Prevalence of HPV Infection And Cervical Intraepithelial Neoplasia And Attitudes towards HPV Vaccination among Chinese Women Aged 18-25 in Jiangsu Province
2011-07-10ShangyingHuYingHongFanghuiZhaoAdamLewkowitzFengChenWenhuaZhangQinjingPanXunZhangCindyFeiHuiLiYoulinQiao
Shang-ying Hu, Ying Hong, Fang-hui Zhao*, Adam K. Lewkowitz, Feng Chen, Wen-hua Zhang, Qin-jing Pan, Xun Zhang, Cindy Fei, Hui Li You-lin Qiao
1Department of Epidemiology & Biostatistics, Institute of Basic Medical Sciences, Chinese Academy of Medical Sciences; School of Basic Medicine, Peking Union Medical College, Beijing 100730, China
2Department of Cancer Epidemiology,3Department of Gynecological Oncology,4Department of Pathology, Cancer Institute/Hospital, Chinese Academy of Medical Sciences; Peking Union Medical College, Beijing 100021, China
5Department of Gynecology and Obstetrics, Affiliated Drum Tower Hospital, Nanjing University Medical School, Nanjing 210008, China
6Mount Sinai School of Medicine, New York City, New York, USA
7New York University School of Medicine, New York City, New York, USA
Prevalence of HPV Infection And Cervical Intraepithelial Neoplasia And Attitudes towards HPV Vaccination among Chinese Women Aged 18-25 in Jiangsu Province
Shang-ying Hu1,2, Ying Hong5, Fang-hui Zhao2*, Adam K. Lewkowitz6, Feng Chen2, Wen-hua Zhang3, Qin-jing Pan4, Xun Zhang4, Cindy Fei7, Hui Li1, You-lin Qiao2
1Department of Epidemiology & Biostatistics, Institute of Basic Medical Sciences, Chinese Academy of Medical Sciences; School of Basic Medicine, Peking Union Medical College, Beijing 100730, China
2Department of Cancer Epidemiology,3Department of Gynecological Oncology,4Department of Pathology, Cancer Institute/Hospital, Chinese Academy of Medical Sciences; Peking Union Medical College, Beijing 100021, China
5Department of Gynecology and Obstetrics, Affiliated Drum Tower Hospital, Nanjing University Medical School, Nanjing 210008, China
6Mount Sinai School of Medicine, New York City, New York, USA
7New York University School of Medicine, New York City, New York, USA
Objective:Few data are available on the epidemiology of HPV and cervical cancer among Chinese women younger than 25 years old. This study aimed to estimate the HPV infection rate and the prevalence of cervical intraepithelial neoplasia (CIN) in women aged 18-25, as well as their knowledge of and attitudes towards HPV vaccination.
Methods:A population-based cervical cancer screening study was conducted on women aged 18-25 in Jiangsu province in 2008. Participants provided socio-demographic, reproductive and behavioral information and completed a survey about their knowledge of and attitudes towards HPV vaccination. Women then underwent a gynecologic exam to provide two cervical exfoliated cell samples for high risk HPV DNA testing and liquid-based cytology (LBC) as well as visual inspection with acetic acid (VIA). Women testing positive for any test were referred to colposcopy and biopsy. The gold standard for diagnosis of cervical lesions was directed or random biopsies.
Results:Within the sample of 316 women, 3.4% of them were diagnosed with CIN grade 2 or worse lesions and 17.1% were found to be positive for HPV DNA. Among these young women, extra-marital sexual behavior of them (OR=2.0, 95%CI: 1.1-3.8) or their husbands (OR=2.6, 95%: 1.4-4.7) were associated with an increased risk of HPV positivity. Although overall HPV awareness was low, after a brief educational intervention, 98.4% reported they would electively receive HPV vaccination and would also recommend that their daughters be vaccinated. However, most urban and rural women reported their ideal maximum out-of-pocket contribution for HPV vaccination to be less than 500 RMB and 50-100 RMB, respectively.
Conclusion:Our study indicates cervical disease burden is relatively high among sampled Chinese women aged 18-25. Appropriate educational interventions for female adolescents and strategies to subsidize vaccine costs are definitely needed to ensure the effectiveness of vaccination campaigns in China.
Cervical cancer; Cervical intraepithelial neoplasia; Human papillomavirus; Knowledge; Attitude
INTRODUCTION
Cervical cancer is the second most common cancer among women worldwide, with an estimated 88% of the annual incidence occurring in developing countries[1]. The People’s Republic of China accounts for 14% of the world’s annual incidence of cervical cancer (75,500 new cases) and 12% of the world’s annual mortality from cervical cancer 1111(34,000 deaths)[1]. The etiology of cervical cancer, and precancerous cervical intraepithelial neoplasia (CIN) has been clearly established as high-risk human papillomavirus (HPV)[2,3]. Multiple studies have demonstrated that the prevalence of CIN and HPV infection varies by age[4-6]. Though several population-based screening studies reported the prevalence of HPV infection and CIN in China[7-13], most studies focused on women older than 30 or 35. Very few data exist describing HPV and CIN prevalence among Chinese women younger than 25 years old.
The well-established etiology of cervical cancer has allowed for the development of HPV vaccines as primarycervical cancer prevention methods. Currently, two prophylactic HPV vaccines are commercially available, Gardasil (Merck & Co., USA) and Cervarix (GlaxoSmith-Kline, Belgium). Both vaccines target HPV-16 and -18, which cause 70.1% of invasive cervical cancers worldwide[14-16]. The Gardasil vaccine additionally targets HPV-6 and -11, responsible for about 83% of genital warts[17]. These HPV vaccines are heralded to be promising methods to decrease HPV infection and cervical cancer incidence and have been widely utilized in many developed countries. However, in order to achieve significant reduction in worldwide cervical cancer incidence, the HPV vaccine must be introduced in low-resource countries as well. Both vaccine companies are currently conducting clinical trials in China and preparing to apply for approval from State Food and Drug Administration. To assess the potential impact HPV vaccines may have in China, it is imperative to determine the burden of HPV infection and cervical disease in young Chinese women.
To address this gap in knowledge, we conducted a population-based cervical cancer screening study examining 316 women aged 18-25 in Jiangsu Province from June to August, 2008. Our study aimed to estimate the CIN prevalence and HPV infection rate by cytology and histology in this population. In addition, we conducted quantitative surveys to determine participants’ knowledge of and attitudes towards HPV infection, cervical cancer, and HPV vaccination in order to determine major obstacles facing future vaccination campaigns in China.
MATERIALS AND METHODS
Study Subjects
This population-based cross-sectional study targeted the female population aged 18-25 in Jiangsu Province, China, using a cluster sampling design with the commune as the unit of cluster. Research was conducted at three investigational sites: one rural site (Binhai County), one suburban site (Jintan County), and one urban site (Xuzhou City). Eligible women were mentally and physically competent, sexually active, not pregnant, with an intact uterus and had no history of CIN, cervical cancer, or pelvic radiation. Menstruating women were excluded until menstruation finished. All women provided written informed consent. This study was approved by the Institutional Review Board of the Cancer Foundation of China.
Study Procedure
Local health workers recruited women via door-to-door solicitation. All eligible women were invited to participate in the study at the local clinic. At the initial research visit, women were informed about the study’s risks and benefits, research procedures, and confidentiality assurance, and those who agreed to participate then provided written informed consent. Prior to the clinical examination, trained health-care workers reassessed participants to ensure eligibility before asking them in a private setting about socio-demographic, reproductive and behavioral information. Participants then completed a survey about HPV infection and attitudes to HPV vaccination.
After the interviewer-administered questionnaire, a gynecological examination was conducted to collect two vials of exfoliated cervical cell samples for liquid-based cytology (LBC) (ThinPrep®, Hologic, Bedford, MA, USA) and high-risk HPV DNA testing before conducting visual inspection with acetic acid (VIA). Women who were VIA positive or suspicious for cancer (SFC) received colposcopy (Goldway, Shenzhen China) with directed biopsies. Women were called back for colposcopy two weeks after the initial visit if they had negative VIA but positive HPV DNA test or cytology results of atypical squamous cells-cannot exclude high-grade squamous intraepithelial lesion (ASC-H) or low-grade squamous intraepithelial lesion and worse (LSIL+). Directed biopsies were taken for women with positive HPV and negative or atypical squamous cells of undetermined significance (ASC-US) on cytology if colposcopy findings were abnormal. Directed and random biopsies were both done for the women with ASC-H or LSIL+ on cytology (For abnormal quadrants, the most abnormal areas received directed biopsy. For normal quadrants, random biopsies of the squamo-columnar junction (SCJ) were taken at two, four, eight and ten o’clock)[7]. If the SCJ could not be visualized with colposcopy, endocervical curettage (ECC) was performed. Patients with CIN grade 2 or worse (CIN2+) lesions were treated according to local medical standards.
Oncogenic HPV DNA Testing
Carcinogenic HPV DNA testing was performed using the high-risk probe set of Hybrid Capture 2 (HC2, Qiagen Inc., Gaithersburg, MD, USA), which detects 13 carcinogenic HPV types (HPV 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59 and 68). The HC2 sampling device was placed in preservative solution, stored at room temperature, and transported to the HPV lab at the Cancer Institute, Chinese Academy of Medical Sciences (CICAMS), where certified technicians performed the HC2 test. Results were expressed in relative light units (RLU) and compared with the mean RLU from a minimum positive control set at 1.0 pg/mL. Samples ≥1.0 were positive, and <1.0 were negative.
Cytology Diagnosis
The cytology sampling device was placed in PreservCyt liquid-based cytology preservative medium, stored at room temperature, and transported to CICAMS, where processing, staining and classification was performed according to the Bethesda system[18]. Samples were read as being within normal limits (negative), ASC-US, atypical glandular cells of uncertain significance (AGC), ASC-H, LSIL, high-grade squamous intraepithelial lesion (HSIL), squamous cell carcinoma (SCC), adenocarcinoma in situ (AIS), or adenocarcinoma (ADC). A junior cytopathologist diagnosed all slides before a senior cytopathologist reviewed them forquality control, confirming the diagnosis of the junior cytologist. If there was disagreement between the two cytopathologists, the senior cytopathologist’s diagnosis was final.
Biopsy Diagnosis
Biopsy samples were processed via paraffin-embedding, sectioning, and staining before being read by CICAMS pathologists. CIN nomenclature was used to categorize histological findings: negative, CIN grade 1, 2, or 3 (CIN1, CIN2, or CIN3), SCC, AIS, or ADC. All biopsy slides were reviewed by a senior pathologist. If more than one biopsy specimen was taken from one woman, the final diagnosis was based on the highest grade.
The gold standard of cervical abnormalities was biopsy. However, women without biopsy results but negative or ASC-US on cytology and negative for HPV were classified as being true negatives, according to our previous study’s results, which concluded these women had very low risk for high-grade lesions[7]. Women with negative or ASC-US on cytology and positive for HPV, but negative colposcopy, and who had no biopsy, were considered as negative or CIN1 under the assumption that they had low risk for high-grade lesions.
The HC2 test technicians, cytologists and pathologists were blinded to the results of other tests when making diagnoses.
Statistical Analyses
Statistical analyses were carried out to describe the prevalence of CIN by study site, and the prevalence of high-risk HPV by cytological and pathological classification as well as by study site. Unadjusted odd ratio (OR) and corresponding 95% confidence interval (95%CI) of eachfactor were calculated using a univariate logistic regression model for exploring the association between HPV infection and main characteristics. All variables that were significant in the univariate analysis were then entered in an unconditional, multiple logistic regression model to adjust the other variables. The description on the attitudes to HPV vaccine was also performed.

Table 1.Demographic Characteristics of the 316 women screened
Continuous variables were evaluated by calculating their means and standard deviations. The differences between independent groups were estimated by univariate analysis of variance. Categorical data were presented with percentages and examined by chi-square tests. Data were analyzed with the statistical software SAS 9.1 (SAS Institute Inc., Cary, NC, USA).
RESULTS
In total, 316 eligible women were screened from June to August, 2008. Among them, 31.3% (99/316) were from Binhai County (rural), 33.6% (106/316) were from Jintan Country (suburban), and 35.1% (111/316) were from Xuzhou City (urban). Main characteristics of the study subjects are shown in Table 1. The mean age was 23.2 years (SD: 1.7; range: 18-25), with more than half (51.3%, 162/316) between 24 to 25 years old. On average, 47.8% (151/316, range from 14.1% in rural site to 79.3% in urban site) had completed high school. Nearly all (98.7%, 312/316) were non-smokers and the majority 87.3% (276/316) abstained from alcohol. The mean age at first sexual intercourse was 20.2 (SD: 1.9; range: 15-25) years, with no difference between three sites. Nearly all rural women (99.0%, 98/99) were married. Among unmarried participants, urban woman were more likely to engage in sexual behavior (10.8%, 12/111) compared to those in the rural site (χ2=8.34,P=0.02). Over half of urban women (59.5%, 66/111) used condoms for contraception, while 40.4% (40/99) of rural women used intrauterine devices (IUDs). On average, 27.9% (88/316) of participants had more than one sexual partner, and 29.4% (93/316) of women’s husbands had extra-marital sexual relationships. The highest rates of extra-marital sexual activity occurred in suburban populations [32.1% (34/106) in women and 40.6% (43/106) in their husbands].

Table 2.Detection of high-risk human papillomavirus (HPV) according to main demographic characteristics
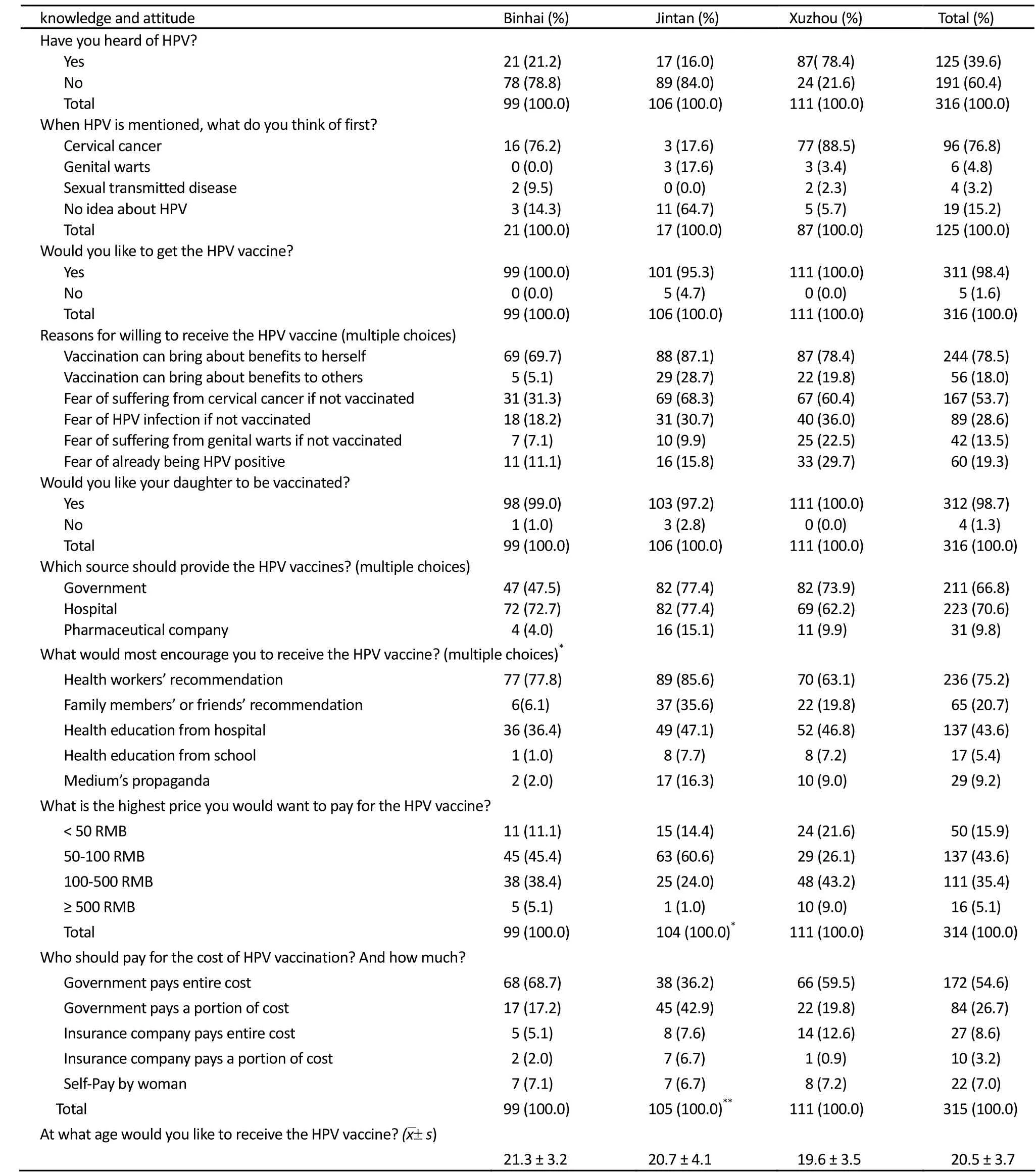
Table 3. 316 women’s knowledge of and attitude towards HPV vaccination
The overall prevalence of high-risk HPV was 17.1% (54/316). The suburban site had the highest HPV prevalence (23.6%, 25/106), followed by the urban (14.4%, 16/111) and rural site (13.1%, 13/99) (χ2=4.81P=0.09). 95.3% of women (301/316) had satisfactory cytology results. Among them, the proportion of negative, ASC-US and the other lesionsworse than ASC-US was 85.4% (257/301), 9.0% (27/301) and 5.6% (17/301), respectively. Abnormal cytology rates were statistically comparable at all three sites (χ2=0.78P=0.68). High-risk HPV occurred in 61.4% (27/44) of women with cytology abnormalities, and in only 10.5% (27/257) of cytologically normal women (χ2=66.01,P<0.0001). Finally, 292 women received biopsy-confirmed or assumed final diagnoses, excluding 24 women who did not follow up with colposcopy (10 with positive HC2, and 14 with negative VIA, negative HC2 but unsatisfactory cytology). 93.5% (273/292) of biopsies were negative, while 3.1% (9/292), 1.7% (5/292), and 1.7% (5/292) were diagnosed as CIN1, CIN2 and CIN3, respectively. Rural (4.3%, 4/92) and suburban sites (4.2%, 4/95) had higher CIN2+ prevalence than the urban site (1.9%, 2/105), but this difference was not statistically significant (χ2=1.15,P=0.56). The HPV prevalence in women with negative histology, CIN 1, CIN 2 and CIN 3 was 10.3% (28/273), 77.8% (7/9), 80.0% (4/5) and 100.0% (5/5), respectively.
Table 2 shows the relationship between HPV infection and some major characteristics. Self-reporting multiple lifetime sexual partners (OR=2.0, 95%CI: 1.1-3.8) and husband’s ex-marital sexual relationships (OR=2.6, 95% CI: 1.4-4.7) were found to increase the risk of HPV infection. Multiple pregnancies (21.4%, 34/159) correlated with a higher rate of HPV positivity than none or only one pregnancy (12.7%, 20/157) (OR=1.9, 95% CI: 1.0-3.4). When the number of sexual partners, husbands’ extra-marital sexual relationships and pregnancies were included in a multiple logistic regression model, the significant OR was the husband’s ex-marital sexual behavior (OR=2.1, 95% CI: 1.1-4.1). Marriage, age of sexual debut, and condom usage were not statistically significant in our sample, though women who were unmarried (27.3%, 6/22), had earlier sexual behavior (≤19 years old) (20.6%, 22/107) or did not use condoms (18.0%, 36/200) for contraception seemed to have higher HPV positive rate. No significant association was found between HPV infection and age, education level, or age at first pregnancy.
Table 3 shows women’s knowledge of and attitudes to HPV and HPV vaccine. In total, only 39.6% of women (125/316) heard of HPV. Compared to suburban (16.0%, 17/106) and rural (21.2%, 21/99) women, more urban women (78.4%, 87/111) knew HPV (χ2=108.43,P<0.0001). Among women who heard of HPV, 76.8% (96/125) knew HPV is related to cervical cancer. After a simple education intervention on HPV infection, HPV related disease and prophylactic HPV vaccine, almost all women (98.4%, 311/316) were willing to be vaccinated, regardless of whether they had originally heard of HPV. The benefits of HPV vaccination (78.5%, 244/311) and fear of getting cervical cancer (53.7%, 167/311) or HPV infection (28.6%, 89/311) were the three most common reasons for electing to receive HPV vaccination. Nearly all women (98.7%, 312/316) reported they would like their daughters to be vaccinated, if they had a daughter. The average age they thought would be appropriate to get vaccinated was 20.5 (SD: 3.7) years old. Hospitals (70.6%, 223/316) and government (66.8%, 211/316) were expected to be the major suppliers for the HPV vaccine, while health workers’ recommendation (75.2%, 236/314) and hospital-based health education (43.6%, 137/314) were the most two acceptable sources for information about HPV vaccination. In terms of HPV vaccine cost, though urban women were willing to pay more (χ2=9.2,P=0.01), 43.6% of women (137/314) were willing to pay 50-100 RMB for vaccination and 35.4% (111/314) would pay 100-500 RMB. More than half (54.6%, 172/315) of the women thought HPV vaccination should be fully government-subsidized, and 26.7% (84/315) thought vaccination cost should be partially government subsidized.
DISCUSSION
Few population-based studies exist describing the epidemiology of HPV and cervical cancer among Chinese women younger than 25 years old as well as their knowledge of HPV and attitudes towards HPV vaccination[7-13]. Our study bridged this gap, demonstrating the high cervical cancer disease burden of sampled Chinese women aged 18-25. Among participants, the overall prevalence of high-risk HPV was 17.1%, with 14.6% of women having abnormal cervical cytology and 3.4% of women diagnosed with CIN2+. Extra-marital sexual behavior of women and their husbands played an important role in HPV positivity among these young women. Overall HPV awareness was low. After a brief educational intervention, most women responded that they would receive HPV vaccination and would also recommend that their daughters be vaccinated. However, the financial cost would be a significant barrier for the vaccination of Chinese women.
Multiple large population-based studies have been published about HPV, CIN, and cervical cancer prevalence in China that indicated the HPV prevalence ranges from 6% in Beijing[13]to 18-23 percent in Shanxi province[7-8]. However, these studies focused on women aged 35 to 50, and those that included women younger than 25 years generally categorize them as a subgroup with sample size ranged from 40 to 56[9-11]. Within our significantly larger population of 316 women, we found a relatively high prevalence (17.1%) of oncogenic HPV among women aged 18-25 in Jiangsu province. Our findings are consistent with those from a recent large population-based multi-center survey of HPV prevalence in China that concluded the prevalence of oncogenic HPV DNA was high in rural and urban Chinese women and peaked among women aged 20-25 and again in women aged 40-45[5], supporting other studies[4,19], including a global meta-analysis[19]. Our data showed that the suburban women had the highest HPV prevalence (23.6%), followed by urban (14.4%) and rural (13.1%) women, supporting a prior study concluding that rural areas in Asia exhibited consistently high HPV prevalence rates independent of age while urban areas in Asia exhibited high prevalence in the women younger than25 years old[4].
In our population of young women, the high HPV prevalence was related to their sexual relationships with multiple partners and their husbands’ extramarital sexual relationships. Our findings agree with those from previous population-based studies associating HPV infection with sexual behavior risk factors[8,9]. The increased salience of sexual risk factors in China, a traditionally conservative culture, may be a result of the behavioral changes stemming from the rapid industrialization and urbanization the country has experienced during the past two decades[21,22]. Considering the relatively high prevalence of HPV infection in young women, the increasing risk of HPV infection, and the continued industrialization of China, the burden of disease related to HPV is likely to increase in the future.
Moreover, this study reported a high prevalence (3.4%) of CIN 2+ lesions among young women in Jiangsu Province. Although our study found no cases of cervical cancer in these young women, the high prevalence of pre-cancerous lesion suggests that there may be a large HPV-related disease burden in young women throughout China. Our reported CIN prevalence was consistent with a previous rate (2.9%) reported in rural Shanxi Province for women aged 30-54[23]. In addition, the high HPV prevalence from our study was significant in light of its enrollment of young women aged 18-25, compared with other studies using a broader age range. Our findings indicate that HPV vaccination is urgently needed in China to reduce the disease burden of HPV infections and prevent Chinese women from developing cervical cancer.
To our knowledge, this study is the largest ever conducted on HPV and cervical intraepithelial neoplasia (CIN) prevalence in Chinese women aged 18-25. Nevertheless, a potential limitation to our study remains for its relatively small population size. We utilized very sensitive screening methods to find the HPV infection or cervical lesion women. As such, our results remain significant in terms of describing the prevalence of HPV and cervical cancer lesions in an understudied research population, Chinese women aged 18-25.
This pilot study also examined the attitudes of young women towards the HPV vaccination. After receiving simple education about HPV infection, HPV-related disease, and prophylactic HPV vaccine, 98.4% of the women reported they would elect to receive the HPV vaccination, agreeing with prior studies in China[24]. However, 94.9% of them reported that they would not contribute more than 500 RMB out-of-pocket for total vaccination costs. There was slight variation of the upper threshold for vaccine payment between rural and urban groups, with 43.2% of urban women selecting 100-500 RMB and 45.4% of rural women selecting 50-100 RMB. Although urban women were willing to pay more for the vaccination, the fact that only 5.1% of women were willing to pay more than 500 RMB for the vaccine suggests that, without government or insurance subsidies, vaccine cost may prohibit HPV vaccine uptake in China, particularly in women from impoverished rural areas. In addition, we found that most Chinese young women trusted the recommendations of health workers, agreeing with a Hong-Kong-based study that concluded women viewed doctors as important sources of information on cervical cancer[25]. This finding indicates the importance of educating health workers about cervical cancer, HPV and HPV vaccine. Our survey also highlights a potential public health programmatic difficulty with HPV vaccination. Women in our study suggested that they were willing to receive HPV vaccination at age 20.5 years, though women self-reported their sexual debut at an average of 20.2 years. Since maximizing the prophylactic potential of the vaccine requires administration before sexual debut, HPV vaccination education in China, which emphasizes the prophylactic nature of the vaccine, must be provided to female Chinese teenagers.
In conclusion, our study reports a relatively high prevalence of HPV and high-grade CIN in young Chinese women, an understudied research population, from Jiangsu Province. In addition to demonstrating the potential cervical cancer burden in sampled young Chinese women, our study highlights some challenges facing primary cervical cancer prevention in China. Though the introduction of the HPV prophylactic vaccine would prevent cervical cancer among Chinese women, to ensure the effectiveness of vaccination campaigns, the Chinese government must first develop appropriate educational interventions for female Chinese adolescents and determine how to subsidize the vaccine costs.
Acknowledgments
The authors wish to thank the local collaborators from Centers for Disease Control and Prevention (CDC) of Jiangsu Province at Xuzhou city, Binhai county and Jintan county and the women who participated in our study in Jiangsu province, as well as GlaxoSmithKline (GSK) Biologicals for their generous support.
REFERENCES
1. Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 2010; 127:2893-917.
2. Bosch FX, Lorincz A, Muñoz N, et al. The causal relation between human papillomavirus and cervical cancer. J Clin Pathol 2002; 55:244-65.
3. Walboomers JM, Jacobs MV, Manos MM, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol 1999; 189:12-9.
4. Franceschi S, Herrero R, Clifford GM, et al. Variations in the age-specific curves of human papillomavirus prevalence in women worldwide. Int J Cancer 2006; 119:2677-84.
5. Qiao YL, Franceschi S, Belinson JL, et al. HPV prevalence in Chinese women: A population-based multiple center survey in mainland China. Oral presentation 1B-01, 24th International Papillomavirus Conference and Clinical Workshop; 2007 Nov 3-9; Beijing, China.
6. Trottier H, Franco EL. The epidemiology of genital human papillomavirus infection. Vaccine 2006; 24(Suppl 1):S1-15.
7. Belinson J, Qiao YL, Pretorius R, et al. Shanxi Province Cervical Cancer Screening Study: a cross-sectional comparative trial of multipletechniques to detect cervical neoplasia. Gynecol Oncol 2001; 83:439-44.
8. Zhao FH, Forman MR, Belinson J, et al. Risk factors for HPV infection and cervical cancer among unscreened women in a high-risk rural area of China. Int J Cancer 2006; 118:442-8.
9. Li LK, Dai M, Clifford GM, et al. Human papillomavirus infection in Shenyang City, People’s Republic of China: A population-based study. Br J Cancer 2006; 95:1593-7.
10. Dai M, Bao YP, Li N, et al. Human papillomavirus infection in Shanxi Province, People’s Republic of China: a population-based study. Br J Cancer 2006; 95:96-101.
11. Shi JF, Wu RF, Liu ZH, et al. Distribution of human papillomavirus types in Shenzhen women. Zhongguo Yi Xue Ke Xue Yuan Xue Bao (in Chinese) 2006; 28:832-6.
12. Zhang X, Wang CY, Shi JF, et al. Study on the prevalence of human papillomavirus infection and distribution of types in Shenyang City. Zhonghua Liu Xing Bing Xue Za Zhi (in Chinese) 2007; 28:954-7.
13. Zhao R, Zhang WY, Wu MH, et al. Human Papillomavirus infection in Beijing, People’s Republic of China: a population-based study. Br J Cancer 2009; 101:1635-40.
14. Clifford GM, Smith JS, Plummer M, et al. Human papillomavirus types in invasive cervical cancer worldwide: a meta-analysis. Br J Cancer 2003; 88:63-73.
15. Muñoz N, Bosch FX, Castellsagué X, et al. Against which human papillomavirus types shall we vaccinate and screen? The international perspective. Int J Cancer 2004; 111:278-85.
16. Smith JS, Lindsay L, Hoots B, et al. Human papillomavirus type distribution in invasive cervical cancer and high-grade cervical lesions: a meta-analysis update. Int J Cancer 2007; 121: 621-32.
17. Wang H, Qiao YL. Human papillomavirus type-distribution in condylomata acuminata of mainland China: a meta-analysis. Int J STD AIDS 2008; 19:680-4.
18. Solomon D, Davey D, Kurman R, et al. The 2001 Bethesda System: terminology for reporting results of cervical cytology. JAMA 2002; 287:2114-9.
19. de Sanjosé S, Diaz M, Castellsagué X, et al. Worldwide prevalence and genotype distribution of cervical human papillomavirus DNA in women with normal cytology: a meta-analysis. Lancet Infect Dis 2007; 7:453-9.
20. Shi JF, Qiao YL, Smith JS, et al. Epidemiology and prevention of human papillomavirus and cervical cancer in China and Mongolia. Vaccine 2008; 26(Suppl12):M53-9.
21. Zhao FH, Hu SY, Zhang SW, et al. Cervical cancer mortality in 2004-2005 and changes during last 30 years in China. Zhonghua Yu Fang Yi Xue Za Zhi (in Chinese) 2010; 44:408-12.
22. Chen XS, Gong XD, Liang GJ, et al. Epidemiologic trends of sexually transmitted diseases in China. Sex Transm Dis 2000; 27:138-42.
23. Qiao YL, Sellors JW, Eder PS, et al. A new HPV-DNA test for cervical-cancer screening in developing regions: a cross-sectional study of clinical accuracy in rural China. Lancet Oncol 2008; 9:929-36.
24. Li J, Li LK, Ma JF, et al. Knowledge and attitudes about human papillomavirus (HPV) and HPV vaccines among women living in metropolitan and rural regions of China. Vaccine 2009; 27:1210-5.
25. Lee PW, Kwan TT, Tam KF, et al. Beliefs about cervical cancer and human papillomavirus (HPV) and acceptability of HPV vaccination among Chinese women in Hong Kong. Prev Med 2007; 45(2-3):130-4.
10.1007/s11670-011-0025-3
2010−11−11;Accepted2010−12−28
*Corresponding author.
E-mail: zhaofangh@cicams.ac.cn
© Chinese Anti-Cancer Association and Springer-Verlag Berlin Heidelberg 2011
杂志排行
Chinese Journal of Cancer Research的其它文章
- Cancer Incidence And Mortality in China, 2006
- Time Trends of Cancer Incidence in Urban Beijing, 1998-2007
- Health Economic Assessment for Screening of Gastric Cancer in A High Risk Population in Northeastern China
- Plasma Vitamin D Levels And Vitamin D Receptor Polymorphisms Are Associated with Survival of Non-small Cell Lung Cancer
- Current Status of Diagnosis And Treatment of Primary Breast Cancer in Beijing, 2008
- Factors Affecting Mesenchymal Stromal Cells Yield from Bone Marrow Aspiration