Acute coalescent mastoiditis in a 16-month-old child due to Streptococcus pneumoniae infection
2024-03-05MagdalenaPszczoowskaMonikaMorawskaKochmanKatarzynaReslerKatarzynakalskaTomaszZatoski
Magdalena Pszczołowska ,Monika Morawska-Kochman ,Katarzyna Resler ,Katarzyna Pękalska ,Tomasz Zatoński
1Department and Clinic of Otolaryngology,Head and Neck Surgery,Wrocław Medical University,Borowska 213,Wrocław,Poland
2Department of General Radiology,Interventional Radiology and Neuroradiology,Wrocław Medical University,Borowska 213,Wrocław,Poland
ABSTRACT Rationale:Acute otitis media is a common disease in early childhood,and is usually caused by Streptococcus pneumoniae (S.pneumoniae).Acute mastoiditis is a complication of acute otitis media and can involve not only the mucoperiosteum of the middle ear but can also spread to the periosteum by destroying the mastoid bone (acute coalescent mastoiditis).In addition,the infection can extend through the surrounding bones or the emissary veins beyond the mastoid’s air cells,leading to subperiosteal abscesses.Patient’s Concern:A 16-month-old female patient was hospitalized due to the purulent discharge of the left ear and the symptoms of right mastoiditis (swelling and redness of the skin).Diagnosis:Bilateral acute coalescent mastoiditis caused by S.pneumoniae infection.The computer tomography revealed bilateral bone destruction of the mastoid and abscesses found behind the auricle on both sides.Interventions:The patient underwent intravenous antibiotic therapy and surgical treatment.Outcomes:The patient was discharged 14 days after hospitalization with an improved condition.Lessons:Improperly treated acute coalescent mastoiditis can lead to extracranial and intracranial complications,sometimes serious and even life-threatening.Complications are prevalent in children under 2 years,in whom the disease progresses more rapidly and severely.The vaccination with a 13-valent vaccine may not result in sufficient immunity against S.pneumoniae,a predominant pathogen in children affected by acute coalescent mastoiditis.
KEYWORDS: Acute otitis media;Acute coalescent mastoiditis;Streptococcus pneumoniae;Children;Case report
1.Introduction
Acute coalescent mastoiditis (ACM) is a rare complication of acute otitis media (AOM).ACM is typically preceded by AOM,nearly all patients suffer from one or more otologic problems[1].It may affect various age groups.In the current opinion,Streptococcus pneumoniae (S.pneumoniae) is considered to be the predominant pathogen in children affected by ACM.It is the most common and the most likely cause of the most acute forms of the disease and complications[1].Another frequent pathogen is Streptococcus pyogenes[2].This case report aims to discuss the management of acute,bilateral coalescence mastoiditis in a young patient with AOM.
2.Case report
Ethical approval was gained from the local ethical committee and written informed consents were obtained from the parents of the patient for participation and publication of this case report as well as accompanying images.
A 16-month-old female who attends the nursery with no relevant disease or family history was admitted to the otolaryngology department due to the purulent discharge of the left ear and the symptoms of right mastoiditis (swelling and redness of the skin).The medical history indicated a previous hospitalization due to an upper respiratory tract infection and the patient was treated with antibiotics (cefadroxil p.o.,later modified to cefuroxime p.o.for a month).She was fully vaccinated according to the local vaccination recommendations.
On admission,the patient’s body temperature was 38.7 °C.The otoscopic examination showed that the right tympanic membrane was perforated and the left one inflamed.The computer tomography revealed bilateral bone destruction of the mastoid.Bilateral tympanic cavities were filled with inflamed granulation tissue.Ossicles were not intact on both sides.Moreover,there were intensifying organized abscesses found behind the auricle on both sides:the right one was 21 mm × 46 mm in the axial plane,and the left one was 20 mm × 39 mm (Figure 1A-1C).
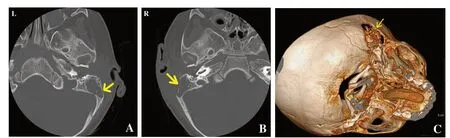
Figure 1.(A,B) Preoperative CT scans of a 16-month-old female patient showing extensive inflammatory changes in the ears and the pyramids of temporal bones (arrows).The changes are more exacerbated on the right side.(C) Preoperative CT-scan (3D image) showing loss of temporal bone (arrow).
The bacterial culture from the ear revealed the presence of S.pneumoniae (cefotaxime and vancomycin susceptible).Intravenous antibiotic therapy with cefuroxime was administered.The patient then underwent the surgical treatment of right-sided antromastoidectomy with abscess drainage,and the same procedure was performed consecutively a few days later on the left side.At surgery,on both sides,a subperiosteal abscess and a significant loss of the bone mastoid process were found.Antibiotic therapy was modified based on the results of the microbiological examination.The patient was treated with intravenous vancomycin (up to 14 days),ceftriaxone,and locally on filters with ciprofloxacin.
After the treatment,the bacterial culture was sterile,and on the following days,there were Enterococcus faecalis (ampicillin,linezolid,and vancomycin susceptible) and Pseudomonas aeruginosa (amikacin,cefotaxime,and vancomycin sensitive) present.
Because of the abnormal morphology and blood test results,the child was consulted twice by a pediatrician and a hematologist.The laboratory tests results showed absolute lymphocytosis up to 80% (normal range:20%-40%),the granulocytic system 8% (normal range:0%-0.05%),the number of neutrophils 1 300/mm3(normal range:1 500-8 000/mm3),band and eosinophilic neutrophils 1% (normal range:1%-5%),monocytes 10%-30% (normal range:4%-8%),platelet count above 400 000 μL (normal range:140 000-440 000 μL),and normocytic anemia.Due to the low levels of hemoglobin (8.1 g/dL) (normal range:11.5-15.5 g/dL) and albumin (2.6 g/dL) (normal range:4.6-7.4 g/dL),a one-time blood transfusion was administered to the patient without complications.In addition,normalization of acute-phase proteins was observed.
The patient was discharged 14 days after hospitalization.On the last examination,there was no discharge from the external ear canals.The otoscopic examination revealed intact tympanic membranes in both ears with a healed incision line in the retroauricular region.Otolaryngology care was continued in the patient’s local town.However,she was admitted to the otolaryngological department two years later due to a recurrence of acute purulent otitis with the discharge of the right ear in order to undergo intravenous antibiotic therapy (cefuroxime).The result of blood tests showed no abnormalities.However,microbiological culture from the ear revealed again the presence of S.pneumoniae (amoxicillin,clindamycin,erythromycin,levofloxacin,and trimethoprim/sulfamethoxazole susceptible).The local and general conditions of the patient were improved after the treatment.
3.Discussion
ACM is a rare complication of AOM,affecting less than 0.01% of patients with AOM[3].However,the risk of death in intracranial otogenic impediments is estimated at 10%[3].The occurrence of subperiosteal abscess is estimated at 50% diagnosed with ACM[3].During inflammation,hyperplastic mucosa in the epitympanum occludes the aditus ad antrum,entrapping purulent material within the mastoid air cells.The pressure exerted by the purulent content crushes the bony septation of mastoid air cells and causes necrosis.The diagnosis of ACM is made based on clinical and radiological presentation[3].
Imaging tests are very helpful in the diagnosis of ACM.Magnetic resonance imaging,however,in this disease entity,is not as accurate as computer tomography due to inferior estimation of bone destruction[4].
ACM should be distinguished from perichondritis of the auricle as well as benign and malignant tumors of the mastoid bone.Acute mastoiditis may be sometimes mistakenly diagnosed as ACM[3].Severe complications of ACM may be distinguished as extracranial and intracranial.The first kind includes subperiosteal abscess,facial nerve palsy,labyrinthitis,and Bezold abscess.A subperiosteal abscess is recognized in about half of the patients with ACM.Among the intracranial complications,meningitis,intracranial abscess,and venous sinus thrombosis can be found[3].
The human nasopharynx is the main reservoir for S.pneumoniae,which usually leads to asymptomatic colonization.Carriage rates of S.pneumoniae are the highest among young children (37%) and may rise to up to 58% in crowded environments such as daycare centers[5].The main risk factors of ACM are recurrent AOM,age below 24 months,impaired immune system,incorrectly pneumatized mastoid process (due to the narrow aditus and antrum which are an obstacle to evacuation of inflammatory tympanic mucosa),and lack of vaccination or inadequate treatment of AOM[3].As a result of inflammation caused by S.pneumoniae,the temporal bone may be damaged due to bone resorption.The resultant influx of inflammatory cells produces a host of cytokines such as PGE2,IL-1,and RANK-L,which promote resorption through osteoclasts,the primary bone resorbing cell.In ACM,stimulatory inflammatory cell products initiate osteoclast activity and disturb the balance between protective and destructive processes[5].Also,bone marrow macrophages and osteal macrophages participate in the destruction of bones.After inflammasome activation,they promote bone destruction by producing IL-1β or IL-18,which causes activation of more macrophages.It leads to a higher rate of phagocytose,which increases the level of immunological response and bone resorption[6].Inflammasome activation is observed in monocytes and neutrophils,which increases antimicrobial and pro-inflammatory abilities and promotes bone destruction.It was also proven that the destruction of the bone is not only caused by the response of the host’s immune system but also by the pathogen’s biofilm[7].
In the presented case,massive destruction induced by S.pneumoniae disturbed both mastoid processes.This raised suspicion of the child having immunity disorders,however,diagnostics performed after the otolaryngology treatment did not reveal any abnormality.Antibiotics seem to reduce pain at two to seven days compared with placebo.However,antibiotics generally have poor bone penetration and pharmacokinetic bioavailability in bone,which creates additional therapeutic challenges.A combination of three altered the penicillinbinding proteins (PBPs):PBP1a,-2b,and/or -2x,which protects S.pneumoniae against beta-lactams or the presence of ermB gene encoding for a methylase responsible for the dimethylation of a specific adenine in 23S rRNA,A2058 in domain V,leading to a decreased affinity to macrolides,may cause growing resistance to antibiotics among these pathogens[4].In cases of uncomplicated ACM,intravenous antibiotic therapy and surgical treatment of ACM is efficient.The drug selection should be made based on whether a patient has a previous history of AOM.Mastoidectomy allows for cleaning of the infected area and prevents recurrence[8].It should be performed if there is no clinical improvement after 48 hours of intravenous antibiotic therapy.Early drainage prevents further complications[3].Surgical treatment and correct antibiotic therapy were successfully administered in our case.
Considering the topic of S.pneumoniae infection,the preventive role of vaccination should be mentioned.The goal of pneumococcal vaccination is to stimulate effective anti-pneumococcal antibodies,mucosal immunity response,and immunological memory.Immunization of infants and young children with the pneumococcal conjugate vaccine has significantly decreased nasal carriage rates and pneumococcal disease in all age groups[8].Currently,two pneumococcal vaccines are available:the 23-valent pneumococcal polysaccharide vaccine and the 13-valent pneumococcal proteinconjugate vaccine (PCV13).Beginning in 2010,immunization of children with the PCV13 was recommended.In the present case,the child was vaccinated with the PCV13,however,the vaccine did not effectively protect against the infection.This may be explained by Vaughn,who found that anti-pneumococcal IgG protection is poor in PCV13-immunized children with recurrent AOM.The near absence of immunity to common non-PCV13 pneumococcal serotype is explained by the author as the result of a lack of natural bacterial exposition,or a relative state of immunodeficiency,in which natural exposures to pneumococci fail to stimulate protective immunity[7].
The presented case is unique because of the single-time presence of abscesses in both ears and massive bilateral destruction of bones.Despite antibiotic treatment,bilateral acute otitis causes massive bone destruction.The vaccination with a 13-valent vaccine may not result in sufficient immunity against S.pneumoniae.Evaluation of anti-pneumococcal immunity should be considered if the severe presentation of AOM appears after PCV13 vaccination.
Conflict of interest statement
The authors report no conflict of interest.
Funding
This study received no extramural funding.
Data availability statement
The data supporting the findings of this study are available from the corresponding authors upon request.
Authors’ contributions
MMK and KR:conception,design of the work,data collection,review and editing of the manuscript.MP:data collection,interpretation of data,original draft preparation and writing.KP:data collection.TZ substantively revised manuscript and supervision.
杂志排行
Journal of Acute Disease的其它文章
- Cardiovascular risk factors affecting COVID-19 outcomes at a tertiary referral hospital in northwest Iran:A prospective cohort study
- Correlation of neutrophil to lymphocyte ratio to severity of coronary artery disease and in-hospital clinical outcomes in patients with acute coronary syndrome:A prospective observational study
- A 10-year review and epidemiology of animal bite cases in Gerash city,south of Iran:A retrospective cross-sectional study
- Relationship between nutritional therapy and beneficial bacteria ratio in severe disease
- Clinical profile and risk factors of symptomatic and asymptomatic hypoglycemia in neonates admitted to NICU in a tertiary care center:A cross-sectional study
- Paradoxical systemic toxicity by inhaled paraquat poisoning:A case report
