In vitro study on the transmission of multidrug-resistant bacteria from textiles to pig skin
2023-12-22PavlinaLenaSpyridonKarageorgosMariaLiatsouArisAgouridisNikolaosSpernovasilisDemetrisLamnisosPanagiotisPapageorgisConstantinosTsioutis
Pavlina Lena,Spyridon Karageorgos,Maria Liatsou,Aris P Agouridis,Nikolaos Spernovasilis,Demetris Lamnisos,Panagiotis Papageorgis,Constantinos Tsioutis
Abstract BACKGROUND The survival of microorganisms on textiles and specifically on healthcare professionals’ (HCP) attire has been demonstrated in several studies. The ability of microorganisms to adhere and remain on textiles for up to hours or days raises questions as to their possible role in transmission from textile to skin via HCP to patients.AIM To evaluate the presence, survival and transmission of different multidrugresistant bacteria (MDRB) from HCP attire onto skin.METHODS Three MDRB [methicillin-resistant Staphylococcus aureus (MRSA); vancomycinresistant Enterococcus faecium (VRE); carbapenem-resistant Klebsiella pneumoniae, CRKP)] were inoculated on textiles from scrubs (60% cotton-40% polyester) and white coat (100% cotton) at concentrations of 108 colony-forming units (CFU), 105 CFU, and 103 CFU per mL. The inoculation of swatches was divided in time intervals of 1 min, 5 min, 15 min, 30 min, 1 h, 2 h, 3 h, 4 h, 5 h, and 6 h. At the end of each period, textiles were imprinted onto pig skins and each skin square was inverted onto three different selective chromogenic media. Growth from the pig skin squares was recorded for the 3 MDRB at the three above concentrations, for the whole length of the 6-h experiment.RESULTS MRSA was recovered from pig skins at all concentrations for the whole duration of the 6-h study. VRE was recovered from the concentration of 108 CFU/mL for 6 h and from 105 CFU/mL for up to 3 h, while showing no growth at 103 CFU/mL. CRKP was recovered from 108 CFU/mL for 6 h, up to 30 min from 105 CFU/mL and for 1 min from the concentration of 103 CFU/mL.CONCLUSION Evidence from the current study shows that MRSA can persist on textiles and transmit to skin for 6 h even at low concentrations. The fact that all MDRB can be sustained and transferred to skin even at lower concentrations, supports that textiles are implicated as vectors of bacterial spread.
Key Words: Textiles; Attire; Multidrug-resistant bacteria; Methicillin-resistant Staphylococcus aureus; Vancomycin-resistant Enterococcus faecium; Extended-spectrum b-lactamase; Pig skin; Skin; Transmission
INTRODUCTION
It is well established that textiles can carry micro-organisms, a fact with raises concerns for their ability to transmit them either onto skin or to other textiles[1]. Previous studies and systematic reviews have demonstrated the ability of pathogens, including multidrug-resistant bacteria (MDRB), to survive on healthcare professionals’ (HCP) attire, devices and surfaces in hospitals and long-term care facilities, thus raising the need to study their potential to contribute to transmission[1-4].
Cyprus is considered a high-prevalence country for MDRB. In fact, in healthcare-associated infections in Cyprus hospitals in 2020, methicillin-resistantStaphylococcus aureus(S.aureus) (MRSA) was detected in 49.1% of invasive infections byS.aureus, vancomycin-resistantEnterococcus faecium(E.faecium) (VRE) accounted for 44.1% of enterococci, and isolates ofKlebsiella pneumoniae(K.pneumoniae) exhibited multidrug resistance in 18.2% and carbapenem resistance in 19.8%[5]. Further to this, in a previous study, our group demonstrated the presence of several different MDRB on HCP uniforms in hospitals and long-term care facilities in Cyprus, including MRSA, VRE, extended-spectrum b-lactamase (ESBL)-producing bacteria and carbapenem-resistant bacteria[1]. These findings suggest that MDRB may be transmitted in different ways within healthcare settings, thus raising the need to identify additional areas for targeted interventions and improvement.
A demonstrable means to evaluate the role of attire and textiles in the transmission cycle, is by studying the degree of transmission of micro-organisms from fabrics to skin. To achieve this, it is necessary to use an alternative to human skin with similar properties, such as pig skin, in order to allow accuratein-vitroexperimentation[6]. The similarities between human and pig skin lie in the structure of epidermis and thickness ratios between dermis and epidermis, as well as in hair follicle and blood vessel patterns. In contrast to the skin of other animals used in laboratory studies, the dermal collagen and elastic content of the pig skin are more similar to the skin of humans. Furthermore, Schmooket al[7] demonstrated in anin-vitrostudy of percutaneous absorption, that in the absence of human tissue, pig skin was the most suitable model.
Based on current literature, including experimental and observational studies, we hypothesize that MDRB can carry the ability to survive on textiles to a considerable extent to be isolated and to transmit onto skin. Our aim was to evaluate the survival potential of different MDRB on different types of textiles and to evaluate their potential for transmission onto skin, using representative strains such as MRSA, VRE and carbapenem-resistantK.pneumoniae(CRKP).
MATERlALS AND METHODS
Aims
The aim of the current study was to determine the viability of MDRB over a 6-h period, which mimics the usual duration of a hospital shift, on two types of textiles and to evaluate whether these inoculated textiles can colonize pig skin using three MDRB (MRSA, VRE and CRKP) at different concentrations. Study approval was not required as it did not involve human subjects or animals. The strains were retrieved from a previous study that was approved by the Cyprus National Bioethics Committee (decision number “EEBK EΠ 2018.01.155”).
Materials
Fresh MRSA, VRE and CRKP cultures were grown from previously isolated organisms from HCP uniforms from a previous study, that were stored in -20 °C. After 24 h of incubation, the organisms were prepared at 0.5 MacFarland standard each. Their precise concentrations were calculated: 1.18 × 108CFU/mL MRSA, 1.6 × 108CFU/mL forE.faecium, and 1.14 × 108CFU/mL forK.pneumoniae.All 3 organisms were serially diluted from 108CFU down to 102CFU. The concentrations of 108, 105, and 103CFU per mL were used during the process.
Textile swatches were cut in squares of 1.5 cm × 1.5 cm and sterilised in 100 °C in dry oven for 2 h. The swatches were taken from uniforms and scrubs used in healthcare settings in order to mimic txextiles used in real-life conditions, with a composition of 60% cotton and 40% polyester (T1, taken from a used scrub uniform of a nurse, who had worn it for 6 mo), and 100% cotton (T2, taken from a white coat used by a physician for 6 mo). Aluminium foil squares of 1.5 cm × 1.5 cm were cut and heat sterilised in the same manner as the cloth swathes. These would be used as a barrier when pressure would be applied on cloth or skin.
Fresh pig skin (commercially retrieved 24 h after slaughtering), cleared from most of the fat under the dermis, was scrubbed and washed with chlorhexidine soap and then with alcohol. The cleaned skin was then dried in examination paper and kept covered to avoid drying. When the experiment was ready to begin, square pieces of 1.5 cm × 1.5 cm of skin were cut using sterilized blades. Negative control skin samples were incubated on the 3 chromogenic media to ensure the absence of the 3 microorganisms used. The specialized chromogenic media used were CHROMO agar, MRSA medium, chromo VRE, and chromo ESBL.
Experimental design
The current experimental study was designed in duration and environmental conditions that mimic the working conditions within a 6-h HCP shift. Temperature of the laboratory room was kept constant at 22.9-23.5 °C and humidity of 49%-53% and the experiment was conducted on the bench.
Each microbial concentration had 10 stations allocated at time intervals of 1 min, 5 min, 15 min, 30 min, 1 h, and then every hour for a total of 6 h and at three different concentrations. Each station had in place: 2 cloth swatches (T1 & T2), 2 respective skin squares (S1 &S2) and chromogenic plates, for each of the 3 dilutions of the microorganisms (Figure 1).
Figure 1 Experimental set up: Each station contains 2 cloth swatches (T1 & T2), 2 pig skins (S1 & S2), and one chromogenic agar.
Firstly, 2 cloth swatches in each station were inoculated with 50 μL of each dilution in each column. The inoculation started from 6 h up to 1 min, guided by stopwatches. At the end of each time slot, each cloth swatch was placed on top of the skin square. The cloth was applied onto skin with a pressure of 100 Gr (friction asset) for 5 s and foil was placed over it for protection. Afterwards and following the same technique, each skin square was pressed onto the chromogenic agar. The plates were then incubated at 37 °C. After 24 h, the incubated plates were checked and incubated for an additional 24 h. When the 48-h incubation period ended, the chromogenic plates were inspected, and the presence of growth was recorded. We did not perform a concentration count at each station; the results indicated presence or not. Thus, the experiment was performed based on the assumption that even a small amount of bacteria could be transmitted and possibly cause infection.
RESULTS
Over a period of 6 h and at different time points, a total of 3 MDRB (MRSA, VRE, CRKP) were inoculated in 3 different concentrations (108CFU/mL, 105CFU/mL, 103CFU/mL) on 2 different cloth textiles (T1, T2) and then each cloth was applied on a pig skin square (S1, S2 respectively). The skin inoculates were then cultured on special medium for 48 h and MDRB growth was recorded.
All findings demonstrating the recovery of the 3 MDRB from skin and textiles are presented in Table 1. Recovery times for all 3 MDRB were the same in both skin swatches S1 and S2 that were in contact with T1 (60% cotton and 40% polyester) and T2 (100% cotton), respectively. Overall, no differences were observed in terms of growth for each MDRB between the two types of textiles. MRSA exhibited the highest recovery. In specific, recovery of MRSA was successful at all time intervals and for all 3 concentrations (108CFU/mL, 105CFU/mL and 103CFU/mL). MRSA remained detectable and could be transmitted throughout the 6-h experiment duration. VRE was recovered from the highest concentration of108CFU/mL for the whole duration of the 6-h period and for up to 3 h from the 105CFU/mL concentration. No recovery of VRE was recorded from the lowest concentration of 103CFU/mL. CRKP was also recovered from the highest concentration of 108CFU/mL for the total duration of 6 h (duration of the experiment) and for 30 min from the second highest concentration (105CFU/mL), whereas it was recovered for only up to 1 min from the lowest concentration of 103CFU/mL.
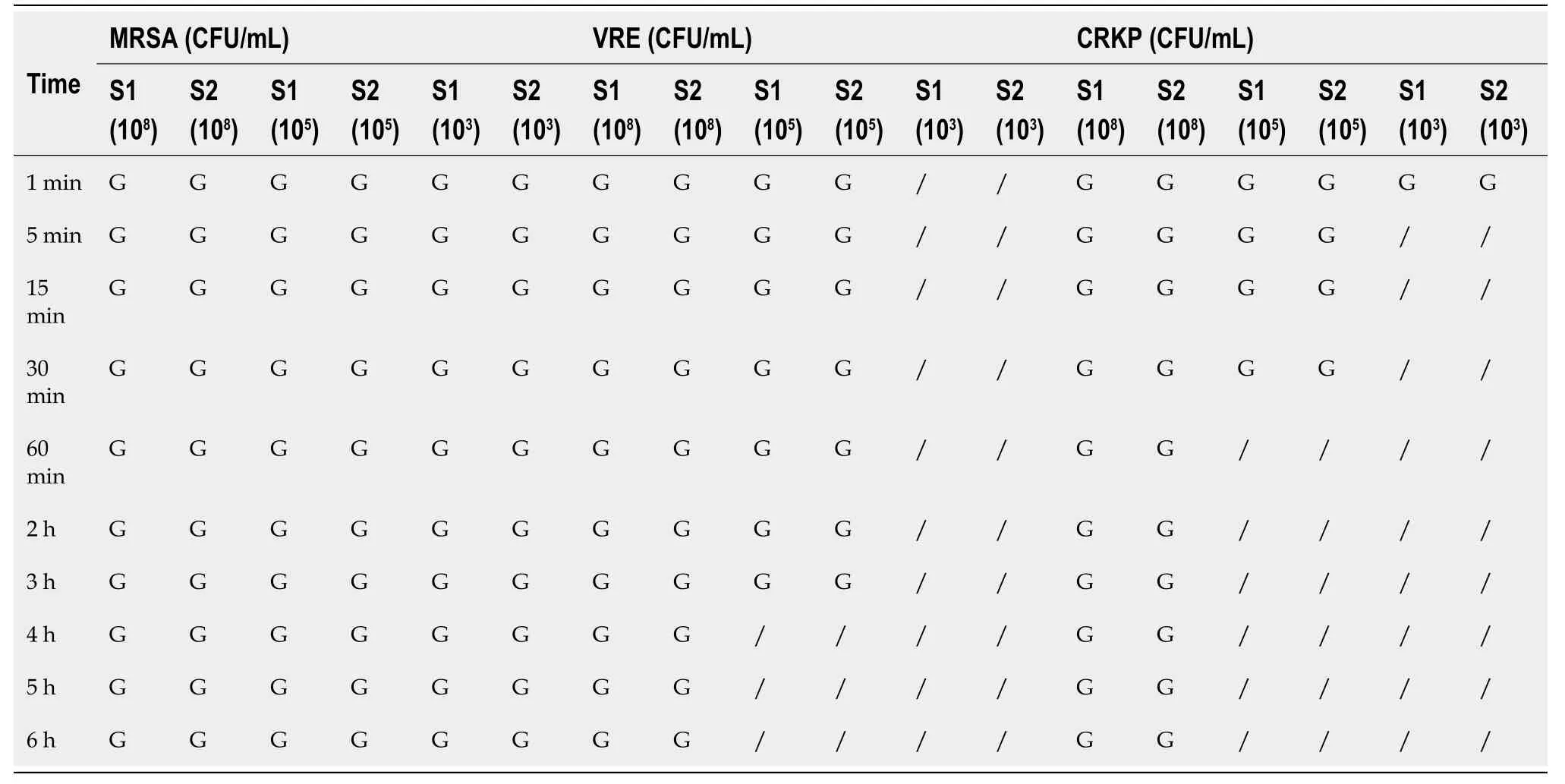
Table 1 Growth indicated in skin swatches S1 from textile T1 (cotton-polyester cloth) and S2 from T2 (100% cotton cloth), when imprinted on chromogenic agars at three concentrations
Conclusively, our results support the sustainability of MRSA for the maximum of the duration of the study in all concentrations. The other gram-positive coccus (VRE) also remained for the whole duration of the study but only in the highest concentration, whereas VRE was not isolated for the lowest concentration. In contrast, the gram-negative bacterium (CRKP) remained for less time in the concentration of 105CFU/mL and for only 1 min at the lowest concentration.
DlSCUSSlON
In our study, involving the transfer and presence of MDRB as a result of contact between textiles and pig skin, MRSA exhibited the longest persistence out of the 3 studied MDRB and over the duration of 6 h of the experiment. VRE and CRKP were both detected at the highest concentration of 105CFU/mL, for up to 3 h and 30 min, respectively. The presence of MDRB, as recorded on both textile types that were used in the study, was also confirmed on pig skin, which provides evidence of potential for transfer of bacteria and MDRB onto skin from contaminated textiles and furthermore, suggesting this as a transmission mode to patients. The study results show that gram-positive cocci, such as staphylococci and enterococci, are more resilient on textiles and in the environment over time, whereas CRKP also showed prolonged presence at higher concentrations.
To our knowledge, only few previous studies have evaluated the transferability of bacteria onto skin. Butleret al[8] conducted a study on the transfer of bacteria onto pigskin by use of white coats. Specifically, MRSA, VRE andAcinetobacter baumannii(A.baumannii) (reported as pan-resistant) were inoculated on cloth swatches and rubbed on sanitized pigskin. All 3 MDRB exhibited ability to transfer from cloth to pig skin at time intervals of 1, 5 and 30 min, whereasA.baumanniiwas transferred up to a dilution of 1:1000. Desaiet al[9] also confirmed sustainability and transmission of MRSA from cotton towels and bedsheets to pig skin for long periods reaching up to 14 d, whereas Sattaret al[10] reported transfer of MRSA from textiles (cotton and polycotton) to other textiles and to finger skin. The transfer was fivefold higher when the textile was moist and when there was friction. Varshneyet al[11] in a study transfer between textiles ofAcinetobacter calcoaceticus,Escherichia coli(E.coli) andS.aureus,also reported that cell transfer varied between 5%-61% when friction was applied compared to non-friction, which suggested the importance of the role of rubbing between same textiles. Malnicket al[12] examined the transfer of bacteria between fabric and surrogate skin taking into consideration the effect of surface energy and surface roughness of fabrics, while usingE.coliandS.aureusagainst 100% cotton, 100% polyester and a 50-50 blend of both. Their conclusion was that the 100% polyester attracted the highest number of bacteria.
The survival ability of microorganisms on textiles has been previously addressed by several studies. Kocaet al[13] used different fabrics, such as cotton, cotton-polyester, silk, and wool. To assess persistence of a variety micro-organisms, including yeasts, fungi, MRSA, VRE and ESBL-producing bacteria. Results showed that VRE had its longest survival on cotton-polyester fabrics (51 d, and 49 d on 100% cotton, silk and wool). MRSA had the longest survival period of 41 d on wool and 37 d on cotton silk and cotton-polyester. RespectivelyE.colishowed its longest survival for 45 d on cotton, silk and wool, and on cotton-polyester 37 d. These findings were confirmed by Malnicket al[12] who showed that 50% of VRE-swabbed pyjamas and bed sheets yielded micro-organisms overnight. Similarly, Neely and Maley[3] studied the survival of strains of MRSA and VRE on five different types of materials used commonly in hospitals: 100% cotton (which represented cloths and towels), cotton-polyester, 100% polyester, and 100% polypropylene plastic (represented which splash aprons). MRSA had the longest survival on polypropylene plastic (> 51 d), followed by 40 d (polyester), and 21 d (cotton). VRE exhibited long survival periods of > 80 d on polypropylene plastic and polyester, and 22 d on the other materials.
In agreement with the above findings, a literature review supported that contaminated textiles can harbour bacteria and consequently transmit infection for weeks[14]. Current evidence supports survival and persistence on textiles not only of bacteria, but also mycobacteria, fungi and viruses. Specifically, VRE can survive for more than 90 d, MRSA for up to 56 d andK.pneumoniaefor 11 d. Survival at room temperature favoured polyester against cotton. Even though there is only a limited number of reported healthcare-associated infection outbreaks associated with contaminated textiles[15-19], their involvement may be undermined, and not sought out during incidences or as part of the general infection control process.
Taken cumulatively, the findings of our study add insight to the literature and clearly suggest that staff attire, including uniforms and scrubs, when contaminated, can transmit pathogenic micro-organisms onto patients’ skin, thus acting as bacterial vectors. It can also be assumed that contaminated hands can in turn contaminate uniforms[10]. Hence, strict and targeted preventive measures targeting textile and attire are needed to break the chain of transmission. Current evidence from various studies suggests against the use of white coats and ties in healthcare settings, as they are more frequently contaminated compared to other HCP attire[4]. On the other hand, short-sleeved uniforms can be more beneficial as regards to lower transmission of pathogenic micro-organisms[20]. However, these measures alone seem insufficient to control MDRB spread and support the need for additional control measures, such as ensuring application of appropriate home laundering practices, use of a hospital laundry service, wearing single-use protective aprons or gowns wherever applicable, promoting hand hygiene before and after patient interaction, daily uniform change, and application of contact precautions particularly in high-prevalence settings[21,22]. Our experimental study was performed under the same environmental conditions for all 3 studied MDRB. Therefore, the different observations in regard to time intervals and concentrations among the 3 studied MDRB in our study, probably reflect the properties of these bacterial strains.
The strength of the current study lies in its design, which aimed to resemble as much as possible a real-life situation. Specifically, in addition to evaluating the possibility of textile inoculation and transfer onto pig skin, we confirmed the viability of clinically important MDRB over time, in an attempt to mimic the environmental conditions in healthcare settings during HCP shifts. Our findings demonstrate that 6 h after MDRB inoculation of textiles, transfer from a dry textile surface on pig skin was possible. Simulation of real-life conditions showed that MDRB can survive, grow and transmit from textiles of two different compositions onto pig skin, which is the closest parallel to human skin.
Limitations of our study include the small spectrum of micro-organisms used and the fact that we used only two types of fabrics. We also acknowledge the fact that during our experiment, we didn’t quantify the bacterial colony concentrations after inoculation. However, we performed the experiment under the hypothesis that bacterial persistence through time and transmission is evidence that textiles can be infectious, regardless of the growth amount. In addressing the current research gaps in the literature and the limitations of our study, future studies can include inoculation of textiles not solely with pure bacterial cultures, but also mixed with organic matter such as bodily fluids, to better emulate real-life conditions. Furthermore, the role of skin flora could be investigated in the survival of microorganisms on textiles and to evaluate their effect on MDRB binding capacity and replication.
Of note, only few similar studies have attempted to associate textiles with the transmission and survival of microorganisms. In line with the general perception that the risk of transmission from textiles is low, there is not enough emphasis given to the importance of cleaning and decontamination of textiles, compared to other inanimate surfaces[22,23]. However, our findings are supportive that textiles can be responsible for the transmission of pathogens in healthcare settings and thus, they should be managed accordingly. Moreover, our study strongly suggests that textiles should be included in the transmission triad “patient - healthcare professional - environment”. To this end, healthcare settings should opt to analyse all possible steps in the chain of transmission and introduce appropriate action plans that include reduction of transmission risk through textiles and HCP attire. In the absence of protocols for testing uniform cleanliness and compliance, our findings provide evidence towards enforcing appropriate measures to reduce bacterial reservoirs in healthcare settings.
CONCLUSlON
In conclusion, the current experimental study using 3 types of MDRB, provides evidence of their sustainability and transmission from textiles to skin. MRSA exhibited maximum sustainability for the whole duration of the 6-h study in all concentrations, VRE also remained for the whole duration of the study but only in the highest concentration, whereas CRKP remained for less time overall. Cumulatively, our data adds support to increasing evidence that textiles should be considered as vehicles of transmission in the healthcare setting.
ARTlCLE HlGHLlGHTS
Research background
The isolation of microorganisms from textiles, including healthcare professionals’ (HCP) attire, has been previously demonstrated in several studies.
Research motivation
The ability of microorganisms to adhere and survive on textiles, raises questions as to their possible role in transmission from textile to skin in healthcare environments.
Research objectives
The present experimental study aimed to evaluate the presence, survival and transmission of different multidrugresistant bacteria (MDRB) from HCP attire onto skin.
Research methods
Inoculation of 3 MDRB [methicillin-resistantStaphylococcus aureus(MRSA); vancomycin-resistantEnterococcus faecium(VRE); carbapenem-resistantKlebsiella pneumoniae, CRKP)] on textiles from two types of textiles (60% cotton-40% polyester and 100% cotton) at 3 different concentrations (108CFU, 105CFU and 103CFU per mL) and at different time intervals ranging from 1 min to 6 h. At the end of each time period, textiles were imprinted onto pig skins and each skin square was inverted onto selective chromogenic media. Growth from the pig skins was recorded for the 3 MDRB at the three above concentrations, for the whole length of the 6-h experiment.
Research results
Recovery of MDRB from pig skins differed for each strain, with MRSA recording the longest and most sustained recovery at all concentrations and for up to 6 h. VRE showed no growth from 103CFU/mL and was recovered from 108CFU/mL for 6 h and from at 105CFU/mL for up to 3 h.CRKP was recovered from 108CFU/mL for 6 h, up to 30 min from 105CFU/mL and for only 1 min from 103CFU/mL.
Research conclusions
Evidence from the current study shows that all 3 studied MDRB can be sustained and transferred onto skin, with MRSA showing the highest level of persistence on textiles and transmission to skin even at low concentrations.
Research perspectives
Our findings support that textiles can be implicated as vectors of bacterial spread.
ACKNOWLEDGEMENTS
The current study was performed as part of the PhD thesis of Dr Pavlina Lena, at the European University Cyprus.
FOOTNOTES
Author contributions:Lena P contributed to the conceptualization of this study; Lena P, Liatsou M, Lamnisos D, Papageorgis P, and Tsioutis C involved in the methodology of the manuscript; Lena P, Karageorgos S, Agouridis AP, Spernovasilis N, Lamnisos D, Papageorgis P, and Tsioutis C participated in the formal analysis and investigation of this manuscript; Lena P, Karageorgos S, and Tsioutis C drafted the manuscript; Lena P, Karageorgos S, Agouridis AP, Spernovasilis N, and Tsioutis C contributed to the review and editing of this manuscript; Lena P, Papageorgis P, and Tsioutis C involved in the supervision of this study; and all authors approved final article version published.
lnstitutional review board statement:Approval was not required it did not involve human subjects or animals.
Conflict-of-interest statement:All the authors report no relevant conflicts of interest for this article.
Data sharing statement:No additional data to those presented in the study are available.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Cyprus
ORClD number:Nikolaos Spernovasilis 0000-0002-6981-8535; Constantinos Tsioutis 0000-0002-7865-8529.
S-Editor:Wang JJ
L-Editor:A
P-Editor:Yuan YY
杂志排行
World Journal of Experimental Medicine的其它文章
- Altered expression of miR-125a and dysregulated cytokines in systemic lupus erythematosus: Unveiling diagnostic and prognostic markers
- Red cell distribution width: A predictor of the severity of hypertriglyceridemia-induced acute pancreatitis
- Ground level utility of Access, Watch, Reserve classification: lnsights from a tertiary care center in North lndia
- Exploring the mechanism of action bitter melon in the treatment of breast cancer by network pharmacology
- Research on nanosciences involvement in pharmaceutical education should be reinforced
