Contemporary outcomes of patients undergoing robotic-assisted radical cystectomy:A comparative analysis between intracorporeal ileal conduit and neobladder urinary diversions
2024-01-11JordnRichShivrmCumrsmyDnielRntiEtienneLvlleeKyrollisAttllJohnSfkinosNikhilWingnkrPeterWiklundRezMehrzin
Jordn M.Rich , Shivrm Cumrsmy , Dniel Rnti ,Etienne Lvllee , Kyrollis Attll , John P.Sfkinos ,Nikhil Wingnkr , Peter N.Wiklund ,b, Rez Mehrzin ,*
a Department of Urology, Icahn School of Medicine at Mount Sinai, New York, NY, USA
b Department of Urology, Karolinska University Hospital, Solna, Sweden
KEYWORDS
Abstract Objective: We aimed to compare perioperative and oncologic outcomes for patients undergoing robotic-assisted radical cystectomy (RARC)with intracorporeal ileal conduit(IC) and neobladder (NB) urinary diversion.Methods: Patients undergoing RARC with intracorporeal urinary diversion between January 2017 and January 2022 at the Icahn School of Medicine at Mount Sinai,New York,NY,USA were indexed.Baseline demographics, clinical characteristics, perioperative, and oncologic outcomes were analyzed.Survival was estimated with Kaplan-Meier plots.Results: Of 261 patients(206[78.9%]male),190(72.8%)received IC while 71(27.2%)received NB diversion.Median age was greater in the IC group (71 [interquartile range, IQR 65-78]years vs.64 [IQR 59-67] years, p<0.001) and BMI was 26.6 (IQR 23.2-30.4) kg/m2.IC group was more likely to have prior abdominal or pelvic radiation (15.8% vs.2.8%, p=0.014).American Association of Anesthesiologists scores were comparable between groups.The IC group had a higher proportion of patients with pathological tumor stage 2 (pT2) tumors (34[17.9%] vs.10 [14.1%], p=0.008) and pathological node stages pN2-N3 (28 [14.7%] vs.3[4.2%], p<0.001).The IC group had less median operative time (272 [IQR 246-306] min vs.341 [IQR 303-378] min, p<0.001) and estimated blood loss (250 [150-500] mL vs.325 [200-575] mL, p=0.002).Thirty- and 90-day complication rates were 44.4% and 50.2%,respectively, and comparable between groups.Clavien-Dindo grades 3-5 complications occurred in 27 (10.3%) and 34 (13.0%) patients within 30 and 90 days, respectively, with comparable rates between groups.Median follow-up was 324(IQR 167-552)days,and comparable between groups.Kaplan-Meier estimate for overall survival at 24 months was 89% for the IC cohort and 93% for the NB cohort (hazard ratio 1.23, 95% confidence interval 1.05-2.42,p=0.02).Kaplan-Meier estimate for recurrence-free survival at 24 months was 74% for IC and 87% for NB (hazard ratio 1.81, 95% confidence interval 0.82-4.04, p=0.10).Conclusion: Patients undergoing intracorporeal IC urinary diversion had higher postoperative cancer stage, increased nodal involvement, similar complications outcomes, decreased overall survival, and similar recurrence-free survival compared to patients undergoing RARC with intracorporeal NB urinary diversion.
1.Introduction
Bladder cancer is the 5th most common malignancy in adults in the United States, with more than 80 000 cases diagnosed per year[1].Radical cystectomy(RC)via an open(ORC)or robotic-assisted(RARC)approach remains the gold standard treatment for muscle invasive bladder cancer and high-risk non-muscle invasive bladder cancer [2-4].In recent years, multiple randomized control trials have shown benefits of RARC compared to ORC in terms of reducing perioperative morbidity, transfusion rate, and complications,which in turn has led to increased uptake of this technique [5-8].Despite the advantages, widespread adoption has not been achieved, likely owing to the technical challenge of the procedure.Furthermore, due to the difficulty of reconstructive phase robotically,many perform diversions extracorporeally which can mitigate some of the benefits of the robotic approach [9].
Complication rates after RC are high, primarily due to the bowel manipulation and urinary diversion(UD)[10].UD is usually classified as continent or incontinent.The most common type of incontinent UD is an ileal conduit (IC),where urine is diverted from the ureters through the ileum to a stoma at the abdominal wall [11].Alternatively, the most common continent UD is the orthotopic neobladder(NB),where a continent reservoir is created out of a portion of the intestine, allowing the patient to void through the native urethra [12,13].IC is utilized more often since NB is a technically challenging procedure performed almost exclusively at high-volume academic centers [14].
Some studies have found that patients with a NB more often preserve body image due to avoidance of an external appliance as well as maintaining control of continence,though overall quality of life studies have been inconclusive[15-21].Appropriate patient selection is vital for NB, as it is contraindicated in patients in whom the urethra is nonfunctional or involved with tumor [12].Additionally,due to the reconstructive nature of the procedure, NB requires active upkeep of the reservoir and proper healing,so patients must be carefully selected based on age and comorbidities to ensure its success [15].NB also possesses more contraindications than IC, including short life expectancy, severe inflammatory bowel disease, and significant liver or kidney dysfunction, all of which contribute to an overall healthier patient population[15,22].However,most patients undergoing RC, including elderly, are still candidates for NB.
Overall, few large comparative studies with short- to medium-term outcomes exist for RARC with totally intracorporeal UD(ICUD).In this study,we aimed to characterize contemporary outcomes for a large cohort of patients who underwent RARC with ICUD, specifically comparing perioperative,complications,and oncologic outcomes for patients undergoing RARC with intracorporeal IC and NB.
2.Patients and methods
2.1.Study population
Using a prospectively maintained Icahn School of Medicine at Mount Sinai Institutional Review Board (#10-1180)approved institutional database of all patients who underwent RC, we retrospectively reviewed the charts of all patients undergoing RARC who had UD between January 2017 and January 2022.All procedures were performed by three surgeons(Wiklund PN,Sfakianos JP,and Mehrazin R).All surgeons in this study are urologic oncologists with a high volume of robotic experience.They all have performed more than 500 RARC with UD and have passed their learning curve for this procedure.Patients who had extracorporeal diversion, cutaneous urostomy, or those procedures performed in an emergency setting were excluded.UD were performed as previously described [23].Ureteral stents for IC and ileal NB were removed on postoperative day (POD)10 and Foley catheter for ileal NB on POD 21, unless it was clinically indicated to leave in place for longer.As part of our enhanced recovery after surgery protocols, we utilized a non-opioid protocol for all patients as previously described [24].Additionally, we used early dietary initiation and ambulation on POD 1.
2.2.Data collection
Patient-specific information in the following categories was collected: demographics (age, sex, intravesical or neoadjuvant chemotherapy, prior abdominal or pelvic radiation, clinical tumor stage [cT], pathological tumor stage [pT] and pathological nodal stage [pN] according to the American Joint Committee on cancer tumor-node-metastasis [TNM] system, and postoperative adjuvant treatment), surgical data (diversion type,operative time, estimated blood loss [EBL], and length of stay), and clinical data preoperatively (body mass index, smoking history, and American Society of Anesthesiologists status).Data were collected within 90 days of RARC regarding complications and hospitalizations.Additionally, cancer recurrence and survival data were collected as of the latest follow-up.Complications were graded according to the Clavien-Dindo classification system [25].
2.3.Study outcomes
The primary outcomes of our study were incidence of postoperative complications within 90 days as well as cancer recurrence and mortality at follow-up.We also assessed readmission rates within 90 days of RARC.
2.4.Statistical analysis
All analyses were performed using Python version 3.8.Descriptive statistics depicted baseline patient characteristics, operative information, and incidence of complications.Continuous variables were described by medians with interquartile ranges (IQRs), while categorical variables were depicted with counts and percentages.Differences in baseline characteristics and postoperative data were compared between diversion methods using the Mann-Whitney U test for continuous variables, and the Chi-square or Fisher’s exact test for categorical variables.Additionally, Kaplan-Meier plots depicting recurrence-free survival (RFS) and overall survival (OS) for both groups were made.Additionally, 24-month estimates for metastasis-free survival (MFS) and cancer-specific survival(CSS) were calculated.Log-rank tests were used to compare RFS, MFS, CSS, and OS.In all analyses, variables with p-value of <0.05 were considered statistically significant.
3.Results
Baseline demographics and clinical information is presented in Table 1.Of the 261 patients,190(72.8%)received IC while 71 (27.2%) received NB.A smaller proportion of male patients were in the IC group compared with NB group(73.7% vs.93.0%, p<0.001).Median age was greater in the IC group (71 [IQR 65-78] years vs.64 [IQR 59-67] years,p<0.001).Median body mass index was 26.6 (IQR 23.2-30.4) kg/m2and comparable between groups.There were more patients with prior abdominal or pelvic radiation in the IC group (30 [15.8%] vs.2 [2.8%], p=0.014).Neoadjuvant chemotherapy was utilized in 64 (24.5%) patients with comparable rates between groups.

Table 1 Baseline characteristics.
Intraoperative and postoperative outcomes are presented in Table 2.Nerve-sparing procedure was utilized in 55 (77.5%) of NB patients.Forty-eight (67.6%) underwent bilateral nerve-sparing procedure and 7 (9.9%) underwent unilateral nerve-sparing procedure.The IC group had a smaller median EBL (250 [IQR 150-500] mL vs.325[200-575] mL, p=0.002) and operative time (272 [IQR 246-306] min vs.341 [IQR 303-378] min, p<0.001), but longer median length of stay (5 [IQR 4-6] days vs.4 [IQR 3-5] days, p=0.007).One hundred and sixteen (44.4%)complications occurred within 30 days, and 131 (50.2%)occurred within 90 days,both comparable between groups.Ninety-seven (37.2%) Clavien-Dindo grades 1-2 complications occurred, and 34 (13.0%) Clavien-Dindo grades 3-5 complications occurred with comparable rates between the groups.Clavien-Dindo grades 3-5 complications occurred in 27 (10.3%) and 34 (13.0%) patients within 30 days and 90 days, respectively.Overall, 50 (19.2%) readmissions occurred within 30 days and 68(26.1%)readmissions within 90 days, with comparable rates between groups.
Pathologic outcomes are presented in Table 3.The IC group had a higher proportion of patients with pT2 tumors(34 [17.9%] vs.10 [14.1%], p=0.008) and pN2-N3 (28[14.7%] vs.3 [4.2%], p<0.001).Positive surgical margins were found in 9 (3.4%) patients with comparable rates between groups.Overall, median follow-up was 324 (IQR 167-552) days.Cancer recurrence has occurred in 48 (18.4%) patients.Mortality occurred in 14 (5.4%) patients.Kaplan-Meier analysis of OS is shown in Fig.1.Estimated OS at 24 months was 89% for the IC cohort and 93%for the NB cohort (hazard ratio [HR] 1.23, 95% confidence interval [CI] 1.05-2.42, p=0.02).Kaplan-Meier analysis of RFS is shown in Fig.2.Estimated RFS at 24 months was 74%for IC and 87%for NB(HR 1.81,95%CI 0.82-4.04,p=0.10).Estimated MFS at 24 months was 86% for IC and 91% for NB(HR:1.56, 95%CI 1.29-1.89,p=0.07).Estimated CSS at 24 months was 95% for IC and 99% for NB (HR: 3.66, 95% CI 2.22-5.08, p<0.001).

Table 2 Information on intraoperative and postoperative outcomes.
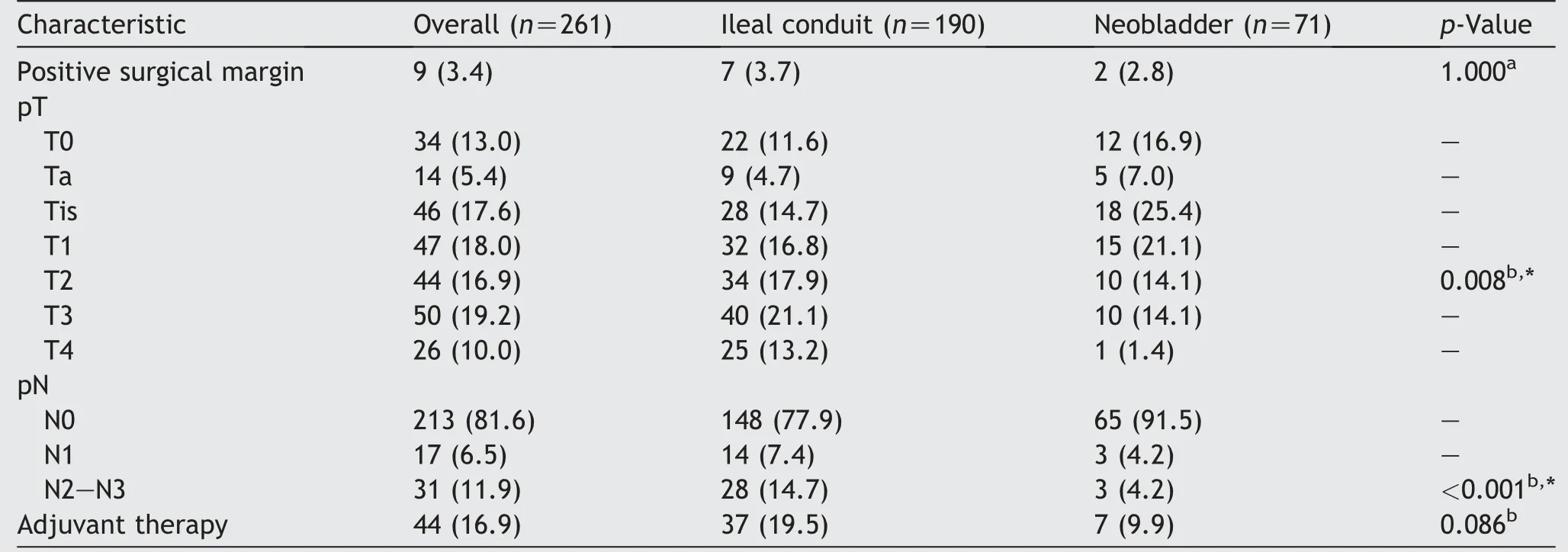
Table 3 Pathologic outcomes.
4.Discussion
In this study, we compare perioperative, complications,and oncologic outcomes between patients who underwent RARC with ICUD using IC versus NB.Our data demonstrate that the biggest differences between these two groups were in baseline characteristics and perioperative data.No significant difference was seen in complication rates or RFS, but OS was worse for patients undergoing RARC with IC.

Figure 1 Kaplan-Meier curve for overall survival (n=261).HR, hazard ratio; CI, confidence interval.
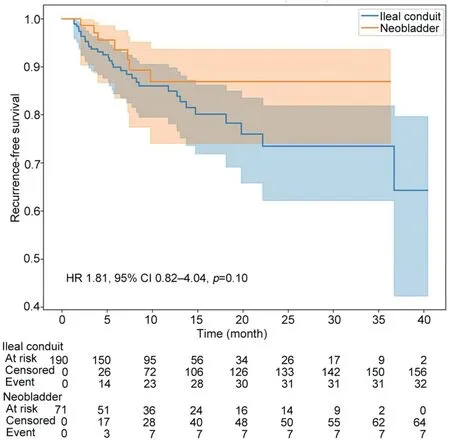
Figure 2 Kaplan-Meier curve for recurrence-free survival(n=261).HR, hazard ratio; CI, confidence interval.
Several differences were seen in baseline characteristics between the IC and NB groups, including age, male gender,and history of prior abdominopelvic radiation.This likely represents a selection bias; patients undergoing NB require careful patient selection, and thus tend to be younger and healthier [16,20,26].The differences seen in perioperative data included a shorter operative time, less EBL, and longer hospital stay for the IC group.Operative time and EBL are explained by a difference in the technical aspects between the two surgeries,with NB representing a more complicated surgery and often nerve-sparing procedure or organ preservation, compared to IC, especially intracorporeally, and thus requiring more time to perform[15].No differences were seen in complications between the two groups; 30- and 90-day complications as well as readmissions were similar for both groups, and rates were in line with prior robotic series reported in randomized control trials [6-8].Mastroianni et al.[8] reported 42%complication rate and 28% readmission rate at Day 90 in the RARC group in their recent randomized trial.Parekh et al.[7] reported a 67% 90-day complication rate in the RARC group in their 2018 randomized trial.Catto et al.[6]reported a 63.4% rate of complication within 12 weeks and 21.8% readmission rate within 12 weeks in the RARC group of the iROC trial.Most studies concluded that overall 90-day complication rates do not differ between these two diversion techniques [14,27,28], with one study showing fewer high-grade complications with NB [27] and another finding increased reoperations in NB [14].Our study is the largest to compare these outcomes in NB and IC in RARC with totally ICUD.
Kaplan-Meier analysis demonstrated worse OS and CSS for the IC group but no statistically significant difference in RFS or MFS.Oncologic outcomes after RC depend on many variables, including tumor stage, lymph node positivity,margin status, lymphovascular invasion, age, and other comorbidities[26].The baseline differences in age,pT,and pN likely account for the decreased OS seen in the IC group.Most other studies have found that IC and NB result in equivocal oncologic outcomes, even when stratified by pathologic stage[13,29].However,Su et al.[26]found that OS and CSS were worse in IC patients compared to NB patients.Like in our study, those receiving NB tended to be male and younger; however, unlike in our study, they included predominantly ORC patients.Our study provides valuable data on the short-term outcomes for a large group of patients receiving exclusively RARC with ICUD.
NB has more contraindications compared to IC,although most patients considering RARC are candidates for NB[13,16].NB also requires intense upkeep, especially in the first year after surgery.Furthermore, manual dexterity is needed as it may necessitate intermittent straight catheterization [13].Additionally, NB is a more technically challenging surgery that is performed mostly at high-volume centers [15].It is important to consider that there is evidence that surgeons who perform RARC at the beginning of their learning curve achieve inferior perioperative and functional outcomes, and all surgeons in this study have well passed their learning curve for this procedure [30].Despite the technical challenges associated with the procedure,we showed that in experienced hands,RARC with totally intracorporeal NB can achieve comparable perioperative, complications, and oncologic outcomes compared to IC.RARC with NB is undergoing continued exploration, with some studies finding viability in patient populations in which the procedure was previously thought to be contraindicated, like those with poor renal function[31].Future studies may discover further expansion in the proportion of patients in whom NB can be successful.
Our study does have limitations that should be noted.First, our results may not be generalizable to a community setting due to all surgeries being performed at a single high-volume tertiary referral center.Additionally, our data do not include nerve-sparing information for IC patients or urethrectomy information which can affect RC time.We also only track total operative time, and thus we were not able to compare surgical time of the RC portion of the procedure or diversion time which may have provided interesting differences between techniques.Furthermore,data regarding cancer recurrence and mortality are limited by the follow-up of less than 1 year, and many BC recurrences occur over 1 year after RC [32].There was only one death in the NB group despite many patients with non-organ confined and pN2-N3 disease, and longer follow-up would surely yield more detailed oncologic outcomes.In addition,the retrospective nature of our analysis limits a more thorough and careful comparison between the two groups.As we have noted, there were statistically significant differences in baseline factors between the two groups due to differences in indications for each procedure,which invariably impact postoperative and oncologic outcomes.The aim of our study was to describe and compare outcomes between these two diversion types in a large contemporary cohort.However, our cohort was not large enough to perform a propensity-matched analysis to come to stronger conclusions regarding the impact of the type of diversion itself on the outcomes.Finally, in this study, we did not assess quality of life metrics or functional outcomes like continence which is of utmost importance for the NB group.These outcomes will be of high interest in future studies comparing diversion types in RARC.
5.Conclusion
In this large single-institutional study, patients undergoing RARC with intracorporeal NB had similar complications outcomes and improved OS compared to patients undergoing RARC with intracorporeal IC.Further studies,especially prospective ones, are needed to fully characterize the major differences between these two groups.
Author contributions
Study concept and design: Reza Mehrazin, Peter N.Wiklund, John P.Sfakianos.
Data acquisition:Reza Mehrazin,Peter N.Wiklund,John P.Sfakianos, Kyrollis Attalla, Jordan M.Rich, Etienne Lavallee, Nikhil Wangankar.
Data analysis: Daniel Ranti.
Drafting of manuscript: Jordan M.Rich, Shivaram Cumarasamy, Reza Mehrazin.
Critical revision of the manuscript: Reza Mehrazin.
Conflicts of interest
The authors declare no conflict of interest.
Acknowledgements
We would like to acknowledge the Menon Family Foundation for its financial support of the research for the author Rich JM.
杂志排行
Asian Journal of Urology的其它文章
- Robot-assisted adrenalectomy: Step-by-step technique and surgical outcomes at a high-volume robotic center
- The application of internal suspension technique in retroperitoneal robot-assisted laparoscopic partial nephrectomy with a new robotic system KangDuo Surgical Robot-01: Initial experience
- A systematic review of robot-assisted partial nephrectomy outcomes for advanced indications: Large tumors (cT2-T3), solitary kidney, completely endophytic, hilar,recurrent, and multiple renal tumors
- Three-dimensional automatic artificial intelligence driven augmented-reality selective biopsy during nerve-sparing robot-assisted radical prostatectomy:A feasibility and accuracy study
- First 100 cases of transvesical single-port robotic radical prostatectomy
- Robot-assisted oncologic pelvic surgery with Hugo™robot-assisted surgery system: A single-center experience
