Retrospective analysis of discordant results between histology and other clinical diagnostic tests on helicobacter pylori infection
2024-03-07XiaohuaQiKevinKuanTonyElJabbourYungtaiLoQiangLiuYananFang
Xiaohua Qi,Kevin Kuan,Tony El Jabbour,Yungtai Lo,Qiang Liu,Yanan Fang
Abstract BACKGROUND A reliable test is essential for diagnosing Helicobacter pylori (H. pylori) infection,and crucial for managing H. pylori-related diseases.Serving as an excellent method for detecting H. pylori infection,histologic examination is a test that clinicians heavily rely on,especially when complemented with immunohistochemistry (IHC).Additionally,other diagnostic tests for H. pylori,such as the rapid urease test (CLO test) and stool antigen test (SA),are also highly sensitive and specific.Typically,the results of histology and other tests align with each other.However,on rare occasions,discrepancy between histopathology and other H. pylori diagnostic tests occurs.AIM To investigate the discordance between histology and other H. pylori tests,the underlying causes,and the impact on clinical management.METHODS Pathology reports of gastric biopsies were retrieved spanning August 2013 and July 2018.Reports were included in the study only if there were other H. pylori tests within seven days of the biopsy.These additional tests include CLO test,SA,and H. pylori culture.Concordance between histopathology and other tests was determined based on the consistency of results.In instances where histology results were negative while other tests were positive,the slides were retrieved for re-assessment,and the clinical chart was reviewed.RESULTS Of 1396 pathology reports were identified,each accompanied by one additional H. pylori test.The concordance rates in detecting H. pylori infection between biopsy and other tests did not exhibit significant differences based on the number of biopsy fragments.117 discrepant cases were identified.Only 20 cases (9 with CLO test and 11 with SA) had negative biopsy but positive results in other tests.Four cases initially stained with Warthin-Starry turned out to be positive for H. pylori with subsequent IHC staining.Among the remaining 16 true discrepant cases,10 patients were on proton pump inhibitors before the biopsy and/or other tests.Most patients underwent treatment,except for two who were untreated,and two patients who were lost to follow-up.CONCLUSION There are rare discrepant cases with negative biopsy but positive in SA or CLO test.Various factors may contribute to this inconsistency.Most patients in such cases had undergone treatment.
Key Words: Helicobacter pylori;Discordance;Gastric biopsy;Histology;Rapid urease test;Stool antigen test;Helicobacter pylori culture
INTRODUCTION
Helicobacter pylori(H. pylori) infection is directly associated with chronic gastritis,gastric/duodenal ulcer,MALT lymphoma,and gastric adenocarcinoma[1-4].It is crucial to diagnoseH. pyloriinfection accurately and promptly for the clinical management of associated diseases[1].Various methods forH. pyloridetection,both invasive and noninvasive,have been developed[1,5].Invasive tests include histological examination,rapid urease test (CLO test),andH. pyloriculture.Noninvasive tests include urease breath test (UBT),stool antigen test (SA),and serology testing forH. pyloriantibody[1,5].
Each diagnostic method has its advantages and disadvantages.No single test is universally acknowledged as a gold standard for detectingH. pyloriinfection[4].A well accepted approach is combining two or more detection methods[4].The selection of diagnostic tests depends on various factors,including test availability,sensitivity,specificity,cost,and turnaround time.Although non-invasive tests like UBT offer high sensitivity and specificity for detectingH. pylori,upper gastrointestinal (GI) endoscopy with biopsy remains the preferred method,particularly for individuals over 60 or those with alarming symptoms,as recommended by the American College of Gastroenterology[6].In our hospital,the initial evaluation for symptomatic patients typically involves gastric biopsy and another method.Commonly employed other tests include SA,CLO test,andH. pyloriculture.Clinicians place particular emphasis on the morphological assessment of gastric biopsy,especially when combined with immunohistochemistry (IHC),considering it one of the most accurate methods.While the results of other clinical tests generally align with biopsy findings,occasional rare discrepancies may pose challenges for clinicians,especially in cases where biopsy results are negative but other clinical tests are positive.
This study aims to clarify and characterize the discrepancies between various diagnostic tests and histological interpretations.A retrospective study is conducted to compare the results of gastric biopsy diagnoses with otherH. pyloridiagnostic tests.Additionally,ancillary tests used for the histologic diagnosis ofH. pylori-associated gastritis are evaluated.
MATERIALS AND METHODS
Data collection
The research received approval from the Institutional Review Board of the hospital (2016-6957).Pathology reports of gastric biopsies were extracted from the hospital's in-house database using Clinical Looking Glass (version 4.4.2) spanning from August 2013 to July 2018.Reports were chosen based on specimens originating from the stomach,with comments indicating the presence or absence ofH. pyloriorganism.Inclusion criteria mandated the presence of otherH. pyloridiagnostic tests conducted within seven days of the biopsy.Other clinical tests included in the study were: (1) Rapid urease test (CLO test);(2) stool antigen test (SA);and (3)H. pyloriculture.In instances of multiple tests within a two-week window,the result closest to the biopsy date was considered.Data extracted from the reports included the number of stomach biopsy fragments collected during endoscopy,procedure dates,H. pyloristatus,and the stains used for histologic diagnosis.Test results were considered concordant when both biopsy and clinical tests provided the same diagnosis forH. pyloriinfection;otherwise,they were labeled as discordant.In cases where a negative biopsy with a positive clinical test were identified,histologic slides were retrieved for re-assessment,and the patient's chart was reviewed.
Statistical analysis
The inter-test agreement between histology and another diagnostic test (CLO test,H. pyloriculture,or stool test) for detectingH. pyloriinfection was assessed utilizing the kappa statistic.An excellent agreement was defined as a kappa value ≥ 0.75,fair to good agreement as a kappa value between 0.4 and 0.75,and poor agreement as a kappa value < 0.4.Concordance referred to the alignment between histology and another diagnostic test onH. pyloridetection,with the concordance rate calculated as the number of concordant cases divided by the total number of cases.Differences in concordance rates among various diagnostic tests with histology in detectingH. pyloriinfection were assessed using chisquare tests.Statistical analyses were conducted using SAS version 9.4 (SAS Inc.,Cary,NC,United States),and p-values of 0.05 or less were deemed statistically significant.
RESULTS
A total of 1396 pathology reports were identified.The majority of biopsies (n=1199) were stained solely with Warthin-Starry (WS) stain.Only a small number of cases were reported withH. pyloriIHC stain only (n=81),both WS and IHC stains (n=60),or no special stain used (n=56) (Table 1).Among them,392 cases tested positive forH. pylorithrough morphological examination,with WS stain,and/or with IHC.Each biopsy was accompanied by only one additionalH.pyloritest (CLO test,SA,orH. pyloriculture).Both CLO test andH. pyloriculture were invasive,conducted on the day of the biopsy.SA was performed within seven days of the biopsy.The summary of additional test results (CLO test,SA,orH. pyloriculture) is presented in Table 2.
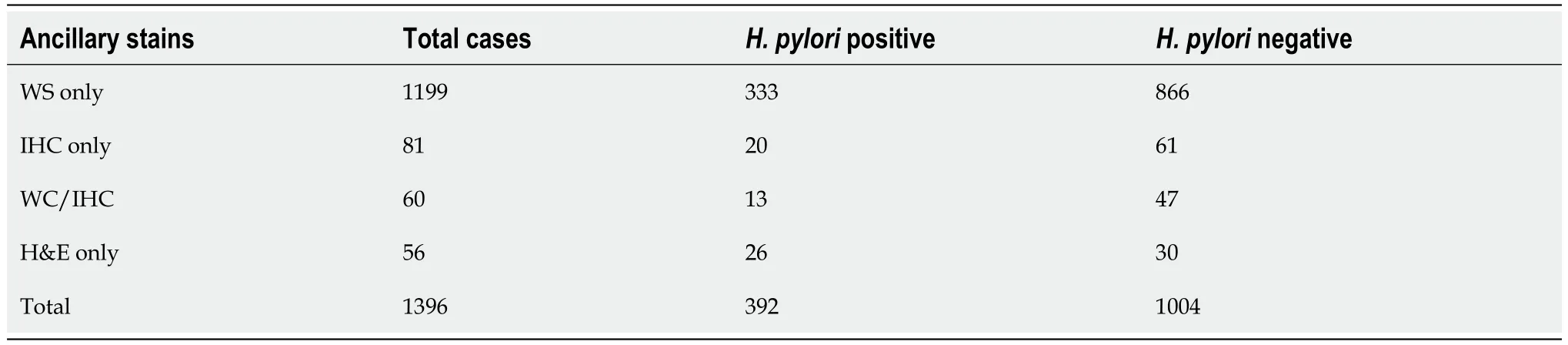
Table 1 Gastric biopsy cases with ancillary stains
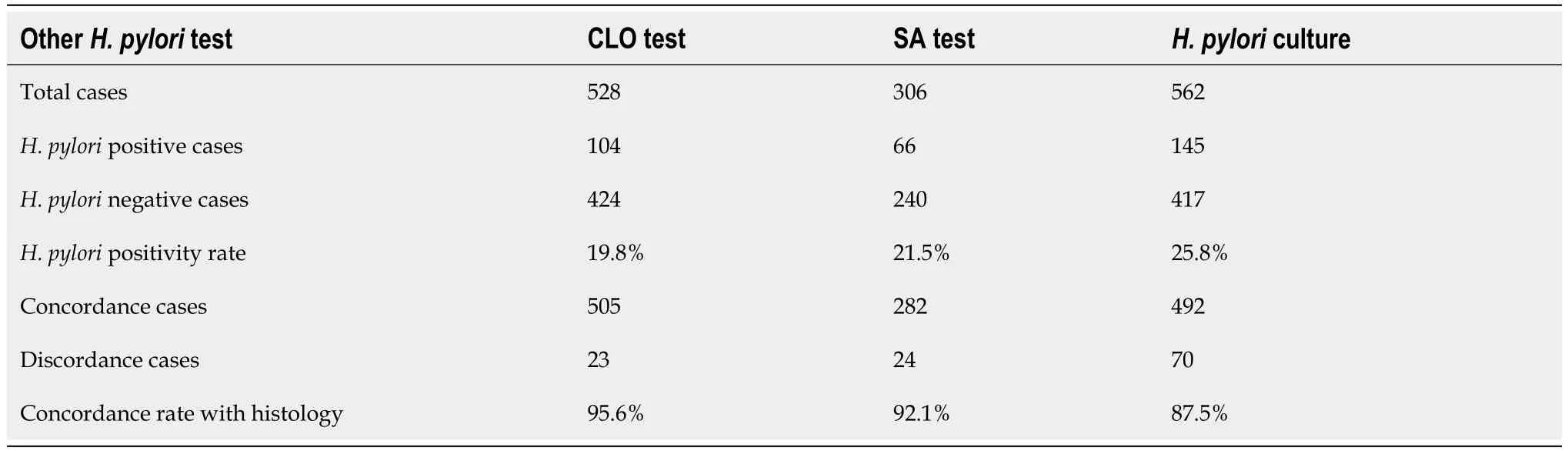
Table 2 Concordance rate between histology and three other Helicobacter pylori tests
The overall concordance rate between histology and other diagnostic tests was high (n=1279;91.6%).CLO test and stool antigen tests demonstrated significantly higher concordance rates with biopsy in detectingH. pyloriinfection compared toH. pyloriculture (95.6% for CLO testvs92.2% for SAvs87.5% for culture;P< 0.001) (Table 2).The estimated kappa statistic for assessing agreement in identifyingH. pyloriinfection between histology and other diagnostics were 0.86 for CLO test (95%CI: 0.81–0.92;Table 3),0.77 for stool antigen test (95%CI: 0.68–0.86;Table 4),and 0.72 for culture (95%CI: 0.66–0.78;Table 5) respectively.
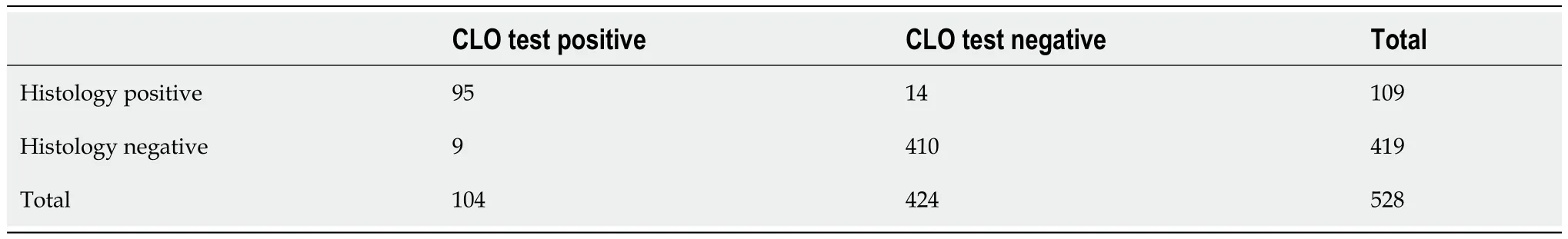
Table 3 Assessment of concordance between histology and rapid urease test
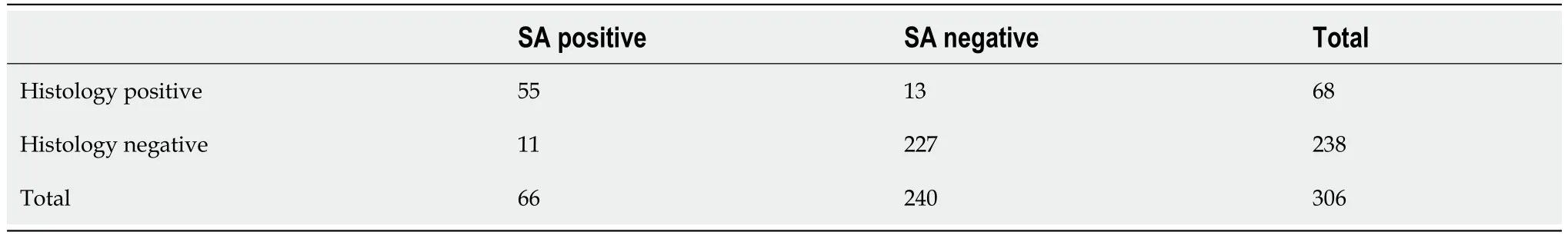
Table 4 Assessment of concordance between histology and stool antigen test
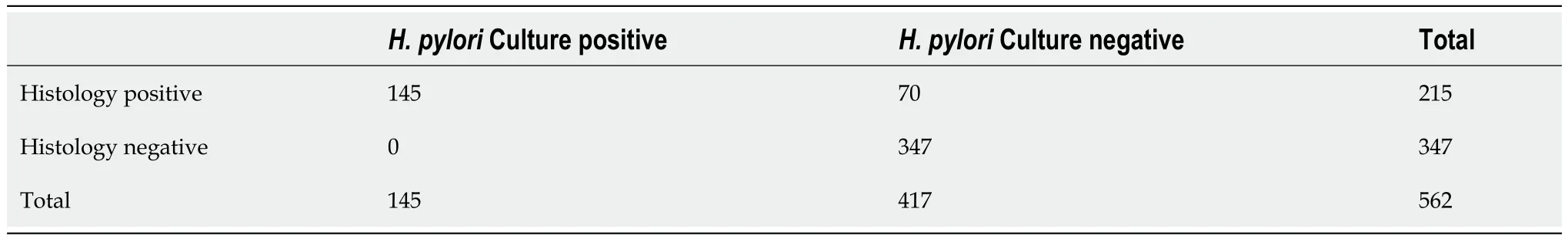
Table 5 Assessment of concordance between histology and Helicobacter pylori culture
The correlation between concordance rates and the number of biopsy fragments was also examined (Figure 1).The number of biopsy fragments exhibited considerable variation across cases,ranging from 1 to 6 or more: 83 cases (1 fragment),321 cases (2 fragments),229 cases (3 fragments),262 cases (4 fragments),132 cases (5 fragments),and 364 cases (6 fragments and above).Additionally,5 cases lacked information on fragment numbers.Notably,the concordance rates in detectingH. pyloriinfection between biopsy and other clinical diagnostic tests did not differ significantly by the number of fragments (88.0%vs93.5%vs92.1%vs92.7%vs93.2%vs89.2%,P=0.268;Figure 1).
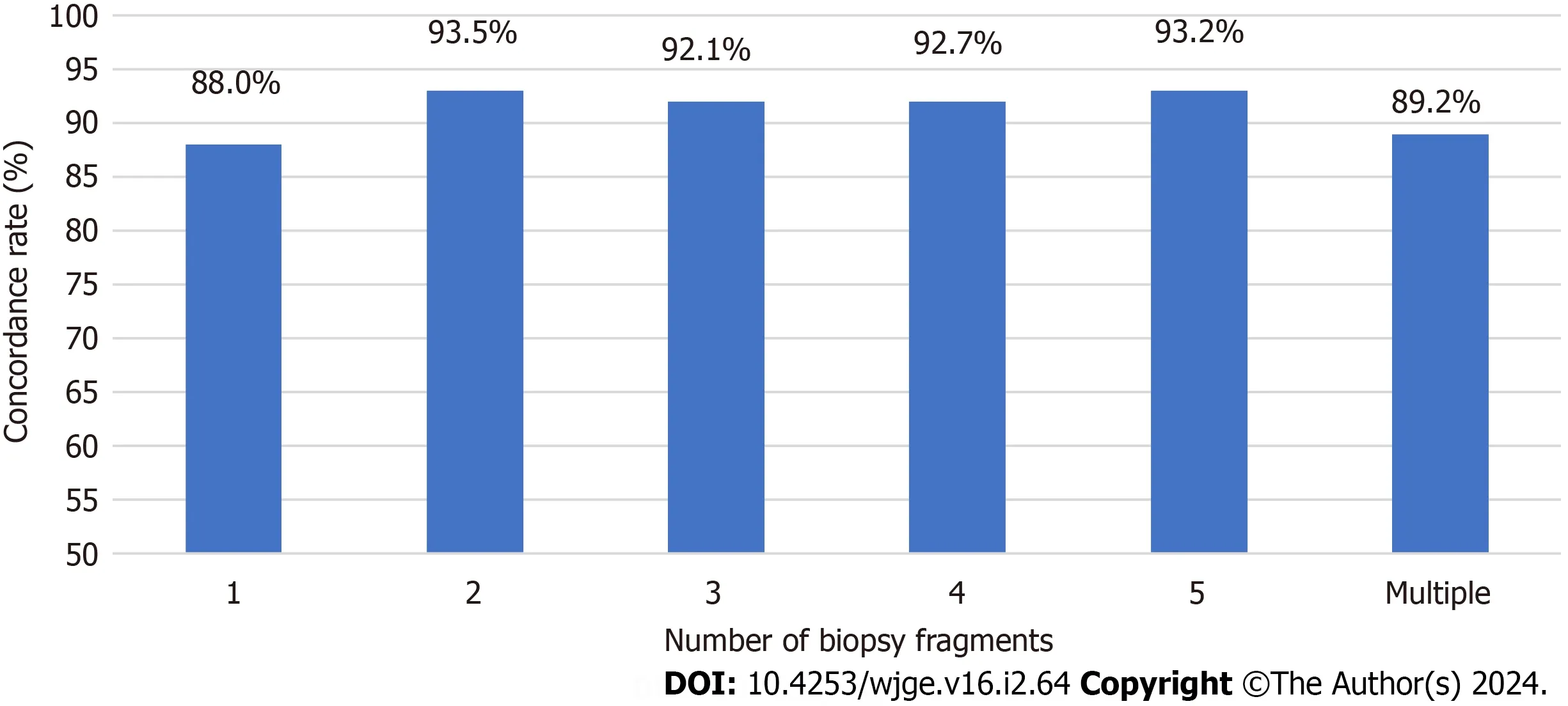
Figure 1 Concordance rate between histology and other Helicobacter pylori tests based on numbers of biopsy fragments. Multiple: 6 fragments and up.Concordance rate is labeled on top of each column.
The majority of cases exhibiting discordance were those with a positive biopsy but negative results in otherH. pyloritests (97 cases).Among these cases,a significant proportion involved bacterial culture (70 cases).Additionally,there were14 instances of negative CLO tests and 13 cases with negative SA tests,despite a positive histological diagnosis.Conversely,there were only 20 cases with negative biopsy results but positive results in other tests (SA or CLO test;Tables 3-5).All 20 cases were reported to exhibit chronic inactive inflammation on histological examination,with one case also displaying focal active gastritis.No atrophy was observed in any case.Sixteen cases were available for reassessment,with IHC staining performed on those cases not previously tested.In this reevaluation,four cases were found to be positive forH. pyloriby IHC,despite previous reports indicating negativity.A review of the original H&E slides and WS stains for these four cases revealed the presence of rare and/or morphologically atypicalH. pyloriorganisms.Among them,all four cases showed inactive chronic gastritis,and one exhibited focal chronic active gastritis.Additionally,it was observed that three of these patients were under proton pump inhibitor (PPI) treatment at the time of biopsy.Consequently,these four cases were excluded from subsequent assessment.Among the remaining 16 'true' discrepant cases,only four cases had four or more fragments from gastric biopsy,while 12 had three fragments or fewer submitted for histologic examination.Ten cases were on PPI either when biopsied and/or tested for SA (Table 6);six were on PPI when biopsied but not tested for SA;three were on PPI when biopsied and tested;while one was on PPI only when tested for SA but not biopsied.Additionally,three cases (case 8,9,and 15) were on antibiotics in addition to PPI when biopsied,as the treatment (triple or quadruple therapy) was initiated after a positive SA result a few days before the biopsy procedure.The majority of patients received treatment forH. pyloriinfection,with the exception of two patients who were untreated,and two patients who were lost to follow-up (Table 6).According to the clinical chart,the decision for treatment was determined by various factors,including clinical presentation,endoscopy findings,pathology results other thanH. pyloriinfection status,and occasionally repeated biopsy or otherH. pyloritests (as observed in cases 13 and 15).
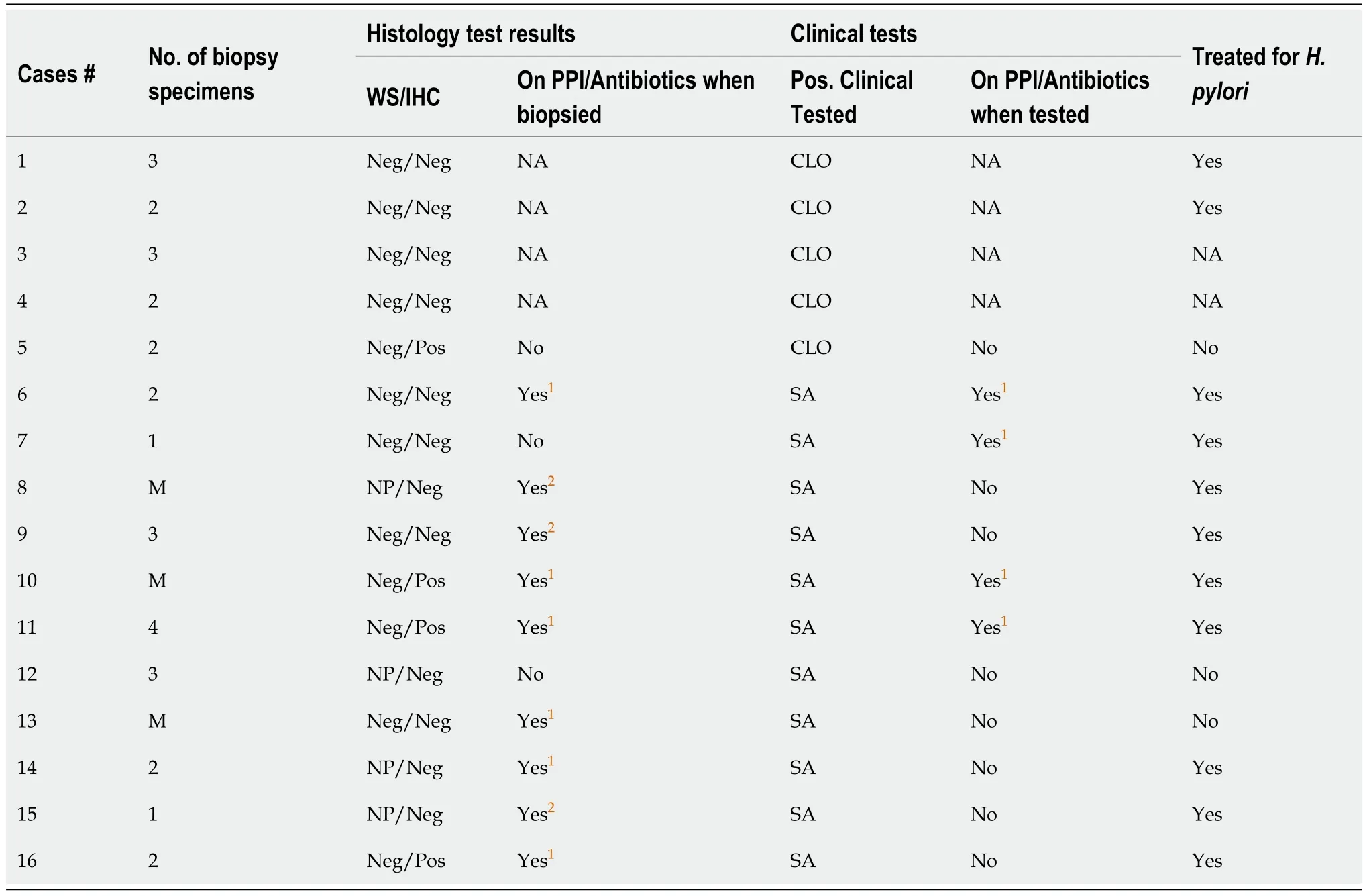
Table 6 Discrepant cases with negative histology but positive rapid urease test or stool antigen test
DISCUSSION
While histology is commonly regarded as the preferred method for symptomatic patients[6,7],otherH. pyloridiagnostic tests are equally crucial,often being more convenient,less invasive,and cost-effective,yet maintaining high sensitivity and specificity[4].Discrepancies between biopsies and the results of otherH. pyloridiagnostic tests can occasionally arise.No single test is considered the gold standard alone[4].Nevertheless,clinicians prioritize the morphological assessment of gastric biopsies,especially when augmented with immunohistochemistry,considering it as one of the most accurate approaches.Negative clinical test results may be deemed false negatives when the corresponding biopsy is positive.However,the discrepancy between a negative biopsy and a positive clinical test result can pose a challenge for physicians.This study's objective is to elucidate and characterize the discordance between histopathology and other clinical diagnostic tests in determiningH. pyloristatus.
The CLO test,SA test,andH. pyloribacterial culture were selected for comparison with histology,as they are the most employed tests in conjunction with upper GI endoscopy at our hospital.Both the CLO test and SA test exhibit high sensitivity and specificity,whileH. pyloriculture has nearly 100% specificity with slightly lower sensitivity[4].Our findings indicate excellent agreement between histology and the CLO test and stool antigen test (with Kappa values exceeding 0.75).H. pyloriculture demonstrates a slightly lower but still commendable concordance rate (Kappa value of 0.72) mainly due to its higher false negative rate.
The sensitivity and diagnostic accuracy ofH. pyloriare impacted by the sampling during biopsy.It is recommended by the Sydney protocol[8] to submit four biopsy samples forH. pyloridetection: Two from the antrum and two from the body.An additional sample from incisure angularis is advised for gastritis characterization[3,8].In our study,most cases have less than five biopsy fragments submitted (Figure 1),and there is no available data regarding the origin of these fragments.Interestingly,the number of gastric samples obtained during each endoscopy did not significantly influence the concordance rate between histological diagnosis and otherH. pyloritests in our study.However,it is essential to note that concordance does not equate to test accuracy,as concordant results can be either false positives or false negatives.Treatment status at the time of testing is unknown,and both results could be affected by PPI or antibiotics,even if they are concordant.
Most cases have WS stain for histologic diagnosis,as WS stains were automatically ordered from 2013 to 2015 at our hospital.WS stain was preferred overH. pyloriIHC stain due to its lower cost and quicker turnaround time.Recent studies indicate that ancillary stains provide little additional benefits to H&E stains forH. pyloridetection[2,9],particu-larly in cases without inflammation.Since 2016,there have been no further automated orders for special stains on GI biopsy in our laboratory,informed by both literature findings and our own experiences.In our investigation of discrepant cases,four biopsy cases initially reported as negative forH. pylorilater revealedH. pyloriorganisms through IHC.All four cases exhibited inactive chronic gastritis with one displayed focal active chronic gastritis.Upon re-examination of the H&E slides and WS stains,rare and/or morphologically atypicalH. pyloriorganisms were identified.Notably,three patients were noted to be on PPI,potentially altering bacterial appearance and making identification challenging with H&E andspecial stains[10,11].In this case,immunohistochemistry would help identify rare and/or morphological atypicalH.pyloriorganisms in cases with other evidence ofH. pyloriand inflammatory mucosa.
There are 16 discrepant cases,excluding 4 instances whereH. pyloriwas detected by IHC after initially being negative by H&E and WS.Several factors may contribute to the disparity between a negative biopsy and a positive CLO test or SA test.Firstly,the presence of organisms may be reduced or absent due to medications such as PPI and/or antibiotics[12].Additionally,these medications can alter the appearance of bacteria,making recognition challenging[3,11].Among the patients,10 were on PPI before the biopsy procedure and/or otherH. pyloritests,with the majority (6 cases) only taking PPI before biopsy,not before otherH. pyloritests.For these 6 cases,results from otherH. pyloritests are more likely reliable than histology.Secondly,sampling may contribute to the discrepancy,with 12 out of 16 cases having three fragments or fewer.Although the overall number of gastric samples does not significantly affect the concordance rate,as discussed previously,this may differ when patients are on PPI,particularly if they were on PPI for one test but not for another.Lastly,some results could be false positives from CLO test or SA tests,as both can yield false positive results[13-16].
It is important to note that despite conflicting results presented to clinicians,most patients received treatment without additional testing,except in two cases.This could be attributed to multiple factors,including limited test availability,insurance coverage constraints,challenges in discontinuing medications to minimize testing interference,or delays in treatment.The choice to pursue treatment is influenced by various factors,including clinical symptoms,endoscopic observations,pathology findings other thanH. pyloriinfection status,and occasionally the repetition of biopsies or otherH.pyloritests.
CONCLUSION
Our findings demonstrated that both CLO test and SA tests exhibit high concordance rates with histological diagnoses.The concordance rate between histology andH. pyloriculture is slightly lower,primarily attributed to the lower sensitivity of theH. pyloriculture assay.Importantly,the concordance rate shows no significant difference by the number of fragments obtained during the biopsy procedure.There are rare instances of discrepancies,whereH. pyloridiagnosis is negative by histology but positive by CLO test or stool antigen test.Multiple factors may contribute to these discrepancies.Even though histological examination showed negative results forH. pyloriin these cases with discrepancies,most patients still received treatment.Correlating with clinical history,past laboratory results,and follow-up testing may assist in clinical management.
ARTICLE HIGHLIGHTS
Research background
DeterminingHelicobacter pylori(H. pylori) status is essential in the management ofH. pylori-related diseases.No single test is universally recognized as the gold standard alone.Typically,symptomatic patients at our hospital undergo upper GI endo-scopy with biopsy,often accompanied by an additionalH. pyloritest.The results generally align with each other,although discrepancies arise occasionally.
Research motivation
The clinician places particular emphasis on gastric biopsy results,especially when supplemented with immunohistochemistry (IHC),often considering it the most accurate.Rare cases where biopsy results are negative while other clinical tests show positivity can present challenges for clinicians.
Research objectives
The goal of this retrospective study is to examine the discordance between histopathology and alternativeH. pyloritests,explore the underlying causes,and assess the implications for clinical management.
Research methods
Pathology reports of gastric biopsies were retrospectively retrieved from August 2013 to July 2018.Inclusion in the study required the presence of otherH. pyloritests within seven days of the biopsy,including rapid urease test (CLO test),stool antigen test (SA),andH. pyloriculture.The concordance between histopathology and other tests was evaluated based on result consistency.In cases where histology was negative while other tests showed positivity,the slides underwent reassessment,and the clinical chart was examined.
Research results
1396 pathology reports were identified,each accompanied by one additionalH. pyloritest.The concordance rates between biopsy and other tests did not show significant differences based on the number of biopsy fragments.117 discrepant cases were identified.Only 20 cases (9 with CLO test and 11 with SA) had negative biopsy but positive results in other tests.Four cases initially stained with Warthin-Starry stain turned out to be positive forH. pyloriwith subsequent IHC staining.Among the remaining 16 true discrepant cases,10 patients were on proton pump inhibitors before the biopsy and/or other tests.Most patients underwent treatment,except for two who were untreated,and two patients who were lost to follow-up.
Research conclusions
Our findings reveal that both SA and CLO test demonstrate high concordance rates with histological diagnoses.The concordance rate between histology andH. pyloriculture is slightly lower,mainly due to the lower sensitivity of theH.pyloriculture assay.Importantly,the concordance rate remains consistent regardless of the number of gastric biopsy fragments.Rare instances of discrepancies exist,whereH. pyloridiagnosis is negative by histology but positive by SA or CLO test.Multiple factors may contribute to the discordance.Despite histological examination showing negative results forH. pyloriin these cases with discrepancies,most patients still received treatment.Correlation with clinical history,past laboratory results,and follow-up testing may aid in clinical management.
Research perspectives
This retrospective study was conducted at a singular tertiary medical center.It would be intriguing to conduct similar retrospective research in other hospitals to compare discordance rates between histology and otherH. pyloritests and variations in clinical management.
FOOTNOTES
Co-first authors:Xiaohua Qi and Kevin Kuan.
Author contributions:Qi X and Kuan K contributed equally to this work;Fang Y and Liu Q designed the research study;Qi X and Kuan K performed the data extraction;Kuan K,Qi X,Jabbour T,Liu Y,and Fang Y performed the data analysis and interpretation of the results;Fang Y,Kuan K,and Qi X wrote the manuscript,Lo Y is a Biostatistics professor and performed the statistical analysis;Fang Y,Kuan K and Qi X revised the manuscript;and all authors read and approved the final version.
Institutional review board statement:This study was reviewed and approved by the Albert Einstein College of Medicine Institutional Review Board (IRB No: 2016-6957).
Informed consent statement:This is a retrospective study with a focus on quality assurance (QA).The institutional review board (IRB) granted a waiver of consent.
Conflict-of-interest statement:All the authors declare no conflicts of interest for this article.
Data sharing statement:De-identified dataset available from the corresponding author at yfang@montefiore.org.Participants gave informed consent for data sharing.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:United States
ORCID number:Xiaohua Qi 0000-0003-3706-7586;Kevin Kuan 0000-0001-6818-2179;Tony El Jabbour 0000-0002-6823-1919;Yungtai Lo 0000-0002-2694-4830;Qiang Liu 0009-0001-5769-1397;Yanan Fang 0000-0002-1112-9569.
Corresponding Author's Membership in Professional Societies:College of American Pathologists,1231720.
S-Editor:Liu JH
L-Editor:A
P-Editor:Xu ZH
杂志排行
World Journal of Gastrointestinal Endoscopy的其它文章
- Association between triglyceride-glucose index and colorectal polyps: A retrospective cross-sectional study
- Comparative efficacy and safety between endoscopic submucosal dissection,surgery and definitive chemoradiotherapy in patients with cT1N0M0 esophageal cancer
- Coca-Cola consumption vs fragmentation in the management of patients with phytobezoars: A prospective randomized controlled trial
