自发性急性脑出血患者血浆sCD163/sTWEAK比值与预后的关系
2024-04-01张文超杨雪辉尹涛王睿健张盟盟
张文超 杨雪辉 尹涛 王睿健 张盟盟


摘要:目的 探究自發性急性脑出血(ACH)患者血浆可溶性CD163(sCD163)/可溶性肿瘤坏死因子样凋亡弱诱导因子(sTWEAK)比值与预后的关系。方法 纳入ACH患者90例作为病例组,根据格拉斯哥预后评分将病例组分为预后不良组(38例)和预后良好组(52例);另选取同期体检健康者45例为对照组。酶联免疫吸附试验检测血浆sCD163、sTWEAK水平并计算sCD163/sTWEAK比值。分析血浆sCD163、sTWEAK水平及sCD163/sTWEAK比值与临床资料的相关性;Logistic回归分析ACH患者预后不良的影响因素;受试者工作特征(ROC)曲线分析sCD163/sTWEAK比值对ACH患者预后不良的预测价值。结果 病例组血浆sCD163、sTWEAK水平及sCD163/sTWEAK比值均显著高于对照组;预后良好组上述指标均低于预后不良组(P<0.05)。预后良好组血肿体积、美国国立卫生研究院卒中量表(NIHSS)评分、高血压及幕下出血比例均低于预后不良组,低密度脂蛋白胆固醇(LDL-C)高于预后不良组(P<0.05)。相关性分析表明,血浆sCD163、sTWEAK水平及sCD163/sTWEAK比值与出血部位、血肿体积、NIHSS评分、白细胞计数、血小板计数、中性粒细胞/淋巴细胞比值(NLR)呈正相关(P<0.05)。Logistic回归分析显示,sCD163/sTWEAK比值、出血部位、血肿体积、NIHSS评分为ACH患者预后不良的影响因素(P<0.05)。ROC曲线结果表明,sCD163/sTWEAK比值评估ACH患者预后不良的AUC为0.850,敏感度和特异度分别为86.84%和69.23%。结论 sCD163/sTWEAK比值在ACH患者血浆中水平较高,并与预后不良有关,该值对此类患者的预后有一定预测价值。
关键词:脑出血;细胞因子TWEAK;预后;可溶性血红蛋白清道夫受体163蛋白;可溶性肿瘤坏死因子样凋亡弱诱导因子
中图分类号:R743.34文献标志码:ADOI:10.11958/20231437
The relationship between plasma sCD163/sTWEAK ratio and prognosis in patients with spontaneous acute cerebral hemorrhage
ZHANG Wenchao1, YANG Xuehui1△, YIN Tao2, WANG Ruijian2, ZHANG Mengmeng2
1 Department of Neurosurgery, Harison International Peace Hospital, Hengshui 053000, China;
2 Department of Neurosurgery, Hengshui People's Hospital
△Corresponding Author E-mail: Yxh1069@163.com
Abstract: Objective To investigate the relationship between the ratio of soluble hemoglobin scavenger receptor 163 protein (sCD163)/soluble tumor necrosis factor-like weak inducer of apoptosis (sTWEAK) in plasma and prognosis in patients with spontaneous acute cerebral hemorrhage (ACH). Methods From August 2020 to August 2022, 90 patients with ACH admitted to the Department of Neurosurgery, Harison International Peace Hospital, Hengshui City were regarded as the research group. According to the Glasgow outcome scale, patients with ACH were separated into the poor prognosis group (n=38) and the good prognosis group (n=52). Another 45 healthy examinee who underwent physical examination were used as the control group. Enzyme linked immunosorbent assay (ELISA) was applied to detect plasma sCD163 and sTWEAK levels, and the sCD163/sTWEAK ratio was calculated. Pearson method was applied to analyze the correlation between plasma sCD163, sTWEAK levels, sCD163/sTWEAK ratio and clinical data. Logistic regression was applied to analyze influencing factors of poor prognosis in patients with ACH. Receiver operating characteristic (ROC) was applied to analyze the predictive value of sCD163/sTWEAK ratio for poor prognosis of patients with ACH. Results The plasma levels of sCD163, sTWEAK and sCD163/sTWEAK ratio were obviously higher in the research group than those in the control group (P<0.05). The plasma levels of sCD163, sTWEAK and sCD163/sTWEAK ratio were obviously lower in the good prognosis group than those in the poor prognosis group (P<0.05). Hematoma volume, National Institutes of Health Stroke Scale (NIHSS) scores, hypertension and subtentorial hemorrhage were lower in the good prognosis group than those in the poor prognosis group, and low density lipoprotein cholesterol (LDL-C) was higher in the good prognosis group than that in the poor prognosis group (P<0.05). Correlation analysis showed that plasma sCD163, and sTWEAK levels and the sCD163/sTWEAK ratio were positively correlated with bleeding site, hematoma volume, NIHSS score, white blood cell count, platelet count and neutrophil/lymphocyte ratio (NLR) (P<0.05). Results of Logistic regression analysis showed that sCD163, sTWEAK, sCD163/sTWEAK ratio, hematoma volume, bleeding site and NIHSS score were influencing factors for poor prognosis in patients with ACH (P<0.05). Results of receiver operating characteristic showed that the AUC of sCD163/sTWEAK ratio in evaluating poor prognosis of patients with ACH was 0.850, and the sensitivity and specificity were 86.84% and 69.23%. Conclusion The sCD163/sTWEAK ratio has a high level in the plasma of patients with ACH, which is associated with poor prognosis and has important value in predicting the prognosis of patients with ACH.
Key words: cerebral hemorrhage; cytokine TWEAK; prognosis; soluble hemoglobin scavenger receptor 163 protein; soluble tumor necrosis factor-like weak inducer of apoptosis
脑出血是脑卒中最常见的类型,其早期死亡和长期残疾的风险较高[1]。自发性脑出血常由小血管疾病引起,包括深穿支动脉病变或脑淀粉样血管病;尽管自发性脑出血占所有卒中的比例较低,但其导致卒中发病率和死亡率的比例较高,且很少有经过验证有效的急性或预防性治疗方法[2]。血红蛋白清道夫受体163蛋白(CD163)是单核细胞和巨噬细胞上的血红蛋白清除受体,与炎症有关,被认为是活化的M2巨噬细胞的标志物,在炎症反应中上调,能促进血管生成和基质金属蛋白酶的产生,可溶性CD163(soluble CD163,sCD163)通过膜蛋白的蛋白水解和外结构域分解释放到血浆中,在炎症期间,病原体和损伤相关的刺激会诱导sCD163脱落[3-4]。可溶性肿瘤坏死因子样凋亡弱诱导因子(soluble tumor necrosis factor‐like weak inducer of apoptosis,sTWEAK)是TNF超家族的细胞因子,能改变血脑屏障通透性,诱导基质金属蛋白酶和促炎细胞因子在大脑中过表达,与血管内皮功能障碍、神经血管病变和心脑血管预后密切相关,在脑出血患者体内水平升高[5]。sCD163能与sTWEAK相互作用,sCD163/sTWEAK比值与C反应蛋白水平显著相关,是各种疾病中比单独sCD163和sTWEAK水平更显著的预测因子[6]。但目前關于sCD163/sTWEAK比值与急性脑出血(acute cerebral hemorrhage,ACH)患者预后关系的研究相对较少。鉴于此,本研究主要分析ACH患者血浆sCD163/sTWEAK比值与预后的关系。
1 对象与方法
1.1 研究对象 选取衡水市哈励逊国际和平医院神经外科2020年8月—2022年8月收治的ACH患者90例并作为病例组,平均年龄(43.51±6.25)岁,男51例,女39例。纳入标准:(1)符合《中国脑出血诊治指南(2019)》诊断标准[7]。(2)进行了影像学检查。(3)首次发病。(4)在发病12 h内入院接受治疗。(5)临床资料完整。排除标准:(1)脑梗死、脑肿瘤等。(2)神经系统疾病。(3)凝血功能障碍。(4)免疫系统紊乱。(5)进行过相关治疗。(6)脏器功能障碍。另选取同期体检健康者45例为对照组;平均年龄(42.87±6.11)岁,男25例,女20例。2组年龄(t=0.569)、性别(c2=0.015)比较差异无统计学意义(均P>0.05)。本研究经医院伦理委员会批准(伦理号:2022-2-037-1),患者对研究内容知情并同意。
1.2 方法
1.2.1 血浆sCD163、sTWEAK水平测定 采集所有受试者入院24 h内空腹静脉血5 mL,乙二胺四乙酸抗凝处理,1 000 r/min离心15 min分离血浆。酶联免疫吸附试验(试剂盒购自上海江莱生物科技有限公司)检测血浆sCD163和sTWEAK水平,实验具体操作按试剂盒说明进行。计算sCD163/sTWEAK比值。
1.2.2 临床资料收集及预后随访 收集患者性别、年龄、体质量指数(BMI)、糖尿病、冠心病、高血压、入院时血肿体积、出血部位、血压、血糖、总胆固醇(TC)、三酰甘油(TG)、发病至手术时间、手术时间、白细胞计数(WBC)、低密度脂蛋白胆固醇(LDL-C)、血小板计数(PLT)、中性粒细胞/淋巴细胞比值(NLR)、美国国立卫生研究院卒中量表(NIHSS)评分等资料。在对患者随访3个月后,通过格拉斯哥预后评分(GOS)评估预后[8],根据GOS将病例组分为预后不良组(GOS≤3分)38例和预后良好组(GOS>3分)52例。
1.3 统计学方法 采用SPSS 25.0处理数据,计数资料以例(%)表示,组间比较采用χ2检验;计量资料以[x] ±s表示,组间比较采用t检验。Pearson法分析血浆sCD163、sTWEAK水平及sCD163/sTWEAK比值与血肿体积、NIHSS评分、WBC、PLT、NLR的相关性,Spearman法分析与出血部位的相关性;Logistic回归分析ACH患者预后不良的影响因素;受试者工作特征(ROC)曲线分析sCD163/sTWEAK比值对ACH患者预后不良的预测价值。P<0.05为差异有统计学意义。
2 结果
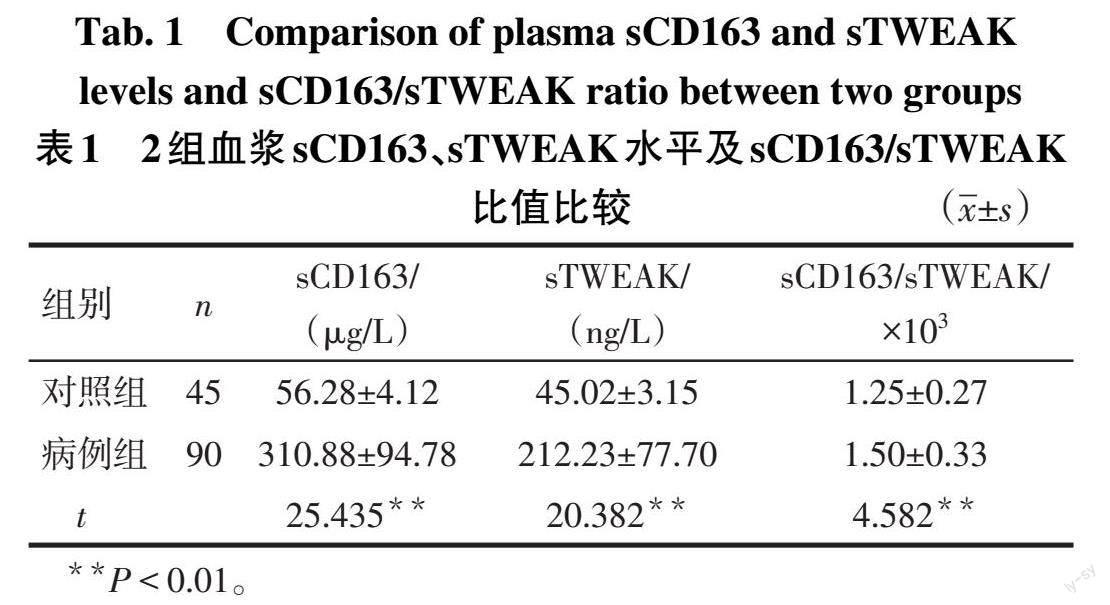
2.1 病例组和对照组血浆sCD163、sTWEAK水平及sCD163/sTWEAK比值比较 病例组血浆sCD163、sTWEAK水平及sCD163/sTWEAK比值均显著高于对照组(P<0.05),见表1。
2.2 预后良好组和预后不良组血浆sCD163、sTWEAK水平及sCD163/sTWEAK比值比较 预后良好组患者血浆sCD163、sTWEAK水平及sCD163/sTWEAK比值显著低于预后不良组患者(P<0.05),见表2。
2.3 2组患者临床资料比较 预后良好组和预后不良组患者性别、年龄、BMI、糖尿病、冠心病、发病至手术时间、手术时间、TC、TG、收缩压、舒张压、血糖比较差异无统计学意义(P>0.05),预后良好组血肿体积、NIHSS评分、WBC、PLT、NLR、高血压及幕下出血比例低于预后不良组,LDL-C高于预后不良组(P<0.05),见表3。
2.4 sCD163/sTWEAK与出血部位等指标的相关性分析 相关性分析表明,病例组血浆sCD163、sTWEAK水平及sCD163/sTWEAK比值与出血部位、血肿体积、NIHSS评分、WBC、PLT、NLR均呈正相关(P<0.05),见表4。
2.5 ACH患者预后不良的影响因素分析 sCD163、sTWEAK及sCD163/sTWEAK比值存在共线性,因此选择以sCD163/sTWEAK比值、高血压、WBC、血肿体积、PLT、LDL-C、NLR、NIHSS评分(均为实测值)、出血部位(幕下出血=1,幕上出血=0)为自变量,以ACH患者预后状况为因变量(不良=1,良好=0),采用逐步向前法进行Logistic回归分析。结果显示,sCD163/sTWEAK比值、出血部位、血肿体积、NIHSS评分为ACH患者预后不良的影响因素(P<0.05),见表5。
2.6 sCD163、sTWEAK及sCD163/sTWEAK比值对ACH患者预后不良的预测价值 ROC曲线分析结果显示,最佳截断值为1.43×103时,sCD163/sTWEAK比值评估患者预后不良的敏感度和特异度更好,见表6、图1。
3 讨论
3.1 ACH的治疗现状 脑出血占所有急性脑血管事件的10%~30%,致残率和死亡率较高,血肿可引发早期炎症反应,从而增强出血性脑内损伤[9]。ACH患者可能出现血肿扩张、神经功能障碍等症状,与患者预后密切相关[10]。自发性脑出血预后较差,且受多种因素影响,近年来尽管此类患者的急性期管理取得了重大进展,但目前尚无特定治疗方法能改善临床结果和远期结局[11]。因此,寻找合适的血浆指标对早期评估ACH患者预后可能具有重要意义。而本文通过检测患者血浆sCD163、sTWEAK水平并计算sCD163/sTWEAK比值来分析其与ACH患者预后的关系。
3.2 sCD163与ACH的发生及预后的关系 CD163是单核巨噬细胞的清道夫受体,与炎症反应有关;sCD163由膜蛋白的蛋白水解产生,以可溶形式释放到血清或其他体液中,其水平升高与癌症患者预后不良有关[12]。有研究表明,血清sCD163水平是巨噬细胞活性的标志物,具有抗炎活性和免疫调节作用,其水平上调可引起巨噬细胞活化和增殖,对活化T淋巴细胞的产生和增殖具有直接抑制作用;sCD163水平的升高可能是炎症增加的标志,其在缺血性和出血性脑卒中的继发性损伤中具有重要作用[13]。Drieu等[14]研究表明,CD163在脑脊液-动脉液流循环中起到关键作用,脑脊液循环不畅与脑出血后颅内压升高、铁离子神经元毒性等不良预后因素有关。ACH患者血清sCD163水平显著高于健康人群,其水平与血肿扩张有关,血清sCD163高表达可促进ACH患者血肿吸收,可作为ACH患者不良结局的预后标志物[15]。在本研究中,ACH患者血浆sCD163水平显著升高,预后良好患者sCD163水平低于预后不良者,说明sCD163水平与ACH患者预后可能具有一定关系。
3.3 sTWEAK及sCD163/sTWEAK与ACH发生及预后的关系 sTWEAK在单核细胞和内皮细胞中均有表达,能与跨膜Ⅰ型蛋白Fn14受体结合,导致信号通路的刺激和促炎分子的释放,与脑出血患者早期血肿生长有关,可作为预测脑出血发生和脑出血患者不良功能结局的生物标志物[16]。有研究表明蛛网膜下腔出血患者血清sTWEAK水平较高,与炎症和出血严重程度密切相关,其浓度升高可能造成患者不良临床结局[17]。在本研究中,ACH患者血浆sTWEAK水平较高,且预后良好患者显著低于预后不良者,说明sTWEAK水平可能与ACH患者预后有关。刘莹等[18]研究表明,脑梗死后血清sTWEAK水平较高,其高水平会加重缺血后脑损伤。赵宾等[19]研究表明,血清sTWEAK水平与急性脑梗死患者脑白质病变密切相关,且其水平随病变程度增加而上调。Altintas等[20]研究表明,心肌梗死预后不良患者sCD163、sTWEAK水平较高,sCD163与sTWEAK水平呈正相关。sCD163/sTWEAK比值增加与心脑血管疾病和外周动脉疾病嚴重程度和远期死亡率有关[21]。本研究中,病例组sCD163/sTWEAK比值较高,预后良好组sCD163/sTWEAK较低。Logistic回归分析表明sCD163/sTWEAK比值与ACH患者预后关系密切。ROC曲线结果表明,sCD163/sTWEAK比值对ACH患者预后不良具有良好的预测价值,进一步证实了该比值在ACH患者预后评估中的作用。
综上所述,sCD163/sTWEAK比值在ACH患者血浆中水平较高,与患者预后不良有关,对预测ACH患者预后具有一定价值。但目前关于sCD163/sTWEAK比值与ACH患者预后关系的研究相对较少,且本研究中样本量较小,随访时间较短,限制了研究结论普遍性,后续需增加样本量深入研究。
参考文献
[1] 张昆龙,薛白洁,肖玮,等. 重复经颅磁刺激对神经病理性疼痛患者疼痛和情绪的影响[J]. 中国现代神经疾病杂志,2022,22(11):940-947. ZHANG K L,XUE B J,XIAO W,et al. Effects of repetitive transcranial magnetic stimulation on pain and emotion of patients with neuropathic pain[J]. Chin J Contemp Neurol Neurosurg,2022,22(11):940-947. doi:10.3969/j.issn.1672-6731.2022.11.005.
[2] HOSTETTLER I C,SEIFFGE D J,WERRING D J. Intracerebral hemorrhage:an update on diagnosis and treatment[J]. Expert Rev Neurother,2019,19(7):679-694. doi:10.1080/14737175.
2019.1623671.
[3] STUHR L K,MADSEN K,JOHANSEN A Z,et al. Combining sCD163 with CA 19-9 increases the predictiveness of pancreatic ductal adenocarcinoma[J]. Cancers (Basel),2023,15(3):897. doi:10.3390/cancers15030897.
[4] NIELSEN M C,HVIDBIERG G R,CLARIA J,et al. Macrophage activation markers,CD163 and CD206,in acute-on-chronic liver failure[J]. Cells,2020,9(5):1175. doi:10.3390/cells9051175.
[5] DA SILVA-CANDAL A,CUSTODIA A,L?PEZ-DEQUIDT I,et al. sTWEAK is a leukoaraiosis biomarker associated with neurovascular angiopathy[J]. Ann Clin Transl Neurol,2022,9(2):171-180. doi:10.1002/acn3.51502.
[6] SCS?NBAUER R,LICHTENAUER M,PAAR V,et al. Regular training increases sTWEAK and its decoy receptor sCD163-does training trigger the sTWEAK/sCD163-axis to induce an anti-inflammatory effect?[J]. J Clin Med. 2020,9(6):1899. doi:10.3390/jcm9061899.
[7] 中华医学会神经病学分会,中华医学会神经病学分会脑血管病学组. 中国脑出血诊治指南(2019)[J]. 中华神经科杂志,2019,52(12):994-1005. Chinese Medical Association Branch of Neurology,Group of Cerebrovascular diseases, Branch of Neurology,Chinese Medical Association. Chinese Guidelines for Diagnosis and Treatment of cerebral hemorrhage(2019)[J]. Chinese Journal of Neurology,2019,52(12):994-1005. doi:10.3760/cma.j.issn.1006-7876.2019.12.003.
[8] 骆金轮,吴非,祝东强,等. 血清HMGB-1 MIF PDGF预测急性脑出血短期预后的临床价值[J]. 河北医学,2021,27(5):785-789. LUO J L,WU F,ZHU D Q,et al. Clinical value of serum HMGB-1 MIF PDGF in predicting short-term prognosis of acute cerebral hemorrhage[J]. Journal of Hebei Medical Sciences,2019,27(5):785-789. doi:10.3969/j.issn.1006-6233.2021.05.018.
[9] LATTANZI S,BRIGO F,TRINKA E,et al. Neutrophil-to-lymphocyte ratio in acute cerebral hemorrhage:a system review[J]. Transl Stroke Res,2019,10(2):137-145. doi:10.1007/s12975-018-0649-4.
[10] 王丹丹,王學建,潘南南. CT岛征和黑洞征及其联合征象对原发性脑出血早期血肿扩大的预测价值[J]. 天津医药,2021,49(2):199-202. WANG D D,WANG X J,PAN N N. The prognostic value of CT island sign,black hole sign and their combined signs for the hematoma enlargement in patients with early stage of primary intracerebral hemorrhage [J]. Tianjin Med J,2021,49(2):199-202. doi:10.11958/20200831.
[11] OLIVEIRA M A L. Surgery for spontaneous intracerebral hemorrhage[J]. Crit Care,2020,24(1):45. doi:10.1186/s13054-020-2749-2.
[12] QIAN S,ZHANG H,DAI H,et al. Is sCD163 a clinical significant prognostic value in cancers? a systematic review and meta-analysis[J]. Front Oncol,2020,10:585298. doi:10.3389/fonc.2020.585297.
[13] BHATTACHARYA A,ASHOURI R,FANGMAN M,et al. Soluble receptors affecting stroke outcomes:potential biomarkers and therapeutic tools[J]. Int J Mol Sci,2021,22(3):1108. doi:10.3390/ijms22031108.
[14] DRIEU A,DU S,STORCK S E,et al. Parenchymal border macrophages regulate the flow dynamics of the cerebrospinal fluid[J]. Nature,2022,611(7936):585-593. doi:10.1038/s41586-022-05397-3.
[15] 王靖萱,陳丹阳,王佳慧,等. 血清炎性标志物在脑出血预后评估中的作用研究进展[J]. 神经损伤与功能重建,2022,17(12):785-787. WANG J X,CHEN D Y,WANG J H,et al. The role of serum inflammatory markers in prognosis evaluation of cerebral hemorrhage[J]. Nerve Injury and Functional Reconstruction,2022,17(12):785-787. doi:10.16780/j.cnki.sjssgncj.20220909.
[16] SILVA-CANDAL A,LOPEZ-DEQUIDT I,RODRIGUEZ-YANEZ M,et al. sTWEAK is a marker of early haematoma growth and leukoaraiosis in intracerebral haemorrhage[J]. Stroke Vasc Neurol,2021,6(4):528-535. doi:10.1136/svn-2020-000684.
[17] DAI J X,CAI J Y,SUN J,et al. Serum soluble tumor necrosis factor-like weak inducer of apoptosis is a potential biomarker for outcome prediction of patients with aneurysmal subarachnoid hemorrhage[J]. Clin Chim Acta,2020,510(1):354-359. doi:10.1016/j.cca.2020.07.052.
[18] 刘莹,王力娜,崔丽丽,等. TWEAK,NF-κB在脑梗死大鼠脑组织的表达及氧化苦参碱对其表达的影响[J]. 脑与神经疾病杂志,2020,28(3):137-143. LIU Y,WANG L N,CUI L L,et al. TWEAK,expression of NF-κB in brain tissue of rats with cerebral infarction and effect of oxymatrine on its expression [J]. Journal of Brain and Neurological Diseases,2020,28(3):137-143. doi:CNKI:SUN:LYSJ.0.2020-03-002.
[19] 赵宾,史肖锦,钟平. 急性脑梗死患者早期血清肿瘤坏死因子样弱凋亡诱导剂水平与脑白质病变的相关性[J]. 卒中与神经疾病,2021,28(1):54-57. ZHAO B,SHI X J,ZHONG P. Correlation between serum levels of tumor necrosis factor-like weak apoptosis inducer and white matter lesions in patients with acute cerebral infarction [J]. Stroke and Neurological Diseases,2021,28(1):54-57.
[20] ALTINTAS M S,EYERCI N,KARAYIGIT O,et al. Low sCD163/TWEAK ratio at first day after acute myocardial infarction associated with adverse cardiac remodeling in non-elderly patients[J]. Kardiologiia,2022,62(10):49-55. doi:10.18087/cardio.2022.10.n2155.
[21] MRAK D,ZIERFUSS B,HOBAUS C,et al. Evaluation of sCD163 and sTWEAK in patients with stable peripheral arterial disease and association with disease severity as well as long-term mortality[J]. Atherosclerosis,2021,317(1):41-46. doi:10.1016/j.atherosclerosis.2020.11.026.
(2023-10-07收稿 2023-11-30修回)
(本文编辑 李鹏)
