A systematic review of the factors significantly influencing the quality of life of living liver donors
2023-11-26YuexinShiHimingZhngZhijunZhu
Yuexin Shi ,Himing Zhng ,Zhijun Zhu ,*
a School of Nursing, Peking University, Beijing, China
b Liver Transplantation Center,National Clinical Research Center for Digestive Diseases,Clinical Center for Pediatric Liver Transplantation,Beijing Friendship Hospital, Capital Medical University, Beijing, China
Keywords:Living donors Liver transplantation Psychosocial functioning Quality of life Systematic review
ABSTRACT Objective: This systematic review aimed to synthesize the literature on factors influencing the quality of life in living liver donors post-donation and to provide a reference for developing targeted interventions in clinical practice.Methods: A systematic search guided by the PRISMA 2020 approach was performed on specific databases: PubMed,EMBASE,CINHAL with full text,Web of Science,and ProQuest Dissertations &Theses databases.Peer-reviewed articles published in English from inception to October 2022 covering crosssectional studies and longitudinal studies on factors affecting the quality of life of living liver donors after donation were included in this systematic review.The methodological quality of the studies was examined using a modified version of the National Institutes of Health Quality Assessment Tool.Results: A total of 6,576 studies were retrieved,and 16 eligible studies were finally included.Four types of independent influencing factors: sociodemographic (gender,donor age,education,ethnicity,and marital status),donation-related (length of hospital stay and number of hospitalizations/hospital visits related to donation surgery,recipient outcome,time from donation,complications,donation decision,ambivalence about donating,donor-recipient relationship),health-related (body mass index and predonation physical symptoms),and psychosocial (pre-donation physical and mental score,household income,anxiety,depression),were extracted from the included studies.Several studies consistently identified old age,recipient death,recent donation,postoperative complications experienced by donors,and donor concerns about their well-being as negative influencing factors on physical function.Female donors,low education levels,longer hospital stays,and/or more hospital visits due to donation,poor recipient outcome,recent donation,pre-donation concerns regarding their well-being,and first-degree relative and spouse/partner donors were reported in several studies as negative predictors for psychological status.Factors affecting social function were considered by only two included articles.Conclusions: The quality of life of living liver donors could be affected by both donation surgery and psychosocial factors.Based on the above-influencing factors,clinical nurses can develop targeted interventions to improve the quality of life of living liver donors.
What is known?
· Evidence has indicated that living liver donors have impaired psychological status and social function after recent donation;however,declined physical function may persist for longer postdonation.
· Complications and related medical outcomes among living liver donors have been systematically documented.
· A synthesis of the factors influencing the quality of life of living liver donors is still absent.
What is new?
· Four kinds of factors (sociodemographic,donation-related,health-related,and psychosocial characteristics) are related to changes in quality of life for living liver donors.These factors should be considered when screening donors before donation and formulating interventions.
· Social function has gained little attention when examining the quality of life of living liver donors,and few valid assessment tools exists to assess their social function.
1.Introduction
Global Transplant Observatory data reports that 34,047 liver transplants were completed in 2018 worldwide,and 19.2% were from living donors (http://www.transplant-observatory.org/).Living donor liver transplantation is the optimal treatment option for end-stage liver disease and mitigates the scarcity of deceased donor organs.Liver donors who underwent surgery donate part of their liver tissue,which might have degrees of impact on their health,such as post-operation pain,scar-shame,and psychosocial problems [1,2].For this reason,researchers have analyzed the procedure’s clinical outcomes and sought to comprehensively understand the quality of life (QoL) of liver donors [3,4].The World Health Organization defines QoL as individuals’perceptions of their position in life in the context of the culture and value systems in which they reside in relation to their goals,expectations,standards,and concerns [5].QoL is a multidimensional concept typically assessed as personal self-reported physical functioning,psychological state,social relationships,and environmental aspects [6,7].
Living liver donation does have an impact on the QoL of liver donors.Our previous meta-analysis found [2] that compared with pre-donation,obvious declined physical functioning was presented in liver donors for a considerably long time.Impaired social and psychological QoL affected donors for a shorter time after their donation.The recommendation from the International Liver Transplantation Society guideline suggested that long-term routine follow-up and necessary intervention are essential for living liver donors [8].
The QoL of living liver donors has been confirmed to be influenced by multiple factors.For example,published studies have reported that female sex [9-11],education level of less than a bachelor’s degree [12,13],experiencing complications [14],longer post-donation hospitalization [10,11,15],and recipient death[11-13,16] were predictors of poor physical-and mental-healthrelated QoL.Old age is a good and poor predictor of liver donors’physical and mental health[17].A comprehensive understanding of these positive and negative impacts on the QoL of living liver donors could be helpful to both clinical practitioners and donors.Specifically,it could be beneficial for clinicians and nurses to monitor donors with elevated risk factors and set targeted interventions for them.Donors with psychosocial factors should be treated as a vulnerable group needing increased attention and further assessment before and after donation.Data on positive and negative factors influencing QoL are critical for donor-informed consent and to ensure relevant psychological interventions are provided in advance.Several reviews have summarized the data on medical outcomes and the psychosocial status of living liver donors[18-20].However,a systematic review or synthesis of the evidence on predictors or factors influencing their QoL is still absent.In this systematic review,we synthesized the literature on predictors of QoL and factors influencing QoL in living liver donors to help clinical nurses identify vulnerable donors and take timely interventions to improve liver donors’ QoL.
2.Methods
This systematic review was presented according to the PRISMA 2020 approach.The protocol for this systematic review is available at PROSPERO (CRD42023464295).
2.1.Search strategy
Five databases:PubMed,Embase,CINHAL with full text,Web of Science,and ProQuest Dissertations &Theses were searched for studies published between database inception and October 2022.In addition,the references of included studies were searched manually.We used a combination of Medical Subject Headings(MeSH) or Emtree terms with the text words to retrieve database references.The specific search strategy using PubMed as an example is presented as follows:((((“Liver Transplantation”[Mesh])OR ((((“Liver Grafting”[Title/Abstract]) OR (“Liver Transplant*”[Title/Abstract])) OR (“Hepatic Transplant*"”[Title/Abstract])) OR (“Hepatic Grafting”[Title/Abstract]))) OR ((Transplant*[Title/Abstract]) AND ((liver[Title/Abstract]) OR (Hepatic[Title/Abstract])))) AND ((“Living Donors”[Mesh]) OR ((donor*[Title/Abstract]) OR (donation[Title/Abstract])))) AND ((“Quality of Life”[Mesh]) OR (((((((((((“Life Quality”[Title/Abstract]) OR (“Quality Of Life”[Title/Abstract])) OR (QoL[Title/Abstract])) OR (psychosocial[Title/Abstract])) OR (social[Title/Abstract])) OR (emotion[Title/Abstract]))OR(mental[Title/Abstract]))OR(well being[Title/Abstract])) OR (psychologic*[Title/Abstract])) OR (physical[Title/Abstract])) OR (environment[Title/Abstract]))).Minor changes in search strategy were required to adapt the search to the other databases (e.g.,keywords related to “quality of life” and “liver transplantation” were only used when searching the ProQuest Dissertations&Theses database and CINHAL because of the limited number of studies in these databases).Potential unpublished studies were retrieved from the System for Information on Grey Literature (SIGLE) database (http://opensigle.inist.fr/).
Eligibility of studies for inclusion was based on the following criteria:1)living liver donors must have been enrolled in the study after the donation;2) studies must have analyzed the factors affecting donor QoL using multivariate analysis;3)the self-reports of donor QoL was based on four domains as defined in our previous study [2]: physical functioning (physical activity,physical symptom,pain,and fatigue),psychological status(e.g.,feelings,worries,and tension),social relationships(social activity;relationships with relatives,friends,and others;and social support),and environment(physical safety and security,home environment,living condition,work satisfaction,financial resources,leisure activities,and physical environment);4) cross-sectional or longitudinal study design,and 5) peer-reviewed articles published in English.Articles were excluded if they were conference proceedings,abstracts only,commentaries,editorials,newsletters,or research protocols.
2.2.Selection of studies
First,the articles retrieved from the databases were imported into Endnote X9 Software,a reference management software program with which duplicates could be removed.Then,two authors(Y.Shi and H.Zhang) independently screened the titles of the remaining records for relevance to the review topic.Articles unrelated to the review topic were deleted directly.We reviewed the full text of articles that potentially met the inclusion criteria for further determination.Disagreements about selection were resolved through discussion with the third author (Z.Zhu).
2.3.Data evaluation
The methodological quality of each study was evaluated by two authors (Y.Shi and H.Zhang) independently,and all authors discussed discrepancies until a consensus was reached.A modified version of the National Institutes of Health (NIH) Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies was employed [21],which contains eight items with possible answers “yes,” “no,” “cannot determine,” “not applicable” or “not reported.” Six items (items 6,7,8,9,10,and 12) were removed because they were relevant to cohort studies.Adjustment for confounding was considered sufficient if studies adjusted for at least one sociodemographic variable(e.g.,age).The adequacy of the sample size was judged by whether it reached at least 15 times the number of independent variables.A quality percentage score was calculated for each study based on the number of “yes” responses divided by the total number of applicable questions and given the following quality ratings: poor (<60%),adequate/fair (60%-69%),good(70%-79%),and strong (≥80%) [22].
2.4.Data analysis
We synthesized the study results using a narrative approach.The description of each study’s characteristics (first author,publication year,country),sample size,donor-recipient type,donor age,surgical techniques,QoL assessment tool(s),data collection points,and complications were extracted and listed in Table 1.The statistically significant factors affecting any dimension of QoL (physical function,psychological status,social function,and environment)calculated using multivariate analysis were summarized and classified according to their attributes.Any discrepancies during data analysis were resolved through discussions among authors(Y.Shi,H.Zhang &Z.Zhu) to reach a consensus.

Table 1 The characteristics of the included studies (n=16).
3.Results
3.1.Search process
The systematic search yielded 6,576 records,of which 1,429 were screened as duplicates.A total of 5,081 records were excluded based on their titles and abstracts against the eligibility criteria.The full text of 66 articles was further assessed,and 50 were excluded.The excluded articles included 43 that only described the current QoL of liver donors without regression analysis,six that were unrelated to the QoL of liver donors,and an article that included liver donation candidates.Our systematic review finally had 16 papers[9-15,23-31] (Fig.1).
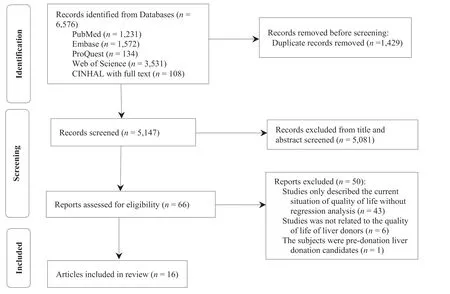
Fig.1.The PRISMA flow diagram for search strategy.
3.2.Characteristics of the included studies
The articles came from the following countries: USA (n=5),Japan(n=4),China(n=2),Canada(n=1),Poland(n=1),South Korea (n=1),Singapore (n=1),and Germany (n=1).The data from 3,783 living liver donors were analyzed finally.Most(n=12)of the included articles reported on the adoption of the 36-item Short-Form Health Survey (SF-36) to assess QoL.The other assessment instruments are summarized in Table 1.The overall rate of complications experienced by donors in the included studies ranged from 4.5%to 41.1%[9,13].Among them,the Clavien Grade I complication rate was reported to be 1.8%-20.2% [2,14],Grade II was 2.9%-25.4% [13,14],and Grade III or higher was 0.5%-7.2%[13,30] (Table 1).Meanwhile,Table 1 shows the methodological quality results for each study.The quality of three articles[12,26,28]was assessed as “poor” quality,and two articles [25,30] were evaluated as “fair” quality.
3.3.Factors influencing QoL of living liver donors
Various risk factors related to the QoL of living liver donors were identified across the studies.These risk factors were grouped into sociodemographic,donation-related,health-related,and psychosocial characteristics.
3.3.1.Sociodemographic characteristics
Female.One article[11]identified that being a female donor was associated with more physical symptoms (e.g.,pain and fatigue post-donation),and four articles [9,11,14,27] reported that female donors had a poor psychological status and more worries.
Donor age.Three articles [9,14,27] confirmed that older-aged donors had a poor physical function;however,inconsistency was found in the relationship between donor age and psychological status,with two studies separately reporting that older age of donors was associated with an increase in health-related worries[11]and poor mental state [9] in donors.Another two articles [17,27]showed that old age positively predicted better psychological status,whereas one article [30] found that younger donors had improved self-esteem.Regarding social function,one article [23]reported that older donor age was a positive factor for an improved relationship between donor and recipient.
Recipient’s age.One article found that child recipients were a negative factor for social function (e.g.,lack of understanding of donors’ health) [27].
Education.One[13]and three[12,13,24]articles identified that a low level of education (less than a bachelor’s degree) was an independent influencing factor for poor physical and psychological QoL,respectively.
Ethnicity and marital status.One article[13]found that Hispanic ethnicity was associated with poor physical function.Another article [11] reported that marriage before donation was associated with higher fatigue.
3.3.2.Donation-related characteristics
Length of hospital stay and number of hospitalizations/hospital visits related to donation surgery.Five articles [11,14,15,23,27] identified that longer hospital stays and an article[24]found that being hospitalized during the first month after donation,as well as more frequent hospital visits related to the donation were independent risk factors in living liver donors for all four domains of QoL.For example,the donors would experience more physical problems,such as pain and fatigue [11],more health-related worries and stress [11],more after-effects [27],significantly impaired mental health [15],poor social function [14],a greater burden of postdonation costs and decreased income due to the donation [23].
Recipient outcome(death/complication/severity of liver disease pre-donation).Two articles reported that recipient death was a factor associated with poor physical function in donors [13] and continuing physical symptoms (physically not “back to normal,”pain,and fatigue) [11].One article [31] indicated that donors who donated to a recipient with Clavien-Dindo grade III or IV complications were more likely to have higher role-physical scores in SF-36.Regarding psychological status,four articles indicated that the recipient’s death was a negative factor influencing the psychological level of the donor [12,13,27] and was likely to induce physical stress [11] in the donor.Regarding social function,one article indicated that donors whose recipients died had less potential to report being held in high esteem by the recipient’s family or receiving gratitude from them [23] and had low satisfaction with liver donation [27].
Time from donation.Recent donation was determined as a negative predictor for all three QoL domains.Five articles[11-13,25,29] identified that recent donation was a negative predictor of physical QoL of living liver donors,especially within six months post-donation [11,13],during which time living liver donors were likely to have lower levels of vitality and more physical problems (unable to perform some physical activities,slower than expected recovery,higher levels of abdominal/back pain,and more fatigue).Regarding psychological status,three articles [11,23,25]reported that recent donation was associated with lower mental component summary score and more worries (about their recipient).In addition,one article[23]reported that recent donors(three months and six months post-donation) bore a higher financial burden (decreased income,burdensome medical expenses,job change,or modification due to donation).
Post-donation complications.Two articles [11,14] reported that postoperative complications experienced by donors were a risk factor for poor physical function and induced high abdominal and back pain levels.One article[14]found that living liver donors with two or more complications were more likely to have poor mental and socially related QoL.Donors with no postoperative complication likely had better physical function and higher satisfaction,supported by two articles [12,30].
Donation decision.One article [14] found that donors encouraged by someone to donate were more likely to report improved family relationships,and another article [11] showed that donors who were discouraged from donating by someone were likely to have more physical symptoms.
Concern for own well-being.Concerns by living liver donors about their pre-donation was a negative predictor for their physical[10,13] and psychological [10,24,25] QoL.
Ambivalence about donating.Two articles [11,23] reported that living liver donors with high ambivalence about donating were more likely to worry about their recipients and their health.One article[23]found that donors with low levels of ambivalence about donation experienced a greater decrease in income due to donation.
Donor-recipient relationship.Two articles [11,23] reported that first-degree relative donors and spouse/partner donors were more likely to report donation as being physically stressful and were more worried about their recipients.In contrast,one article [23]indicated that donors donating to first-degree relatives or a spouse/partner were more likely to report being held in high esteem and expressing gratitude by their families.
Other factors.Other independent influencing factors for poor physical function of donors included having a male child recipient[29],use of analgesics associated with postoperative pain [26],taking more days off work for reasons related to donation [14],anticipation that life would be more worthwhile after donation[11],and anticipation of long-term health effects [11].Other negative influencing factors for social function included the number of months until recovery to preoperative health status [14];preoperative prediction of a long time off work (>three months)[23];concern about missing work [23];working in a technical,clerical,or lower-level position [23];and having pre-donation concern about who would pay donation costs [23].
3.3.3.Health-related characteristics
Body mass index.One article[11]reported that donors with high body mass index (BMI) (25.0-29.9 kg/m2) were more likely to report being unable to do some physical activities after donation,and another article[23]found that donors with BMI <30 had more worries about their recipients.
Pre-donation physical symptoms.One article [11] found that donors with abdominal/back pain or fatigue before donation were more likely to experience the same symptoms post-donation.
3.3.4.Psychosocial characteristics
Pre-donation physical component summary score and mental component summary score.Two articles [11,12] identified that high physical component summary and/or mental component summaryscores pre-donation were a positive factor for donors having fewer physical symptoms,lower levels of abdominal or back pain and better mental health post-donation.One article [11] found that lower pre-donation mental component summary score was independently associated with physical and mental issues in donors,such as health-related worries,not feeling physically back to normal,and feeling physically stressed.
Household income.One article [11] identified that higher household income was a negative factor for postoperative recovery but a positive factor for abdominal/back pain,and another one[23]reported that donors with lower household income were more likely to report post-donation costs as a burden.
Trait anxiety.One article [26] indicated that trait anxiety was associated with significant postoperative pain;another article[24]reported that past or present psychiatric diagnosis was a negative predictor of the psychological function of living liver donors.
A study from Noma et al.[28] that did not classify QoL into different domains,and the results showed that recipient age at the onset of hepatic disease was positively associated with the mean health-related QoL of donors,whereas a high depression score of recipients (Beck Depression Inventory) was negatively related to mean QoL score.
4.Discussion
This systematic review summarized the factors significantly influencing the QoL of living liver donors.Sixteen articles from eight countries were included.Although the included studies and previous syntheses of the evidence reported that the overall QoL of living liver donors is good [13,29,32],they were still affected by invasive surgery and post-donation complications,and aspects of QoL were indeed impaired among the donors in our review.We extracted four kinds of factors influencing QoL:sociodemographic,donation-related,health-related,and psychosocial.
Some negative factors could be modified,and others could not.Being female [9,11,27],low education levels [12,13,24],old age[24,27,30],recent donation [11,13,25,29],recipient death[11-13,27],and being a first-degree relative or spouse/partner donor [11,23] were consistently determined by several articles as factors negatively influencing donor physical function or psychological status.Donors with risk factors that are difficult to modify through intervention could be identified as vulnerable (e.g.,females,low education levels).Strict screening of physical and mental aspects of functioning is essential,with closer attention paid to vulnerable groups before and after donation.The transplant team can also give additional attention to living liver donors at vulnerable times,such as after a recent donation(especially within six months post-donation) and donors who have recently experienced recipient death [11,27,31].
Postoperative complications experienced by donors[11,14],predonation physical or psychological status(e.g.,physical component summary score/mental component summary score,concerns regarding their well-being) [10,24,25] were screened to affect different aspects of the QoL of donors.The overall rate of complications experienced by donors in the included studies ranged from 4.5% to 41.1% [9,13].It can be seen that invasive surgery is not beneficial for healthy organ donors.Living organ donation has been controversial because it contradicts the principle of “non-invasive medical ethics” [33].However,living donor transplantation is considered an ethically acceptable undertaking to save another’s life.Protecting living donor’s safety is paramount to any living organ transplant program.Weng et al.[34] explored a web-based self-care instruction for reducing symptom distress and improving the QoL of living liver donors.Although the effectiveness of this intervention on symptoms of distress and QoL in liver donors is currently unclear,it is a meaningful attempt.A previous study[35]using guided and tailored internet-based cognitive-behavioral intervention provided to living kidney donors with impaired mental-related QoL before and after donation had preliminary results indicating that the donors felt their problems had improved.We think that a nurse-led,web-based psychosocial assessment and intervention pre-donation and at different stages post-donation could effectively protect the physical and mental health of living liver donors.
Social function is an essential QoL domain,but it has received little attention in the study of QoL of living liver donors.This may result from a lack of effective tools to assess social function.Only two studies included in our review focused on factors influencing social QoL.A study from Japan reported social components score by combining role-physical,role-emotional,and social-functioning subscales score of SF-36 [14].Another study used self-developed assessment questionnaires to assess social and environmentalrelated QoL [23].Both of these studies mainly concerned the family relationships and financial issues.Unexpected post-donation problems,such as the living liver donor requiring more recovery or experiencing complications,a long hospital stay,or frequent hospitalizations,may worsen socially related QoL.They may also cause donation-related financial strain (e.g.,burdensome postdonation costs and loss of income).Donation-related physical function,psychological status,and social function could be mutually affected.Poor social function may influence the physical and psychological aspects of QoL because medical treatment postdonation may be restricted due to impaired social roles,decreased income,and the burden of donation-related medical expenses [23,32].Donors’ social and environmental-related QoL should be treated equally as important as other aspects.A specific social function assessment tool should be developed for use with living donors in future studies.
This systematic review had some limitations.First,a limited number of studies could be included,and many were of small sample size,which limited the strength of evidence.Second,most studies adopted cross-sectional designs,so causality in the relationships between potential risk factors and QoL could not be established.Consequently,the influencing factors summarized in this review reflect associations rather than causations.Third,in most studies,the SF-36 was used to assess QoL.Although the SF-36 is widely recognized as an effective QoL measurement tool,it is not targeted at living liver donors.Only one of the included studies used a donor-specific QoL assessment tool.Finally,we could not merge data in a meta-analysis because of the limited statistics the included studies provided;hence,this is merely a systematic review that provides a narrative summary of the existing evidence.
5.Conclusion
Currently,there is a serious shortage of transplant organs worldwide,and as a result,living donor liver transplantation is already prevalent in many countries.Therefore,growing international consensus suggested that the long-term impact of living liver donation demands greater attention in both research and clinical arenas[8,36].We summarized potential negative factors that could provide convenient information for nurses and clinicians to develop targeted donor interventions.Candidates for liver donation must be informed of all possible outcomes after donation.Donors with risk factors and donors at time points of heightened vulnerability deserve increased attention,and by identifying these,specific interventions can be carried out for modifiable risk factors to minimize possible negative effects.Social function is also an important element in the QoL of donors and requires greater attention from nurses and clinicians.
On the one hand,the development of a valid assessment tool is necessary for measuring donation-related outcomes.On the other hand,helping donors to activate their social support system,not only their healthcare team but also their family,friends,and even other donors,may benefit donors in dealing with potential risks and issues.If we are to obtain informed consent from donors ethically and responsibly and develop appropriate post-donation clinical surveillance plans,conducting short and long-term cohort studies could help with knowing the impact of living liver donation on donors’ health.Multicenter,prospective,and longitudinal studies are welcomed in future study designs to confirm causality between potential factors and the QoL of living liver donors.
Funding
This work was supported by National Natural Science Foundation of China (grant number 71974008).The funding organization did not have any roles in the survey’s design,implementation,and analysis.
CRediT authorship contribution statement
Yuexian Shi:Conceptualization,Methodology,Data curation,Writing-original draft,Funding acquisition.Haiming Zhang:Data curation,Software.Zhijun Zhu:Conceptualization,Writing -review&editing.
Declaration of competing interest
The authors have declared no conflict of interest.
Data availability statement
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
Acknowledgments
None.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2023.09.012.
杂志排行
International Journal of Nursing Sciences的其它文章
- The associations among nurse work engagement,job satisfaction,quality of care,and intent to leave: A national survey in the United States
- 《国际护理科学(英文)》2024年征稿
- Meaning of community activity participation for older adults in couple households
- The implementation and impacts of national standards forcomprehensive care in acute care hospitals: An integrative review
- Nurse-coordinated home-based cardiac rehabilitation for patients with heart failure: A scoping review
- Effectiveness of a family-based program for post-stroke patients and families: A cluster randomized controlled trial
