Long-Term Chinese Herbs Decoction Administration for Management of Hot Flashes Associated with Endocrine Therapy in Breast Cancer Patients
2011-07-10DongXueHongSunPingpingLi
Dong Xue, Hong Sun, Ping-ping Li
Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education), Department of Integrative Medicine, Peking University School of Oncology, Beijing Cancer Hospital & Institute, Beijing 100142, China
Long-Term Chinese Herbs Decoction Administration for Management of Hot Flashes Associated with Endocrine Therapy in Breast Cancer Patients
Dong Xue, Hong Sun, Ping-ping Li*
Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education), Department of Integrative Medicine, Peking University School of Oncology, Beijing Cancer Hospital & Institute, Beijing 100142, China
Objective:To evaluate the effect of Chinese herbs decoctionShu-Gan-Liang-Xueon endocrine therapyassociated hot flashes symptom in breast cancer patients.
Methods:Sixty-six patients with breast cancer receiving adjuvant endocrine therapy were categorized to two groups, the control group received endocrine therapy alone, the other group is administered with Chinese herbs decoctionShu-Gan-Liang-Xuebesides the endocrine therapy:Shu-Gan-Liang-Xuedecoction was administered above 6 months per year for more than 2 years. Frequency of hot flashes per day was recorded, and the effect ofShu-Gan-Liang-Xuedecoction on hot flashes symptom being assessed with Kupperman Scoring Index.
Results:Sixty cases were analyzed, 32 cases in endocrine therapy combining Chinese herbs decoction group, 28 cases in mere endocrine therapy group. For hot flashes symptom, in Chinese herbs decoction administration group, 7 cases (21.9%) reported symptom disappeared, 22 cases (68.7%) reported symptom alleviated, 3 cases (9.4%) reported symptom not changed; in endocrine therapy alone group, 5 cases (17.9%) reported symptom disappeared, 13 cases (46.4%) reported symptom alleviated, 10 cases (10/28, 35.7%) reported symptom not changed. The difference between two groups was statistically significant (P=0.013). For sleeping disorder, in Chinese herbs decoction administration group, 27 cases (84.4%) reported symptom improved, 5 cases (15.6%) reported no change; in endocrine therapy alone group, 16 cases (57.1%) symptom improved, 12 cases (42.9%) reported no change in sleeping disorder (P=0.019),the difference was also ofsignificance statistically.
Conclusion:Long-term Chinese herbs decoction administration remarkably improved hot flashes symptom and sleeping disorder associated with endocrine therapy, meanwhile without definite toxicity and influence on the risk of recurrence of tumor.
Breast cancer; Endocrine therapy; Tamoxifen; Hot flashes; Chinese herbs decoction
INTRODUCTION
Breast cancer is the most common malignancy and is the second only to lung cancer as a cause of cancer death in United States[1]. In China, breast cancer is the leading cancer with increasing morbidity in urban female population. In accordance with NCCN guidelines patients with invasive breast cancers that are estrogen receptor (ER) or progesterone receptor (PR) positive should be considered for adjuvant endocrine therapy regardless of patient age, lymph node status or whether or not being administered adjuvant chemotherapy[2]. Tamoxifen is the most firmly established adjuvant endocrine therapy for both premenopausal and postmenopausal women, and a number of studies have also evaluated aromatase inhibitors in the 111treatment of postmenopausal patients with early breast cancer. Tamoxifen and aromatase inhibitors have different side effect profiles, but they both contribute to hot flashes[3]. Hot flashes is one of the most common and distressing symptoms of breast cancer patients, approximately 75% of postmenopausal women who had breast cancer report experiencing hot flashes[4]. Compared with menopausal women without breast cancer, breast cancer survivors had hot flashes that were significantly more frequent, severe, distressing, and of longer duration. Breast cancer survivors were less likely to use hormone replacement and more likely to have tried nonhormonal prescription interventions in the past, but reported significantly less effectiveness from hot flashes treatments. Breast cancer survivors with severe hot flashes reported significantly greater mood disturbance; higher negative affect; more interference with daily activities including sleep, concentration, sexuality and poorer overall quality of life compared with survivors with no hot flashes to mild hot flashes[5]. In Asia[6,7], hot flashes is still adistressing and bothersome symptom in breast cancer patients, seriously impaired quality of life of breast cancer patients. In consideration of the hormone dependent feature of breast cancer, hormone replacement therapy for menopausal women with breast caner is not withheld, some other pharmacological and non-pharmacological approaches are widely under study. Chinese herbs decoction for management of endocrine therapy-associated hot flashes is characteristic of Traditional Chinese Medicine (TCM).
This article describes the effect of Chinese herbs decoctionShu-Gan-Liang-Xuefor management of endocrine therapy-associated hot flashes and sleeping disorders.
MATERIALS AND METHODS
Clinic Data and Treatment
From October 2004 through November 2010, 66 patients with pathologically confirmed, ER and/or PR positive breast cancer and discomfort complaint including hot flashes were treated at Peking University Cancer Hospital and Institute.
Sixty-six patients selected one of the following therapy regimen based on their own willingness: one group receiving endocrine therapy alone, the other group being administered with Chinese herbs decoctionShu-Gan-Liang-Xuebesides the endocrine therapy. All the participants were administered tamoxifen at preliminary period and complained hot flashes symptom. During the following 4-5 years, according to updated NCCN guidelines about adjuvant endocrine therapy, some participants’prescription were switched from tamoxifen to aromatase inhibitor.
The Shu-Gan-Liang-Xue decoction is composed of the following herbs: radix bupleurt, radix paeoniae alba, schisandra chinensis, peony Bark, radix cynanchi atrati, lithospermum erythrorhizon, which is a compound decoction originated from TCM classics and modified with clinical experience as fixed herbal component. The decoction was administered orally twice one day, morning and evening before meal above 6 months per year and persisted administration more than 2 years. The institutional review boards (IRB) at the School of Oncology, Peking University, Beijing approved this study.
Follow up
We designed case report form (CRF) to collect information including all the medical records. We called each patient by telephone and asked for telephone interview with patient personally, with patients’ permission, we inquired their hot flashes symptom and sleeping disorder status. For subjects who couldn’t be reached at first phone call we double checked the contact information registered in medical records and previous trial, and called 3 times at different time of the workday and weekend to reach them.
Effectiveness Evaluation
We record the frequency of hot flashes per day and with the widely recognized and implemented Kupperman Scoring Index[8,9]to rank hot flashes symptom as mild symptom (frequency of hot flashes lower than 5 times per day), severe symptom (frequency of hot flashes more than 5 times per day).
To compare the Kupperman Index obtained before and after treatment, hot flashes were classified as symptom no change, symptom alleviated (severe to mild) and symptom disappeared (severe or mild to no symptom).
Sleeping disorder was evaluated with 0-10 visual analogue scale, 0 score means no sleeping disorder, 10 score means the most severity patient can imagine, 1-3 sore is mild, 4-6 score is middle, 7-10 score is severe, middle and severe symptom are defined as sleeping disorder. Sleeping disorder was classified as no change and improved (from severe, middle to mild or no symptom).
Statistical Analysis
Statistical analysis was performed with SPSS 13.0 statistics software (Chicago, IL, USA). Sleeping disorder between groups was analyzed with chi-square tests, change of hot flashes symptom between two groups was analyzed with Wilcoxon tests. A P value of less than 0.05 was considered statistically significant.
RESULTS

Table 1.Baseline of hot flashes and sleeping disorder symptoms in two groups
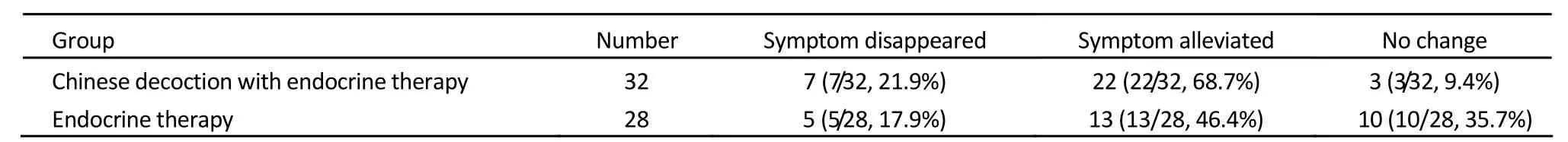
Table 2.Change of hot flashes symptom in two groups*

Table 3.Change of sleeping disorder in two groups*
Among 60 patients who completed clinical survey, 3 (5%) reported experiencing a recurrence of breast cancer either in the breast (n=2) or in a distant site (n=1), of them 1 patient is in the long-term Chinese herbs decoction administration group. No evidence showed the correlation of Chinese herbs decoction administration and cancer recurrence.
DISCUSSION
In this clinical study, we focus on the common and distressing hot flashes symptom in breast cancer patients. For some patients without good control and management of this symptom, the routine procedure of endocrine therapy might be hampered. Poor adherence to medication and incomplete understanding of the benefits and side effects of regular administration, cancer relapse and recurrence will happen[10,11]. So, good control of hot flashes symptom is guarantee of patients’ adherence to endocrine therapy which is a high beneficial choice for breast cancer patients. Acute tryptophan depletion[12]and CYP2D6 genotype[13]are involved in the mechanism of hot flashes. The severity and frequency of hot flashes may be an independent predictor of tamoxifen efficacy, in one clinical study[14], women who reported hot flashes at baseline were less likely to develop recurrent breast cancer than those who did not report hot flashes (12.9% vs. 21%,P=0.01). Hot flashes were a stronger predictor of breast cancer specific outcome than age, hormone receptor status, or even the difference in the stage of the cancer at diagnosis (Stage I versus Stage II).
Treatments for hot flashes symptom in breast cancer patients were classified into pharmacological and nonpharmacological approaches[15,16]. With the understanding of hot flashes mechanism, pharmacological agent includes Selective serotonin-reuptake inhibitors (SSRIs) and antidepressant drugs, recommendations by guidelines of National Comprehensive Cancer Network, venlafaxine and some other SSRIs are effective interventions in deceasing hot flashes[17,18], but recent evidence has suggested contaminant use of tamoxifen with certain SSRIs may decrease plasma levels of endoxifen, an active metabolite of tamoxifen, so the pharmacokinetics of tamoxifen maybe interfered[19,20]the interrelation should be considered[21]. Long term hormonal replacement therapy in breast cancer patients is regarded as contradictions[22]for long periods, but with results of two independent randomized clinical trials, the association of risk of breast cancer recurrence and menopausal hormone therapy was still questioned, limited by the significant heterogeneity between two studies, the final conclusion need further discussion[23]. In one clinical trial, long term use (up to 3 years or longer) of low dose megestrol acetate (< or =20 mg of megestrol acetate per day) showed continued control of hot flashes and well tolerated[24]. Venlafaxine has been the research hotspot for alleviating hot flashes in breast cancer patients, in several clinical trials[20,25,26], different doses and timing of venlafaxine were administered, it showed effect in alleviating hot flashes, but for long term administration, limited by its side effects, some patients dropped out. According to the results of one open-label crossover study[27]newly published in JCO, breast cancer survivors prefer venlafaxine over gabapentin for the treatment of hot flashes. Venlafaxine was associated with increased nausea, appetite loss, constipation, and reduced negative mood changes compared with gabapentin, whereas gabapentin was associated with increased dizziness and appetite compared with venlafaxine (allP<0.05). Besides the above chemical drugs with definite molecular structure, several complementary and alternative medicines frequently used by patients have also been studied[15], including soy isoflavones[28,29], black cohosh[30]and some other compound decoctions, behavior strategy including hypnosis[31], dietary pattern[32,33], patients education, relaxation exercise and acupuncture[34,35]. Although in many randomized or placebo controlled trials, the complementary interventions didn’t show significant effect compared with placebo, they played an important role in hot flashes symptom control and showed a promising prospect. To support the use of one of more of these herbal drugs in the treatment of hot flashes in breast cancer patients, more evidence from well-controlled clinical trials is needed.
In china, TCM is an alternative approach for management of hot flashes. Most studies are carried out inmenopausal women, few studies focus on hot flashes associated with endocrine therapy in breast cancer patients. Based on the characteristic of pattern differentiation theory in TCM, different patterns are diagnosed and different decoctions are prescribed, the result of trial is difficult to duplicate and disseminate. Some of the decoctions for alleviating hot flashes symptom involve herbs that containing phytoestrogen, whether it will interact with tamoxifen and impact on the effect of endocrine therapy like some SSRIs is still controversial and under discussion.
ForShu-Gan-Liang-Xuedecoction of this study, with the results in previous research, this decoction is safein vivoand vitro experiments without side effects and toxicities[36-38]. In our clinical study, it proved this point, no apparent liver and kidney toxicities associated with long term Chinese herbs decoction administration, no definite correlation between cancer relapse and Chinese herbs decoction administration in that recurrent case, but limited by sample size of enrolled patients, larger and randomized controlled clinical study is needed. The instrument used to assess hot flashes symptom is Kupperman Index, which was the first widely accepted attempt to measure the severity of menopausal complaints in women[8,9]. This instrument focuses primarily on symptomatic relief, assessed on the basis of the physician's summary of the severity of the climacteric complaints, and it’s easy to put into clinical practice. In current studies daily diary recording hot flashes and questionnaires[5,20,39]of health related quality of life are implemented to assess hot flashes symptom, with these questionnaires, besides hot flashes symptom, more information about quality of life of breast cancer survivors is collected and focused. Either original Kupperman index or complicated QOL questionnaires[27], they are in the category of subjective measurement. One randomized clinical trial compared subjective and objective hot flash measures[40]among breast cancer survivors initiating aromatase inhibitor therapy. A sternal skin conductance monitor was used in trial to provide objective measure of hot flashes; findings indicated dissimilarities between subjective and objective measures of hot flashes. Despite statistical significance, there was little clinically meaningful change in hot flashes after initiating aromatase inhibitor therapy. To question the conventional measurement of the subjective hot flashes symptom, it’s a meaningful and thought-provoking attempt.
Long term follow up for breast cancer survivors after primary treatment including endocrine therapy is feasible and acceptable to patients; breast cancer patients with hot flashes express their interest in learning more regarding more strategies for hot flashes symptom control and improvement of quality of life[41-43]. In this clinical study, combined with endocrine therapy, long-term Chinese herbs decoction administration achieved a remarkable effect on improving hot flashes symptom and sleeping disorder associated with endocrine therapy without definite toxicity and influence on the recurrence risk of breast cancer patients. Limited by the sample size, this study could not provide high class evidence for the evaluation of the role of TCM in breast cancer treatment, whether it should be used for special symptom control or general rehabilitation or prevention for cancer relapse, and if so, for how long time administration should be recommended, it is still a controversial topic, especially to some oncologists received systematic west medicine education. We reported the experience of our institution to evoke further discussion about the practice of TCM in cancer treatment.
REFERENCES
1. Jemal A, Siegel R, Xu J, et al. Cancer statistics, 2010. CA Cancer J Clin 2010; 60:277-300.
2. The NCCN Clinical Practice Guidelines in Oncology (NCCN GuidelinesTM) Breast Cancer (Version 2.2010). ©2010 National Comprehensive Cancer Network, Inc. Available from: NCCN.org. Accessed December 1st 2010.
3. Early Breast Cancer Trialists' Collaborative Group. Tamoxifen for early breast cancer: an overview of the randomised trials. Lancet 1998; 351:1451-67.
4. Chang YC, Parker J, Dooley WC. Hot flash therapies in breast cancer survivors. Support Cancer Ther 2006; 4:38-48.
5. Carpenter JS, Johnson D, Wagner L, et al. Hot flashes and related outcomes in breast cancer survivors and matched comparison women. Oncol Nurs Forum 2002; 29:E16-25.
6. Ashraf M, Biswas J, Majumdar S, et al. Tamoxifen use in Indian women--adverse effects revisited. Asian Pac J Cancer Prev 2009; 10:609-12.
7. Dorjgochoo T, Gu K, Kallianpur A, et al. Menopausal symptoms among breast cancer patients 6 months after diagnosis: a report from the Shanghai Breast Cancer Survival Study. Menopause 2009; 16:1205-12.
8. Kupperman HS, Blatt MHG, Wiesbader H, et al. Comparative clinical evaluation of estrogenic preparations by the menopausal and amenorrheal indices. J Clin Endocrinol 1953; 13:688-703.
9. Kupperman HS, Wetchler BB, Blatt MH. Contemporary therapy of the menopausal syndrome. J Am Med Assoc 1959; 171:1627-37.
10. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med 2005; 353:487-97.
11. Zhang PY. Cessation administration of Tamxifen in breast cancer patients and analysis of TCM effect. Chin J Integrat Surg (in Chinese) 2005; 11:493-4.
12. Carpenter JS, Yu M, Wu J, et al. Evaluating the role of serotonin in hot flashes after breast cancer using acute tryptophan depletion. Menopause 2009; 16:644-52.
13. Henry NL, Rae JM, Li L, et al. Association between CYP2D6 genotype and tamoxifen-induced hot flashes in a prospective cohort. Breast Cancer Res Treat. 2009; 117:571-5.
14. Mortimer JE, Flatt SW, Parker BA, et al. Tamoxifen, hot flashes and recurrence in breast cancer. Breast Cancer Res Treat 2008; 108:421-6.
15. Kligman L, Younus J. Management of hot flashes in women with breast cancer. Curr Oncol 2010; 17:81-6.
16. Hickey M, Saunders C, Partridge A, et al. Practical clinical guidelines for assessing and managing menopausal symptoms after breast cancer. Ann Oncol 2008; 19:1669-80.
17. Loprinzi CL, Kugler JW, Sloan JA, et al. Venlafaxine in management of hot flashes in survivors of breast cancer: a randomised controlled trial. Lancet 2000; 356:2059-63.
18. Loibl S, Schwedler K, von Minckwitz G, et al. Venlafaxine is superior to clonidine as treatment of hot flashes in breast cancer patients--a double-blind, randomized study. Ann Oncol 2007; 18:689-93.
19. Garber K. Tamoxifen pharmacogenetics moves closer to reality. J Natl Cancer Inst 2005; 97:412-3.
20. Jin Y, Desta Z, Stearns V, et al. CYP2D6 genotype, antidepressant use, and tamoxifen metabolism during adjuvant breast cancer treatment. J Natl Cancer Inst 2005; 97:30-9.
21. Brauch H, Mürdter TE, Eichelbaum M, et al. Pharmacogenomics of tamoxifen therapy. Clin Chem 2009; 55:1770-82.
22. Debourdeau P, Bachelot T, Zammit C, et al. Treatment of hot flashes in women with a previous diagnosis of breast cancer. Bull Cancer. 2004;91:339-49.
23. von Schoultz E, Rutqvist LE, Stockholm Breast Cancer Study Group. Menopausal hormone therapy after breast cancer: the Stockholm randomized trial. J Natl Cancer Inst 2005; 97:533-5.
24. Quella SK, Loprinzi CL, Sloan JA, et al. Long term use of megestrol acetate by cancer survivors for the treatment of hot flashes. Cancer 1998; 82:1784-8.
25. Carpenter JS, Storniolo AM, Johns S, et al. Randomized, double-blind, placebo-controlled crossover trials of venlafaxine for hot flashes after breast cancer. Oncologist 2007; 12:124-35.
26. van Gool AR, Bannink M, Bontenbal M, et al. Clinical experience with venlafaxine in the treatment of hot flushes in women with a history of breast cancer. Neth J Med 2005; 63:175-8.
27. Bordeleau L, Pritchard KI, Loprinzi CL, et al. Multicenter, randomized, cross-over clinical trial of venlafaxine versus gabapentin for the management of hot flashes in breast cancer survivors. J Clin Oncol 2010; 28:5147-52.
28. Van Patten CL, Olivotto IA, Chambers GK, et al. Effect of soy phytoestrogens on hot flashes in postmenopausal women with breast cancer: a randomized, controlled clinical trial. J Clin Oncol 2002; 20:1449-55.
29. MacGregor CA, Canney PA, Patterson G, et al. A randomized double-blind controlled trial of oral soy supplements versus placebo for treatment of menopausal symptoms in patients with early breast cancer. Eur J Cancer 2005; 41:708-14.
30. Jacobson JS, Troxel AB, Evans J, et al. Randomized trial of black cohosh for the treatment of hot flashes among women with a history of breast cancer. J Clin Oncol 2001; 19:2739-45.
31. Elkins G, Marcus J, Stearns V, et al. Randomized trial of a hypnosis intervention for treatment of hot flashes among breast cancer survivors. J Clin Oncol 2008; 26:5022-6.
32. Pierce JP, Natarajan L, Caan BJ, et al. Dietary change and reduced breast cancer events among women without hot flashes after treatment of early-stage breast cancer: subgroup analysis of the Women's Healthy Eating and Living Study. Am J Clin Nutr 2009; 89:1565S-71S.
33. Gold EB, Pierce JP, Natarajan L, et al. Dietary pattern influences breast cancer prognosis in women without hot flashes: the women's healthy eating and living trial. J Clin Oncol 2009; 27:352-9.
34. Filshie J, Bolton T, Browne D, et al. Acupuncture and self acupuncture for long-term treatment of vasomotor symptoms in cancer patients--audit and treatment algorithm. Acupunct Med 2005; 23:171-80.
35. Nedstrand E, Wijma K, Wyon Y, et al. Vasomotor symptoms decrease in women with breast cancer randomized to treatment with applied relaxation or electro-acupuncture: a preliminary study. Climacteric 2005; 8:243-50.
36. Sun H, Li PP, Xie YT. Impact of Shu Gan Liang Xue decoction combined with tamoxifen on the growth and estrogen receptor expression in human breast cancer cell line MCF-7. China Cancer (in Chinese) 2005; 14:607-10.
37. Sun Y, Li PP. The Shuganliangxue decoction’s effects on the metabolism of tamoxifen. Chin J Exp Tradition Med Formul (in Chinese) 2009; 15:76-9.
38. Sun Hong, Xue Dong, Gao Fei, et al. Effect of shugan liangxue compund for relieving hot flashes in breast cancer patients. Zhongguo Zhong Xi Yi Jie He Za Zhi (in Chinese) 2009; 29:30-3.
39. Loprinzi CL, Zahasky KM, Sloan JA, et al. Tamoxifen-induced hot flashes. Clin Breast Cancer 2000; 1:52-6.
40. Otte JL, Flockhart D, Hayes D, et al. Comparison of subjective and objective hot flash measures over time among breast cancer survivors initiating aromatase inhibitor therapy. Menopause 2009; 16:653-9.
41. Ganz PA, Desmond KA, Leedham B, et al. Quality of life in long-term, disease-free survivors of breast cancer: a follow-up study. J Natl Cancer Inst 2002; 94:39-49.
42. Ganz PA, Greendale GA, Petersen L, et al. Managing menopausal symptoms in breast cancer survivors: results of a randomized controlled trial. J Natl Cancer Inst 2000; 92:1054-64.
43. Carpenter JS, Andrykowski MA, Cordova M, et al. Hot flashes in postmenopausal women treated for breast carcinoma: prevalence, severity, correlates, management, and relation to quality of life. Cancer 1998; 82:1682-91.
10.1007/s11670-011-0074-7
ases
treatment, 60 cases who met the study eligibility with detailed clinical medical record were included in our study, 6 cases were lost of follow up. Baseline demographic and disease-related characteristicsof the 60 cases in the follow-up study are shown in Table 1. Combined with routine endocrine therapy, 32 patients have accomplished long-term ChineseShu-Gan-Liang-Xuedecoction administration, 28 patients have only taken endocrine agent. The response of hot flashes symptom in two groups is shown in Table 2. Hot flashes could be controlled considerably in Chinese herbs decoction administration group, 7 cases (7/32, 21.9%) reported symptom disappeared, 22 cases (22/32, 68.7%) reported symptom alleviated, 3 cases (3/32, 9.4%) reported no change; in merely endocrine therapy group, 5 cases (5/28, 17.9%) reported symptom disappeared, 13 cases (13/28, 46.4%) reported symptom alleviated, 10 cases (10/28, 35.7%) reported no change. Difference between two groups showed significant difference (P=0.013). The change of sleeping disorder is shown in Table 3, in Chinese herbs decoction administration group, 27 cases (27/32, 84.4%) symptom improved, 5 cases (5/32, 15.6%) reported no change in sleeping disorder; in merely endocrine therapy group, 16 cases (16/28, 57.1%) symptom improved, 12 cases (12/28, 42.9%) reported no change in sleeping disorder. The difference showed significant difference (P=0.019).
Received2010−05−27;Accepted2010−12−14
*Corresponding author.
E-mail: lppma123@yahoo.com.cn
© Chinese Anti-Cancer Association and Springer-Verlag Berlin Heidelberg 2011
杂志排行
Chinese Journal of Cancer Research的其它文章
- Incidence And Mortality Trend of Cervical Cancer in 11 Cancer Registries of China
- Reversion of Multidrug-Resistance by Proteasome Inhibitor Bortezomib in K562/DNR Cell Line
- Elevated Circulating Levels of Osteopontin Are Associated with Metastasis in Advanced Non-Small Cell Lung Cancer
- Correlation Between Hyaluronic Acid,Hyaluronic Acid Synthase And Human Renal Clear Cell Carcinoma
- Validation And Reliability of Distress Thermometer in Chinese Cancer Patients
- Mobilization of Peripheral Blood Stem Cells Using Regimen Combining Docetaxel with Granulocyte Colony-stimulating Factor in Breast Cancer Patients