariate analysis was performed for prognostic factors by using the Cox regression test. The Chi-square and stepwise logistic regression test were adopted to evaluate risk factors of PVTT.Pvalues of less than 0.05 were regarded as statistically signif i cant.
Results
Overall and disease-free survival rates
The overall 1-, 3-, and 5-year survival rates of patients with SHCC were 82.9%, 54.7% and 47.8%, respectively (56±4 months; 95% conf i dence interval (CI) 48-65) (Fig. 2). Correspondingly, the 1-, 3-, and 5-year diseasefree survival rates were 70.3%, 36.4% and 22.5%, respectively (38±3 months; 95% CI: 31-44).

Fig. 2.Survival of patients with SHCC after curative resection.A: overall survival;B: disease-free survival. SHCC: solitary hepatocellular carcinoma.
Factors predictive for prognosis of patients with SHCC
Univariate analysis showed that Edmondson-Steiner grade, TNM stage, serum AFP level and PVTT were predictive for the overall and disease-free survival of SHCC patients, whereas tumor size inf l uenced the overall survival (P<0.05; Table 1). Other parameters were not statistically signif i cant (Table 1). In the Cox regression test, Edmondson-Steiner grade and TNM stage were independent prognostic markers for the overall and disease-free survival of the patients (P<0.05; Table 2).
Factors associated with PVTT in patients with SHCC
PVTT was preliminarily diagnosed by imagingexaminations in 13 patients and pathologically conf i rmed in 17. By the Chi-square test, serum AFP level (χ2=6.528,P=0.011) and Edmondson-Steiner grade (χ2=7.373,P=0.007) were associated with PVTT (Table 3), whereas gender, age, HBsAg, HCV, liver cirrhosis, Child-Pugh grade and tumor size were not signif i cant (Table 3). Of the signif i cant factors, AFP, the single preoperative variable, carried a sensitivity of 64.7% (11/17), a specif i city of 66.9% (93/139), a positive predictive value of 19.3% (11/57), and a negative predictive value of 93.9% (93/99). In stepwise logistic regression analysis, Edmondson-Steiner grade was of independent predictive power for PVTT in SHCC (RR=3.467, 95% CI: 1.032-11.65,P=0.044), whereas marginal signif i cant difference for AFP level was also shown (RR=2.685, 95% CI: 0.894-8.065,P=0.078).

Table 1.Factors predictive for prognosis of SHCC after curative resection
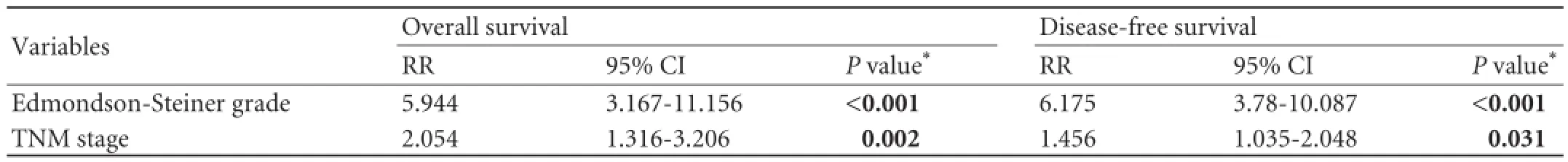
Table 2.Independent prognostic factors of SHCC after curative resection

Table 3.Univariate factors associated with PVTT in SHCC
Discussion
SHCC, compared with multiple nodular HCC, is strongly suggested to have better prognosis.[6-10]Satisfactory fi ve-year overall and disease-free survival rates (79.6% and 41.1%, respectively) were achieved in a Japanese cohort of patients with SHCC who had undergone hepatic resection.[12]However, the present series presented a relatively poorer prognosis (the fi veyear overall and disease-free survival rates of 47.8% and 22.5%, respectively). Demographic characteristics such as smaller tumor size (3.13 cm) and higher HCV positivity (66.5%) in the Japanese patients might account in part for the observed difference, because the two features were shown to be associated with better prognosis of HCC.[5,20,21]However, the variables inf l uencing the prognosis of SHCC, which were deemed controversial in previous studies,[11,12]remain to be elucidated. The signif i cant risk factors for early death included gross tumor classif i cation, tumor diameter, macroscopic portal vein invasion, microscopic growth pattern, microscopic vascular invasion and the width of surgical margin.[11]However, tumor-related factors do not inf l uence the prognosis of SHCC after partial hepatectomy.[12]Univariate analysis in our study revealed that Edmondson-Steiner grade, TNM stage and preoperative serum AFP level were signif i cant markers for the overall and disease-free survival of patients, along with vascular invasion, tumor size and PVTT (Table 1). The present study is the fi rst to identify these newly introduced factors as prognostic indicators for SHCC, although they were reported to be prognostic in other subsets of HCC.[22-24]Among these factors, Edmondson-Steiner grade and TNM stage were of independent prognostic implications, suggesting that the two variables might be particularly important. Another phenomenon that should be noted is that all the prognosticators were tumor-related, strongly indicating the pivotal role of tumor characteristics in the prognosis of SHCC, and supporting the fi nding of Kondo et al.[11]
PVTT, arising from the invasion of HCC cells into the portal vein, is well acknowledged as a special type of metastasis in HCC.[25]The presence of PVTT is associated with unfavorable prognosis of HCC.[13-15]Recently, some investigators reported that tumor response after TACE was signif i cantly affected by PVTT,[26]which is consistent with our fi nding. Currently, imaging examinations remain the gold standard in the diagnosis of PVTT. However, the diagnostic power, especially the sensitivity, is unsatisfactory.[16]Studies[27-31]found that some cancer-related molecules such as platelet-derived endothelial cell growth factor (PD-ECGF), vascular endothelial growth factor(VEGF), thrombomodulin, angiopoietin 2, ephrin B2 and low molecular weight protein have the potential to serve as biomarkers of PVTT in HCC. However, the predictive power of conventional clinical and pathological parameters is less well evaluated. Another study[17]demonstrated the signif i cant association of age, gamma-glutamyltransferase, number of segmental invasion, microvascular invasion, and segment location of S2, S3, S4 and S6. In our study, serum AFP level and Edmondson-Steiner grade were associated with PVTT. It was reported that tumor differentiation is closely related to vascular invasion and proliferation in HCC.[32,33]The fi nding that poorly differentiated HCC carries an increased expression of angiogenic factors and high microvessel density might account, at least in part, for this correlation.[32,34]Therefore, the relation of PVTT and Edmondson-Steiner grade in SHCC might be easily understood. However, data regarding the aforementioned factors could not be obtained before surgery. In addition, we identif i ed serum AFP level as a potential signif i cant marker of PVTT by univariate analysis. Researchers[35-38]observed that AFP could promote proliferation, mediate escape of immune surveillance and inhibit apoptosis in human HCC cells, via regulation of the expression of c-Fos, c-Jun, N-Ras, Fas/FasL and caspase-3. Other experiments using specif i c stealth RNAi of AFP also conf i rmed its impact on the proliferation and apoptosis of HCC cells.[39]Currently, there has been no direct evidence for the role of AFP in invasion/metastasis of HCC cells. However, high AFP value (>400 ng/mL) was found in well, moderately and poorly differentiated HCC.[40]There was a relationship between differentiation and vascular invasion.[33]Thus AFP may be associated with PVTT, an important manner of vascular invasion of HCC. Of course, AFP, the sole preoperative parameter, in the present study did not show a sensitivity and a specif i city for PVTT. It was not superior to those previously reported for CT scanning,[16]indicating that the predictive power of this variable was limited in this cohort. In future, more indepth investigations with larger sample sizes might be necessary for a fi nal conclusion.
In summary, our data indicate that factors relating to post-surgical prognosis and PVTT in SHCC are all tumor-related. Edmondson-Steiner grade and TNM stage might be of particular importance in survival analysis, whereas the accurate preoperative prediction of PVTT by clinicopathological parameters remains diff i cult.
Contributors:ZL proposed the study and wrote the fi rst draft. ZL, RJA, WSB, CSG and QQ analyzed the data. All authors contributed to the design and interpretation of the study and to further drafts. ZL is the guarantor.
Funding:This study was supported by a grant from the Beijing Municipal Fund for Key Disciplines, China (100230446).
Ethical approval:Not needed.
Competing interest:No benef i ts in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Parkin DM, Pisani P, Ferlay J. Estimates of the worldwide incidence of eighteen major cancers in 1985. Int J Cancer 1993;54:594-606.
2 Parkin DM, Bray F, Ferlay J, Pisani P. Estimating the world cancer burden: Globocan 2000. Int J Cancer 2001;94:153-156.
3 Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin 2005;55:74-108.
4 Rahbari NN, Mehrabi A, Mollberg NM, Müller SA, Koch M, Büchler MW, et al. Hepatocellular carcinoma: current management and perspectives for the future. Ann Surg 2011; 253:453-469.
5 Tandon P, Garcia-Tsao G. Prognostic indicators in hepatocellular carcinoma: a systematic review of 72 studies. Liver Int 2009;29: 502-510.
6 Takata M, Yamanaka N, Tanaka T, Yamanaka J, Maeda S, Okamoto E, et al. What patients can survive disease free after complete resection for hepatocellular carcinoma?: A multivariate analysis. Jpn J Clin Oncol 2000;30:75-81.
7 Nathan H, Schulick RD, Choti MA, Pawlik TM. Predictors of survival after resection of early hepatocellular carcinoma. Ann Surg 2009;249:799-805.
8 Fan J, Yang GS, Fu ZR, Peng ZH, Xia Q, Peng CH, et al. Liver transplantation outcomes in 1078 hepatocellular carcinoma patients: a multi-center experience in Shanghai, China. J Cancer Res Clin Oncol 2009;135:1403-1412.
9 Waki K, Aikata H, Katamura Y, Kawaoka T, Takaki S, Hiramatsu A, et al. Percutaneous radiofrequency ablation as fi rst-line treatment for small hepatocellular carcinoma: results and prognostic factors on long-term follow up. J Gastroenterol Hepatol 2010;25:597-604.
10 Hsieh MY, Chang WY, Wang LY, Chen SC, Chuang WL, Lu SN, et al. Treatment of hepatocellular carcinoma by transcatheter arterial chemoembolization and analysis of prognostic factors. Cancer Chemother Pharmacol 1992;31: S82-85.
11 Kondo K, Chijiiwa K, Makino I, Kai M, Maehara N, Ohuchida J, et al. Risk factors for early death after liver resection in patients with solitary hepatocellular carcinoma. J Hepatobiliary Pancreat Surg 2005;12:399-404.
12 Kobayashi T, Itamoto T, Tashiro H, Amano H, Oshita A, Tanimoto Y, et al. Tumor-related factors do not inf l uence the prognosis of solitary hepatocellular carcinoma after partial hepatectomy. J Hepatobiliary Pancreat Sci 2011;18:689-699.
13 Ercolani G, Grazi GL, Ravaioli M, Del Gaudio M, Gardini A, Cescon M, et al. Liver resection for hepatocellular carcinoma on cirrhosis: univariate and multivariate analysis of risk factors for intrahepatic recurrence. Ann Surg 2003;237:536-543.
14 Zhou J, Fan J, Wu ZQ, Qiu SJ, Huang XW, Yu Y, et al. Liver transplantation for patients with hepatocellular carcinoma at the Liver Cancer Institute of Fudan University, China. ChinMed J (Engl) 2005;118:654-659.
15 Kawaoka T, Aikata H, Takaki S, Hashimoto Y, Katamura Y, Hiramatsu A, et al. Transcatheter chemoembolization for unresectable hepatocellular carcinoma and comparison of fi ve staging systems. Hepatol Res 2010;40:1082-1091.
16 Lee HK, Park SJ, Yi BH, Yeon EK, Kim JH, Hong HS. Portal vein thrombosis: CT features. Abdom Imaging 2008;33:72-79.
17 Lü WP, Dong JH, Huang ZQ, Shi S, Guo DY, Liu YS. Clinical related factors of portal vein tumor thrombosis in patients with hepatocellular carcinoma: a logistic regression analysis. Zhonghua Wai Ke Za Zhi 2008;46:733- 736.
18 Sobin LH, Wittekind C. TNM classif i cation of malignant tumors. 6th ed. New York: Wiley-Liss; 2002:81-83.
19 Edmondson HA, Steiner PE. Primary carcinoma of the liver: a study of 100 cases among 48900 necropsies. Cancer 1954;7: 462-503.
培育并推出德艺双馨、具有全国影响力的领军人物和名家大师,发挥领军人物在画派中的引领作用,提升画派的凝聚力和感召力,既是漓江画派长期的战略任务,也是紧迫的现实课题。
20 Chen CH, Huang GT, Yang PM, Chen PJ, Lai MY, Chen DS, et al. Hepatitis B- and C-related hepatocellular carcinomas yield different clinical features and prognosis. Eur J Cancer 2006;42:2524-2529.
21 Cescon M, Cucchetti A, Grazi GL, Ferrero A, Viganò L, Ercolani G, et al. Role of hepatitis B virus infection in the prognosis after hepatectomy for hepatocellular carcinoma in patients with cirrhosis: a Western dual-center experience. Arch Surg 2009;144:906-913.
22 Choi GH, Kim DH, Choi SB, Kang CM, Kim KS, Choi JS, et al. The preoperative positivity for serum hepatitis B e antigen did not affect overall survival after curative resection of hepatitis B virus-related hepatocellular carcinoma. J Gastroenterol Hepatol 2009;24:391-398.
23 Huang J, Zhang X, Tang Q, Zhang F, Li Y, Feng Z, et al. Prognostic signif i cance and potential therapeutic target of VEGFR2 in hepatocellular carcinoma. J Clin Pathol 2011;64: 343-348.
24 Mailey B, Artinyan A, Khalili J, Denitz J, Sanchez-Luege N, Sun CL, et al. Evaluation of absolute serum α-fetoprotein levels in liver transplant for hepatocellular cancer. Arch Surg 2011;146:26-33.
25 Wang T, Hu HS, Feng YX, Shi J, Li N, Guo WX, et al. Characterisation of a novel cell line (CSQT-2) with high metastatic activity derived from portal vein tumour thrombus of hepatocellular carcinoma. Br J Cancer 2010;102: 1618-1626.
26 Vogl TJ, Nour-Eldin NE, Emad-Eldin S, Naguib NN, Trojan J, Ackermann H, et al. Portal vein thrombosis and arterioportal shunts: effects on tumor response after chemoembolization of hepatocellular carcinoma. World J Gastroenterol 2011;17: 1267-1275.
28 Guo L, Kuroda N, Toi M, Miyazaki E, Hayashi Y, Enzan H, et al. Increased expression of platelet-derived endothelial cell growth factor in human hepatocellular carcinomas correlated with high Edmondson grades and portal vein tumor thrombosis. Oncol Rep 2001;8:871-876.
29 Zhou J, Tang ZY, Fan J, Wu ZQ, Ji Y, Ye SL. The potential of plasma thrombomodulin as a biomarker of portal vein tumor thrombus in hepatocellular carcinoma. J Cancer Res Clin Oncol 2001;127:559-564.
30 Li Q, Xu B, Fu L, Hao XS. Correlation of four vascular specif i c growth factors with carcinogenesis and portal vein tumor thrombus formation in human hepatocellular carcinoma. J Exp Clin Cancer Res 2006;25:403-409.
31 Qiu JG, Fan J, Liu YK, Zhou J, Dai Z, Huang C, et al. Screening and detection of portal vein tumor thrombiassociated serum low molecular weight protein biomarkers in human hepatocellular carcinoma. J Cancer Res Clin Oncol 2008;134:299-305.
32 Suehiro T, Matsumata T, Itasaka H, Yamamoto K, Kawahara N, Sugimachi K. Clinicopathologic features and prognosis of resected hepatocellular carcinomas of varied sizes with special reference to proliferating cell nuclear antigen. Cancer 1995;76:399-405.
33 Makatsoris T, Petsas T, Tsamandas AC, Pagoni N, Papathanassiou Z, Karavias D, et al. Hepatocellular carcinoma in hepatectomized patients: biologic and therapeutic implications. Anticancer Res 2005;25:3067-3073.
34 Wada H, Nagano H, Yamamoto H, Yang Y, Kondo M, Ota H, et al. Expression pattern of angiogenic factors and prognosis after hepatic resection in hepatocellular carcinoma: importance of angiopoietin-2 and hypoxia-induced factor-1 alpha. Liver Int 2006;26:414-423.
35 Li MS, Li PF, Chen Q, Du GG, Li G. Alpha-fetoprotein stimulated the expression of some oncogenes in human hepatocellular carcinoma Bel 7402 cells. World J Gastroenterol 2004;10:819-824.
36 Li M, Liu X, Zhou S, Li P, Li G. Effects of alpha fetoprotein on escape of Bel 7402 cells from attack of lymphocytes. BMC Cancer 2005;5:96.
37 Li M, Zhou S, Liu X, Li P, McNutt MA, Li G. alpha-Fetoprotein shields hepatocellular carcinoma cells from apoptosis induced by tumor necrosis factor-related apoptosisinducing ligand. Cancer Lett 2007;249:227-234.
38 Li M, Li H, Li C, Zhou S, Guo L, Liu H, et al. Alpha fetoprotein is a novel protein-binding partner for caspase-3 and blocks the apoptotic signaling pathway in human hepatoma cells. Int J Cancer 2009;124:2845-2854.
39 Yang X, Zhang Y, Zhang L, Zhang L, Mao J. Silencing alphafetoprotein expression induces growth arrest and apoptosis in human hepatocellular cancer cell. Cancer Lett 2008;271:281-293.
40 Oishi K, Itamoto T, Amano H, Fukuda S, Ohdan H, Tashiro H, et al. Clinicopathologic features of poorly differentiated hepatocellular carcinoma. J Surg Oncol 2007;95:311-316.
Received November 28, 2011
Accepted after revision April 5, 2012
AuthorAff i liations:Department of General Surgery, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences/Peking Union Medical College, Beijing 100730, China (Zhou L, Rui JA, Wang SB, Chen SG and Qu Q)
Li Zhou, MD, Department of General Surgery, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences/Peking Union Medical College, Beijing 100730, China (Tel: 86-10-65296007; Fax: 86-10-65296010; Email: lizhou02@hotmail.com)
© 2013, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(13)60008-9
猜你喜欢
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Terry's nail:an overlooked physical finding in cirrhosis
- Melanoma in the ampulla of Vater
- Hepatic portal venous gas in pancreatic solitary metastasis from an esophageal squamous cell carcinoma
- News
- Drainage by urostomy bag after blockage of abdominal drain in patients with cirrhosis undergoing hepatectomy
- TRAIL-induced expression of uPA and IL-8 strongly enhanced by overexpression of TRAF2 and Bcl-xL in pancreatic ductal adenocarcinoma cells