Effectiveness of fit testing versus fit checking for healthcare workers respiratory protective equipment: A systematic review
2023-11-26CharlotteGokoElizabethForsterMatthewMasonPetaAnneZimmerman
Charlotte Goko ,Elizabeth Forster ,Matthew Mason ,Peta-Anne Zimmerman ,c,e
a School of Nursing & Midwifery, Griffith University, Australia
b Menzies Health Institute Queensland, Griffith University, Australia
c Collaborative for the Advancement of Infection Prevention and Control, Australia
d University of the Sunshine Coast, Queensland, Australia
e Infection Control Department, Gold Coast Hospital and Health Services, Australia
Keywords:Fit-testing Fit-checking Healthcare personnel Respiratory protective devices Personal protective equipment User seal check
ABSTRACT Objective: Respiratory protection is critical in healthcare to minimise the risk of airborne infections for healthcare workers (HCWs).It emphasizes the use of proper fitting of particulate filter respirators and equivalent respiratory protective equipment (RPE) to ensure a good facial seal.The systematic review aimed to compare the effectiveness of fit testing and fit checking for HCWs’ respiratory protective equipment.Methods: A systematic review of the literature exploring RPE for HCWs to determine the effectiveness of fit-testing versus fit-checking from January 2003 to April 2022 was identified using CINAHL Complete via EBSCO Host,Cochrane Library,EMBASE,PubMed,and MEDLINE via Ovid electronic databases,and grey literature.The study protocol was registered with PROSPERO (registration number: CRD42020213968).Results: Of the 561 articles identified in the search,25 articles (22 quantitative studies and three guidelines) were included in this review.Overall,these studies suggest fit-testing as a method that is more effective,widely adopted,and reliable in assessing the effectiveness of RPE;however,a respiratory program should include both fit-testing and fit-checking to maximise effectiveness of the RPE.The COVID-19 epidemic highlighted a lack of knowledge among HCWs regarding fit-checking and fit-testing,and relevant education increased the effectiveness of respiratory equipment protection.Conclusion: It is imperative that both fit-testing and fit-checking is implemented in order to ensure HCW safety.It is recommended to integrate education,fit-testing and fit-checking into a comprehensive respiratory protective program run by trained fit-testers.There is also a need for practical testing methods that incorporate the clinical environment.
What is known?
· Healthcare workers (HCWs) are vulnerable to transmission of airborne pathogens;respiratory protective equipment is essential to provide HCW respiratory protection by use of a respirator,the most common being N95/P2 filtering facepiece respirators(FFRs) and powered air-purifying respirators.
· N95/P2 or FFRs are intended to attain a close facial fit and effective filtration of airborne particles.All HCWs required to wear a N95/P2 respirator need to be educated on the significance of fit-checking and to know how to fit-check.
· Annual fit-testing is recommended to comply with US s501025010 OSHA requirements and Australian and New Zealand Standard (AS/NZS) 1715:2009.
What is new?
· Fit-testing is the more effective,most widely adopted and reliable method of assessing the effectiveness of respiratory protective equipment (RPE);however,fit-testing and fit-checking maximises the effectiveness of the RPE.There is also a need for testing methods that incorporate the environment in which the equipment will be used.
· Additionally,participation and education of HCWs in the selectionand effectiveness tests of the protective equipment will increase the efficacy of protection and testing methods.Hospitals and policymakers are recommended to integrate education,fit-testing and fit-checking into a comprehensive respiratory protective program run by trained fit-testers.
1.Introduction
Healthcare associated infection(HAI)is a major concern within any hospital or healthcare setting.Healthcare workers(HCWs)are at risk of exposure to HAI[1].The protection of HCWs from airborne diseases and infections is a priority within the healthcare system as it reduces the risk of HAI.The importance of monitoring and limiting airborne transmissible diseases has greatly increased more recently with emerging respiratory infectious diseases,including COVID-19 caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) [1,2].The COVID-19 pandemic has revealed deficiencies in global and Australian healthcare systems in the protection of HCWs from transmission of SARS-CoV-2 and other respiratory viruses [3].For example,the supply of appropriate personal protective equipment (PPE) as well as testing and checking of PPE was delayed or insufficient [3].A primary step in infection prevention and control is ensuring the effectiveness of respiratory protective equipment.This will help in preventing or limiting transmission of airborne pathogens.N95/P2 particulate respirators filter at least 95% of airborne particles,with the protection provided dependent on the filter’s efficiency and seal quality[4].This is done through testing methods of varying efficacy.Two key methods utilised within the healthcare industry will be explored within this review: fit-testing and fit-checking/user seal testing.Fit-testing determines the brand,model,and size of the respirator that achieves an adequate seal on an individual’s face.There are two methods of fit-testing,which are quantitative and qualitative fit-testing.
The COVID-19 pandemic highlighted significant deficiencies in global healthcare systems in the protection of HCWs from transmission of COVID-19 and other respiratory pathogens [3].Transmission of SARS-CoV-2 in healthcare settings has been a major issue throughout the COVID-19 pandemic worldwide,especially during the first waves in 2020[5].In Australia,for example,during the first wave in the state of Victoria,22% of HCWs who tested positive for SARS-CoV-2,the virus that causes COVID-19,reportedly acquired the virus through workplace transmission [6].However,this increased to at least 69%during the second wave,highlighting the urgent need for better protection for front-line HCWs [3].The prevalence of infection among HCWs worldwide varied from 0.3%to 43.3% [5].The COVID-19 pandemic is also responsible for significant loss of life among HCWs,with the WHO estimating 80,000 to 180,000 HCW deaths globally,and these figures may be underreported [5].Among hospitalized patients with confirmed COVID-19,up to 41% were infected in healthcare settings,according to different studies [5].As new strains of COVID-19 emerge and are identified,HCWs will continue to be faced with the need for continued respiratory protection.Due to the risk of infection and mortality for HCWs and patients,determining the effectiveness of fit testing versus checking is urgently needed.
Qualitative fit-testing is influenced by the wearer;it uses a test agent such as saccharin or Bitrex (a bitter tasting substance).This agent enables the user to sense the presence of the test agent within the respirator by taste,smell,or the urge to cough if the fit of the respiratory protective equipment (RPE) is not adequate [6].Quantitative fit-testing requires the use of specialized particle counting equipment (such as PortaCount™Plus machine) to provide numerical measurements called fit factor.The PortaCount™Plus machines work by measuring the concentration of microscopic dust particles in the ambient air and then measuring the concentration of those dust particles that leak into the respirator.The ratio of these two concentrations is called the fit factor[6,7].A fit factor value of 100 or greater is the criterion for achieving a pass for a disposable N95/P2 respirator [8].The more reliable method of measuring effectiveness would be one that is quantitative,as it removes the wearer’s individual influence [9].See Table 1 for a summary of the procedures involved in these methods.

Table 1 Fit testing and fit checking procedures.
Regardless of the method used to determine fit-testing,user seal checking is required to be performed by the individuals each time a respirator is used.Fit-checking or user seal checking is a process conducted to ensure that the RPE creates a facial seal to minimise the number of particles that bypass the filter through gaps between the wearer’s skin and the respirator seal and is performed each time it is used [2].
This systematic review aimed to answer the research question:Effectiveness of fit-testing versus fit-checking for HCW respiratory protective equipment.The protocol for this review is registered in PROSPERO under the registration number CRD42020213968,available at https://www.crd.york.ac.uk/prospero/.
2.Methods
A systematic review to identify research exploring RPE for HCWs was undertaken to determine the reported effectiveness of fit-testing versus fit-checking.This review was guided by an integrated approach in accordance with the JBI methodology for mixed methods systematic reviews using JBI SUMARI [10].This involved assembling the qualitised data from quantitative studies with the qualitative data.Assembled data was categorised and pooled together based on similarity in meaning to produce a set of integrated findings.Reporting of this systematic review complied with Preferred Reporting Items for Systematic Reviews and Metaanalysis (PRISMA) guidelines [11].The records of screened articles were recorded in a PRISMA flowchart in Fig.1.The Mixed Methods Appraisal Tool(MMAT)was used to assess the relevance and results of the included studies.The MMAT was used to screen articles based on several screening questions that helped identify the quality and clarity of the articles based on the analysis that was conducted [12].
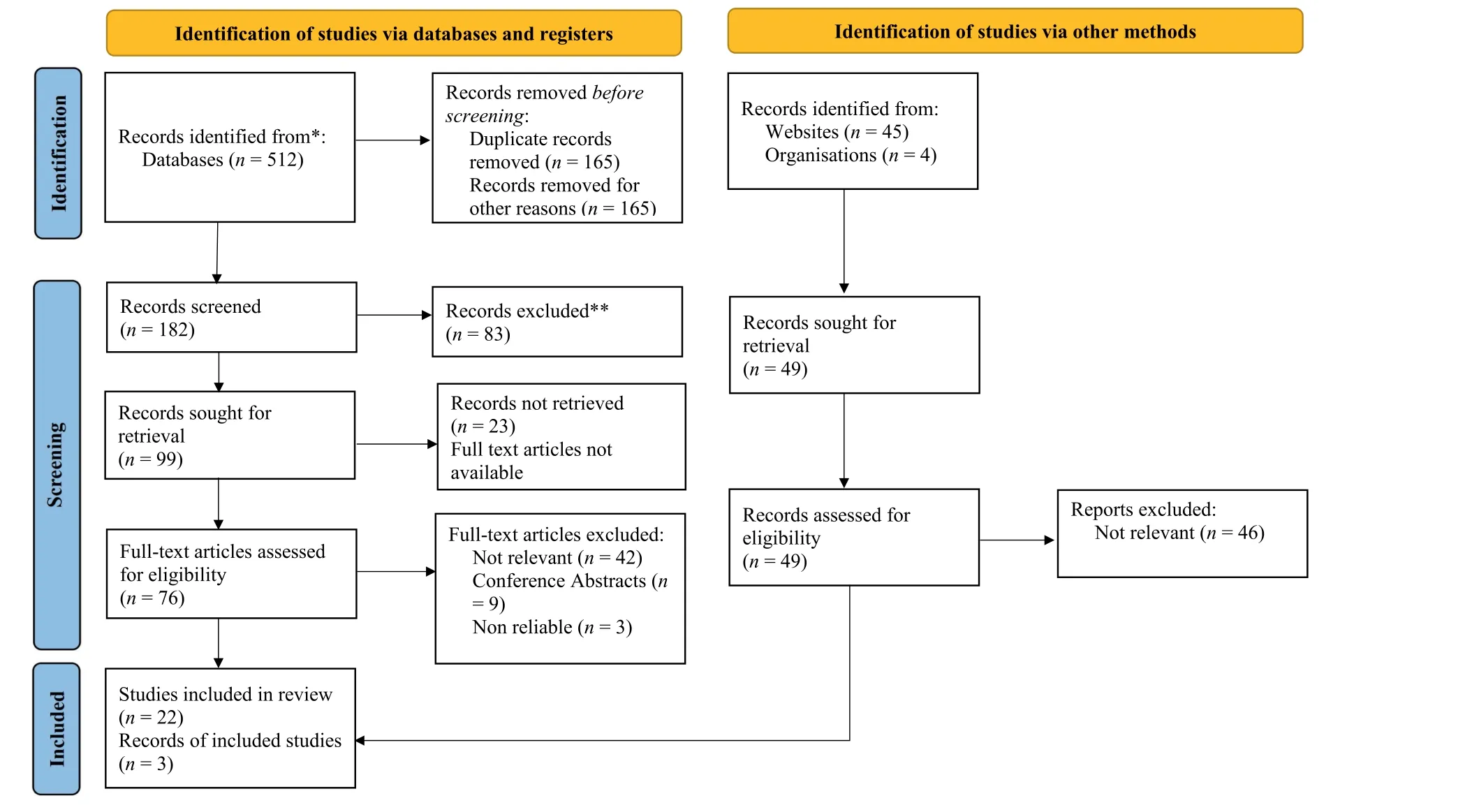
Fig.1.Flow diagram of the systematic review process.
2.1.Data collection
A comprehensive and systematic search of 5 databases,including CINAHL Complete via EBSCO Host,Cochrane Library,EMBASE,PubMed,and MEDLINE via Ovid,was conducted.A search of grey literature,including international guidelines and standards relevant to respiratory protection,was also undertaken.A health research librarian was consulted to develop the search strategy in the initial stages.The reference lists of identified studies and grey literature were screened,and citation tracking was also performed to identify further literature.The search was limited to studies available in English from 2003 to April 2022 in order to capture previous literature related to respiratory pandemics,such as severe acute respiratory syndrome (SARS),Middle East respiratory syndrome(MERS),and the COVID-19 pandemic.
The search strategy included various combinations of Medical Subject Headings(MeSH)terms and keywords identified in the first search.These included but were not limited to Fit test*,Mask*,Respirator*,User seal check* and health profession/doctor/nurse/clinician,allied health,or hospital.These articles were thenexported to Endnote version 20.2.1.15749 and further screened using the inclusion and exclusion criteria.Inclusion criteria sought studies from any geographical location published in English between January 2003 and April 2022.A range of study types(quantitative,qualitative,and mixed methods,and grey literature)that examined health care worker fit-checking and fit-testing of N95/P2 respiratory protective equipment were included.Studies focusing on non-healthcare worker occupational groups (mining,building,and construction) and conference abstracts,reviews,editorials,commentaries,or policy statements were excluded.
2.2.Study selection
Two reviewers(CG and PZ)independently screened the title and abstracts of studies against inclusion and exclusion criteria;discrepancies were resolved by a third reviewer (MM).Studies for inclusion were critically appraised using the MMAT,and suitable studies were collated in a data extraction table.Data to be extracted included type of study,participants,location of study,aims and objectives,study design and methods,and findings.
2.3.Data analysis
A data extraction table was developed for extracting data for the review.All data items extracted were cross-checked by PZ to ensure relevant articles are included.Due to the heterogeneity of the included studies,the findings are presented as a narrative synthesis[13].
3.Results
The database search of articles from January 2003 to April 2022 returned 512 articles;49 additional records were identified through other sources.Of the database search,76 articles remained as full text review following a review of the titles and abstracts and the exclusion of duplicates.After screening the 76 articles against the study’s inclusion and exclusion criteria,54 articles were excluded.Of the 49 other records,three met the criteria and were included in the review.As indicated in the PRISMA diagram(Figs.1),22 articles from the database search and three documents(guidelines) from other searches met the inclusion criteria and were included in the final systematic review.
Of the 22 quantitative studies [1,3,4,8,14-31] identified in Table 2,five were from Korea,six from China,five from Australia,and six from the United States.Seven of the studies reviewed on the effectiveness of facial seals were quantitative studies.Chan et al.[8]was the only observational study conducted within a hospital setting;all other studies were conducted in a simulation environment.The MMAT was used to appraise the methodological quality of the included quantitative studies in this systematic review.The 22 quantitative studies met the criteria;however,some of the chosen methodologies impacted the quality of the study.Three geographical documents (guidelines) [2,6,32] are listed in Table 3.

Table 2 Summary of studies included in the review.

Table 3 Grey literature.
In this review,three main themes emerged;‘Methods to determine facial seal’which focused on the effectiveness of fit testing and fit checking;‘effectiveness of healthcare worker training’ focused on how effective education/training is to achieving a good facial seal,and ‘contextual nature of determining a seal’ which explored the validity of facial seal assessment based on the context that evaluation occurred.
3.1.Methods to determine facial seal
A predominant focus within the included literature was facial seal effectiveness,particularly the methods used to determine how effective facial seals are both in normal fit-testing/checking sessions and in simulated work activities.The two assessments mentioned within the included studies were fit-testing and fitchecking,and the procedures for these tests are outlined earlier in the paper in Table 1.
Six studies in this review looked at the effectiveness of fittesting [2,8,14-17].Fit-testing is identified as an important element of respiratory protection programs to ensure the wearer is issued a respirator that is the correct size,provides a good facial seal and gives an adequate level of protection [8,18].Fit-testing also provides an educational opportunity for the user to improve respirator seal [8].
Excluding fit-testing and relying strictly on a user fit-check is disputed by Danyluk et al.[14] due to this method incorrectly indicating a proper fit on several occasions or incorrectly indicating a properly fitting respirator as defined by a fit-test.In a study by Derrick et al.[19] the user felt that the respirator fitted when the observed fit factor was very low.Fit-checking is inadequate for detecting gross leakage in donning N95/P2 respirators;therefore,fit-checking is not an appropriate surrogate for respirator fit-testing[14,19,20].Fit-testing is recommended to be used to determine the fit of N95/P2 respirators,and a user seal check must be done in a well-defined respiratory program including fit-checking [14,20].Lam et al.[20]recommended that quantitative fit-testing be used to determine the fit of N95 respirators.
3.2.Effectiveness of healthcare worker training
The effectiveness of fit-testing and fit-checking is dependent upon the reliability and quality of the measures used.The COVID-19 pandemic highlighted a lack of knowledge among HCWs regarding fit-checking and fit-testing,and this led to HCWs undergoing education regarding respiratory protection,fit-testing,and proper fitchecking principles,which increased the effectiveness of respiratory equipment protection[3].Training healthcare providers in respiratory protection could significantly improve the fit factor and adequate protection rate [1].Furthermore,proper protection performance of the respirator during fit-testing was improved after training [1].Or,Chung &Wong [21] study supports the role of ongoing education in fit-checking.Chan et al.[8] recommend hospitals and policymakers integrate education,fit-testing,and fitchecking into a comprehensive respiratory protective program.
3.3.Contextual nature of determining a seal
The contextual nature of fit-testing/checking poses some challenges to the effectiveness of fit-tests.Fit-testing is generally not being tested in hospitals and other actual practice conditions where there is also a high risk of airborne disease transmission[1,15,16,17,20,24,22,23).This lack of contextual testing means that although N95/P2 respirators passed the fit-test,in high-risk situations,such as during cardiopulmonary resuscitation where wearers are performing chest compressions,there is no guaranteed protection against respiratory infections [27].To tackle this issue,a new fittest,personal respirator sampling test (PRST),has been proposed,which can be undertaken whilst the wearer performs clinical activities,and the detection of face seal leakage can be monitored[21].If implemented,the PRST can help wearers evaluate the actual performance of their respirators during HCW activities in the clinical setting [21].The use of PRST is supported by Hauge et al.[25]and Viscusi et al.[26],who suggest that an initial fit-test during a simulated task could be a better way of ensuring the effectiveness of fit-tests.
4.Discussion
This study identified the effectiveness of fit-testing compared to fit-checking for HCW RPE.The findings in studies from Australia,China,Korea,and USA produced three themes: 1) methods to determine facial seal,2)effectiveness of healthcare worker training,and 3) contextual nature of determining a seal.The COVID-19 pandemic highlighted the need for the education of HCWs regarding fit-testing and proper fit-checking protocols,which subsequently allowed for the increased effectiveness of respiratory equipment protection [3].
Seven studies from various Australian tests reviewed the effectiveness of fit-testing and collected quantitative data that showed the importance and effectiveness of fit-testing when either paired with fit-checking or as a stand-alone method.Additionally,education on fit-testing plays a crucial role in increasing the effectiveness of HCW protection,especially in China [3,8].However,overall,these studies lack an assessment of the retention rates of education over time [8].Further repeat studies with fit-testing education integrated with a respiratory protection program would be highly beneficial to hospitals and policy makers [8].
Another point from Korea discussed the importance of the type of RPE chosen that ensures adequate protection [27].During the education component of the study by Myong et al.[27],there is a strong emphasis on educating HCWs on the type of RPE and the type of protection each affords after conducting a fit-test.This reoccurring theme suggests the importance of the type of RPE that is explored by various professionals and academics,such as in the study of Korea Lee et al.[22],that the type of respirator can influence the protective performance of healthcare providers.Furthermore,simulation studies from Korea by Kim et al.[1]revealed that training HCWs in a respiratory protection program may significantly improve the fit factor and adequate protection rate of the three types of respirators.To further establish this,the introduction of fit training,whereby HCWs are initially given training on fit-checking and fit-testing at the time of employment,then refreshed annually as per the Australian Standard (AS/NZS 1715:2009) or during a global pandemic.This would be beneficial to the safety of HCWs by ensuring that a chosen respirator will provide a good facial seal,as indicated by studies from Korea and Australia[1,3,28].
The contextual nature whereby fit-testing occurs also poses some challenges to the effectiveness of fit-tests.In China,fit-testing is not being tested in high activity roles where there is also a high risk of airborne disease transmission [29].This lack of contextual testing,as shown from Korea in the table above,means that although certain types of respirators,such as the N95/P2,passed the fit-test,in high-risk situations,such as during chest compressions,this did not guarantee protection against respiratory infections [24].To address this problem,a new fit-test (PRST) has been proposed that can be undertaken whilst the wearer performs clinical activities and where the detection of face seal leakage can be monitored.Multiple studies from Australia demonstrated that the use of an initial fit-test during a simulated task could be a better way in ensuring their effectiveness of fit-tests [20,30].This idea of multi-phase tests,especially in the USA,is supported by Viscusi et al.[26],who suggest there are benefits to performing a user seal check on some models for HCWs who have previously passed a fittest for those same respirator models.
Upon further analysis of fit-testing and fit-checking policies,Chughtai et al.[33] do raise a concerning issue that despite Australian guidelines outlining fit-checking policies,at the ground level,these guidelines are not necessarily translating into practice.Chughtai et al.[33] conducted a study using twenty healthcare workers in which most participants were not aware of the hospital respiratory protection policies.Furthermore,participants reported that they had not received any training nor had they participated in a fit-test prior to the study [24].It was found that this was secondary to the limited role that HCWs play in the selection of respirators.Consequently,supporting the idea that for the effectiveness of any of the methods of testing to increase,the context in which the tests are conducted is highly important.By using practicing HCWs to test and select the respiratory protective equipment,it allows for educational opportunities that benefit the hospital and the HCW simultaneously[24].Hospitals must not only implement but also educate their HCWs on these policies and conduct fit-tests that allow HCWs to be involved in decision making regarding what protective equipment should be supplied[6,31,32].
It can be argued that in USA and Korea if hospitals are to conduct fit-tests to help determine the type of respiratory equipment to use,then a better model would be to implement facial seal checks in various hospital settings to complement fit-testing and ensure good facial seal is achieved each time a respirator is worn[14,27,34].This then allows for the effectiveness of the tests to be quantified in a context in which the participants would ultimately be using the equipment.This would not only ensure that HCWs could be assured regarding the quality or facial seal effectiveness of respiratory protection used but also be confident in the effectiveness.
4.1.Limitations
The search was limited to only studies available in English;this may have led to selection bias due to the inclusion of only a subset of papers creating an incomplete data set.The Cochrane Handbook acknowledges the risk of bias in otherwise high-quality reviews when non-English studies are not included [34].Furthermore,some studies had small sample sizes,which may limit the power and generalisability of the study findings.Some studies also used a single model of respirator to contact fit-testing due to shortages of respirators during the COVID-19 pandemic.Whilst the discussion tried to compare fit testing and fit checking it’s difficult to separate the two processes as they are all important processes to ensure safety and protection from infections,that in itself became a limitation to this study.
4.2.Recommendations and implications for practice
A respiratory protection program is vital and should include staff education and training in fit-testing and fit-checking to ensure a good seal is achieved in order to reduce HCWs’ risk of exposure.For the ongoing safety of HCWs,fit-testing,fit-checking,and education can be completed during staff induction and annually as per the Australian standard (AS/NZS 1715:2009) or/and during global pandemics.Future repeat studies incorporating education as a part of fit-testing integrated with a Respiratory Protection Program(RPP) are needed to assess retention rates of education over time.The two processes cannot be separated as they are components of the respiratory protection program.
5.Conclusion
Fit-testing is identified as an important element of RPE to ensure the wearer uses a correct size respirator that provides a good facial seal and gives an adequate level of protection.Moreso,fit checking is recommended at the point of use;therefore,used together,fit testing and fit checking maximise the effectiveness of the RPE.Multiple studies in Australia,USA,Korea,and China using various quantitative and qualitative methods highlighted that fit-testing and fit-checking education and training for HCWs improves the effectiveness of respirators.Achieving good facial seal improves the fit factor.There is also a need for testing methods that incorporate the environment in which the equipment will be used.The two are not the same yet they are part of the respiratory program to achieve an effective facial seal.Comparatively,fit checking is done each time a respirator is worn whilst fit testing is done at least once per annum.Additionally,participation and education of HCWs in the selection and effectiveness tests of the protective equipment will increase the effectiveness of protection and testing methods.Hospitals and policymakers are recommended to integrate education,fit-testing,and fit-checking into a comprehensive respiratory protective program run by trained fit-testers.
Ethical consideration
This review used data from published studies therefore ethics approval was not required or sought.
Funding
Nothing to declare.
Data availability statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
CRediT authorship contribution statement
Charlotte Goko:Conceptualization,Methodology,Validation,Formal analysis,Investigation,Data curation,Writing -original draft,Writing-review&editing,Project administration.Elizabeth Forster:Conceptualization,Methodology,Validation,Formal analysis,Investigation,Resources,Data curation,Writing -review &editing,Supervision,Project administration.Matthew Mason:Conceptualization,Methodology,Validation,Formal analysis,Investigation,Resources,Writing -review &editing,Supervision.Peta-Anne Zimmerman:Conceptualization,Methodology,Validation,Formal analysis,Investigation,Resources,Data curation,Writing -review&editing,Supervision,Project administration.
Declaration of competing interest
We have no conflicts of interest to disclose.
Acknowledgement
We would like to acknowledge the Griffith University librarians for their expertise and assistance during data collection of this research.
Appendix A.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2023.09.011.
杂志排行
International Journal of Nursing Sciences的其它文章
- The associations among nurse work engagement,job satisfaction,quality of care,and intent to leave: A national survey in the United States
- 《国际护理科学(英文)》2024年征稿
- Meaning of community activity participation for older adults in couple households
- The implementation and impacts of national standards forcomprehensive care in acute care hospitals: An integrative review
- Nurse-coordinated home-based cardiac rehabilitation for patients with heart failure: A scoping review
- Effectiveness of a family-based program for post-stroke patients and families: A cluster randomized controlled trial
