Comparative efficacy and safety between endoscopic submucosal dissection,surgery and definitive chemoradiotherapy in patients with cT1N0M0 esophageal cancer
2024-03-07ShuAiLuoYuYingSunYaTingZengChunYuHuang
Shu-Ai Luo,Yu-Ying Sun,Ya-Ting Zeng,Chun-Yu Huang
Abstract BACKGROUND Endoscopic submucosal dissection (ESD) and surgical resection are the standard of care for cT1N0M0 esophageal cancer (EC),whereas definitive chemoradiotherapy (d-CRT) is a treatment option.Nevertheless,the comparative efficiency and safety of ESD,surgery and d-CRT for cT1N0M0 EC remain unclear.AIM To compare the efficiency and safety of ESD,surgery and d-CRT for cT1N0M0 EC.METHODS We retrospectively analyzed the hospitalized data of a total of 472 consecutive patients with cT1N0M0 EC treated at Sun Yat-sen University Cancer center between 2017-2019 and followed up until October 30th,2022.We analyzed demographic,medical recorded,histopathologic characteristics,imaging and endoscopic,and follow-up data.The Kaplan-Meier method and Cox proportional hazards modeling were used to analyze the difference of survival outcome by treatments.Inverse probability of treatment weighting (IPTW) was used to minimize potential confounding factors.RESULTS We retrospectively analyzed patients who underwent ESD (n=99) or surgery (n=220) or d-CRT (n=16) at the Sun Yat-sen University Cancer Center from 2017 to 2019.The median follow-up time for the ESD group,the surgery group,and the d-CRT group was 42.0 mo (95%CI: 35.0-60.2),45.0 mo (95%CI: 34.0-61.75) and 32.5 mo (95%CI: 28.3-40.0),respectively.After adjusting for background factors using IPTW,the highest 3-year overall survival (OS) rate and 3-year recurrence-free survival (RFS) rate were observed in the ESD group (3-year OS: 99.7% and 94.7% and 79.1%;and 3-year RFS: 98.3%,87.4% and 79.1%,in the ESD,surgical,and d-CRT groups,respectively).There was no difference of severe complications occurring between the three groups (P ≥ 0.05).Multivariate analysis showed that treatment method,histology and depth of infiltration were independently associated with OS and RFS.CONCLUSION For cT1N0M0 EC,ESD had better long-term survival and lower hospitalization costs than those who underwent d-CRT and surgery,with a similar rate of severe complications occurring.
Key Words: Retrospective study;cT1N0M0;Esophageal squamous cell carcinoma;Endoscopic submucosal dissection;Surgery;Definitive chemoradiotherapy
INTRODUCTION
Esophageal cancer (EC) is an aggressive and poorly prognostic gastrointestinal tumor and one of the common causes of cancer death[1].Over the past few decades,the proportion of patients with cT1N0M0 EC has increased due to improvements in endoscopic techniques and increased awareness of disease prevention.Approximately 90% of EC are squamous cell carcinoma (SCC) and vary by geographical region,with SCC being more common in Central Asia and China[2].According to the depth of infiltration,cT1N0M0 EC is classified as mucosal carcinoma (T1a) and submucosal carcinoma (T1b),regardless of lymph node status.
In the European Society of Endoscientific Oncology and the National Comprehensive Cancer Network guidelines,endoscopic resection is recommended for mucosal (T1a) lesions,surgical resection is recommended for patients with submucosal (T1b) lesions,and definitive chemoradiotherapy (d-CRT) is recommended for patients who are unable or unwilling to undergo surgery[3,4].Endoscopic resection can accurately stage the patients,reduce the surgical complications,and achieve the effect of curative resection[5-7],but carries a higher risk of recurrence (especially for large lesions).And radical esophagectomy is usually associated with postoperative complications,including anastomotic fistula,vocal cord paralysis,and pneumonia[8].
d-CRT is the standard treatment for patients with locally unresectable esophageal squamous cell carcinoma (ESCC) and an alternative treatment option for locally resectable ESCC[9-13].However,in clinical practice,d-CRT is often selected as an alternative therapy for cT1N0M0 EC patients,depending on the comorbidities,tumor localization,and widespread expansion.Few reports have described the use of d-CRT in patients with stage I ESCC.A parallel group controlled trial conducted in Japan found that the survival of CRT in cT1bN0M0 ESCC was comparable to surgery and had acceptable toxicity[14].However,the trial was conducted in Japan,and it was not clear about the generalizability of the evidence to different countries,while elderly patients and those not medically fit for surgery were excluded or underrepresented in the trial,and the study mainly included thoracic EC,thus questioning the generalizability of the results.Given the lack of sufficient evidence for the comparative efficacy of different treatments in cT1N0M0 EC,especially the role of d-CRT,we conducted this first retrospective study to compare the efficacy and complications of endoscopic submucosal dissection (ESD),surgery and d-CRT.
MATERIALS AND METHODS
Patient selection
We retrospectively analyzed patients with cT1N0M0 EC treated with ESD,surgery and d-CRT between January 2017 and December 2019 at the Cancer Center of Sun Yat-sen University.The inclusion criteria were as follows: (1) All patients met the diagnostic criteria for cT1N0M0 EC: the tumor tissue was limited to the esophageal mucosa or submucosa without lymph node or distant metastasis (cT1N0M0),and the diagnosis was made by endoscopy,pathological biopsy and imaging evaluation;(2) Patients with histology of SCC or precancerous lesions;(3) Patients without other concomitant malignancies;and (4) Patients with complete clinical medical records.
The study was performed in accordance with the guidelines of the Declaration of Helsinki and was approved by the institutional review board of the Sun Yat-sen University Cancer Center.
Preoperative and postoperative evaluation
The preoperative and postoperative evaluations mainly included endoscopic,imaging and histopathological examinations.Endoscopic examinations were performed by physicians with more than 6 years of endoscopic experience in the Department of Endoscopy of Sun Yat-sen University Cancer Center.Endoscopic examinations generally included conventional endoscopy with white light imaging for all lesions;magnifying endoscopy with narrow-band or blue laser imaging (commonly referred to as ME-NBI/BLI) using a GIF-H260Z (Olympus Corporation,Tokyo,Japan) or EG-L590ZW gastroscope (Fujifilm Corporation,Tokyo,Japan) for suspicious lesions;ultrasound endoscopy utilizing 7.5 MHz,10 MHz,or 12 MHz radical scanning probes (SU 9000,EG-530UR2,Fujifilm;EU-ME2,Olympus) or a 20-MHz miniature probe (UM-DP20-25R,Olympus) was applied for identifying the depth of tumor infiltration or metastasis of lymph nodes.Preoperative enhanced computed tomography (CT),magnetic resonance or positron emission tomography/CT were performed to assist in the diagnosis of esophageal carcinoma.Postoperative follow-up examinations were started 1-2 mo after the end of treatment,once every 3 mo during the initial 2 years,once every 6 mo from 2 to 5 years,and once a year after 5 years.R0 resection was defined as complete resection of the tumor,and histopathology showed a negative resection margin and no tumor residue after ESD or surgery therapy.Complete response (CR) was defined as the disappearance of the primary tumor and the absence of irregular erosive lesions,ulcerative lesions,or apparently elevated lesions as observed during endoscopy and/or the absence of malignant cells in biopsy specimens after d-CRT therapy[15].
ESD,surgery and d-CRT
ESD was performed by endoscopists with extensive experience.All inpatients were placed in the left lateral position with general anesthesia under tracheal intubation.The esophageal lesion was stained with Lugol solution,and the resection margin was marked with adenomatous polyposis coli or high-frequency electrocoagulation.A mixed liquid (0.9% NS: Sodium hyaluronate=4:1) was injected into the submucosa,the submucosa was dissected on the surface of the intrinsic muscular layer after circumferential incision outside the marked points,and the lesion was completely excised.Finally,the specimen was laid flat,fixed on a cork board with pins,soaked in formalin and sent for pathological examination.The intrinsic muscular layer of the esophagus was carefully examined endoscopically for any additional damage or residual tumor at the resection margin.The decision to add other additional treatments was made after a thorough evaluation based on the pathological findings and the therapeutic wishes of the patient and their family.In this study,2 patients underwent radical EC resection after ESD because of the positive resection margin of the pathological specimen.
Surgery was performed by experienced surgeons in our hospital.After general anesthesia was stabilized,the patients were placed in a supine position.After routine disinfection,surgeons removed the esophageal tumors,dissected the peripheral lymph nodesviathoracotomy or thoracoscopy and reconstructed the digestive tract using a laparotomy or laparoscopic approach.In this study,the pathological examination of 1 patient after esophagectomy indicated that tumor cells were visible at the resection margin of the specimen,so an extended surgical procedure was implemented.
The d-CRT regimen was discussed and decided by physicians with extensive experience in the medical oncology and radiotherapy departments of our hospital.d-CRT consisted of 5 courses of albumin paclitaxel (45-60 mg/m2) and cisplatin (20-25 mg/m2) on Day 1 every week along with concurrent radiotherapy by the intensity-modulated radiotherapy technique.Radiation therapy was delivered using megavoltage equipment (≥ 6 MV).The patients were treated 5 d per week at 1.8 to 2.0 Gy/d for a total dose of 60 Gy.The target volume of radiotherapy was individualized according to the primary tumor site and metastasis.The clinical target volume of mid-thoracic EC was defined as the gross tumor volume with a 3 cm margin for upper and lower extents and the lymph node target volume (gross tumor volume-nd) with a 0.5 to 1 cm margin for three-dimensional extents.The planned target volume was decided according to the actual positional error and was generally formed by a 0.5 cm margin for three-dimensional outward extents based on the clinical target volume and a 0.3 cm margin for cervical or upper thoracic EC fixed by head,neck and shoulder mesh.
Statistical analysis
The statistical methods used in this study included Student'sttest (or Mann-WhitneyUtest) and Fisher's exact test (or Pearson's chi-square test).The mean ± standard deviation for normally distributed measures was expressed byttest and the median and interquartile range [M (P25,P75)] for nonnormally distributed measures were expressed by rank sum test;the count data were expressed as percentages (%) and compared by chi-square test (χ2test).To account for selection bias and potential cofounding factors between groups in comparisons of outcome,we performed weighted propensity score analysis to control for differences in baseline characteristics between patients who underwent ESD,surgery and d-CRT.The propensity model was generated using the inverse probability treatment weighting (IPTW) method.Each patient was weighted by inverse probability with the goal of balancing observable features.The Bonferroni correction was needed as a conservative method for probability thresholding to control the occurrence of false positives.The 3-year overall survival (OS) and recurrence-free survival (RFS) were calculated and expressed as months.OS was right censored if the patient was alive at study termination or was lost to follow-up,and patient death was considered an event.In RFS analysis,the recurrence of EC after eradication therapy was considered an event.The follow-up period was calculated from treatment,and the cutoff date was October 30,2022.Follow-up ended when patients died or were lost to follow-up and cause of death and cause of loss analysis was analyzed.Time to recurrence was calculated from the time of treatment to the time of the most recent endoscopic evaluation at our facility or another hospital.The survival curves were plotted using the Kaplan-Meier method,and OS and RFS rates of therapeutic groups were compared by log-rank test.Cox proportional hazards modeling was used to assess the hazard ratios (HRs) and 95% confidence intervals (CIs).All data were analyzed by SPSS version 25.0 (IBM Corp.,Armonk,NY,United States) and R version 4.3.1.All tests were two-sided with a significance level ofP< 0.05.
RESULTS
Patient characteristics and complications
A total of 3911 patients with EC were treated in our hospital between January 2017 and December 2019,including 75 patients with precancerous esophageal lesions and 472 patients with cT1N0M0 EC.After exclusion,we retrospectively analyzed cT1N0M0 EC patients who underwent ESD (n=99) or surgery (n=220) or d-CRT (n=16) at our hospital.Tables 1 and 2 show the baseline characteristics and complications of patients in the ESD,surgery and d-CRT groups before and after IPTW adjustment.
Before IPTW adjustment,patients in the d-CRT group were older than those in the ESD and surgery groups.In the d-CRT group,there were 6 patients with clinical stage T1a (cT1a: M1-2),of whom 4 (66.7%) achieved CR,and 10 patients with clinical stage T1b (cT1b: M3-SM1-3),of whom 8 (80.0%) achieved CR.Among the cT1a patients,an 87-year-old patient developed more serious radiotherapy toxic side effects such as radiation pneumonia and finally died despite achieving CR,while 1 patient who did not achieve CR died of EC and severe complications of radiotherapy.Among the cT1b patients,severe complications were observed in 4 patients who achieved CR and survived,including 3 patients with esophageal stricture and 2 patients with radiation pneumonia.In contrast,1 patient who did not achieve CR died after receiving additional treatments because of lymph node metastasis.Patients in the surgery and d-CRT groups had more complications than those in the ESD group.Esophageal stricture was the main postoperative complication (surgeryvsESDvsd-CRT: 17.7%vs4.1%vs18.8%,P=0.004).
While after IPTW adjustment,the covariate balance in the three groups was improved;the number of background factors withPvalue above 0.05 was increased from 1 to 7.Complication rates were similar in the three groups,with allPvalues > 0.05.
Hospitalization costs and follow-up
Table 3 shows the hospitalization costs and remedies after recurrence or metastasis in the ESD,surgery and d-CRT groups.The median follow-up time was 42.0 mo (95%CI: 35.0-60.2) in the ESD group,45.0 mo (95%CI: 34.0-61.75) in the surgery group and 32.5 mo (95%CI: 28.3-40.0) in the d-CRT group.The ESD group had the lowest hospitalization costs,while the d-CRT group had the highest hospitalization costs among the three groups.One patient died of EC in the ESD group.In the surgery group,16 patients died of progression or metastasis of EC (84.2%),2 patients died of postoperative multiorgan failure,and 2 patient died of severe respiratory disease.Two patients died of EC,and one patient died of severe complications of radiation therapy in the d-CRT group.During the follow-up period,4 patients developed recurrence or metastasis (4.0%),and 3 patients underwent surgical resection of the lesions in the ESD group,while 38 patients in the surgery group developed recurrence or metastasis (17.3%),and 31 patients underwent salvage treatments.Additionally,1 patient in the d-CRT group was treated with palliative chemoradiotherapy after recurrence or multiple metastases.
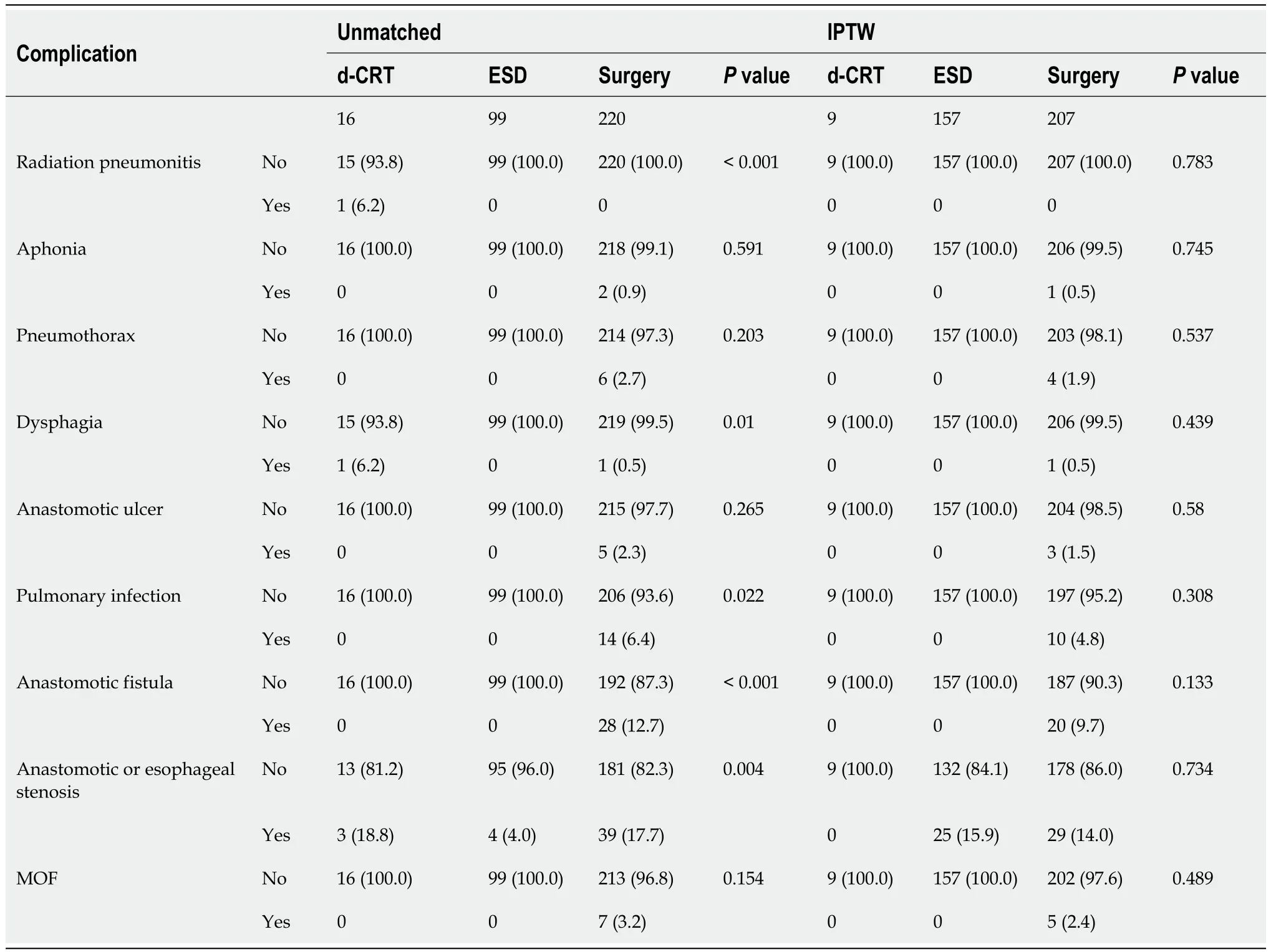
Table 2 Complications before and after inverse probability of treatment weighting adjustment of patients treated by endoscopic submucosal dissection,surgery and definitive chemoradiotherapy
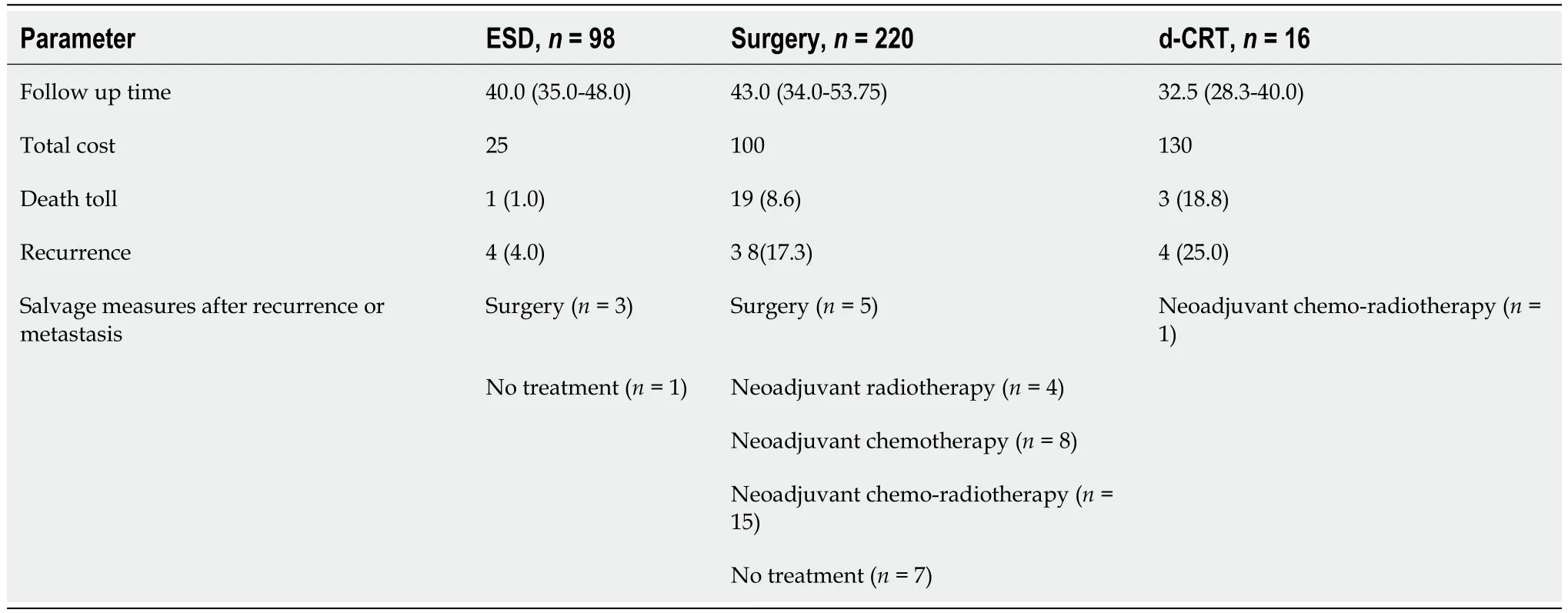
Table 3 Incidence of hospitalization costs and salvage treatments after recurrence or metastasis before inverse probability of treatment weighting adjustment
Survival analysis
To compare 3-year OS and RFS in the ESD,surgery and d-CRT groups,the survival analysis was performed with IPTW adjustment and using Bonferroni correction to control the occurrence of false positives.Figure 1 shows the Kaplan-Meier survival curves before and after IPTW adjustment.The 3-year OS and RFS of ESD were superior to those of surgery and d-CRT (OS: ESD: 99.7%,surgery: 94.7%,d-CRT: 79.1%;RFS: ESD 98.3%,surgery: 87.4%,d-CRT: 79.1%).
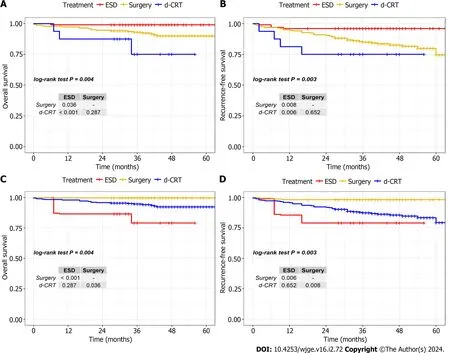
Figure 1 Overall survival and recurrence-free survival of endoscopic submucosal dissection,surgery and definitive chemoradiotherapy before and after inverse probability of treatment weighting analysis. The small table in the figure represents the results obtained from a two-by-two comparison of the survival rates of the three groups.A: Survival curves of overall survival (OS) for patients before inverse probability of treatment weighting (IPTW) adjustment;B: Survival curves of recurrence-free survival (RFS) for patients before IPTW adjustment;C: Survival curves of OS for patients after IPTW adjustment;D: Survival curves of RFS for patients after IPTW adjustment.d-CRT: Definitive chemoradiotherapy;ESD: Endoscopic submucosal dissection.P value was calculated by the log-rank test.
We further investigated the risk factors for OS and RFS in the different treatment modalities.Figure 2 shows the results of the Cox proportional hazards model for OS and RFS after IPTW adjustment.Multivariate analysis showed that treatment method,histology and depth of infiltration were independently associated with OS and RFS.
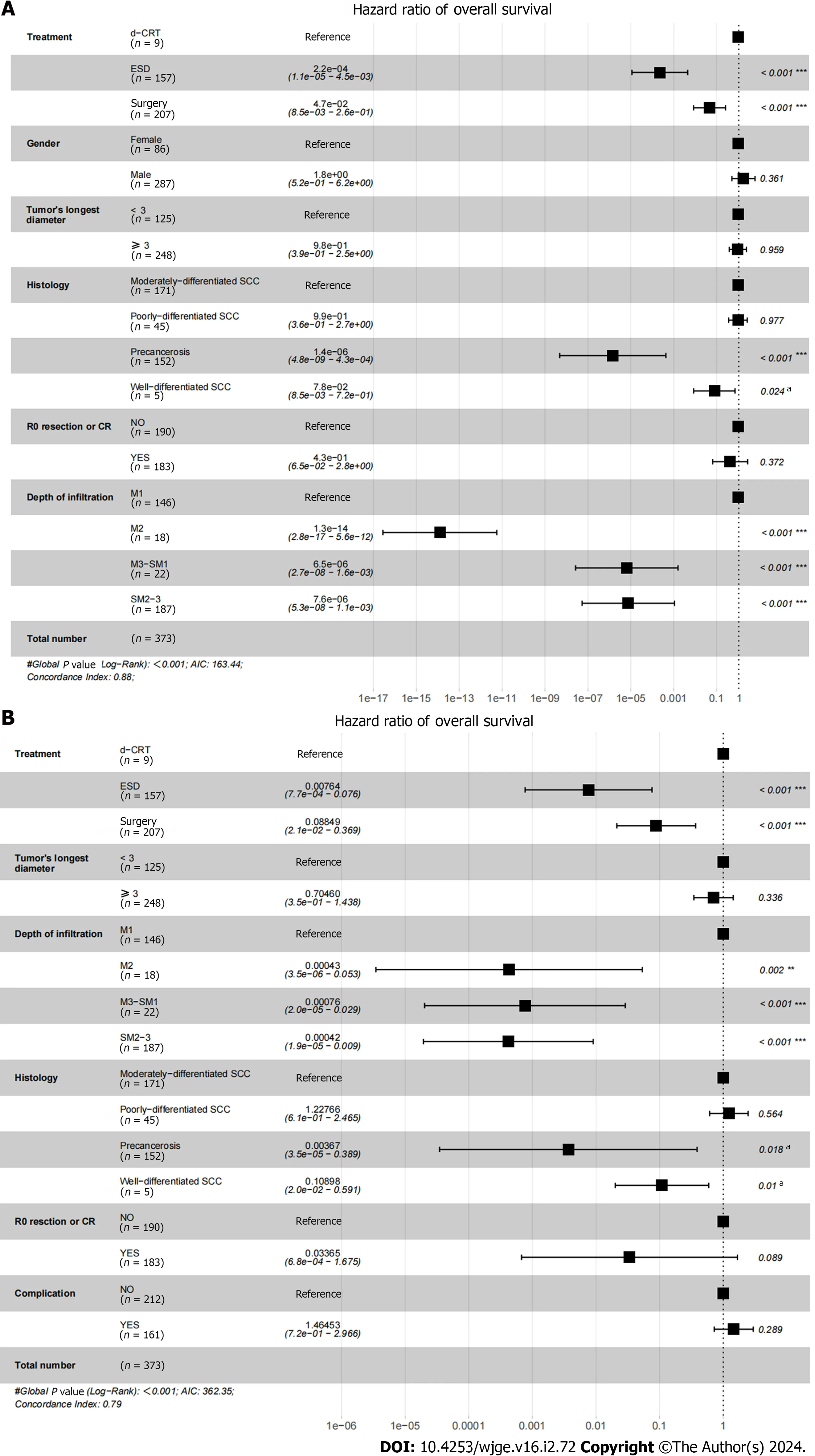
Figure 2 Cox regression estimates of overall survival and recurrence-free survival after inverse probability of treatment weighting
DISCUSSION
Many studies have compared the outcomes of ESD and surgery,or surgery and CRT in the treatment of cT1N0M0 EC,but there is a lack of studies directly comparing the efficacy and safety between ESD,surgery and d-CRT.After analyzing our included patients’ clinical data before and after IPTW adjustment,we found that ESD yielded better OS,RFS rates and lower hospitalized costs than surgery and d-CRT.Multivariate analysis showed that treatment method,histology and depth of infiltration were independently associated with OS and RFS,and it was similar to the previous study[16].
We explored the reasons for the difference in 3-year OS and RFS between the three treatments.We found that the depth of infiltration was more superficial in patients in the ESD group and that the local oncological control rate with ESD or surgery was higher,so patients could achieve tumor-free status to a greater extent.Patients in the d-CRT group were generally older and had high-grade and larger tumors,so EC was more likely to progress to an advanced stage and couldnot achieve CR.Our study showed that the rates of CR and severe complications for patients who received d-CRT were 75.0% and 43.8%,respectively,a relatively lower curative rate and higher complication rate than ESD and surgery.Those factors were perhaps associated with the significant difference in 3-year OS and RFS between the ESD,surgery and d-CRT groups.
Besides,the severe complications were similar among patients treated by these therapies.But we found that esophageal stricture was the major complication of the three treatment methods.Several previous studies have shown that the circumferential extent of the tumor and infiltration depth were independent risk factors for esophageal stricture[17-19].Currently,clinical measures for the prevention and treatment of postoperative esophageal stenosis include esophageal dilatation,esophageal stent placement,mucosal injection or oral steroid hormone[20-22].Meanwhile,somenovel techniques are being investigated by other scholars[23,24].However,the effectiveness of these methods requires more clinical evidence and there is no ideal therapy in current clinical practice,so we are also conducting relevant research on this aspect.
By comparing the efficiency and complication rate between ESD,surgery and d-CRT,we summarize the experience of our center: for early EC with infiltration to M1 or M2,no lymph node metastasis,no distant metastasis,and circumferential extent of tumor < 3/4,ESD was the preferred therapy.In particular,for patients with cervical or upper thoracic esophageal carcinoma,ESD is better than surgery.d-CRT should be attempted for patients who are of advanced age,frail,contraindicated to surgery and have an upper and circumferential extent of ≥ 3/4.
In this study,we firstly conducted a retrospective study with a large sample size to compare the efficacy of early EC treated with ESD,surgery and d-CRT,providing some useful suggestions.However,there are some limitations in our study.First,the sample size of our study was still not large enough,especially because the number of patients in the d-CRT group was insufficient.Second,the study was a single-center retrospective study,which has considerable limitations.Last,the data were obtained mainly from the medical records and follow-up,so there was a certain rate of missing visits and missing data.Therefore,multicenter prospective studies with larger sample sizes or randomized controlled studies are needed to supplement the evidence of our study.
CONCLUSION
This is a first retrospective study to compare OS,RFS and complications of ESD,surgery and d-CRT.In this study,we found that ESD attained better survival benefits and lower hospitalization costs than surgery and d-CRT,and they had similar complications rates.This study provides a more comprehensive analysis of the efficacy and safety of current
analysis among patients with cT1N0M0 EC who underwent endoscopic submucosal dissection,surgery and definitive chemoradiotherapy.A: Multivariate analysis showed that treatment method,histology and depth of infiltration were independently associated with overall survival;B: Multivariate analysis showed that treatment method,histology and depth of infiltration were independently associated with recurrence-free survival (RFS).CR: Complete response.(*) represents the significant difference,and the more the number of “a”,the greater the difference.
cT1N0M0 EC treatment patterns and provides new evidence for the use of ESD in cT1N0M0 EC.
ARTICLE HIGHLIGHTS
Research background
For cT1N0M0 esophageal cancer (EC),the current study has mainly focused on surgery and endoscopic submucosal dissection (ESD),while definitive chemoradiotherapy (d-CRT) is a complementary treatment for cT1N0M0 EC.Studies on estimating the therapeutic effect and safety of d-CRT,surgery and ESD are not sufficient,so this study is important.
Research motivation
Early-stage EC is currently increasing year by year,and its treatment methods are also changing rapidly.It is very important to choose the treatment methods with good prognosis and fewer complications,while some patients have the dilemma of treatment choice due to age,cost and other reasons.It is very important to summarize and compare the advantages and disadvantages of the existing treatment methods,which is very important for the health management of patients with EC.
Research objectives
By comparing the efficiency and safety of ESD,surgery and d-CRT for cT1N0M0 EC,to provide a clinical basis for the treatment selection of cT1N0M0 EC and to achieve better prognosis and quality of survival for EC.
Research methods
We retrospectively analyzed the medical records,pathology,imaging and endoscopic findings,and follow-up results of the cT1N0M0 EC.We met the inclusion criteria and adjusted the effects of confounding factors using the inverse probability of treatment weighting method to conduct survival analysis,Cox proportional risk regression analysis,collected complications and costs,rescue measures after recurrence,and finally evaluated the efficacy and safety of cT1N0M0 EC patients receiving ESD,surgery and d-CRT.
Research results
Results showed that ESD had better survival outcomes,lower hospital costs and more acceptable occurrences of complications.This study provides a more comprehensive analysis of the efficacy and safety of current cT1N0M0 EC treatment patterns and provides new evidence for the use of ESD in cT1N0M0 EC.To our knowledge,our study is the first to compare the effects of all three treatments for cT1N0M0 EC.In addition,there are relatively few studies on d-CRT for cT1N0M0 EC patients,and our study can provide relevant evidence of d-CRT for cT1N0M0 EC,so it has a certain new innovation.
Research conclusions
This is a first retrospective study to compare overall survival,recurrence-free survival and complication rates of ESD,surgery and d-CRT,and show that ESD attained better survival benefits and lower hospitalization costs than surgery and d-CRT,and they had similar complication rates.This study provides a more comprehensive analysis of the efficacy and safety of current cT1N0M0 EC treatment patterns and provides new evidence for the use of ESD in cT1N0M0 EC.
Research perspectives
In the future,we will conduct a subgroup analysis of survival outcomes for the three therapies in cT1N0M0 EC patients,and investigate methods to reduce the occurrence of complications.
FOOTNOTES
Co-first authors:Shu-Ai Luo and Yu-Ying Sun.
Author contributions:Huang CY designed and performed the research and supervised the report;Luo SA performed the research,collected the data,wrote the paper and contributed to the analysis;Sun YY supervised the report,wrote the paper and revised the paper;Zeng YT contributed to the analysis and provided clinical advice.Luo SA and Sun YY have made crucial and indispensable contributions towards the completion of the project and thus qualified as the co-first authors of the paper.
Supported bythe Guangdong Esophageal Cancer Institute Science and Technology Program,No.M 202013;and Guangdong Medical Research Foundation,No.A2021369.
Institutional review board statement:All procedures in studies involving human participants were carried out in accordance with ethical standards and approved by the Ethics Committee (No.SL-B2023-032-01).
Informed consent statement:Patients were not required to give informed consent to the study because the analysis used anonymous clinical data that were obtained after each patient agreed to treatment by written consent.For full disclosure,the details of the study are published on the home page of Sun Yat-sen University Cancer Center.
Conflict-of-interest statement:The authors declare that they have no financial relationships to disclose.
Data sharing statement:The raw data used to support the findings of this study could be obtained by getting in touch with the corresponding author.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORCID number:Shu-Ai Luo 0000-0002-7473-8361;Yu-Ying Sun 0000-0002-5789-256X;Ya-Ting Zeng 0000-0002-2654-5979;Chun-Yu Huang 0000-0002-1346-5961.
S-Editor:Liu JH
L-Editor:Filipodia
P-Editor:Cai YX
杂志排行
World Journal of Gastrointestinal Endoscopy的其它文章
- Association between triglyceride-glucose index and colorectal polyps: A retrospective cross-sectional study
- Retrospective analysis of discordant results between histology and other clinical diagnostic tests on helicobacter pylori infection
- Coca-Cola consumption vs fragmentation in the management of patients with phytobezoars: A prospective randomized controlled trial
