Brucellosis, a diagnostic dilemma, presenting atypically in a child with terminal ileitis: A case report
2023-11-18KokilaBanerieeAmitavaPahariSubhenduROy
Kokila Baneriee, Amitava Pahari, Subhendu ROy
Abstract BACKGROUND Brucellosis is endemic in India with seropositivity rates as high as 10% in children in the eastern states, yet the disease is not on the radar when a differential diagnosis of pyrexia of unknown origin (PUO) is being considered, especially in children in urban set-up.This may be because of the non-specific multitude of systemic symptoms seen in this disease and the lack of awareness among clinicians.
Key Words: Pyrexia of unknown origin; Terminal ileitis; Brucellosis; Case report
INTRODUCTION
Diagnosing pyrexia of unknown origin (PUO) almost always poses serious challenges.Infections in developing countries,like India[1], and non-infectious inflammatory diseases in developed countries are the major causes[2].Globally, 7%-53%of PUO cases go undiagnosed despite thorough workup and advancements in diagnostic techniques[3].The initial diagnostic investigation protocol for PUO should at the very least be a thorough history taking and repeated physical examination, complete blood count with differential cell count, electrolytes, renal and liver function tests, protein electrophoresis, C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), urine culture, chest X-ray, abdominal ultrasonography, and a tuberculin skin test[4-6].The case described here is of a child with PUO that proved to be an immense diagnostic challenge, finally diagnosed as brucellosis, highlighting the need for collecting detailed history and keeping in mind the local infectious epidemiological data.Brucellosis is a major endemic zoonotic disease in developing countries including India, in which systemic generalized symptoms predominate, rather than gastrointestinal complaints.
CASE PRESENTATION
Chief complaints
The patient, a 13-year-old male child, presented to us with undulating fever, loss of appetite, abdominal pain, weight loss along with malaise and myalgia for the last 14 wk.
History of past illness
The child had ventricular septal defect repair in 2018.His current echocardiogram showed mild tricuspid regurgitation.
History of present illness
The child weighed 32 kg, 3 mo prior to coming to us when a local pediatrician was consulted for complaints of intermittently high-grade fever (102-104℉) for the past 5-7 d, malaise, and abdominal pain.His blood investigations showed Haemoglobin: 11.3G/dL, CRP: 11.8 (reference level: 6 mg/L) Total leukocyte count: 3700/cu mm, Neutrophils: 56%,Lymphocytes: 39%, ESR: 30 mm (1sthour), platelets: 210000/cu mm.Dengue NS1 and Malaria dual antigen were negative.The child was treated with amoxicillin-clavulanic acid for 7 d.However, the fever was persistent after an initial remission.The local pediatrician was again consulted after 5 wk.Routine investigations were repeated and found to be normal.Additionally, Widal was reactive at 1:80 for TO and TH antigens.Chest X-ray was normal, abdominal ultrasonography revealed mild splenomegaly.
As the fever was not subsiding, the child was admitted to a tertiary care hospital for PUO evaluation of > 8 wk duration with intermittently high-grade (102-104℉) fever.On general examination, the patient was alert and active, with pallor, but no history of bleeding from any source.The chest was clear and the spleen palpable.Routine blood investigations bore similar results.A sputum acid-fast bacillus smear for 3 consecutive days was negative.Mantoux test and GeneXpert for tuberculosis, from gastric aspirate, were negative.Weil-Felix and Scrub typhus IgM ELISA were nonreactive.Serial Automated blood cultures were done to rule out Infective endocarditis all three blood culture samples yielded no growth of any pathogens after 96 h of aerobic incubation.Routine urine examination revealed no abnormality.As all other investigations were non-suggestive, in the light of an older Widal report of TO: 1:80 and TH: 1:80 positivity,the patient was started on injection ceftriaxone 50 mg/kg body weight in two divided doses, intravenously for 5 d.The patient became afebrile and was discharged in a week.
However, after a few days of remission, the child had a relapse of fever (102-104℉) with chills, abdominal pain, with irregular bowel movements.One month after discharge from the hospital, he visited us in the Outpatient department.
Physical examination
On examination, a few cervical lymph nodes were found enlarged and pallor present.Hepatosplenomegaly (liver 2 cm,spleen 0.5 cm) and abdominal tenderness were noted.His current body weight was 27.7 kg (1stpercentile) < 50 percentile(45 kg) body mass index - 13.1 (1st percentile), < 50 percentile (18.4).
Imaging examinations
Chest X-ray was normal.Ultrasonography of the abdomen showed thickening of the terminal ileum wall with no enlargement of abdominal lymph nodes.A Paediatric Gastroenterologist’s opinion was taken.A differential diagnosis of Luminal Koch’s and Small bowel Crohn’s (IBD) was considered.Colonoscopy and computed tomography (CT) enterography were planned.On Colonoscopy no abnormalities in colon or caecum were noted.No ulcers, friability, granularity,polyp, or tumor seen.The terminal ileal mucosal surface looked normal, hence no biopsy was taken.During computed tomography (CT) enterography, the ileum was not accessible, due to suboptimal distension of loops.Splenomegaly was however noted.The differential diagnosis of luminal Koch’s and inflammatory bowel disease (small bowel Crohn’s disease) was ruled out based on these investigations.
Laboratory examinations
Routine blood investigations revealed a low Haemoglobin (10.5 g/dL) red blood cell (RBC): 4.23 million/cu mm, white blood cell (WBC): 10640/cu mm, and adequate platelets.The differential count was predominantly lymphocytic,(Neutrophils 45%, Lymphocytes 50%); however, the peripheral blood film showed normocytic normochromic anemia, no malaria parasite or abnormal cells seen.The ESR was 60 mm (1sthour).Liver function tests revealed normal bilirubin level, A: G ratio was 1, serum LDH level: 365 IU/L, and globulin level: 4.3 g/100 mL, the serological tests for dengue andmalaria were again negative.The Widal tube agglutination test was non-reactive, (titer: < 1:20, for antibodies toSalmonella typhi(TO, TH) and Paratyphi A (AH) and Paratyphi B (BH) Epstein-Barr virus IgM was negative.Automated Blood culture by BacTAlert revealed growth ofBrucella melitensisafter 5 d of aerobic incubation identified by Vitek 2 Compact.Serology forBrucellawas done later by ELISA, and tested positive forBrucellaIgG: 35.14 U/maleL (positive >12 U/maleL) and IgM: 46.97 U/maleL (positive > 12 U/maleL).TheBrucella melitensisisolate was tested on MALDI-TOF,identified asBrucella spp.The chronological investigations are enumerated in Table 1.
Personal and family history
During this time, the patient’s history of contact with cattle during Bakri-Eid, and consumption of unpasteurized milk was gathered upon questioning.There was no significant family history or similar symptoms in any other family member.
FINAL DIAGNOSIS
The final diagnosis was brucellosis with an atypical presentation of terminal ileitis.
TREATMENT
The patient was treated with doxycycline (3-5 mg/kg body weight) in two divided doses daily for 6 wk, rifampicin (10 mg/kg body weight) once daily for 6 wk, and syrup multivitamin and zinc.
OUTCOME AND FOLLOW-UP
The patient turned afebrile on day 3 of treatment.On follow-up, two months after completion of the antibiotic course, the patient had drastically improved clinically, gained 4 kg body weight, hemoglobin level increased to 12.7 g/dL from 10.2 g/dL, the A: G ratio improved to 1.2 from 1.0, and liver enzymes came back within normal range.
DISCUSSION
Literature review
The gastrointestinal symptoms of brucellosis are frequently present but are usually restricted to loss of appetite.Ileal involvement in human brucellosis is extremely rare.Only seven cases in the literature have been reported to the best of our knowledge, and not a single case from India[7-13].The first case of ileitis was reported by Petrellaet al[7] from Texas in a child, in the year 1988, which was linked to the ingestion of unpasteurized goat milk cheese, during an outbreak ofBrucella melitensis[7].The age and sex of this child and details of diagnosis and treatment are not available.A 15/male patient, from China, living in an endemic area, denied any contact with cattle, had a fever and diffuse abdominal pain of 4 wk duration, and demonstrated mucosal thickening on abdominal Ultrasonography[8].Our patient too had presented with a three-month long history of undulating fever, and abdominal pain, with thickening of mucosa of terminal ileum,demonstrated on ultrasonography.Another patient, an adolescent, 17/male, from Turkey, presenting with features of terminal ileitis and epididymo-orchitis, had a fever for 3 d, whose family dealt in livestock, gave a history of abortion in cattle[9].A 31/male patient from Jordan presenting with ileocolitis, had an 11-mo long history of fever, night sweats,abdominal pain, diarrhea, and bleeding per rectum.Serology was positive forBrucella abortusIgM (1:160).The patient was treated with Rifampicin and Cotrimoxazole for 6 wk.Blood culture was however negative[10].A 68/female fromPortugal tested positive by both blood cultures which showed growth ofBrucellasp.and serology with 4 mo long duration of symptoms[11].Our patient was also positive forBrucella melitensison blood culture and serology reactive forBrucellaIgG and IgM.A 32/male from Pakistan, with fever for 10 d and acute abdominal pain for 1 d, history of unpasteurized milk consumption, had to be operated on twice for intestinal perforation repair.His biopsy revealed inflammation of Peyer’s patches[12].The latest and last reported case is from Mexico, 56/female, with antithrombin III deficiency, presented to the emergency with acute abdomen, and had to be operated on to relieve intestinal obstruction.She was reactive for Rose Bengal Plate agglutination test (RBPT) (1:100).Biopsy revealed ileitis and colitis[13].
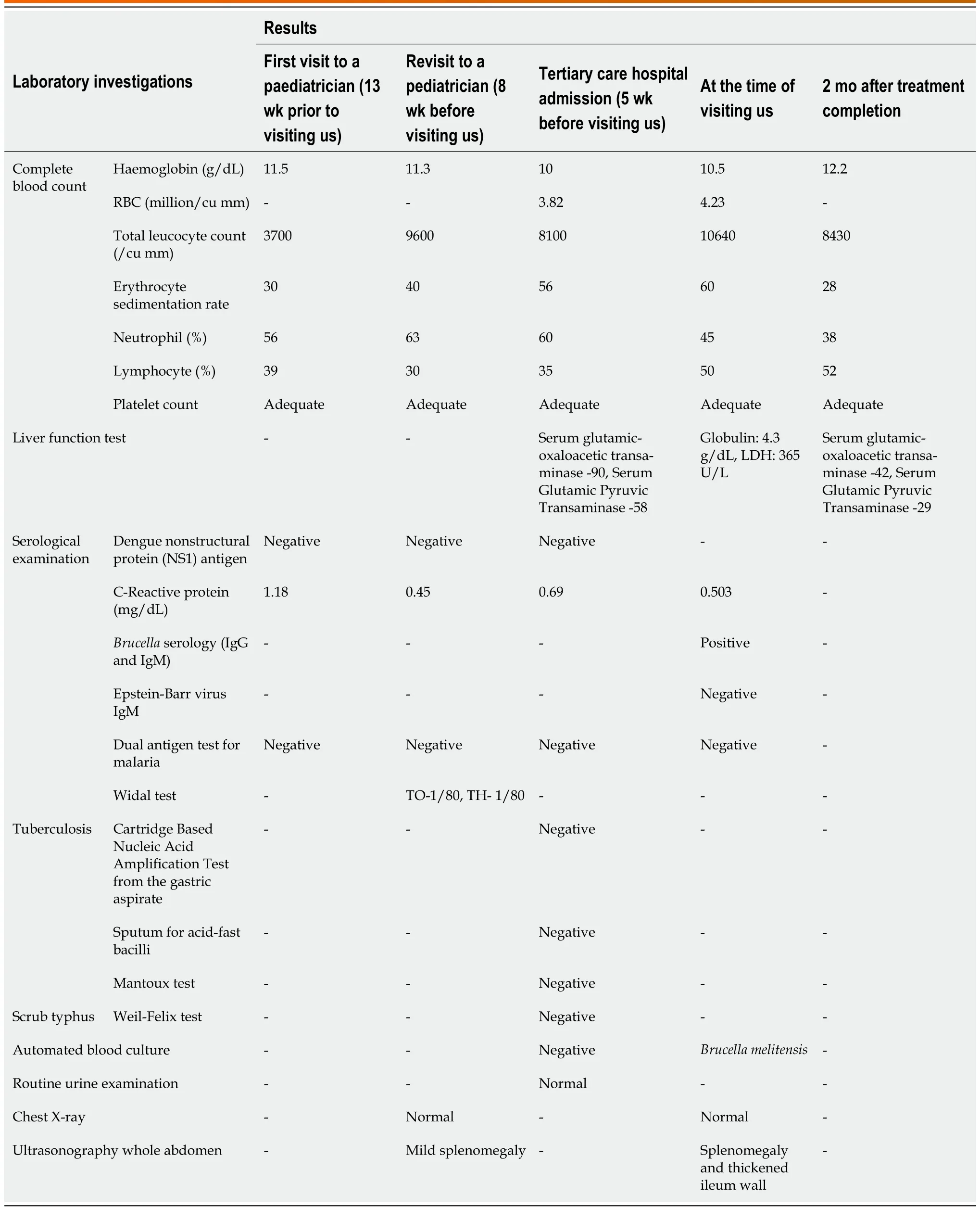
Table 1 Laboratory investigations for diagnosis of pyrexia of unknown origin
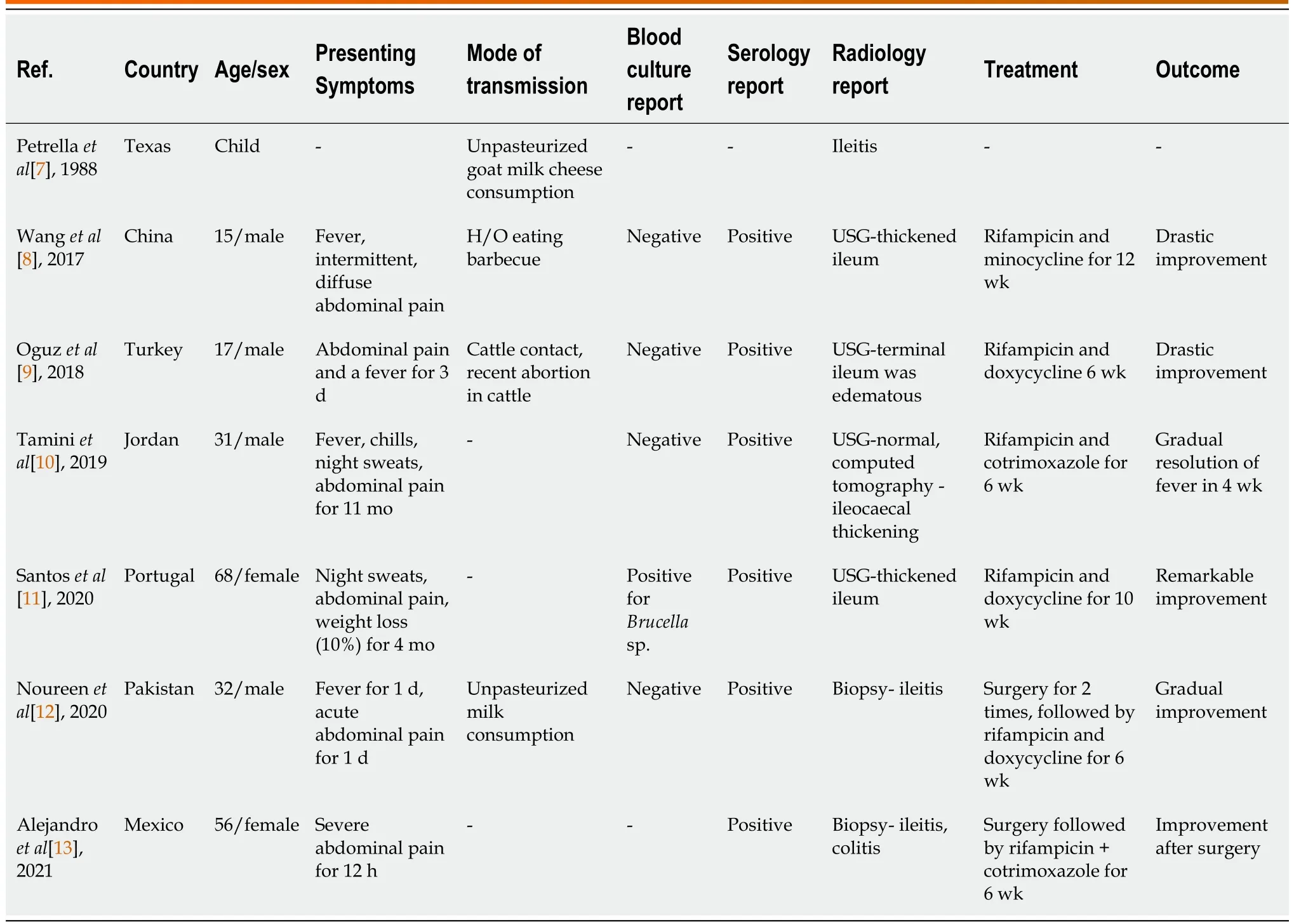
Table 2 Summary of brucellosis cases with terminal ileitis as reported in the literature
A total of 42.8% of cases (3/7) in literature are under 18 years of age.67% (4/7) are males.The duration of symptoms ranged from as short as 12 h to as long as 11 mo.50% of patients (3/6) had symptoms of ≥ 4 wk duration.The commonest symptoms were abdominal pain: 100% (6/6), fever: 83.3% (5/6), malaise: 50% (3/6), significant loss of weight equivalent to 10% of body weight: 16.6%.History of contact with cattle was given by 1/7 patient (14.2%)[9], unpasteurized dairy product consumption by 28.4% (2/7) of patients[7,11] history of eating barbecue 14.2% (1/7 patients)[8] and one 15/male(14.2%) came from a province in North China that is endemic for Brucellosis.For two patients cattle contact or unpasteurized dairy product consumption history was not available.
Serology was positive in all 6/6 (100%) cases for which details are available.Only one patient had a blood culture positive forBrucellasp.(14.2%) The species identification, however, is not available in that case[11].5/7 cases (71.4%)gave radiographic evidence of ileitis, three on ultrasound of abdomen (42.8%)[8,9,11], and one patient by CT scan.His Ultrasonography was normal[10].The Texas child had radiographic evidence of ileitis too, but the method was unknown[7].2/7 of the patients (28.5%) underwent emergency surgery to relieve intestinal obstruction and repair of ileal perforation.Both patients’ biopsies (28.5%) revealed ileitis[12,13].
Antimicrobial therapy was with Rifampicin and Doxycycline in three of the patients, one each from Turkey[9],Portugal[11], and Pakistan[12] for 6, 10, and 6 wk respectively.All three patients improved drastically.One patient each from Jordan[10] and Mexico[13] was treated with Rifampicin and trimethoprim-sulfamethoxazole combination for 6 wk,due to allergy to tetracyclines.The 15-year-old boy from China was treated with Rifampin and Minocycline (due to unavailability of Doxycycline) for a duration of 12 wk[8].Recovery was complete in all cases (100%).Duration of therapy was 6 wk in 4/6 patients (66.6%) It was 12 wk in the Chinese on Minocycline[8].The patient from Portugal had colitis along with ileitis, and diarrhea had not responded at the end of 6 wk, so the treatment was prolonged by an additional 4 wk[11].Treatment details of the first reported case from Texas are unavailable.Our patient responded very well and recovered fully, after treatment with Rifampin and Doxycycline for 6 wk.Table 2 enumerates the summary of brucellosis cases with terminal ileitis as reported in the literature.
Brucella melitensiscauses the most severe infections among allBrucellasp.in humans.It is transmitted mainly through oral route and gains entry through ingestion by infecting the Peyer’s patches in the small intestine[14].Unpasteurized dairy products, improperly cooked meat, or rarely airborne transmission through abortus are common modes[15].Our patient had a history of consumption of unpasteurized milk as well as contact with cattle during Bakri-Eid.
It’s a worldwide zoonotic disease, endemic in Mexico, the Middle East, China, India, and African and Southern European nations[16].In India, serological studies showed 1.28% positivity in rural Nagpur[17], 4.96% in Jammu region[18], 6.02% in Goa region[19], 8.5% in Gujarat[20] and up to 10.6% in Eastern India[21].Yet Brucellosis is a forgotten entity when a differential diagnosis of PUO is being considered especially in children in the urban set-up.It is not just a debilitating illness, it also contributes to a significant economic burden.It has been estimated that annual median losses in India, due to Brucellosis in the human population, is Rs 442.3 million among adults and Rs 185.0 million among children[22].A timely diagnosis can lead to the prevention of both mental and physical agony for the patients and their families along with a much lower financial burden.Given that epidemiological factors and patient history give a significant clue to the etiology of PUO, laboratory testing based on local data and a diagnostic algorithm may be helpful in diagnosing a large proportion of such cases.SinceBrucella melitensisis a difficult-to-isolate pathogen, timely and adequate volumes of sample collection for blood, and bone marrow cultures, along with awareness and expertise on the part of laboratory personnel are important to diagnose this rare isolate.Serology is an easier option to diagnose this disease as the majority of cases are culture-negative.Several serological tests are available.RBPT, with high sensitivity but low specificity and ease of doing the test, is a good screening test.Titers of > 1:8 or 1:16 in endemic areas need to be confirmed by the Standard Tube agglutination test (SAT).SAT titers above 1:320 in endemic areas are suggestive of Brucellosis[23].ELISA assays are extremely sensitive and specific.Other tests like dipstick assays, and lateral flow assays are also available.PCR from samples like classical cerebrospinal fluid is a promising test but with limited availability[23].
CONCLUSION
Alertness and coordination amongst treating pediatrician, physician, and microbiologists can lead to timely diagnosis of this relatively easy-to-treat cause of PUO, preventing dire complications like intestinal perforation and intussusception.To ensure prompt and correct diagnosis, a high index of suspicion, knowledge of local epidemiological data, detailed history collection, rapid access, and an effective healthcare setting are needed.
FOOTNOTES
Author contributions:All authors were involved in the care of the patient; All authors drafted and reviewed the manuscript.
Informed consent statement:Informed written consent was obtained from the patient for publication of this report.
Conflict-of-interest statement:There is no conflict of interest to declare.
CARE Checklist (2016) statement:The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:India
ORCID number:Kokila Banerjee 0000-0002-6896-4207.
S-Editor:Liu JH
L-Editor:A
P-Editor:Yuan YY
