强直性脊柱炎并发干燥综合征患者的临床特点及其实验室检查结果分析
2012-12-07常利华张晓莉李忠义王晓非
常利华,蒋 莉,郭 韵,张晓莉,李忠义,王晓非
(1.中国医科大学附属盛京医院风湿免疫科,辽宁沈阳110022;2.沈阳医学院奉天医院手外二科,辽宁 沈阳110024)
强直性脊柱炎并发干燥综合征患者的临床特点及其实验室检查结果分析
常利华1,蒋 莉1,郭 韵1,张晓莉1,李忠义2,王晓非1
(1.中国医科大学附属盛京医院风湿免疫科,辽宁沈阳110022;2.沈阳医学院奉天医院手外二科,辽宁 沈阳110024)
目的:阐明强直性脊柱炎 (AS)并发干燥综合征 (SS)患者的特点,为该病的治疗及并发症的防治提供依据。方法:选择确诊的AS并发SS患者11例,总结临床特点和实验室检查结果,分别比较AS并发SS与单纯AS和单纯SS患者外周关节受累率、人类白细胞抗原-B27(HLA-B27)阳性率、抗核抗体 (ANA)阳性率和C反应蛋白 (CRP)、血沉 (ESR)及免疫球蛋白水平。结果:11例患者均符合AS和SS的诊断标准,均有腰背痛与口干和 (或)眼干症状;外周关节受累9例,葡萄膜炎1例;影像学示骶髂关节炎双侧≥2级9例,单侧3级1例,单侧4级1例;HLA-B27阳性7例,HLA-B27阳性率 (63.6%)明显低于单纯AS患者 (92.9%)(P<0.05);唾液腺放射性核素检查阳性9例;泪液分泌试验阳性11例;ANA阳性9例,ANA阳性率(81.8%)与单纯SS患者 (84.8%)比较差异无统计学意义;抗SSA抗体阳性8例;抗SSB抗体阳性6例;唇腺病理检查阳性11例。AS并发SS患者CRP、ESR和免疫球蛋白水平高于单纯AS和SS患者,但差异无统计学意义 (P>0.05);与AS患者比较,AS并发SS患者高球蛋白血症发生率升高 (P<0.05)。结论:AS和SS可以同时发生,两病同时并发患者更易出现外周关节受累。
强直性脊柱炎;干燥综合征;抗核抗体;免疫球蛋白
强直性脊柱炎 (ankylosing spondylitis,AS)是以骶髂关节和脊柱慢性炎症、进行性炎症为主的全身性疾病;干燥综合征 (Sjogren’s syndrome,SS)是一种主要累及全身外分泌腺的慢性炎症性自身免疫疾病。二者可单独发病,也可同时出现,但患者同时出现上述2种疾病的报道并不多见。本研究总结11例确诊AS并发SS患者的临床特点和实验室检查结果,旨在提高对AS和SS共存的认识。
1 资料与方法
1.1 一般资料 选择2008年—2011年在中国医科大学附属盛京医院风湿免疫科住院治疗的AS患者488例和SS患者336例,其中同时患有AS和SS患者 (AS+SS组)11例,男性4例,女性7例,年龄18~49岁,平均年龄35岁,病程1~22年,平均病程9.6年。从上述患者中随机选取单纯AS患者 (AS组)42例,男性35例,女性7例,年龄14~52岁,平均年龄29.2岁,病程0.5~36.0年,平均病程12.3年;单纯SS患者(SS组)33例,男性3例,女性30例,年龄17~55岁,平均年龄42.6岁,病程0.5~15.0年,平均病程8.9年。所有患者均符合AS和SS国际分类标准 (修订的纽约标准)的诊断标准。
1.2 实验室检查指标 采用免疫比浊法检测C反应蛋白 (CRP)水平;魏氏法检测血沉 (ESR)水平;免疫比浊法检测免疫球蛋白 (IgA、IgM和IgG)水平;ELISA法检测抗核抗体 (antinuclear antibody,ANA)、抗SSA抗体、抗SSB抗体水平;流式细胞术检测人类白细胞抗原-B27>(HLA-B27)阳性率。
1.3 统计学分析 采用SAS 9.2统计软件进行数据分析。外周关节受累率、HLA-B27阳性率、ANA阳性率和CRP、ESR及高球蛋白血症发生率组间比较采用χ2检验。
2 结 果
2.1 AS并发SS患者临床表现 11例患者均有腰背痛、口干和 (或)眼干症状。其中有炎性腰背痛11例,口干9例,眼干11例,中轴骶髂关节炎11例,外周关节受累9例,单关节炎6例,多关节炎3例 (其中髋关节6例,膝关节4例,踝关节3例,肩关节2例,肘关节1例,腕关节1例,手足小关节3例),葡萄膜炎1例。外周关节受累情况:AS+SS组关节受累率 (9/11,81.8%)高于单纯AS组 (28/42,66.7%)和单纯SS组 (14/33,42.4%),差异有统计学意义 (P<0.05)。见表1。
2.2 实验室检查 单纯AS组患者影像学检查示骶髂关节炎双侧≥2级9例,单侧3级1例,单侧4级1例;HLA-B27阳性7例,阳性率为63.6%,HLA-B27阳性率明显低于单纯AS组 (92.9%),差异有统计学意义 (P<0.05)。单纯SS组患者唾液腺放射性核素检查阳性9例,泪液分泌试验阳性11例,ANA阳性9例,抗SSA抗体阳性8例,抗SSB抗体阳性6例,抗双链DNA抗体、抗Sm抗体、抗U1RNP抗体和抗Scl-70抗体均为阴性,唇腺病理检查阳性11例。ANA阳性率为81.8%,略低于单纯SS组 (84.8%),但差异无统计学意义 (P>0.05)。AS+SS组CRP、ESR和免疫球蛋白水平均高于单纯AS组和SS组,AS+SS组高球蛋白血症发生率明显高于AS组 (P<0.05),其他指标比较差异均无统计学意义。见表2。
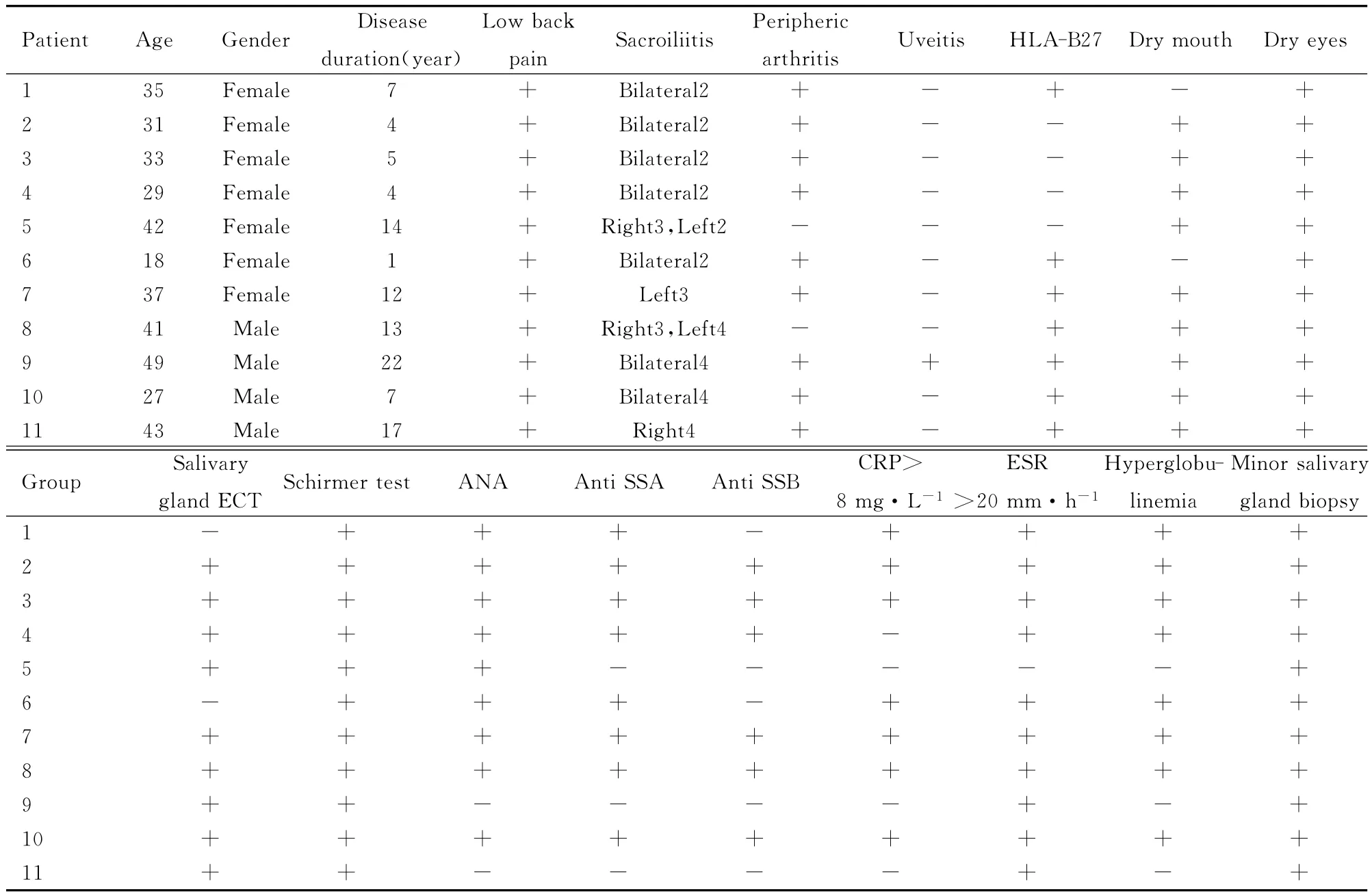
表1 11例AS并发SS患者临床表现Tab.1 Clinical manifestations of 11patients with AS complicated with SS
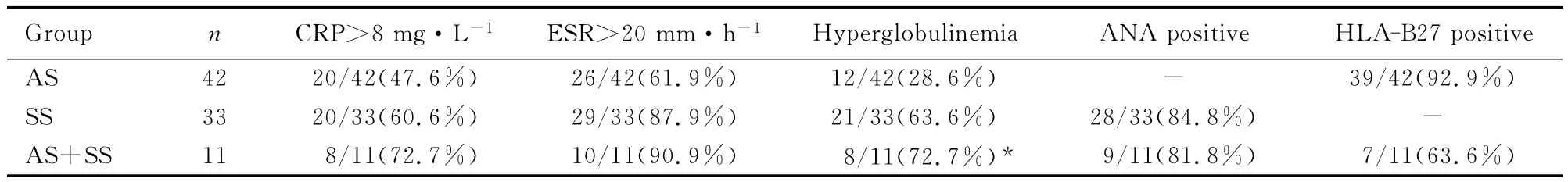
表2 AS+SS组与单纯AS、单纯SS组患者实验室检测结果比较Tab.2 Comparisons of laboratory findings of patients between AS+SS group and AS group,SS group
3 讨 论
AS以累及中轴关节和肌腱、韧带附着点为主,与HLA-B27密切相关。SS是以侵犯外分泌腺为主,以口干、眼干为常见表现的自身免疫性疾病,属于弥漫结缔组织病。本研究中11例患者均符合AS和SS诊断标准,表明二者可以同时发生。
1971年Whaley等[1]首先发现在AS患者中,部分患者并发SS症状,并行唇腺活检发现淋巴细胞 灶, 此 后 陆 续 有 AS 并 发 SS 的 报 道[2-4]。2006年Kobak等[5]报道:在70例确诊的AS患者中筛查SS患者,7例患者 (男性6例,女性1例,平均年龄46.7岁)符合SS的诊断标准,占AS患者的10%,再次证实二者可同时发病,且AS患者中SS发病几率明显高于正常人群,其发病机制尚不清楚,可能与以下遗传、感染、细胞因子及基质金属蛋白酶 (matrix metalloproteinase,MMP)等有关。
3.1 遗传因素 从1973年第1次发现HLA-B27与AS之间的强相关性至今,HLA-B27一直是AS病因中最重要因素[6]。HLA-B27基因位于第6号染色体短区,至少包含31个密切相关的等位基因。SS与免疫遗传因素有关,研究[7]发现:SS与HLA-B8、HLA-DR3有关联,另外,大部分原发性SS患者均有 HLA-DQA1*0501频率增高,提示HLA-DQA1*0501是一个重要的SS相关基因。此外,还有定位于6号染色体主要组织相容性复合物区域中心位置的肿瘤坏死因子 (TNFα)等位基因与SS发病有关。AS与HLA的Ⅰ型B27有密切关联,SS与HLA的Ⅱ型DR3有相关性,1998年Golstein等[2]报道2例AS并发SS患者 HLA的Ⅰ和Ⅱ型表现极其相似而增加了二者共存的机会。
3.2 感染因素 细菌感染与HLA-B27之间的作用可能是AS发病机制的关键因素之一,细菌主要有弯曲杆菌属、衣原体属和志贺菌属等。感染可引起一些无效的多肽结合到HLA-B27上并诱发变态免疫反应,导致胞内细菌的过度增殖和对抗原肽的延迟处理[8]。最早发现的与SS有关的病毒是EB病毒,EB病毒常寄生于人的唾液腺,可在B淋巴细胞和上皮细胞内进行周期性复制,导致淋巴细胞增生。有学者[9]在SS患者唇腺组织、肾脏组织和外周血中均检测到EB病毒的DNA。SS患者的腮腺内存在EB病毒相关的抗原且EB病毒的DNA也已被证实。
3.3 细胞因子因素 AS的免疫病理发病机制与促炎细胞因子表达的上调有关,TNF-α在AS患者体内的表达水平明显高于健康个体的表达水平,并且有证据[10]表明:抗TNF-α治疗能有效地提高AS患者的疗效。血清中IL-6和可溶性IL-2受体水平在AS患者中明显升高。TNF-α在SS患者的腮腺组织内有丰富表达,用寡核苷酸探针与原位杂交的技术检测到SS患者下颌下腺中含有促炎细胞因子IL-6和IL-1,而且这些细胞因子mRNA在浸润淋巴细胞和上皮细胞中均有表达。由此可见,细胞因子参与了AS和SS的发病。
3.4 MMP因素 MMP与其抑制因素的病态失衡会引发炎症,并且在AS患者中已经发现了血清MMP-3的高表达[11],而这与AS的疾病活动度和功能指数有确定的相关关系。Perez等[12]证实SS患者唇腺中的MMP-3mRNA和蛋白水平较对照组增加,且其蛋白增高的程度与腺体组织结构破坏程度相关。因此,AS和SS病程发生发展中MMP-3均发挥了重要作用。
综上所述,AS和SS在发病机制上具有相似之处,但具体机制尚不明确,仍需进一步研究。2种疾病在临床上可以同时出现,因此医生应高度警惕二者并发的可能。对于已确诊的AS病程较长者,特别是中青年女性患者,如出现多个外周关节受累,应注意询问有无口干和 (或)眼干症状并行抗核抗体谱检查,注意并发SS的可能;而确诊为SS患者,同时出现腰背痛、下肢不对称关节炎和色素膜炎时,应行骶髂关节影像学和HLA-B27检查,注意SS并发AS的可能。患者如果同时患AS和SS,更易出现外周关节受累,炎性指标往往升高。AS并发SS治疗上应注意二者兼顾,可给予非甾体抗炎药改善关节症状,如病情需要应用糖皮质激素,应选择合理的剂量及疗程。
[1]Whaley K,Chisholm DM,Willianmson J,et al.Sjogren’s syndrome in psoriatic arthritis,ankylosing spondylitis and Reiter’s syndrome[J].Acta Rheum Scand,1971,17 (2):105-114.
[2]Goldsein MA,Steinfeld S. Ankylosing spondylitis with primary Sjogren’s syndrome:the two case-reports[J].Rev Rheum Eng Ed,1998,65 (6):434-436.
[3]Treves R,Vergne P, Bonnet C,et al. Concomitant ankylosing spondylitis and Sjogren’s syndrome [J].Rev Rheum Eng Ed,1998,65 (12):801.
[4]Tosun M,Karkucak M,Capkin E,et al.Coexisting ankylosing spondylitis and Sjogren’s syndrome:a case report[J].Rheumatol Int,2005,25 (6):478-480.
[5]Kobak S,Kobak AC,Kabasakal Y,et al.Sjogren’s syndrome in patients with ankylosing spondylitis [J].Clin Rheumatol,2007,26 (2):173-175.
[6]Brown MA.Genetics of ankylosing spondylitis [J].Curr Opin Rheumatol,2010,22 (2):126.
[7]Robert L.HLA in health and disease[M].2nd ed.London:Academic Press,2000:353.
[8]Stone MA,Payne U,Sehentag C,et al.Comparative immune responses to candidate arthritogenic bacteria do not confirm a dominant role for Kleb-Siella pneumonia in the pathogenesis of familial ankylosing spondylitis [J].Rheunmtology (Oxford),2004,43 (2):148-155.
[9]Youinou P,Pers JO,Saraux A,et al.Viruses contribute to the development of Sjogren’s syndrome [J]. Clin Expimmunol,2005,141 (7):19-20.
[10]Arends S,Brouwer E,van der Veer E,et al.Baseline predictors of response and discontinuation of tumor necrosis factor-alpha blocking therapy in ankylosing spondylitis:a prospective longitudinal observational cohort study [J].Arthritis Res Ther,2011,13 (1):R94.
[11]Chen CH,Lin KC, Yu DT,et al. Serun matrix metalloproteinases and tissue inhibitors of metalloproteinases in ankylosing spondylitis:MMP-3is a reproducibly sensitive and specific biomarker of disease activity [J].Rheumatology(Oxford),2006,45 (4):414-420.
[12]Perez P,Goicovich E, Alliende C,et al.Differential expression of matrix metalloproteinases in labial salivary glands of patients with primary Sjogren’s syndrome [J].Arthritis Rheum,2000,43 (12):2807-2817.
Analysis of clinical features and laboratory fingdings in patients with ankylosing spondylitis complicated with Sjogren’s syndrome
CHANG Li-hua1,JIANG Li1,GUO Yun1,ZHANG Xiao-li1,LI Zhong-yi2,WANG Xiao-fei1
(1.Department of Rheumatology,Affiliated Shengjing Hospital,China Medical University,Shenyang 110022,China;2.Department of Hand Surgery,Fengtian Hospital,Shenyang Medical College,Shenyang 110024,China)
ObjectiveTo clarify the characteristics of the patients with ankylosing spondylitis(AS)complicated with Sjogren’s syndrome (SS),and to provide basis for its treatment and prevention of complications.Methods11cases diagnosed as AS complicated with SS were selected,and the clinical features and laboratory fingdings were summarized retrospectively;the rate of involved joints,HLA-B27positive rate,antinuclear antibody (ANA)positive rate,and the levels of C-reaction protein (CRP),erythrocyte sedimentation rate(ESR)and immunoglobulin were compared between the patients with AS complicated with SS and the simple AS or SS patients.ResultsAll the 11patients were in line with the diagnostic criteria for AS and SS with low back pain and sicca symptoms;peripheral joints were involved in 9cases.1case had uveitis;the imaging studies showed that there were 9cases of grade 2bilateral sacroiliitis and above,and 1case of grade 3unilateral sacroiliitis,1case of grade 4unilateral sacroiliitis.The HLA-B27was positive in 7cases,and the positive rate (63.6%)was significantly lower than that of simple AS patients (92.9%) (P<0.05).The salivary radionuclide examination was positive in 9cases;the Schirmer test was positive in 11cases.Among 11patients with AS complicated with SS,9cases were ANA positive,the ANA positive rates had no significant difference between patients with AS complicated with SS (81.8%)and simple SS patients (84.89%).The anti-SSA antibodies were positive in 8cases;the anti-SSB antibodies were positive in 6cases;the minor salivary gland biopsy was positive in 11cases.The levels of CRP,ESR,and immunoglobulin of the patients with AS complicated with SS were higher than those of AS patients or SS patients,but the differences were not significant(P>0.05).Compared with AS patients,the incidence of hyperglobulinemia in patients with AS complicated with SS was increased (P<0.05).ConclusionAS and SS can occur at the same time,and the patients with AS complicated with SS are prefer to peripheral joint involvement.
ankylosing spondylitis;Sjogren’s syndrome;antinuclear antibody;immunoglobulin
R593.23
A
1671-587Ⅹ(2012)06-1183-04
2012-05-24
辽宁省科技厅科学计划项目资助课题 (2011225015);辽宁省医学高峰建设工程重点科研项目资助课题(200931)
常利华 (1982-),男,辽宁省阜新市人,医师,医学硕士,主要从事风湿病的临床研究。
王晓非 (Tel:024-96615-1-27111,E-mail:vincentclh@126.com)
