Associations of daily sedentary behavior,physical activity,and sleep with irritable bowel syndrome:A prospective analysis of 362,193 participants
2024-01-25XuGoSifnTinNinghoHungGngSunToHung
Xu Go,Sifn Tin,Ningho Hung,Gng Sun,To Hung
a Department of Occupational and Environmental Health Sciences,School of Public Health,Peking University,Beijing 100191,China
b Department of Epidemiology and Biostatistics,School of Public Health,Peking University,Beijing 100191,China
c Department of Gastroenterology and Hepatology,First Medical Center of People’s Liberation Army General Hospital,Beijing 100853,China
Abstract Background:Irritable bowel syndrome(IBS)substantially affects quality of life and requires early prevention.This study aimed to elucidate the relationships between IBS and daily behaviors,including sedentary behavior (SB),physical activity (PA),and sleep.In particular,it seeks to identify healthy behaviors to reduce IBS risk,which previous studies have rarely addressed.Methods:Daily behaviors were retrieved from self-reported data of 362,193 eligible UK Biobank participants.Incident cases were determined by self-report or health care data according to Rome IV criteria.Results: A total of 345,388 participants were IBS-free at baseline,during a median follow-up of 8.45 years,19,885 incident IBS cases were recorded.When examined individually,SB and shorter (7 h/day) or longer (>7 h/day) sleep duration were each positively associated with increased IBS risk,and PA was associated with lower IBS risk.The isotemporal substitution model suggested that replacing SB with other activities could provide further protective effects against IBS risk.Among people sleeping 7 h/day,replacing 1 h of SB with equivalent light PA,vigorous PA,or sleep was associated with 8.1% (95% confidence interval(95%CI):0.901-0.937),5.8% (95%CI:0.896-0.991),and 9.2% (95%CI:0.885-0.932) reduced IBS risk,respectively.For people sleeping >7 h/day,light and vigorous PA were associated with a 4.8% (95%CI:0.926-0.978)and a 12.0%(95%CI:0.815-0.949)lower IBS risk,respectively.These benefits were mostly independent of genetic risk for IBS.Conclusion:SB and unhealthy sleep duration are risk factors for IBS.A promising way to mitigate IBS risk for individuals sleeping 7 h/day and for those sleeping>7 h/day appears to be by replacing SB with adequate sleep or vigorous PA,respectively,regardless of the genetic predisposition of IBS.
Keywords: Irritable bowel syndrome;Isotemporal substitution model;Physical activity;Sedentary behavior;Sleep
1.Introduction
Irritable bowel syndrome (IBS) is a functional bowel disorder without obvious organic abnormalities,characterized by recurrent abdominal pain or discomfort,altered bowel habits,stool irregularities,and bloating.1,2While generally not causing lethal consequences,IBS can greatly disrupt the daily life and work habits of affected individuals and substantially affect quality of life.Recent evidence suggests that IBS is not solely prevalent in young adults;rather,the disease burden is quite high for middle-aged and older adults as well,3,4which adds another layer of threat to the quality of life and health in an aging population.In terms of economic burden,IBS accounted for approximately half of the referrals to gastroenterology clinics;it yielded greater than Euro8 billion in annual healthcare and indirect costs in Europe and USD10 billion in the US.5However,due to the heterogeneity of the disease and the multiplicity of putative pathophysiological mechanisms of IBS,2,6targeted risk screening and prevention of IBS are currently not applicable.
To date,there is a dearth of studies exploring nonpharmaceutical approaches to lower IBS risk due to the lack of biomarkers and treatments to cure this multifactorial health disorder.6Physical activity(PA),defined as any bodily movements produced by skeletal muscles that result in energy expenditure,has been associated with improvement in gas transit and abdominal distension,symptoms that are frequently observed in IBS patients.6,7However,the most recent Cochrane review suggests that the evidence of PA delaying IBS symptom deterioration as observed in clinical trials might have low certainty because of the limited sample size.8Large cohort studies are required to provide timely evidence on the association between PA and IBS risk.Sedentary behavior(SB)—which refers to any waking activity done while sitting,reclining,or lying with low energy expenditure (1.5 metabolic equivalents,METs),including sitting while watching television or using a computer—is gaining recognition as a risk factor for several long-term conditions independent of PA.9-11Nevertheless,the associations of PA and SB with IBS have only been observed in cross-sectional studies without further considering the fact that the length of a day is fixed and so potential risk reductions associated with bringing sedentary duration down depend on the activity that displaces SB,such as certain types of PA or sleep.Given sleep quality is also closely related to IBS,12another scientific question arises around whether healthy sleep would be an ideal alternative to SB for reducing the risk of IBS.An isotemporal substitution paradigm would directly address such questions by theoretically replacing a certain amount of SB time with an equal amount of time spent on different levels of PA or sleep.13Additionally,IBS has been shown to be associated with genetic background,14but no studies have investigated whether the genetic susceptibility of IBS could interact with the associations between durations of daily behaviors and incident IBS.
Therefore,we explored the prospective associations of the duration of SB,PA,and sleep with the risk of IBS among middle-aged and older participants from the UK Biobank to understand whether the IBS risk during later life could be influenced by SB,PA,and sleep.In particular,we evaluated the potential benefit of replacing SB with light PA (LPA),moderate PA(MPA),vigorous PA(VPA),and sleep using the isotemporal substitution model.Leveraging in-depth genetic information,we further examined whether the genetic predisposition to IBS could modify the relationships between different activities and the incidence of IBS.
2.Methods
2.1.Study design and population
Study design and methods of the UK Biobank have been reported in detail previously.15In brief,UK Biobank is a large-scale prospective study with 502,528 participants aged 37-73 years recruited in 2006-2010 at baseline with multiple ongoing follow-ups.During the initial visit,participants provided information on lifestyle and health data,physical measurements,and their biological samples were collected.This study included 362,193 participants with available information on daily behaviors,potential covariates,and IBS prevalence and incidence over a median follow-up of 8.45 years through December 31,2018 (Supplementary Fig.1).UK Biobank has approval from the North West Multicenter Research Ethical Committee,and all participants provided written informed consent.This study has been conducted using the UK Biobank Resource under application number 44430.

Fig.1.Graphs of the best-fitting models for independent relationships of physical activity,sleep duration,and sedentary time with incident irritable bowel syndrome.TagedEnd
2.2.Definition of IBS
IBS assessment was conducted using the linked hospital admission records (UK Biobank Data-Fields: 41202 and 41204)primarily as well as an ancillary online gastrointestinal health self-assessment questionnaire issued in 2017,which included 169,635 participants.For the hospital records,participants were classified as cases if they had anInternational Classification of Diseases,9th and 10th editions (ICD-9/10) code of primary or secondary diagnosis for IBS (ICD-9: 564.1;ICD-10: K58).For the ancillary questionnaire,participants whose symptoms fulfilled the Rome IV criteria for IBS based on questionnaire data at the time of reporting (UK Biobank Data-Fields: 21025,21026,21027,21028,21031,21032,and 21033)were defined as IBS cases.16If participants gave a positive answer to the question “Have you ever been diagnosed with IBS?” in the ancillary questionnaire (UK Biobank Data-Fields: 21024) but were free of IBS at baseline according to hospital records,he/she would be further considered as an incident IBS case,with the incident date as the median date between the date of taking the questionnaire and the baseline date of visiting the examination center.
2.3.Assessments of SB,PA,and sleep
SB in leisure time was self-reported and collected using questionnaires at baseline.Participants were asked how many hours in a typical day they spent watching television,using a computer,and driving (UK Biobank Data-Fields: 1070,1080,and 1090),which are 3 of the most widespread leisure-time SBs in adults.The length of SB was defined as the sum of time spent doing the 3 activities.PA was quantified using the modified short-form International Physical Activity Questionnaire,which assessed the duration and frequency of PA in leisure time.Weekly PA was summarized using the weekly total MET,calculated by multiplying the MET value of activity by the number of PA hours per week.Based on the guideline of the World Health Organization,PA was categorized as LPA(<3 MET),MPA (3-6 MET).17The mean hours for each PA category per day were calculated using the total number of minutes spent per week divided by 7 days.Sleep duration in a day was the average duration over the last 4 weeks collected by self-report (UK Biobank Data-Fields: 1060) and expressed as integer values.We treated sleep duration as a piecewise variable with a breakpoint at 7 h,which is considered the threshold of healthy sleep duration;each of the 2 sleeping variables had an approximately linear association with mortality,as previously reported.18,19
2.4.Data collection and covariates
Information on socio-demographic characteristics,lifestyle factors,and health status at baseline was obtained by standardized questionnaires.We included age,sex,body mass index(BMI),healthy alcohol intake status,years of education (<10 and10 years),the regular use of pain-relief medications(i.e.,aspirin,ibuprofen,and paracetamol) and/or gastrointestinal agents (i.e.,ranitidine,omeprazole,and laxatives),hypertension,coronary heart disease (CHD),diabetes,and Townsend deprivation index.Detailed measurements of the covariates were reported in supplement methods.Observations with any missing values were excluded from this study.
2.5.Genetic risk score for IBS
Detailed information about genotyping,data imputation,and quality control in the UK Biobank was briefly described in supplement methods.Based on the availability of imputed single nucleotide polymorphisms(SNPs),we created a genetic risk score (GRS) for IBS using 6 IBS-related SNPs validated in both UK Biobank and 23andMe data and based on the largest and most recent genome-wide association studies(GWASs).14Each SNP was recoded as 0,1,or 2 according to the number of risk alleles,and missing SNP values for individuals were imputed by corresponding mean values.This GRS,based on multiple genes,was calculated and weighted by multiplying the odds ratios (ORs) of each included SNP with the number of risk alleles,summing them,and then dividing by the total effect size.The detailed SNPs were demonstrated in Supplementary Table 1.

Table 1 Baseline characteristics of participants in UK Biobank by sedentary time.a
2.6.Statistical analysis
We first tested the associations of each activity with the prevalence of IBS at baseline using logistic regression models that increasingly adjusted for potential covariates.Model 1 adjusted for age,sex,and ethnicity.Model 2 additionally adjusted for BMI,smoking status,healthy alcohol intake,and years of education.Model 3 additionally adjusted for hypertension,CHD,diabetes,Townsend deprivation index,and taking pain-relief medications and/or gastrointestinal agents.
Subsequently,among baseline IBS-free participants,we evaluated their baseline activity with their incident IBS during follow-up.Three algorithms were implemented to understand the role of SB,PA,and sleep in the development of IBS.First,we tested the independent associations of the durations of SB,LPA,MPA,VPA,and sleep with incident IBS using a Cox regression model for each activity (i.e.,independent model).Then,in case longer SB duration increases IBS risk,we simultaneously adjusted for the durations of LPA,MPA,VPA,and sleep in a single partition model to see if additional changes in the 4 behaviors could mitigate the impact of SB on IBS.The third model was the isotemporal substitution model,which explored the effect of substituting SB with equal time of the different types of PA or sleep.This model is based on the realistic assumption that an increase in one behavior will be accompanied by a decrease of equivalent duration (isotemporal) in another behavior while total time of all behaviors is kept constant.13,20This model could be expressed as a basic proportional hazards model as follows:
where Total time=SB time+total PA time+sleep duration.The b1-4represent the effects of substituting 1 h/day SB with 1 h/day LPA,MPA,VPA,and sleep,respectively.Corresponding doseesponse curves for the relationships between different behaviors and the risk of incident IBS were constructed using restricted cubic spline regression.21
Finally,we investigated whether the associations between these behaviors and IBS risk were modified by genetic predisposition to IBS.An interaction term between each behavior and continuous GRS was then generated and implemented in the isotemporal substitution model.A binary GRS constructed by median was further used to categorize the IBS risk.
Four sensitivity analyses were conducted to evaluate the robustness of primary findings:(a)the isotemporal substitution model additionally adjusting for having a healthy diet and for the stress experience over the last 2 years (stress experience over the last 2 years(yes/no)was coded based on the question“In the last 2 years have you experienced any of the following?” with 6 incidences (Data-field 6145)),(b) the isotemporal substitution model excluding participants who developed IBS within the first 2 years of follow-up to avoid reverse causation,(c) the isotemporal substitution model excluding participants without MVPA at baseline to avoid bias from extreme observations,and (d) the isotemporal substitution model by age group to test the robustness of the model in middle-aged and older individuals separately.
SAS Version 9.4 TS1M7 (SAS Institute,Cary,NC,USA)was used to conduct data cleaning and all analyses.A twosidedp-value of<0.05 was considered statistically significant.
3.Results
3.1.Participants’characteristics
As shown in Table 1,participants were mostly white and aged 56.22-8.11 years(meanD).About 35.1%of participants were former smokers,and 55.1% never smoked.The majority had>10 years of education(69.5%),and half reported a healthy daily intake of alcohol.About 53.1%,5.3%,and 4.7%had hypertension,CHD,or diabetes at baseline,respectively,as diagnosed by doctors according to self-reports and medical records.Participants with excessive sedentary time(>6 h/day)were more likely to be overweight or obese individuals,to be current smokers,and to have hypertension,CHD,and diabetes.Although they reported similar sleep duration to other groups,they had much less PA and were more likely to have no MVPA and to take pain-relief medications regularly.
3.2.Associations of SB,PA,and sleep with prevalent IBS
At baseline,16,805 of the total 362,193 participants had IBS.According to the fully adjusted model,SB and shorter(7 h/day)or longer(>7 h/day)sleep duration were each positively associated with increased IBS risk,and 3 types of PA were associated with lower IBS risk,albeit that for MPA was not statistically significant (Table 2).After controlling for potential covariates,individuals without any MVPA had 12.1%(95%confidence interval(95%CI):1.070-1.174)higher odds of having IBS than those with MVPA;and compared to participants with2 h/day of SB,those with excessive SB time had 18.8%(95%CI:1.118-1.263)higher odds of having IBS.
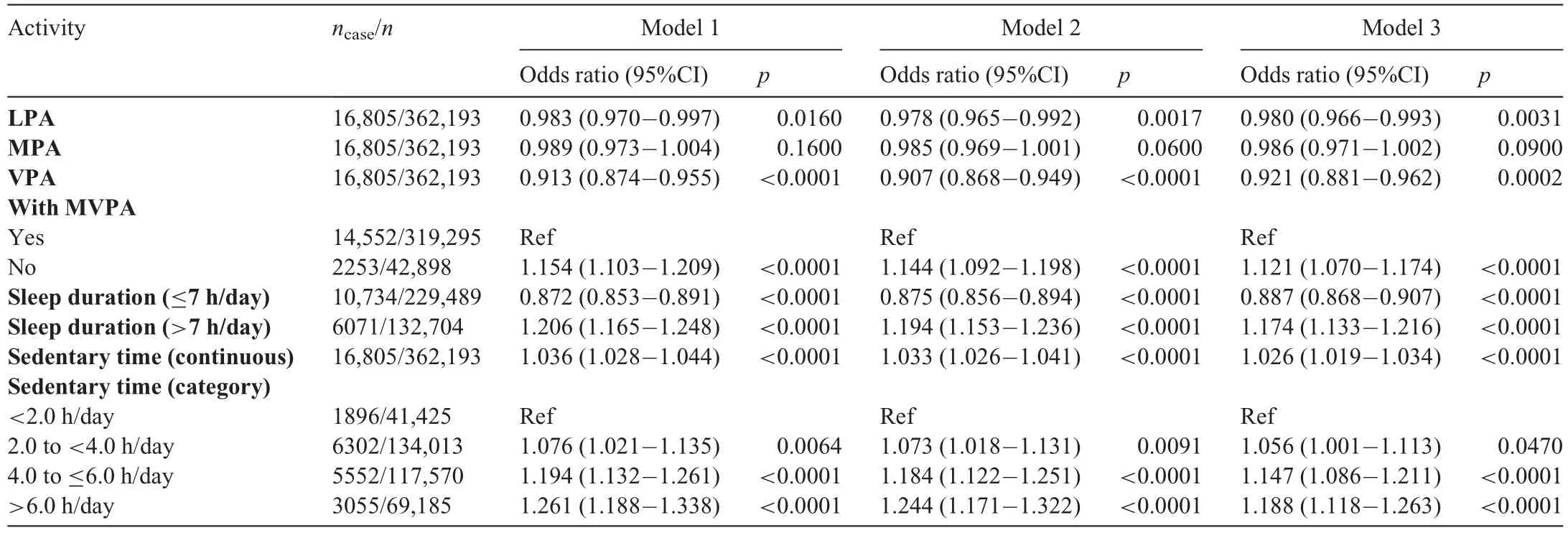
Table 2 Associations of SB,PA,and sleep with the odds of IBS in UK Biobank participants.
3.3.Associations of SB,PA,and sleep with incident IBS
Among the 345,388 participants who were free of IBS at baseline,19,885 of them developed IBS during the follow-up.When examined individually,each activity was significantly associated with IBS risk (Table 3).The fully adjusted model showed that 1 h/day increases in LPA,MPA,and VPA were related to a 6.6% (95%CI: 0.922-0.947),4.7% (95%CI:0.939-0.968),and 11.0% (95%CI: 0.856-0.925) lower risk of IBS,respectively.The same increase in SB was associated with a 1.7%(95%CI:1.010-1.024)higher risk.A 1-h increase in sleep duration showed mixed effects,as seen in U-shaped associations with a 6.2%(95%CI:0.918-0.959)lower risk of IBS for individuals sleeping7 h/day and a 5.5% (95%CI:1.016-1.096) higher risk for individuals sleeping >7 h/day.As shown in Fig.1,sleep duration demonstrated a U-shaped doseesponse relationship with IBS risk,while other activities demonstrated monotonic increasing (SB) and decreasing(PA)trends.
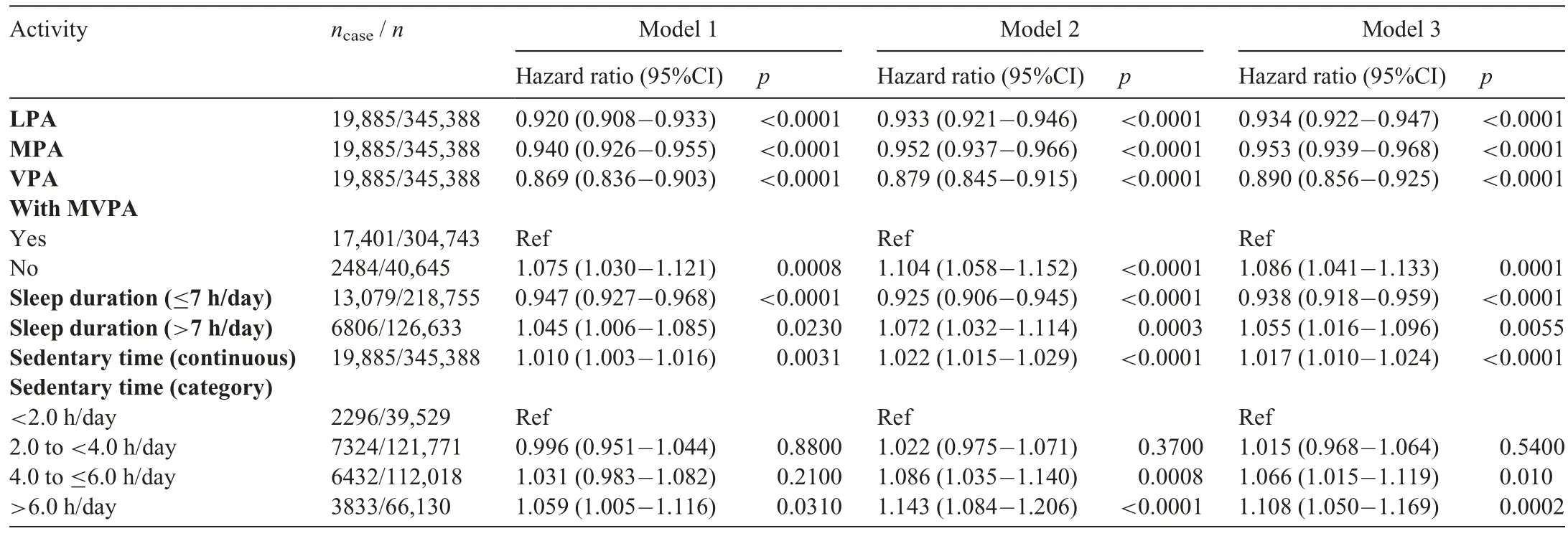
Table 3 Independent associations of SB,PA,and sleep with incident IBS in UK Biobank participants.
Partition models mutually adjusting for SB,PA,and sleep showed that neither increasing PA nor keeping sleep duration at 7 h was able to mitigate the adverse effect of SB on IBS development,with an essentially unchanged increased risk of 1.4%(95%CI:1.007-1.021)(Supplementary Table 2).By the sleep duration category (7 h/day and >7 h/day),effects of SB were only slightly attenuated in individuals with shorter sleep duration (hazard ratio (HR)=1.012,95%CI:1.003-1.020).Estimates of sleep duration were essentially unchanged,but estimates of the various PAs were attenuated to different extents in the partition model by sleep duration.
Subsequently,the isotemporal substitution model was conducted to understand the benefits of replacing SB with PA and healthy sleep.In the whole population (Table 4),replacing 1 h of SB with equivalent LPA was associated with an additional 1.3% reduction in IBS risk (HR=0.929;95%CI:0.914-0.944) compared to increasing LPA by 1 h in the partition model (Supplementary Table 2;HR=0.942;95%CI:0.928-0.956).This reduction was also higher than that yielded from the individual model (Table 3;HR=0.934;95%CI:0.922-0.947).Similar reductions in IBS risk were also observed for MPA,VPA,and sleep.As shown in Table 4,Fig.2,and Supplementary Fig.2,for individuals without adequate sleep,replacing 1 h of SB with equivalent LPA,VPA,and sleep was associated with an 8.1% (95%CI: 0.901-0.937),5.8% (95%CI:0.896-0.991),and 9.2% (95%CI:0.885-0.932)lower IBS risk,respectively.For individuals already sleeping >7 h/day,replacing 1 h of SB with equivalent LPA and VPA were significantly associated with a 4.8% (95%CI: 0.926-0.978) and 12.0% (95%CI: 0.815-0.949) reduction in IBS risk,respectively.Replacement of SB with MPA showed positive but marginal benefit(HR=0.971;95%CI:0.941-1.001).These estimates remained essentially unchanged in the isotemporal substitution model that additionally adjusted for healthy diet and the stress experience over the last 2 years(Supplementary Table 3).
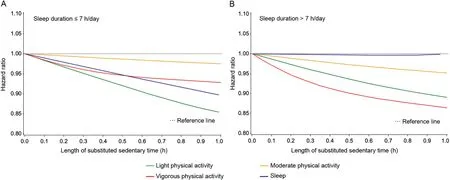
Fig.2.Best-fitting models for the effect of substituting sedentary time for physical activity or sleep in participants by sleep duration category((A)7 h/day and(B)>7 h/day).
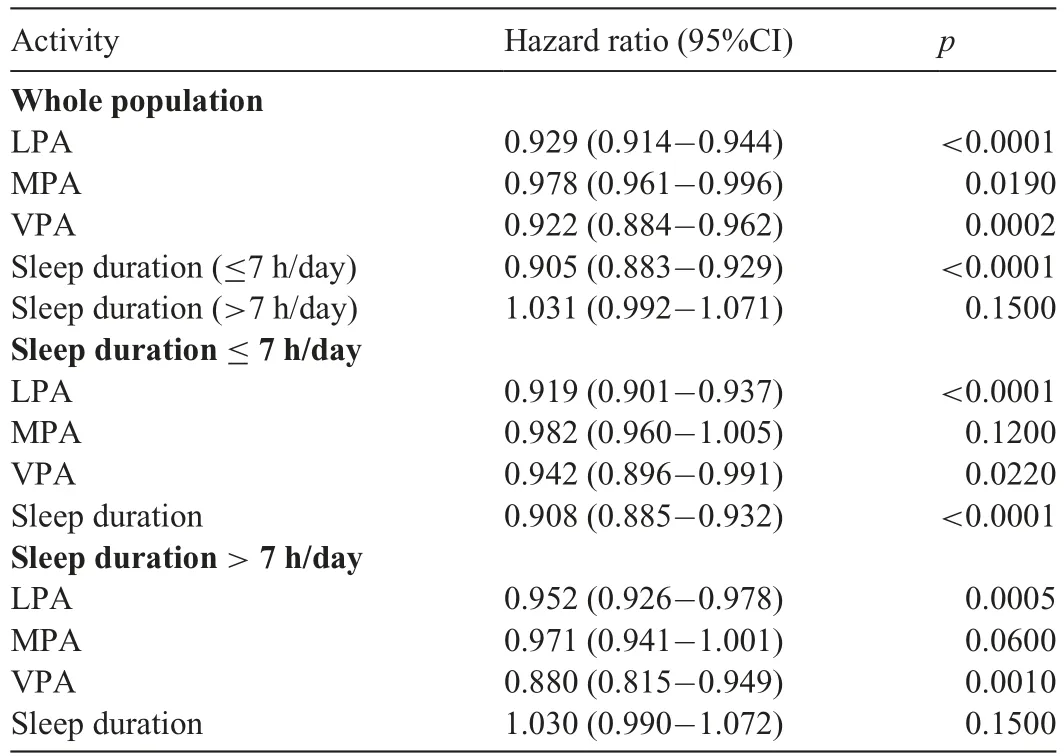
Table 4 Associations of PA and sleep with incident IBS by replacing SB using isotemporal substitution model in the whole population and subpopulations by sleep duration.a
We conducted another 3 sensitivity analyses.When we excluded individuals who had IBS cases occur in the first 2 years of follow-up (Supplementary Table 4),the benefit of replacing SB with equivalent LPA increased slightly,while the benefit of replacing SB with equivalent VPA was reduced.When we excluded those without any MPA or VPA (Supplementary Table 5),the benefits of any PA and healthy sleep were attenuated slightly.For older individuals(60 years),the benefits of healthy sleep duration dropped considerably compared to younger individuals.LPA and VPA showed better risk reduction in older adults sleeping>7 h/day,but the differences were not statistically significant(Supplementary Table 6).

Table 5 Associations of PA and sleep with incident IBS by replacing SB using isotemporal substitution model in subpopulations with high/low genetic risks by sleep duration.a
3.4.Genetic impact on the associations of PA,sleep duration,and sedentary time with incident IBS
Additionally,we tested the interplay between activity and genetic predisposition to IBS by sleep duration in the primary isotemporal substitution model (Table 5).The continuous GRS did not have additional robust impacts on the associations between any activities and IBS risk except for VPA among individuals sleeping >7 h/day (p-interaction=0.019).Replacement of SB with 1 h VPA was associated with a 6.9%lower IBS risk(HR=0.931;95%CI:0.842-1.029)in individuals with high genetic risk,and the IBS risk reduction more than doubled(17.7%lower IBS risk)in those with low genetic risk(HR=0.823;95%CI:0.733-0.924).
4.Discussion
Leveraging a large population-based cohort,our study found that SB was positively associated with higher IBS risk;PA,especially LPA and VPA,could help reduce the risk,and sleeping for a duration of 7 h per day could yield the lowest IBS risk.Although SB and unhealthy sleep duration are risk factors for IBS,replacing SB with LPA or VPA and keeping a healthy sleep duration could mitigate IBS risk regardless of genetic predisposition to IBS.Rather than simply increasing the time of PA or getting adequate sleep,replacing SB with sleep yielded the biggest reduction in IBS risk for people sleeping7 h/day,but VPA could be the best option to reduce IBS risk for people sleeping>7 h/day.
To the best of our knowledge,this is the first study addressing the prospective associations of SB,PA,and sleep duration with IBS in a large population.The cross-sectional association between SB and IBS was reported by Vasquez-Rios et al.9in 2019,who suggested a sedentary lifestyle may be an independent risk factor for IBS in 346 medical students.A possible mechanism is the incapacity of the human body to manage the attenuation of the effect of gravitational force that aids descending colon motility.Furthermore,SB could lead to and enhance chronic partial obstruction,potentially causing IBS.22Their evidence,like ours,highlights the possibility that PA could mitigate IBS risk.Several randomized controlled trials and a qualitative study seeking physical treatment regimens for IBS patients have been conducted over the past decade.7,8,23,24The most recent review of 11 randomized controlled trials with data from 622 participants yielded that PA may improve symptoms but not quality of life or abdominal pain in people diagnosed with IBS.8Unfortunately,since the included findings had relatively low certainty,using PA as part of IBS symptom management warrants further evidence.Unlike the moderate improvement associated with PA in IBS patients,our study observed robust reductions in IBS risk when SB is replaced with LPA and VPA.It could be the case that PA helps prevent IBS,but more solid clues from randomized controlled trials or other experimental studies are needed to validate this finding.
Sleep duration of 7-8 h per day is reported to be an essential element of a healthy lifestyle,potentially reducing the mortality risks of all-cause,cardiovascular diseases,and cancer,as well as the risks of major chronic diseases.19,25In agreement with a previous review,12we found that abnormal sleep duration was associated with IBS at baseline.Many studies have shown the adverse effects of poor sleep in IBS patients,with exacerbated IBS symptoms after experiencing poor sleep.5,12Our study further highlighted that in IBS-free individuals,maintaining a healthy sleep pattern could lower the future risk of IBS,which moreover indicates the bidirectional relationship between sleep and IBS.Sleep quality is also related to mood disorders,including depression and anxiety,26both of which are much more frequent in IBS patients.5This has been underlined by the dysfunction within the bidirectional gutrain axis,which is thought to play a key role in the genesis and maintenance of symptoms in IBS.27In line with this,our GRS was constructed based on 6 SNPs sharing genetic pathways with mood and anxiety disorders.14However,this genetic background only moderately modified the association between VPA and IBS risk for participants sleeping>7 h/day.This could be plausible due to the moderate IBS genome-wide SNP heritability,14which may infer that neuronal pathways play a limited role in the progression of IBS,while behavioral factors are potentially at work via other underlying biological pathways.
Sleep and PA are not independent activities but may interact with each other.Although debate exists,studies have found that sleep duration and PA are bidirectionally linked with limited effects.28,29Many PA-related studies combine MPA and VPA into MVPA when elucidating the health benefits of PA.In our study,VPA outperformed MPA in terms of IBS risk reduction,especially in individuals with adequate sleep.This may be partially explained by the findings of a previous systematic review,28which showed that VPA was associated with better sleep quality in older adults;our sensitivity analysis by age group confirmed this as well.The benefit of replacing SB with VPA may be boosted further by adequate sleep duration.Altogether,evidence implies that further studies are needed to explore detailed exercise suggestions according to age group.
This study has several strengths,including the large sample size,detailed records of intestinal system status and daily behaviors,and phenotype data available on a wide range of potential covariates and genetic variants allowing for the evaluation of gene and environment interaction.Several limitations should be noted as well when interpreting the results.First,as a volunteer cohort,participants in the UK Biobank do not represent the UK population—they tend to be healthier and wealthier.30,31Such individuals may have lower IBS risk and be relatively in better health overall.Second,our IBS identification was according to the ICD-10 codes,which shifted from Rome III to Rome IV during the follow-up.Furthermore,our ancillary online questionnaires were only conducted for~1/3 of the participants.These inconsistencies could lead to misclassification of incident IBS cases and,therefore,to the underestimation of IBS risk in our cohort.Misclassification could distort our findings towards null;our effect-size estimates are therefore conservative.Third,we could not further examine the associations of the activities with different IBS subtypes because of the unavailability of data.Future longterm studies are needed to elucidate whether replacing SB with PA or healthy sleep duration is applicable for reducing the risks of different IBS subtypes.Also,the activity measurement of the UK Biobank did not include other domains like occupation,transportation,and household,and the durations and frequencies were based on self-reported questionnaires.Self-report bias and missing information may compromise the statistical power of the model to detect the differences in IBS risk.For sleep duration,we used the 4-week averaged daily sleep duration to minimize variation,but since people could have various sleep durations over their lifetime and we did not have the data on sleep quality (including but not restricted to sleep latency and sleep efficiency,which could not be yielded from self-reported questionnaires),our sleep duration results ought to be interpreted with caution.Additionally,although we controlled for several factors that could confound our findings,including diet,alcohol,and stress,other risk factors,such as adverse childhood experiences and experience of natural diseases,domestic violence,and bullying were not considered due to lack of data availability.Finally,our participants mostly did not have excessive PA like athletes do.Excessive PA might compromise individuals’ health status by inducing psycho-physical stress and affecting the balance of intestinal microbiota,which may interfere with the stability of the intestinal system and thereby promote IBS development.32
5.Conclusion
Our study investigated the relationships of SB,PA,and sleep with IBS risk in ~0.36 million people,making it one of the largest cohort studies on the subject.Replacing SB with PA and healthy sleep duration could robustly attenuate IBS risk regardless of genetic background.Still,the underlying pathogenesis of IBS is complex,and biological molecular pathophysiology is far from understood.That,along with the paucity of biomarkers and treatments to cure this multifactorial health disorder,warrant future investigations employing larger cohorts and precision measures of activities with wearable monitors or accelerometers to feature the full landscape of the role of healthy behaviors,including regular exercise and highquality sleep,in IBS prevention.
Acknowledgments
Data from the UK Biobank are available in a public,open access repository.The UK Biobank data are available on application to the UK Biobank (www.ukbiobank.ac.uk/).Dr.Xu Gao was supported by grants from China CDC Key Laboratory of Environment and Population Health (2022-CKL-03) and Peking University (BMU2021YJ044).Dr.Gang Sun was supported by the General Program of National Natural Science Foundation of China(32170898).We thank Dr.Chen Chen for the language assistance and the preparation of video slides.
Authors’contributions
XG conceptualized the study,conducted the data cleaning,analyses,and drafted,and reviewed the manuscript;ST coordinated the data collection,and reviewed and revised the manuscript;NH estimated the genetic risk score;GS critically reviewed and revised the manuscript;TH coordinated and supervised the data collection,and reviewed and revised the manuscript.All authors have read and approved the final version of the manucript,and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Supplementary materials
Supplementary materials associated with this article can be found in the online version at doi:10.1016/j.jshs.2023.02.002.
杂志排行
Journal of Sport and Health Science的其它文章
- 2024 Adult Compendium of Physical Activities:A third update of the energy costs of human activities
- Older Adult Compendium of Physical Activities:Energy costs of human activities in adults aged 60 and older
- 2024 Wheelchair Compendium of Physical Activities:An update of activity codes and energy expenditure values
- Alexa,let’s train now!—A systematic review and classification approach to digital and home-based physical training interventions aiming to support healthy cognitive aging
- The influence of resistance exercise training prescription variables on skeletal muscle mass,strength,and physical function in healthy adults:An umbrella review
- A systematic scoping review of study methodology for randomized controlled trials investigating probiotics in athletic and physically active populations
