Comparison of the clinical effects of dual-modality endoscopy and traditional laparotomy for the treatment of intra-and extrahepatic bile duct stones
2024-05-07WeiWangHuiXiaBinDai
Wei Wang,Hui Xia,Bin Dai
Abstract BACKGROUND Bile duct stones (BDSs) may cause patients to develop liver cirrhosis or even liver cancer.Currently,the success rate of surgical treatment for intrahepatic and extrahepatic BDSs is not satisfactory,and there is a risk of postoperative complications.AIM To compare the clinical effects of dual-modality endoscopy (duodenoscopy and laparoscopy) with those of traditional laparotomy in the treatment of intra-and extrahepatic BDSs.METHODS Ninety-five patients with intra-and extrahepatic BDSs who sought medical services at Wuhan No.1 Hospital between August 2019 and May 2023 were selected;45 patients in the control group were treated by traditional laparotomy,and 50 patients in the research group were treated by dual-modality endoscopy.The following factors were collected for analysis: curative effects,safety (incision infection,biliary fistula,lung infection,hemobilia),surgical factors [surgery time,intraoperative blood loss (IBL) volume,gastrointestinal function recovery time,and length of hospital stay],serum inflammatory markers [tumor necrosis factor (TNF)-α,interleukin (IL)-6,and IL-8],and oxidative stress [glutathione peroxidase (GSH-Px),superoxide dismutase (SOD),malondialdehyde (MDA),and advanced protein oxidation products (AOPPs)].RESULTS The analysis revealed markedly better efficacy (an obviously higher total effective rate) in the research group than in the control group.In addition,an evidently lower postoperative complication rate,shorter surgical duration,gastrointestinal function recovery time and hospital stay,and lower IBL volume were observed in the research group.Furthermore,the posttreatment serum inflammatory marker (TNF-α,IL-6,and IL-8) levels were significantly lower in the research group than in the control group.Compared with those in the control group,the posttreatment GSH-Px,SOD,MDA and AOPPs in the research group were equivalent to the pretreatment levels;for example,the GSH-Px and SOD levels were significantly higher,while the MDA and AOPP levels were lower.CONCLUSION Dual-modality endoscopy therapy (duodenoscopy and laparoscopy) is more effective than traditional laparotomy in the treatment of intra-and extrahepatic BDSs and has a lower risk of postoperative complications;significantly shortened surgical time;shorter gastrointestinal function recovery time;shorter hospital stay;and lower intraoperative bleeding volume,while having a significant inhibitory effect on excessive serum inflammation and causing little postoperative oxidative stress.
Key Words: Dual-modality endoscopy;Traditional laparotomy;Ⅰntra-and extrahepatic bile duct stones;Clinical efficacy
lNTRODUCTlON
Bile duct stones (BDSs) are calculi that occur in the hepatobiliary system and are etiologically related to cholestasis,bile duct infection,stenosis or obstruction,and the presence of foreign bodies in the bile duct[1-3].Occurring in the digestive system,BDSs often do not heal spontaneously;moreover,intrahepatic BDSs can easily migrate to the common bile duct and become extrahepatic BDSs,which may progress to cirrhosis and even liver cancer[4].According to epidemiological data,patients with BDSs have a risk of gallstones of up to 15%,which poses considerable challenges to treatment[5].In addition,the heterogeneity of BDSs (stone location,size and other factors) may lead to different clinical symptoms and affect the health of patients to varying degrees[6,7].At present,intra-and extrahepatic BDSs are mainly treated surgically,but the success rate of surgery is not satisfactory,and there is a risk of postoperative complications[8].Therefore,it is necessary to optimize the surgical treatment of intra-and extrahepatic BDSs,which is highly important for improving the treatment experience of such patients.
Traditional laparotomy involves incision,anterograde or retrograde cholecystectomy,choledochoscopic exploration,Ttube drainage,etc.[9,10].Despite its ability to allow stone removal,it is disadvantageous in that it causes large wounds,a large amount of intraoperative blood loss (IBL),and increases the risk of postoperative complications[11].This procedure is particularly inappropriate for older adults with underlying medical conditions,which increase the risk of surgery and affect the treatment efficacy[12,13].Dual-modality endoscopy therapy consisting of duodenoscopy and laparoscopy was discussed in this study;the former allows the removal of extrahepatic BDSs through endoscopic retrograde cholangiopancreatography (ERCP),while the latter allows the complete removal of intrahepatic BDSsvialaparoscopic resection[14].A single case study reported that this combination procedure is safe for patients with gallstones;these patients are unlikely to experience postoperative complications,such as bleeding,bile leakage,or pancreatitis and recover well three months after surgery[15].In another study,compared with preoperative duodenoscopy,laparoscopy combined with intraoperative duodenoscopy for patients with cholecystolithiasis combined with choledocholithiasis had a higher success rate,caused less pain,and required a shorter hospital stay[16].
This study included 95 patients with intra-and intrahepatic BDSs and compared the clinical effects of combination therapy (duodenoscopy+laparoscopy) with those of traditional laparotomy,aiming to provide an optimized scheme for the surgical treatment of such patients.
MATERlALS AND METHODS
General information
Ninety-five patients with intra-and extrahepatic BDSs treated between August 2019 and May 2023 at Wuhan No.1 Hospital were included;45 patients in the control group were treated by traditional laparotomy,and 50 patients in the research group were treated by dual-modality endoscopy.The research and control groups did not differ much in terms of the general data (P> 0.05),which were clinically comparable.Eligibility and exclusion criteria
Eligibility criteria:All the patients correctly diagnosed with intra-and extrahepatic BDSs were free of serious infectious diseases,had intact medical records,could communicate normally and had normal cognitive ability,and had no surgical contraindications.
Exclusion criteria:Patients with hepatobiliary diseases or malignancies,autoimmune deficiency or coagulation dysfunction,poor compliance or cognitive dysfunction,or who were lactating or pregnant.
Treatment methods
The control group was treated by traditional laparotomy.After general anesthesia,a longitudinal incision was made in the patient’s right upper abdomen through the rectus abdominis,or a subcostal oblique incision was created through the costal margin.After laparotomy,the gallbladder was resected anterogradely or retrogradely,and T-tube drainage was performed following lithotomy and routine choledochoscopy to confirm the absence of BDSs.
The research group received dual-modality endoscopy therapy (duodenoscopy and laparoscopy): Patients were placed in the left lateral position during endoscopic sphincterotomy (EST),and ERCP was routinely performed under anesthesia to determine the location of the lesions.In the case of unsuccessful bile duct catheterization,a guide wire was placed in the common bile duct during cholangiography to guide the incision knife.Depending on the conditions of the nipple and the opening,different human papillotomes were selected and inserted to cut the major duodenal papilla.The incision length was determined based on the length of the eminentia medialis of the papillary orifice,which is generally 1-1.5 cm,through which smaller stones (< 1.0 cm) can be removed directly using the ‘basket-in-catheter’ technique;large stones (approximately 2.0 cm) were first crushed with a lithoclast and then removed with a basket catheter.Extraction balloons were used if there were several stones in the common bile duct,especially small stones.After the contrast media was injected to ensure that there was no residual stones,the bile duct was rinsed with normal saline several times,and the duodenoscope was removed.This was followed by 24 h of fasting from both food and water,as well as routine antiinfection treatment.The patient subsequently underwent laparoscopic cholecystectomy under general anesthesia in the supine position and pneumoperitoneum was created by inserting a veress needle.Next,Calot’s triangle was dissected,and the neck of the gallbladder or Hartmann’s pouch was grasped with grasping forceps to pull it to the upper right side.Then,the cystic duct was pulled perpendicular to the common bile duct then bluntly separated from the gallbladder artery.Titanium clips were placed as close to the neck of the gallbladder as possible,after which the two titanium clips were cut with scissors.Finally,the gallbladder artery was found in the posterior inner region,the lower hole was placed to remove the stone,and the drainage tube was routinely placed in the right anterior axillary foramen to extract the stone.
Efficacy
The criteria for treatment efficacy evaluation were as follows: the stones were completely removed,and the clinical symptoms disappeared completely;the stones were not completely removed,and the clinical symptoms were alleviated;and the stones were not removed,and the clinical symptoms did not improve or even worsened.Total effective rate=(marked effectiveness cases and improvement cases)/total cases.
Safety
We observed and recorded the number of patients with incision infections,biliary fistulas,pulmonary infections,and hemobilia in the two groups and calculated the incidence.
Surgical indicators
The surgical duration,intraoperative blood loss (IBL) volume,gastrointestinal function recovery time and length of hospital stay were recorded.
Serum inflammatory markers
Five milliliters of venous blood were collected pre-and postoperatively on an empty stomach in the morning,and serum was obtained after centrifugation to determine tumor necrosis factor (TNF)-α,interleukin (IL)-6 and IL-8 Levels using an enzyme-linked immunosorbent assay (ELISA).
Oxidative stress
Serum levels of glutathione peroxidase (GSH-Px),superoxide dismutase (SOD),malondialdehyde (MDA) and advanced protein oxidation products (AOPPs) were detectedviaimmunofluorescence quantification.
Statistical analyses
In this study,normally distributed data were analyzed (mean ± SD),and between-group and within-group comparisons were made by independent samplettests and pairedttests,respectively.The intergroup differences in count data,described asn(%),were determined byχ2tests.SPSS 21.0 software was used for statistical analysis,and a minimum significance level ofP< 0.05 was used throughout.
RESULTS
Patient general information
Age,sex,disease duration,stone diameter,number of stones,total bilirubin concentration and other general data were similar between the research and control groups (P> 0.05;Table 1).

Table 1 Patient general information
Efficacy in both groups
The evaluation of efficacy revealed a statistically significant difference in the total effective rate between the control and research groups (77.78%vs94.00%,P< 0.05;Table 2).
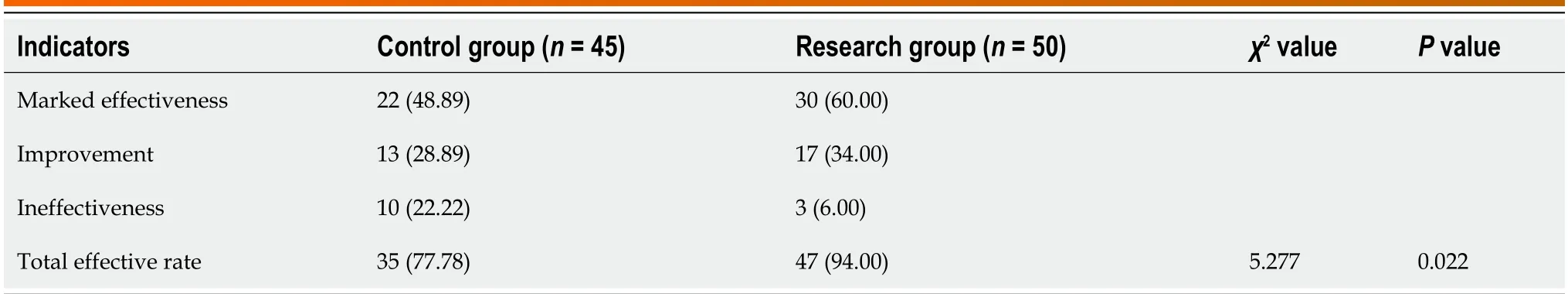
Table 2 Efficacy of the two treatments,n (%)
Safety of the two groups
The total incidence rates of incision infection,biliary fistula,pulmonary infection and hemobilia also differed significantly between the control and experimental groups (20.00%vs4.00%,P< 0.05;Table 3).
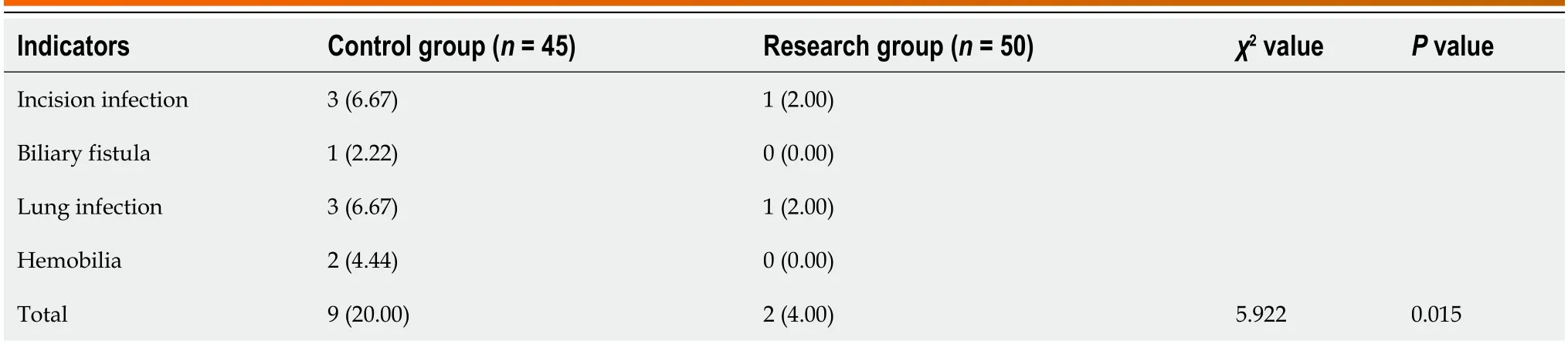
Table 3 Safety of the two groups,n (%)
Surgical indices of both groups
Statistical analysis showed significant differences in surgical time,IBL volume,gastrointestinal function recovery time and length of hospital stay between the two groups,with better results being observed in the research group (P< 0.05;Figure 1).

Figure 1 Surgical indices of the two groups. A: Comparison of surgical times;B: Comparison of intraoperative blood loss volumes;C: Comparison of gastrointestinal function recovery times;D: Comparison of lengths of hospital stay.aP < 0.05 and bP < 0.01 vs the control group.
Serum inflammatory marker levels in both groups
ELISA quantification of serum inflammatory markers such as TNF-α,IL-6 and IL-8 revealed no notable intergroup differences between these indicators pre or postoperatively (P> 0.05);all these indices decreased markedly and to different degrees in both groups after surgery,with even lower TNF-α,IL-6 and IL-8 Levels in the research group (P< 0.05;Figure 2).
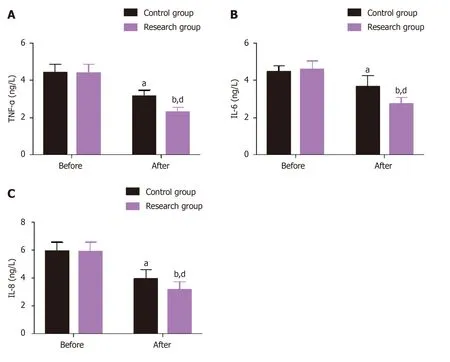
Figure 2 Serum inflammatory marker levels in the two groups. A: Changes in tumor necrosis factor-α before and after treatment;B: Changes in interleukin (IL)-6 before and after treatment;C: Changes in IL-8 Levels before and after treatment in the two groups.aP < 0.05 and bP < 0.01 vs before treatment;dP < 0.05 vs control group.TNF-α: Tumor necrosis factor-α,IL-6: Interleukin-6.
Oxidative stress indices of both groups
Oxidative stress indices such as GSH-Px,SOD,MDA,and AOPPs in the serum were detected by immunofluorescence quantification.No significant differences were identified in these oxidative stress indices between the two groups before treatment (P> 0.05).A significant reduction in GSH-Px and SOD and a marked increase in MDA and AOPPs were observed in the control group after treatment,with lower GSH-Px and SOD and higher MDA and AOPPs levels compared with the research group (P< 0.05;Figure 3).
Figure 3 Oxidative stress indices of the two groups. A: Changes in glutathione peroxidase in the two groups before and after treatment;B: Changes in superoxide dismutase activity in the two groups before and after treatment;C: Changes in malondialdehyde levels before and after treatment in the two groups;D: Changes in the advanced protein oxidation products concentration before and after treatment in the two groups.aP < 0.05 and bP < 0.01 vs before treatment;dP < 0.05 vs control group.GSH-Px: Glutathione peroxidase;SOD: Superoxide dismutase;MDA: Malondialdehyde;AOPPs: Advanced protein oxidation products.
DlSCUSSlON
BDSs are a kind of cholelithiasis,and some patients have subtle clinical symptoms such as dyspepsia and biliary colic[17].Cholelithiasis is known to affect approximately 15% of Americans,with most being women.Factors such as pregnancy and obesity during pregnancy further increase the risk of the disease in women[18].To improve the clinical symptoms of patients with intra-and extrahepatic BDSs and restore their normal life and health,it is necessary to optimize and explore treatment strategies.
Many scholars have explored the pathological identification and surgical treatment of BDSs.For example,Shinet al[19] reported that the use of peroral cholangioscopy can help identify bile duct neoplastic lesions and guide surgery.In addition,Yanget al[20] noted in their study that laparoscopic hepatectomy combined with endoscopic papillary balloon dilation is safe and effective in treating complex BDSs and is beneficial due to rapid postoperative recovery and a low risk of complications.As reported by Lvet al[21],choledochoscopic-guided holmium laser lithotripsy can not only completely remove stones in patients with intractable extra and intrahepatic BDSs but can also prevent postoperative adverse reactions such as biliary tract injury.In this study,the clinical effects of dual-modality endoscopy (duodenoscopy+laparoscopy) and traditional laparotomy in patients with intrahepatic and extrahepatic BDSs were compared and analyzed.The efficacy evaluation showed an evidently higher total effective rate in the research group than in the control group (94.00%vs77.78%),which suggested that duodenoscopy+laparoscopy has a better curative effect in patients with intra-and extrahepatic BDSs.According to the study by Qinet al[14],compared to traditional laparotomy,dual-modality endoscopy increases the surgical success rate,reduces the risk of trauma and shortens the hospital stay for patients undergoing treatment for extrahepatic BDSs,which is consistent with our findings.After assessing the safety of the procedures,the total incidences of incision infection,biliary fistula,pulmonary infection and hemobilia were markedly lower in the research group than in the control group (4.00%vs20.00%),indicating that the combined intervention (duodenoscopy and laparoscopy) is safer than traditional laparotomy for patients with intra-and extrahepatic BDSs.
Subsequent evaluation of surgical indicators revealed that the surgical time,gastrointestinal function recovery time and length of hospital stay were shorter and the IBL volume was lower in the research group than in the control group.Duodenoscopy+laparoscopy is suggested to have a better surgical effect in the treatment of intra-and extrahepatic BDSs and to have significant clinical advantages in reducing surgical time,gastrointestinal function recovery time,hospitalization time and IBL volume.This could be attributed to the fact that surgical procedures such as EST,ERCP and laparoscopic cholecystectomy combined with dual-modality endoscopic therapy are minimally invasive and do not cause water or electrolyte imbalances or disordered physiological functions caused by bile outflow,thus avoiding the risk of postoperative complications and accelerating patient recovery[22,23].In addition,the surgical operator has a larger and clearer surgical field of view under dual-modality endoscopy treatment,which is conducive to shortening the surgical process to some extent[24].In the research by Zhaoet al[25],duodenoscopy plus laparoscopy showed better performance than laparotomy in the treatment of gallstones and extrahepatic BDSs,which was mainly reflected by less IBL,fewer postoperative complications,shorter time to postoperative oral food intake,less fatigue,shorter time to ambulation,shorter postoperative hospitalization time,and faster postoperative recovery,which is similar to our research results.According to the serum inflammatory marker data,the TNF-α,IL-6 and IL-8 Levels in the research group were significantly lower than those in the pretreatment and control groups,suggesting the significant inhibitory effect of duodenoscopy plus laparoscopy on the serum inflammatory markers in patients with intra-and extrahepatic BDSs.Moreover,statistical analysis of the oxidative stress indices revealed no significant changes in GSH-Px,SOD,MDA or AOPPs in the research group after surgery,while the above indices in the control group were significantly different,with notably lower GSH-Px and SOD levels and higher MDA and AOPP levels than those in the research group.These findings show that duodenoscopy plus laparoscopy has little effect on oxidative stress in patients with intra-or extrahepatic BDSs.
Several limitations in this study need to be further considered.First,this was a single-center study with a small number of patients included,which may inevitably lead to information collection bias.In the future,the sample size should be increased,and multicenter data should be included in the analysis to improve the accuracy of the research results.Second,there was no analysis of patient prognosis,which should be supplemented later to better understand the impact of these two treatments on patient prognosis.Finally,the factors that affect the treatment efficacy and safety have not been explored in depth.Supplementing the analysis in this aspect will help to further improve the management efficacy and facilitate the development of methods to improve the efficacy and safety of dual-modality endoscopy to some extent.In the future,the study will be gradually improved with respect to the above perspectives.
CONCLUSlON
In conclusion,duodenoscopy+laparoscopy is better than traditional laparotomy for patients with intra-and extrahepatic BDSs in that it has significantly better clinical efficacy,reduces the risks of surgery and postoperative complications,promotes postoperative rehabilitation,and alleviates serum inflammatory markers while causing little oxidative stress,making it clinically valuable.
ARTlCLE HlGHLlGHTS
Research background
Currently,surgery is still the main treatment for intrahepatic and extrahepatic bile duct stones (BDSs),but the success rate of surgery is unsatisfactory and there is a certain risk of postoperative complications.
Research motivation
It is necessary to optimize the surgical treatment of intrahepatic and extrahepatic BDSs,which is of great significance for improving the treatment experience of such patients.
Research objectives
This study was conducted to clarify the clinical advantages of dual-modality endoscopy (duodenoscopy and laparoscopy) over traditional laparotomy in the treatment of intrahepatic and extrahepatic BDSs.
1. Sneewittchen : Both elements of this compound word are in Low German, although the tale itself is recorded in High German. The High German form of the heroine s name would be Schneeweißchen. The literal translation is Little Snow White (Ashliman 2002). IR & HAHReturn to place in story.
Research methods
Ninety-five patients with intrahepatic and intrahepatic BDSs were included.The control group (n=45) received traditional laparotomy and the research group (n=50) received dual-modality endoscopy (duodenoscopy and laparoscopy).The efficacy,safety,surgical indexes,serum inflammatory indexes,oxidative stress indicators,etc.of the two groups were collected for comparative analysis.
Research results
Compared with the control group,the total effective rate was significantly higher in the research group and the postoperative complication rate was statistically lower.In addition,shorter operation time,smaller intraoperative bleeding volume,faster gastrointestinal function recovery,and less hospitalization time were determined in the research group.Moreover,the research group showed more significant improvements in serum inflammation indexes and alleviation of oxidative stress.
Research conclusions
Compared with traditional laparotomy,dual-modality endoscopy is more effective in the treatment of intrahepatic and extrahepatic BDSs with a lower risk of postoperative complications,which can significantly reduce operation time,gastrointestinal function recovery time,hospital stay,and intraoperative blood loss,while effectively inhibiting serum hyperinflammation and causing less postoperative stress responses.
Research perspectives
Duodenoscopy combined with laparoscopy has higher efficacy and safety than traditional laparotomy in patients with extrahepatic and extrahepatic BDSs.However,this study has some limitations,such as limited cases included,being a single-center experience,and failure to include analysis related to factors affecting prognosis,efficacy and safety,which need to be gradually addressed in future studies.
FOOTNOTES
Co-first authors:Wei Wang and Hui Xia.
Author contributions:Wang W and Xia H contributed equally to this work and are co-first authors;Wang W and Xia H designed the research and wrote the first manuscript;Wang W,Xia H and Dai B contributed to conceiving the research and analyzing data;Wang W and Xia H conducted the analysis and provided guidance for the research;all authors reviewed and approved the final manuscript.
Supported by2021 Municipal Health Commission Scientific Research Project,No.WX21D48;2021 Municipal Health Commission Project,No.WZ21Q11;and 2022 Hubei Provincial Department of Science and Technology Project,No.2022CFB980.
lnformed consent statement:Patients were not required to give informed consent to the study because the analysis used anonymous clinical data that were obtained after each patient agreed to treatment by written consent.
Conflict-of-interest statement:There is no conflict of interest.
Data sharing statement:All data and materials are available from the corresponding author.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORClD number:Bin Dai 0000-0002-0472-8512.
S-Editor:Wang JL
L-Editor:A
P-Editor:Yuan YY
杂志排行
World Journal of Gastrointestinal Surgery的其它文章
- Alcohol associated liver disease and bariatric surgery: Current perspectives and future directions
- Applications of gastric peroral endoscopic myotomy in the treatment of upper gastrointestinal tract disease
- Ex vivo liver resection and auto-transplantation and special systemic therapy in perihilar cholangiocarcinoma treatment
- Evaluation of bacterial contamination and medium-term oncological outcomes of intracorporeal anastomosis for colon cancer: A propensity score matching analysis
- Rescue from complications after pancreaticoduodenectomies at a low-volume Caribbean center: Value of tailored peri-pancreatectomy protocols
- Comparison of prognosis and postoperative morbidities between standard pancreaticoduodenectomy and the TRlANGLE technique for resectable pancreatic ductal adenocarcinoma
