Neurological manifestations of COVID-19 infection: A case series
2023-12-16AyimenKhalidKhanAnamKhanAmmarKhalidKhanShayanSiratMaheenAnwar
Ayimen Khalid Khan, Anam Khan✉, Ammar Khalid Khan, Shayan Sirat Maheen Anwar
1Department of Radiology, Aga Khan University, Karachi, Pakistan
2Department of Neurosurgery, Pakistan Institute of Medical Sciences, Islamabad, Pakistan
ABSTRACT
KEYWORDS: Case series; Coronavirus; COVID-19; Infectious disease; Neurological; MRI
1.Introduction
The World Health Organization proclaimed the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection a pandemic in March 2020[1].It has spread over the world with more than 70 million cases confirmed to date[2].The respiratory system is the most commonly affected, however, this virus has been demonstrated to be neurotropic in various medical research and case reports[3].Patients with SARS-CoV-2 have complaints of headache, nausea, vomiting, myalgia, dizziness, hypogeusia,hyposmia, and decreased consciousness, which reflect nervous system involvement[3,4].
Even though the specific process by which SARS-CoV-2 infects the central nervous system has yet to be discovered, two hypotheses appear to be the most likely[5].The first one is the hematogenous transmission of SARS-CoV-2 from systemic to cerebral circulation,where the virus can damage the capillary endothelium and gain access to the brain due to the slower flow[4].The second route of spread could be via the cribriform plate and olfactory bulb[5].
A wide array of neurological manifestations have been reported in association with COVID-19 infection[6].Comprehensive clinical,radiological, and epidemiological studies are warranted to define the occurrence and burden of neurological symptoms correlated with COVID-19.It’s critical to be aware of the potential neurological symptoms in COVID-19 patients so that clinicians can promptly intervene and manage potentially life-threatening neurologic problems.Hence, we present five cases to highlight neurological and radiological findings significantly associated with SARS-CoV-2 infection.
2.Case reports
This retrospective, consecutive sampling, single-center study was conducted at a tertiary care hospital with patients with SARS-CoV-2 infection and neurological manifestations.Informed consent was obtained from the patients.Approval was obtained from the Aga Khan University ethics committee (Approved number: 2022-8098-23071).A summary of demographic and neurological findings of the studied patients is listed in Table 1.
2.1.Case 1
A 63-years-old male, COVID-19 patient underwent magnetic resonance imaging (MRI) brain for neurological assessment.Multifocal intraparenchymal hemorrhages, mild bilateral intraventricular hemorrhages, and mild subdural hemorrhage along with left tentorium cerebelli were observed (Figure 1A-1C).Cerebral venous sinus thrombosis (CVST) involving the left jugular vein and left sigmoid sinus was noted.Diffuse patchy-meningeal post-contrast enhancement was also identified (Figure 1D-1F).
2.2.Case 2
The MRI of a 60-year-old male patient showed multifocal supra, infratentorial acute, and subacute infarction, in conjunction with hemorrhagic conversion of right cerebellar infarction and mild intraventricular extension.The right cerebellar haematoma compressed the fourth ventricle and subarachnoid hemorrhage with reactive meningeal enhancement was also seen.Intraventricular extension with hemorrhage and diffusion restriction in the occipital horns was observed.In this patient, scalp hematoma with soft tissue swelling and enhancement along the right parietal bone was also detected (Figure 2).
2.3.Case 3
In a 30-year-old male patient, CVST was observed with an area of abnormal signals in the right frontal lobe parasagittal location near the high vertex in association with meningeal enhancement.Thrombosed right cortical vein with right frontal lobe venous infarction and associated hemorrhage, subarachnoid component,and diffuse vascular congestion were observed.These findings were secondary to focal meningoencephalitis.The possibility of venous infarct secondary to underlying CVST with reactive meningeal enhancement was also a differential diagnosis (Figure 3A-3D and Figure 3E-3H).
2.4.Case 4
A 75-year-old male had multifocal acute right cortical and deep watershed territory infarcts in anterior circulation on MRI.Hemorrhagic conversion in the right occipital lobe and diffuse intracranial atherosclerosis with a relatively attenuated right internal carotid artery raised a suspicion of proximal stenosis (Figure 4).
2.5.Case 5
A 1-year-old male patient was diagnosed with COVID-19 encephalopathy mimicking posterior reversible encephalopathy syndrome.On MRI, multifocal acute infarctions in supratentorial brain parenchyma and a few microhemorrhages in the brain were observed (Figure 5).Thromboembolic phenomena secondary to COVID-19 were suspected.No evidence of cerebral venous sinus thrombosis was found.Magnetic resonance angiography examination showed normal intracranial arteries.
3.Discussion
Viruses can infect the neurological system in a variety of ways.Angiotensin-converting enzyme 2 receptors have been found in glial cells and neurons in the brain, making them a possible target ofSARS-CoV-2[6].Hence, the main objective of this study is to report the neurological findings in patients with COVID-19.This article also highlights the mechanism by which this virus tends to conquer the brain cells and cause mild to severe complications.
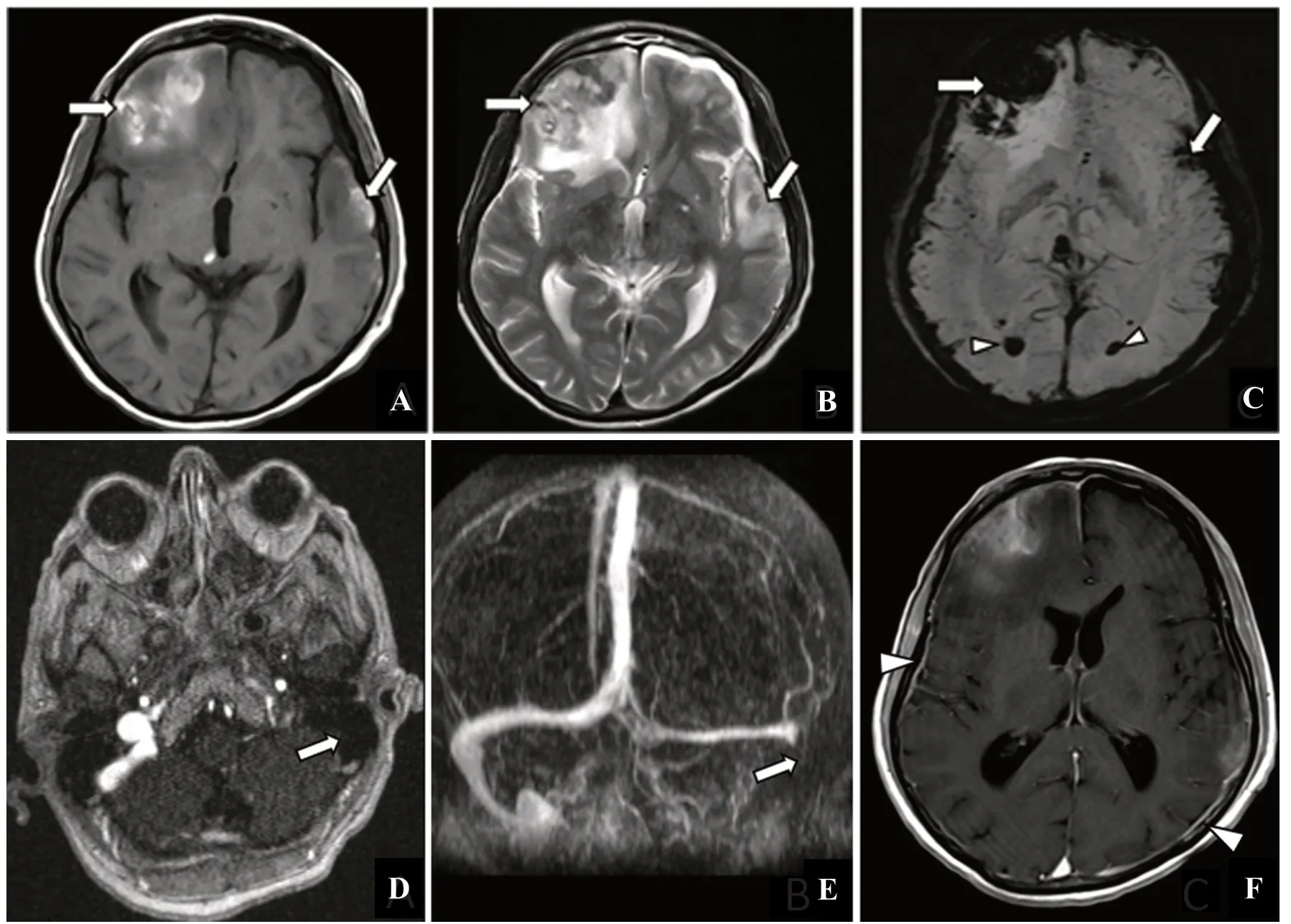
Figure 1.The MRI of a 63-years-old male, COVID-19 patient.(A) Axial T1-weighted, (B) T2-weighted, and (C) susceptibilityweighted images (SWI) showing hyperintense signals on T1 and T2 sequence and corresponding signal dropout on SWI (A-C arrows).Intraventricular hemorrhage is also noted ( C arrowheads).(D) Axial contrast-enhanced magnetic resonance venography, (E) maximum intensity projection, and (F) axial post-contrast T1 showing filling defect in left internal jugular vein and sigmoid sinus (D, E arrows).Diffuse pachy-meningeal enhancement is also seen ( F arrowheads).
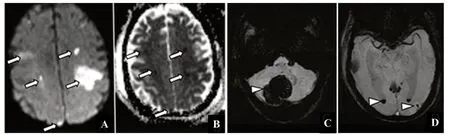
Figure 2.The MRI of a 60-year-old male, COVID-19 patient.(A) Diffusion-weighted imaging, (B) apparent diffusion coefficient, and (C,D) susceptibility-weighted imaging showing multifocal acute and subacute infarcts (arrows).Hemorrhagic conversion of right cerebellar infarct, subarachnoid hemorrhage, and intraventricular extension of hemorrhage were also noted (arrowheads).

Figure 3.The contrast-enhanced magnetic resonance venography of a 30-year-old male, COVID-19 patient showing extensive cerebral venous sinus thrombosis involving superior sagittal sinus and sigmoid sinus (A, C, and D arrows).A thrombosed cortical vein is also seen (B arrowhead).Images A through D represent successive axial sections from the vertex downward.(E, F) Axial T1 pre- and post-contrast and(G, H) coronal FLAIR pre- and post-contrast images showing T1 hypointense and FLAIR hyperintense signals (E, G arrows) in the right parasagittal region with associated meningeal enhancement (F, H arrowhead).

Figure 4.The MRI of a 75-year-old male, COVID-19 patient.(A, C) Diffusion-weighted images, (B) susceptibility-weighted image, and(D) apparent diffusion coefficient image showing multifocal acute right cortical and deep watershed territory infarcts in anterior circulation(arrows).Hemorrhagic conversion in the right occipital lobe (arrowhead).
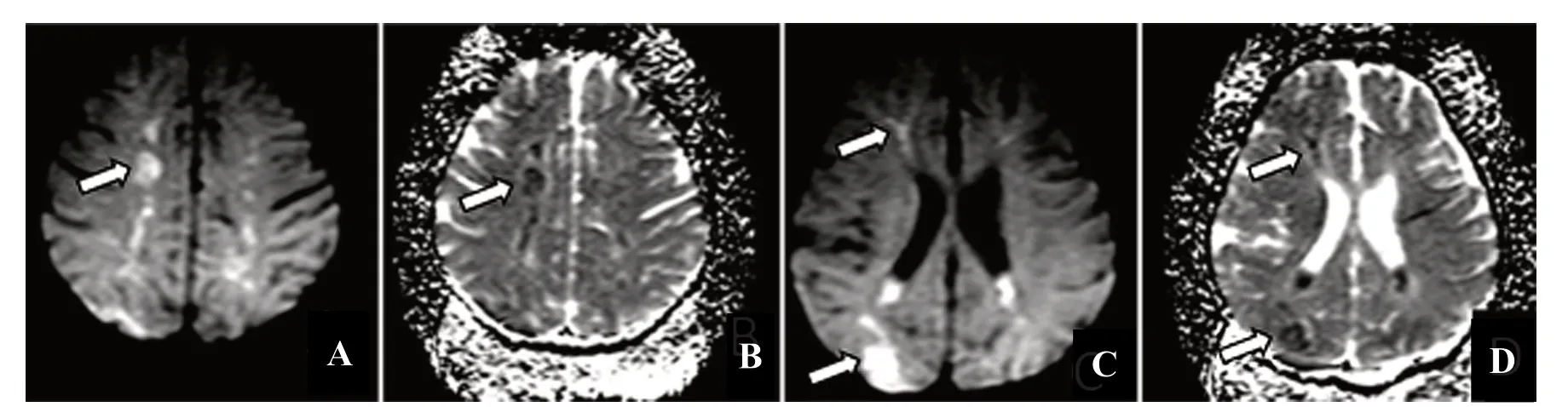
Figure 5.The MRI of a 1-year-old male, COVID-19 patient.(A, C) Diffusion-weighted images and (B, D) apparent diffusion coefficient images showing supratentorial infarcts involving periventricular region and centrum semiovale bilaterally (arrows).
CVST was observed in two patients of different age groups in cases 1 and 3, involving the left internal jugular vein, sigmoid sinus, and superior sagittal sinus, respectively.The patient in case 3 had his entire right lobe affected.A similar case was reported in a younger patient which goes on to show that there might be a link between COVID-19 and deteriorating neurological conditions[7].The mechanism of thrombophilia associated with COVID-19 infection is still unknown.However, one likely explanation could be the intense inflammatory response induced by COVID-19 infection that causes a cytokine storm that can eventually lead to a pro-coagulable state[8,9].Cases 2, 3, and 4 showed multiple hemorrhages and infarctions.For instance, in case 2, an elderly patient, reported hematoma compressing the fourth ventricle.An intriguing thing to notice is that most of the cases of neurological deterioration are found in elderly males rather than females[10].In case 4, the hemorrhaging could be age-related as the patient is old and could have a history of stroke which could have possibly led to this condition.Lastly, a unique case of a 1-year-old male patient having COVID-19 encephalopathy mimicking posterior reversible encephalopathy syndrome is reported in this study.Infarctions and thromboembolism were also observed in this case.This is a condition that is usually found in younger patients suffering from COVID-19.Four similar cases were, however, reported in elderly patients in a study conducted by Delorme et al.[11], suggesting that this disease could also affect different age groups.This study also reported that all the patients showed improved symptoms after immunotherapy, highlighting the fact that the neurological conditions caused by COVID-19 are treatable[11].
COVID-19 appears to have a link to neurological symptoms,according to our findings.However, the neurological manifestations in COVID-19 patients may easily be skipped from detection[12]since imaging of the brain and cerebrospinal fluid analysis were not commonly performed among COVID-19 patients, for neurological symptoms were unexpected.The current state of knowledge about COVID-19-related neuropathology is significantly restricted[13].Due to the under-reporting of neurologic manifestations in the context of pneumonia, conducting thorough neurological clinical tests becomes unlikely.Furthermore, even when there is a clinical suspicion of neurological involvement, COVID-19 patients are kept in strict isolation and have limited access to neuroimaging,thus limiting opportunities to monitor and investigate problems and ramifications[14].However, in order to further describe SARS-CoV-2 and its neuropathologic impacts, efforts must be taken to overcome these obstacles.Moreover, the sheer number of people who are afflicted with this critical illness is expected to exacerbate the burden of long-term cognitive impairment.Therefore, this study emphasizes that degenerative symptoms should be recognized early and treated effectively.
This article has some limitations, such as the inability to generalize, inability to prove a cause-and-effect link, danger of overinterpretation, retrospective design, and reader distraction when focusing on the uncommon.Furthermore, only five cases were discussed in this article and more cases should be included for a more comprehensive and accurate reporting of possible results.
The present report reveals a detailed radiological evaluation of the neurological impact of COVID-19 on patients.The discoveries highlighted in this report would help clinicians to detect neuropathological indications earlier, attempt therapeutic intervention before irreversible injury, and identify compelling neurobiological targets for more effective neurologic injury therapy and prevention.
Conflict of interest statement
The authors report no conflict of interest.
Funding
This study received no extramural funding.
Data availability statement
The data supporting the findings of this study are available from the corresponding authors upon request.
Authors’ contributions
Ayimen Khalid Khan wrote the first draft of the manuscript.All authors reviewed and edited the manuscript and approved the final version of the manuscript.
杂志排行
Journal of Acute Disease的其它文章
- Predictors of hemorrhagic manifestations in dengue: A prospective observational study from the Hadoti region of Rajasthan
- Clinical profile of medication-related emergencies among patients presenting to the emergency department: An observational study
- Risk factors for development of pneumothorax in patients with COVID-19 at a government health facility in North India: An exploratory case-control study
- Imipenem/cilastatin-induced acute eosinophilic pneumonia: A case report
- A public health perspective on dengue in Bangladesh in the twenty-first century
- COVID-19 mortality trends before and after the national vaccination program in Iran: A joinpoint regression analysis
