血清正五聚蛋白3对坏死性软组织感染的诊断效能研究
2024-03-24李成志乔维龙鲁文王静阿布力米提·阿不都哈力克孙向东
李成志 乔维龙 鲁文 王静 阿布力米提·阿不都哈力克 孙向东
[摘要]目的:探讨血清正五聚蛋白3(Pentraxin 3,PTX3)对坏死性软组织感染(Necrotizing soft tissue infection,NSTI)的诊断效能。方法:选取喀什地区第一人民医院2021年6月-2022年6月行急诊手术治疗的158例疑似NSTI患者作为研究对象,根据术后诊断结果将其分为NSTI组(97例)和非NSTI组(61例),另选取同期该院体检中心健康人群97例作为健康组。比较NSTI组、非NSTI组入院即刻和健康组体检时血清PTX3、C-反应蛋白(C-reactive protein,CRP)、降钙素原(Procalcitonin,PCT)、红细胞沉降率(Erythrocyte sedimentation rate,ESR)、白细胞介素-6(Interleukin-6,IL-6)水平,绘制健康志愿者工作特征(Receiver operating characteristic,ROC)曲线分析上述指标对NSTI的诊断效能。另观察NSTI组患者入院即刻、入院第2天、第3天血清炎症指标水平变化,并统计NSTI组患者住院天数、截肢率、死亡率。另外,根据术后诊断结果将NSTI组分为坏死性筋膜炎组和气性坏疽组,比较两组不同时刻血清炎症指标水平变化,并观察各指标对坏死性筋膜炎和气性坏疽的诊断效能。结果:NSTI组、非NSTI组血清PTX3、CRP、PCT、ESR、IL-6水平均高于健康组(P<0.05),NSTI组均高于非NSTI组(P<0.05);ROC曲线分析结果显示,血清PTX3诊断NSTI的灵敏度均高于CRP、PCT、ESR、IL-6;特异度稍低于PCT,但均高于CRP、ESR、IL-6;曲线下面积(Area under the curve,AUC)均高于CRP、PCT、ESR、IL-6。气性坏疽组血清PTX3、CRP、PCT、ESR、IL-6水平均高于坏死性筋膜炎组(P<0.05);ROC曲线分析结果显示,血清PTX3诊断坏死性筋膜炎和气性坏疽的灵敏度均高于CRP、PCT、ESR、IL-6;特异度稍低于PCT,但均高于CRP、ESR、IL-6;AUC均高于CRP、PCT、ESR、IL-6。入院即刻、入院第2天、入院第3天血清PTX3、CRP、PCT、ESR、IL-6水平在组间、时间、交互效应上差异均有统计学意义(P<0.05);入院第3天血清各指标水平均低于入院即刻和入院第2天(P<0.05),且气性坏疽组入院即刻、入院第2天、入院第3天血清各指标水平均高于坏死性筋膜炎组(P<0.05);气性坏疽组住院平均天数、截肢率、死亡率均高于坏死性筋膜炎组(P<0.05)。结论:NSTI患者血清PTX3水平异常升高,且气性坏疽患者均高于坏死性筋膜炎患者,另PTX3對诊断NSTI和鉴别坏死性筋膜炎与气性坏疽的效能均优于CRP、PCT、ESR、IL-6等常规炎症指标。
[关键词]正五聚蛋白3;坏死性软组织感染;坏死性筋膜炎;气性坏疽;死亡
[中图分类号]R639 [文献标志码]A [文章编号]1008-6455(2024)03-0006-06
Study on the Diagnostic Efficacy of Serum Pentraxin 3 in
Necrotic Soft Tissue Infection
LI Chengzhi1,QIAO Weilong1,LU Wen2,WANG Jing3,Abolimiti·ABDULHALIK1,SUN Xiangdong1
(1.Department of Burn Plastic Surgery, 2.Department of Vascular Surgery, 3.Department of Neurosurgery,Kashgar First People's Hospital,Kashgar 844000,Xinjiang,China)
Abstract: Objective To investigate the diagnostic efficacy of serum serum Pentraxin 3 (PTX3) in necrotic soft tissue infection (NSTI). Methods 158 suspected NSTI patients who underwent emergency surgery in Kashgar First People's Hospital from June 2021 to June 2022 were selected as the study subjects, and they were divided into NSTI group (97 cases) and non NSTI group (61 cases) according to the results of postoperative diagnosis. Another 97 healthy people from the physical examination center of the hospital were selected as the health group. The levels of serum PTX3, C-reactive protein (CRP), procalcitonin (PCT), erythrocyte sedimentation rate (ESR) and interleukin-6 (IL-6) in NSTI group, non NSTI group at the time of admission and health group at the time of physical examination were compared, and the receiver operating characteristic (ROC) curve was drawn to analyze the diagnostic efficacy of the above indicators for NSTI. In addition, the changes of serum conventional inflammatory marks levels of patients in the NSTI group at the moment of admission, the second and third days of admission were observed, and the days of hospitalization, amputation rate and mortality rate of patients in the NSTI group were counted. In addition, the NSTI group was divided into necrotizing fasciitis group and gas gangrene group based on the postoperative diagnostic results, and the changes in serum conventional inflammatory marks levels between two groups at different times were compared, and the diagnostic efficacy of each indicator for necrotizing fasciitis and gas gangrene was observed. Results The levels of serum PTX3, CRP, PCT, ESR, IL-6 in NSTI group and non NSTI group were higher than those in healthy group (P<0.05), which in the NSTI group were higher than those in non NSTI group (P<0.05). ROC curve analysis showed that the sensitivity of serum PTX3 in diagnosing NSTI was higher than that of CRP, PCT, ESR and IL-6, and the specificity was slightly lower than PCT, but it was higher than CRP, ESR, IL-6, and area under the curve (AUC) was higher than CRP, PCT, ESR and IL-6. The serum PTX3, CRP, PCT, ESR, and IL-6 levels in the gas gangrene group were higher than those in the necrotizing fasciitis group (P<0.05). The ROC curve analysis results showed that the sensitivity of serum PTX3 in diagnosing necrotizing fasciitis and gas gangrene was higher than that of CRP, PCT, ESR, and IL-6, and the specificity was the same as PCT, but higher than CRP, ESR, and IL-6, and the AUC was higher than CRP, PCT, ESR and IL-6. There were statistically significant differences in serum PTX3, CRP, PCT, ESR and IL-6 levels among groups, time and interaction effects immediately after admission, on the second day of admission and on the third day of admission (P<0.05). The levels of serum indicators on the third day of admission were lower than those immediately and on the second day of admission (P<0.05), and the gas gangrene group had higher levels of serum indicators on the first day, second day, and third day of admission than the necrotizing fasciitis group (P<0.05). The average length of hospital stay, amputation rate and mortality rate in the gas gangrene group were higher than those in the necrotizing fasciitis group (P<0.05). Conclusion The serum PTX3 level in NSTI patients are abnormally elevated, and patients with gas gangrene are all higher than those with necrotizing fasciitis. In addition, PTX3 is more effective in diagnosing NSTI and distinguishing necrotizing fasciitis from gas gangrene than conventional inflammatory indicators such as CRP, PCT, ESR, IL-6.
Key words: Pentraxin 3; necrotic soft tissue infection; necrotizing fasciitis; gas gangrene; mortality
坏死性软组织感染是指伴有坏死的皮下、肌肉或筋膜等软组织层任意间隙的严重细菌感染,该病发病机制复杂,病情进展迅速,需尽早行手术清创或对感染肢体进行截肢,以避免发生感染性休克、器官衰竭等威胁患者生命[1]。但NSTI早期皮肤症状不明显,容易与蜂窝织炎、皮下脓肿等混淆而延误诊断和治疗,从而导致其致残率、致死率升高[2]。既往临床常用实验室风险指标(Laboratory risk index,LRINEC)评分诊断坏死性筋膜炎,该评分系统包括CRP、白细胞计数、血红蛋白等传统实验室指标,然而相关研究发现[3-4],LRINEC评分诊断坏死性筋膜炎的敏感性不足,仅介于36%~80%。因此,积极寻找诊断NSTI的血清学敏感指标对早期识别病情及治疗具有重要意义。PTX3是一种由中性粒细胞、单核细胞和内皮细胞等产生的急性期炎症因子,可反映局部组织的炎症和损伤程度。国外均有研究报道[5-6],PTX3在感染性休克、社区获得性肺炎等方面的预测和诊断价值均优于CRP、PCT等传统炎症指标,但對于PTX3水平在NSTI中的诊断效能尚罕见研究报道。鉴于此,本研究探讨血清PTX3水平对NSTI的诊断效能,旨在为临床诊断提供更准确的血清指标。
1 资料和方法
1.1 一般资料:选取喀什地区第一人民医院2021年6月-2022年6月行急诊手术治疗的158例疑似NSTI(包括疑似坏死性筋膜炎、疑似气性坏疽、疑似Fourniers Gangrene)患者,根据术后诊断将患者分为NSTI组(97例)和非NSTI组(61例),另同期选取在医院体检中心行体检的健康人群97例作为健康组。NSTI组男60例、女37例,年龄49~70岁,平均(59.25±8.96)岁,体质量指数21~29 kg/m2,平均(24.51±2.72)kg/m2,病变部位:下肢52例,上肢20例,会阴13例,腹部9例,头颈部3例;病变范围:4 cm×6 cm~11 cm×16 cm;累及层次:皮肤3例,浅筋膜16例,深筋膜41例,肌层37例。非NSTI组男36例,女25例;年龄48~69岁,平均(58.93±8.73)岁,体质量指数20~29 kg/m2,平均(24.09±2.79)kg/m2,病变部位:下肢33例,上肢13例,会阴7例,腹部6例,头颈部2例;病变范围:3 cm×5 cm~10 cm×15 cm;累及层次:皮肤28例,浅筋膜22例,深筋膜层10例,肌层1例。健康组男58例,女39例;年龄50~68岁,平均(60.23±9.12)岁,体质量指数21~27 kg/m2,平均(24.89±2.85)kg/m2。三组性别、年龄、体质量指数比较差异均无统计学意义(P>0.05)。
1.2 NSTI诊断标准:术后结合患者术前表现、实验室检查、影像学检查及组织学检查进行诊断[7]。患者皮肤表面有瘀斑、水疱、捻发感、麻木感、疼痛,有组织水肿和坏死,伴(或不伴)高温、低血压、心动过速等全身症状;常规抗感染药物治疗效果不佳;实验室检查NSTI危险指标评分升高;超声、X片等影像学检查发现筋膜增厚、水肿、皮下气肿、脓肿形成;术后组织学检查证实有感染。另外,根据诊断结果将坏死性筋膜炎和Fourniers Gangrene患者统一归为坏死性筋膜炎组,将气性坏疽患者(伤口周围触诊有捻发音,细菌培养见粗大的革兰阳性杆菌,X线片检查发现肌群中有气体存在)归为气性坏疽组。
1.3 纳入标准:年龄≥18周岁;所有疑似NSTI患者均行急诊手术治疗;健康人群均经体检确认健康;所有健康志愿者均自愿参与本研究并签署知情同意书。
1.4 排除/剔除标准:术中无法确认NSTI诊断;伴有严重的肝肾功能损害;既往有急性冠脉综合征、高血压脑出血、慢性阻塞性肺疾病急性加重期等器质性疾病;恶性肿瘤;自身免疫性疾病者;有持续感染或炎症者;拒绝参加本研究或依从性较差者。
1.5 方法
1.5.1 手术方法:所有疑似NSTI患者在入院24 h内进行手术清创,在病变部位多处切开,切口穿过感染区域直达正常组织,完全清除脓液和坏死皮肤、皮下脂肪、筋膜组织和正常组织边缘部分。于术中留取标本进行细菌培养,确定致病菌种类,给予抗生素治疗。
1.5.2 血液样本采集及检测:疑似NSTI患者于入院即刻,健康组于体检当天分别采集空腹静脉血2 ml置于枸橼酸钠抗凝管中混匀,在2 h内送往喀什地区第一人民医院检验科应用全自动血沉仪测定ESR值;另采集5 ml静脉血置于普通采血管中,在室温下静置2 h,以3 000 r/min离心20 min分离血清,取上清液置于相应的样品管中,统一置于医院中心实验室-80℃冰箱中保存待测(6个月内检测)。采用双抗体二步夹心酶联免疫吸附实验检测血清PTX3水平,采用免疫速率比浊法检测血清CRP水平,采用化学发光法检测血清PCT水平,采用酶联免疫吸附试验检测血清IL-6水平。另外,NSTI患者在入院后第2天、第3天再次采集血样检测血清PTX3、CRP、PCT、ESR、IL-6水平,血液处理和检测方法与上述一致。
1.6 观察指标
1.6.1 NSTI组、非NSTI组、健康组血清各指标水平比较:比较基线期血清PTX3、CRP、PCT、ESR、IL-6水平,并记录其对NSTI的诊断效能,如截断值、灵敏度、特异度、AUC和95%可信区间(95% credibility interval,95%CI)。
1.6.2 坏死性筋膜炎组和气性坏疽组入院即刻血清各指标水平比较:比较入院即刻两组血清PTX3、CRP、PCT、ESR、IL-6水平,并记录其对坏死性筋膜炎和气性坏疽的鉴别诊断,如记录截断值、灵敏度、特异度、AUC和95%CI。
1.6.3 坏死性筋膜炎组和气性坏疽组不同时刻血清各指标水平比较:记录两组患者入院第2天、第3天的PTX3、CRP、PCT、ESR、IL-6水平,并进行比较。
1.6.4 NSTI患者住院指标:统计NSTI患者住院天数、截肢率、死亡率。
1.7 统计学分析:使用SPSS 26.0行統计学检验,计量资料采用x?±s描述,两组间比较采用独立样本t检验,多样本比较采用单因素方差分析和SNK-q检验,重复测量的资料比较采用重复测量方差分析和LSD-t检验;计数资料采用“n/%”描述,组间比较使用χ2检验,绘制ROC曲线分析血清PTX3、CRP、PCT、ESR、IL-6水平对NSTI以及坏死性筋膜炎和气性坏疽的诊断效能。P<0.05为差异有统计学意义。
2 结果
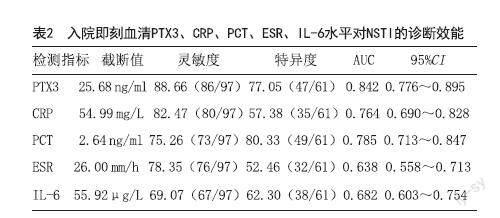
2.1 三组入院即刻血清PTX3、CRP、PCT、ESR、IL-6水平比较:三组血清PTX3、CRP、PCT、ESR、IL-6水平比较差异有统计学意义(P<0.05),NSTI组、非NSTI组血清PTX3、CRP、PCT、ESR、IL-6水平均高于健康组(P<0.05),NSTI组均高于非NSTI组(P<0.05)。见表1。
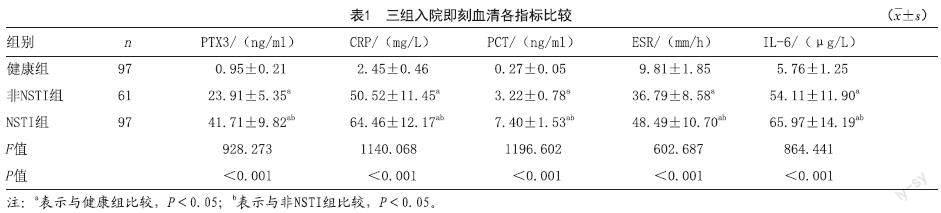
2.2 入院即刻血清PTX3、CRP、PCT、ESR、IL-6水平对NSTI的诊断效能:ROC曲线分析结果显示,血清PTX3诊断NSTI的灵敏度均高于CRP、PCT、ESR、IL-6;特异度稍低于PCT,但均高于CRP、ESR、IL-6;AUC均高于CRP、PCT、ESR、IL-6。见图1、表2。
2.3 坏死性筋膜炎组和气性坏疽组入院即刻血清PTX3、CRP、PCT、ESR、IL-6水平比较:97例NSTI患者中坏死性筋膜炎62例,气性坏疽35例。气性坏疽组血清PTX3、CRP、PCT、ESR、IL-6水平均高于坏死性筋膜炎组(P<0.05)。见表3。
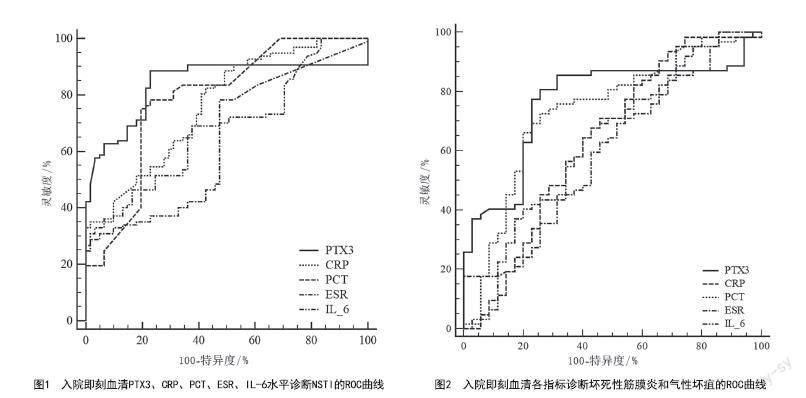
2.4 入院即刻血清PTX3、CRP、PCT、ESR、IL-6水平对坏死性筋膜炎和气性坏疽的鉴别诊断:ROC曲线分析结果显示,血清PTX3诊断坏死性筋膜炎和气性坏疽的灵敏度均高于CRP、PCT、ESR、IL-6;特异度与PCT相同,但均高于CRP、ESR、IL-6;AUC均高于CRP、PCT、ESR、IL-6。见图2、表4。
2.5 NSTI组中坏死性筋膜炎组和气性坏疽组不同时刻血清各指标比较:入院即刻、入院第2天、入院第3天血清PTX3、CRP、PCT、ESR、IL-6水平在组间、时间、交互效应上差异均有统计学意义(P<0.05);坏死性筋膜炎组和气性坏疽组入院即刻和入院第2天血清各指标比较差异均无统计学意义(P>0.05),入院第3天血清各指标水平均低于入院即刻、入院第2天(P<0.05),且气性坏疽组入院即刻、入院第2天、入院第3天血清各指标水平均高于坏死性筋膜炎组(P<0.05)。见表5。
2.6 NSTI组患者住院天数、截肢率、死亡率:NSTI组患者住院平均天数为(37.25±7.23)d,其中坏死性筋膜炎组住院平均天数为(35.85±7.86)d,气性坏疽组住院平均天数为(39.71±8.94)d;截肢率为11.34%(11/97),其中坏死性筋膜炎组截肢率为4.84%(3/62),气性坏疽组截肢率为22.86%(8/35);死亡率8.25%(8/97),其中坏死性筋膜炎组死亡率为3.23%(2/35),气性坏疽组死亡率为17.14%(6/35)。气性坏疽组住院平均天数、截肢率、死亡率均高于坏死性筋膜炎组(P<0.05)。
3 讨论
NSTI具有多种微生物学病因,是一种复杂、罕见的细菌性感染疾病。该病导致软组织广泛损伤、坏死,甚至造成截肢或多器官衰竭,严重威胁患者的生命健康[8]。近年来NSTI的发病率逐渐升高,尽管对该类患者的关注越来越多,但因其早期症状模糊,患者群体异质性较大,缺乏特异性的诊断方法,导致其截肢率及死亡率仍然很高[9-10]。因此,寻找早期快速诊断NSTI的方法,对实现及时和精确的治疗,降低患者严重残疾和死亡的风险,改善预后至关重要。
CRP、IL-6均是炎症早期合成、释放的促炎因子,在炎症反应过程中发挥重要作用[11];PCT是细菌感染的标志物,可判断感染的严重程度;ESR异常升高多见于细菌感染导致的急性改变,在一定程度上能够反映局部病灶的炎症反应程度。既往研究报道[12-13],脓毒症患者CRP、PCT、IL-6、ESR水平均高于普通感染与健康人群。在本研究中NSTI患者血清CRP、PCT、ESR、IL-6水平均高于非NSTI患者和健康人群,表明上述血清指标在不同感染程度及健康人群中存在差异,与上述报道一致。PTX3是由多数炎症细胞和组织细胞产生的一种急性蛋白,通过识别病原微生物,激活补体通路,参与机体的免疫、炎症等反应[14]。血清PTX3在健康机体中不表达或低表达,在机体发生感染后,炎症部位的组织、免疫细胞在白细胞介素1和肿瘤坏死因子的诱导下,可迅速合成并大量分泌PTX-3释放进入血液,导致其水平迅速升高[15]。Ronanki K等[16]研究报道,PTX3水平升高与脓毒症病情有关,能够评估感染严重程度。本研究发现NSTI患者血清PTX3水平均高于非NSTI患者和健康人群,可能有助于鉴别诊断NSTI。
本研究进一步分析血清PTX3、CRP、PCT、ESR、IL-6水平对NSTI的诊断价值,发现IL-6对NSTI诊断效能最低,灵敏度和特异度仅有69.07%和62.30%,研究发现[17],IL-6在新生儿败血症中的诊断效能不足;CRP、ESR诊断NSTI的灵敏度虽然高于IL-6,但特异度仅有57.38%、52.46%,容易导致误诊,影响治疗方案决策;PCT对NSTI诊断的特异度最高,但灵敏度却略低于CRP、ESR,可能由于PCT在感染12~24 h内即可达到高峰,若错过最佳检测时间可能会导致诊断敏感度降低,延误患者治疗;PTX3诊断灵敏度和AUC均高于以上各指标,特异度略低于PCT,在NSTI诊断中凸显优势,可能由于PTX-3与CRP同属于一个超家族,虽出现晚于CRP,但其更加稳定,存在时间更为持久,较CRP能够更迅速反映组织局部炎症、损伤,可作为炎症持续反应的标志物[18]。曾永红等[19]研究也报道在脓毒症诊断中PTX3较CRP、PCT具有更高的灵敏度和特异度,是诊断脓毒血症的重要指标;赵德浩等[20]研究也表明与CRP和白细胞相比,PTX3在颅内感染早期诊断中更具有诊断价值。因此,建议临床在采用常规CRP、PCT等炎症指标诊断NSTI的同时,可增加检测PTX3水平,以提高诊断效能。
本研究结果显示,气性坏疽组血清PTX3、CRP、PCT、ESR、IL-6水平均高于坏死性筋膜炎组,提示以上血清各指标水平在坏死性筋膜炎和气性坏疽中存在差异,可能有助于两者的鉴别诊断。坏死性筋膜炎感染累及皮下脂肪和筋膜组织,但其一般不会损害深层肌肉组织,而气性坏疽是由产气性细菌分泌的酶经糖、蛋白分解后产生大量不溶性气体并积聚,致使血管局部压力增加,加重组织缺血缺氧,促进细菌繁殖和炎症反应,相较于坏死性筋膜炎易侵入机体组织深部导致肌肉组织迅速坏死,致使病情快速恶化至全身感染[21],故在气性坏疽中炎症因子水平相对较高。ROC曲线分析显示,血清PTX3、CRP、PCT、ESR、IL-6对坏死性筋膜炎和气性坏疽均具有一定的鉴别诊断价值,其中PTX3和PCT的诊断效能稍高于CRP、ESR、IL-6,PTX3稍高于PCT,但PTX3鉴别价值有限,建议临床仍需结合患者症状、病原学检查、影像学检查加以鉴别。
本研究结果发现,气性坏疽组入院即刻、入院第2天、入院第3天血清PTX3、CRP、PCT、ESR、IL-6水平均高于坏死性筋膜炎组,入院第2天和入院第3天均呈下降趋势,表明坏死性筋膜炎组和气性坏疽组上述指标均随着治疗时间延长逐渐下降,可能对治疗转归具有一定的评估作用。既往研究发现[22],血清PTX3与颅内感染患者预后情况相关;另有研究报道[23-24],血清CRP、PCT、IL-6与坏死性筋膜炎患者预后有关。由此可推断,血清PTX3、CRP、PCT、ESR、IL-6等指标与坏死性筋膜炎和气性坏疽患者的临床结局有关。另外本研究结果显示,气性坏疽组住院平均天数、截肢率、死亡率均高于坏死性筋膜炎组,说明气性坏疽组患者截肢率和死亡率较高,提示临床应高度重视此类患者,尽早诊断救治,改善患者预后。
综上所述,NSTI患者血清PTX3水平异常升高,且气性坏疽患者高于坏死性筋膜炎患者,血清PTX3有助于诊断NSTI及鉴别坏死性筋膜炎与气性坏疽,其效能优于CRP、PCT、ESR、IL-6等常规炎症指标,有望作为此类疾病的早期诊断标志物。
[参考文献]
[1]Peetermans M,de Prost N,Eckmann C,et al.Necrotizing skin and soft-tissue infections in the intensive care unit[J].Clin Microbiol Infect,2020,26(1):8-17.
[2]Bruun T,Rath E,Madsen M B,et al.Risk factors and predictors of mortality in streptococcal necrotizing soft-tissue infections: A multicenter prospective study[J].Clin Infect Dis,2021,72(2):293-300.
[3]Abdullah M,McWilliams B,Khan S U.Reliability of the laboratory risk indicator in necrotising fasciitis (LRINEC) score[J].Surgeon,2019,17(5):309-318.
[4]Tarricone A,Mata K,Gee A,et al.A systematic review and meta-analysis of the effectiveness of lrinec score for predicting upper and lower extremity necrotizing fasciitis[J].J Foot Ankle Surg,2022,61(2):384-389.
[5]Shi G Q,Yang L,Shan L Y,et al.Investigation of the clinical significance of detecting PTX3 for community-acquired pneumonia[J].Eur Rev Med Pharmacol Sci,2020,24(16):8477-8482.
[6]Hansen C B,Bayarri-Olmos R,Kristensen M K,et al.Complement related pattern recognition molecules as markers of short-term mortality in intensive care patients[J].J Infect,2020,80(4):378-387.
[7]崔瀛書,李怡,代站站,等.坏死性软组织感染的诊治[J].中华损伤与修复杂志(电子版),2019,14(5):374-379.
[8]Kumar T,Kaushik R,Singh S,et al.Determinants of mortality in necrotizing soft tissue infections[J].Hell Cheirourgike,2020,92(5):
159-164.
[9]Nawijn F,Smeeing D P J,Houwert R M,et al.Time is of the essence when treating necrotizing soft tissue infections: a systematic review and meta-analysis[J].World J Emerg Surg,2020,15(1):4.
[10]Eckmann C,Montravers P.Current management of necrotizing soft-tissue infections[J].Curr Opin Infect Dis,2021,34(2):89-95.
[11]曹海萌,盛明珠,汤巧巧.牙周组织再生术联合口腔正畸治疗对慢性牙周炎患者口腔功能及TNF-α,CRP水平的影响[J].中国美容医学,2023,32(1):131-134.
[12]王婷,韦小碗,杨亮,等.脓毒症患者血清PCT、CRP、IL-6和IL-10水平检测及临床意义[J].陕西医学杂志,2020,49(11):1510-1514.
[13]冯彦华,任强,甄磊,等.血清学指标水平变化对儿童急性骨关节感染继发脓毒症的早期预测价值分析[J].河北医科大学学报,2022,43(8):940-944.
[14]Netti G S,Lucarelli G,Spadaccino F,et al.PTX3 modulates the immunoflogosis in tumor microenvironment and is a prognostic factor for patients with clear cell renal cell carcinoma[J].Aging (Albany NY),2020,12(8):7585-7602.
[15]Jiang N,Zhou S,Wang G,et al.Diagnostic value and prognostic significance of CTRP9 combined with pentraxin-3 in acute coronary syndrome[J].Exp Ther Med,2021,21(3):254.
[16]Ronanki K,Bairwa M,Kant R,et al.Pentraxin 3 (PTX3) as a predictor of severity of sepsis in patients admitted to an intensive care unit: A cross-sectional study from north india[J].Cureus,2022,14(8):28282.
[17]劉启星,王斌.IL-6、TNF-α和CRP联合检测在新生儿败血症诊断中的临床意义[J].检验医学与临床,2021,18(15):2272-2274.
[18]Fahmey SS,Mostafa N.Pentraxin 3 as a novel diagnostic marker in neonatal sepsis[J].J Neonatal Perinatal Med,2019,12(4):437-442.
[19]曾永红,徐俊,侯晓琳,等.正五聚蛋白3对脓毒血症的诊断价值[J].中国老年学杂志,2020,40(17):3725-3728.
[20]赵德浩,蒋梁,赵军.PTX3在开颅术后颅内感染中的诊断价值研究[J].重庆医学,2020,49(16):2755-2757.
[21]Leiblein M,Wagner N,Adam E H,et al.Clostridial gas gangrene-a rare but deadly infection: case series and comparison to other necrotizing soft tissue infections[J].Orthop Surg,2020,12(6):1733-1747.
[22]孙占玉,郭智霖,王上桥.血清PTX3和NLRP3联合检测在颅脑损伤术后颅内感染早期诊治中的应用研究[J].热带医学杂志,2022,22(6):837-841.
[23]刘远成,张劲远,李永海,等.肛周坏死性筋膜炎患者4种血液生化指标对疾病预后的预测[J].医学研究生学报,2020,33(2):164-168.
[24]钮柏琳,杜慧敏,廖锐.早期CVVH治疗坏死性筋膜炎并发脓毒性休克的临床研究[J].免疫学杂志,2016,32(2):152-157.
[收稿日期]2022-12-27
本文引用格式:李成志,乔维龙,鲁文,等.血清正五聚蛋白3对坏死性软组织感染的诊断效能研究[J].中国美容医学,2024,33(3):6-11.
