Risk factors and their interactive effects on severe acute pancreatitis complicated with acute gastrointestinal injury
2023-10-21JianHuiChenMeiFenZhangWenChaoDuYanAnZhang
Jian-Hui Chen, Mei-Fen Zhang, Wen-Chao Du, Yan-An Zhang
Abstract
Key Words: Severe acute pancreatitis; Acute gastrointestinal injury; Risk factors; Interactions; Acute physiological and chronic health scoring system II; Creatinine
INTRODUCTION
Severe acute pancreatitis (SAP) refers to a disease in which pancreatic enzymes are activated due to a variety of reasons,resulting in a local inflammatory response. This disease is a common critical condition of the digestive system[1,2]. Statistically, the death rate due to SAP is up to 10%-30%[3], and has been on the rise in recent years, which seriously endangers the life and health of patients. Acute gastrointestinal injury (AGI) is a common complication of SAP. AGI patients have gastrointestinal dysfunction and mucosal injury, which can cause gastrointestinal motility slowing, intestinal obstruction,intestinal flora shift, impaired immune function, ulcer, gastrointestinal bleeding,etc., which aggravates the degree of pancreatitis, causes multiple organ dysfunction, and endangers the life of patients[4]. AGI is an important prognostic factor for SAP patients. Relevant studies have found that when AGI occurs in SAP patients, the mortality and incidence of complications are significantly increased[5]. However, there are numerous risk factors for AGI[6,7]. Therefore, examining the risk factors for AGI is of great significance for controlling the development of AGI, improving the prognosis of SAP,and taking effective intervention measures to improve the treatment of patients. However, most studies have investigated the risk factors for AGI, while reports on the interaction between risk factors are few. Therefore, the present study aimed to analyze the risk factors for AGI and determine their interactive effects on SAP to provide a rationale for clinical treatment.
MATERIALS AND METHODS
General information
A retrospective analysis of 168 patients with SAP treated in our hospital, and enrolled between December 2019 and June 2022 was conducted. Inclusion criteria were as follows: (1) According to the "Guidelines for the diagnosis and treatment of acute pancreatitis in China (2021)"[8], all patients were diagnosed by abdominal color Doppler ultrasound, CT or MRI;and (2) The age of patients ranged from 18 to 65 years. Exclusion criteria were: (1) Patients with gastrointestinal bleeding and complete intestinal obstruction; (2) Severe heart, kidney or other important organ dysfunction; and (3) Long-term use of corticosteroids or immunosuppressants. According to the AGI diagnostic criteria "European Society for the Critical Care Medicine (2012) Consensus on Acute Gastrointestinal Injury"[9], patients were divided into the AGI group (n= 64)and non-AGI group (n= 104).
Clinical data collection
Clinical data were collected from the patients. These data included gender, age, comorbidities (hypertension, diabetes,coronary heart disease), smoking history, acute physiological and chronic health scoring system II (APACHE II) score,and multiple organ dysfunction syndrome (MODS). Admission laboratory indicators included white blood cell (WBC)count in peripheral blood, hemoglobin, total bilirubin, creatinine (CRE), and serum amylase.
Statistical analysis
The SPSS 23.0 software was applied for analysis and processing. Quantitative data that conformed to a normal distribution are shown as mean ± SD, andt-tests were used for comparisons between the groups. Count data are expressed asn(%), and theχ2test was used for comparisons between the groups. Logistic regression was applied to analyze the associated risk factors. The interaction of two factors was investigated using regression models. The attributable proportion of interaction (API), relative excess risk of interaction (RERI) and the synergy index (S) were calculated.P<0.05 was considered statistically significant.
RESULTS
Comparison of clinical and laboratory data between the two groups
Univariate analysis showed that the percentage of patients with MODS, APACHE II score and CRE level were higher in the AGI group than in the non-AGI group, with a significant difference between the two groups (P< 0.05), as shown in Table 1.
Logistic multi-factor analysis of SAP and concurrent AGI
Variables that were statistically significant in univariate analysis were included as independent variables, and the influencing factor variable assignment is shown in Table 2. The results of the multifactorial regression analysis indicated that an APACHE II score > 15 and CRE > 100 µmol/L were risk factors for complications of AGI in patients with SAP (P<0.05), as shown in Table 3.
Interaction analysis of risk factors for AGI
The RERI of the interaction between the increase in APACHE II score and the increase in CRE level was 220.059, the API was 0.678%, and the S was 3.123. This indicated that there was a positive interaction between the two factors, as shown in Table 4.
Receiver operating characteristic curve analysis on the predictive value of APACHE II and creatinine
Receiver operating characteristic (ROC) curve analysis showed that the predictive value of joint detection of APACHE II and CRE was better than that of single detection (P< 0.001). The ROC curves of the three were significantly different (P<0.05) (Figure 1).
DISCUSSION
SAP is a special type of acute pancreatitis, which is caused by biliary tract disease, overeating, and heavy drinking, which leads to the activation of pancreatic enzymes and an acute chemical inflammatory reaction of pancreatic tissue[10]. In the early stage of SAP, a large number of inflammatory mediators, cytokines and bacterial toxins are produced, which lead to hemodynamic abnormalities and damage to organs such as heart, liver, kidney and the gastrointestinal tract, and in severe cases, organ failure[11]. AGI is one of the most common complications in SAP patients. As the gastrointestinal tract is the reservoir for systemic flora, it has functions such as regulating immune and inflammatory functions. When AGI occurs, it causes intestinal flora shift, gastrointestinal ulcer, gastrointestinal nutrition disorders,etc., which aggravate the inflammatory response, induce multiple organ failure in patients, prolong the length of hospital stay, and increase patient mortality[12]. Wanget al[13] found that AGI was an independent risk factor for SAP. Therefore, active treatment of AGI to promote the recovery of gastrointestinal function is the key to alleviating SAP, reducing mortality, and improving prognosis.
The results of this study indicated that patients with SAP complicated by AGI had a significantly higher MODS ratio,leukocyte level, CRE level, and APACHE II score compared to the non-AGI group, with significant differences. Logistic regression analysis indicated that APACHE II scores > 15 and increased CRE levels were the main risk factors for complications of AGI in SAP. Targeted measures should be taken against the above factors to strengthen prevention. The gastrointestinal tract plays an important role in the human body. Various injuries, surgeries, severe infections, massive bleeding and so on can promote the release of inflammatory factors. These inflammatory factors can activate the signal transduction of nuclear factors in gastrointestinal mucosal epithelium, causing microcirculation disorders in the gastrointestinal tract resulting in impaired gastrointestinal function[14]. The findings in the present study indicate that AGI patients have higher levels of WBCs than non-AGI patients. It is suggested that the increase in these indices may be the risk factors of SAP complicated by AGI. CRE is a product of human muscle metabolism, and increased CRE will have a considerable impact on the body. When the CRE level increases, this indicates that the body's metabolism is abnormal,and a large amount of toxins and waste are accumulated, which results in disordered human functions and leads to various metabolic imbalances[15]. In addition, increased CRE level will accumulate in the heart, respiratory system,gastrointestinal system,etc., and will indirectly reflect glomerular and gastrointestinal system dysfunction, which will lead to gastrointestinal injury and systemic injury[16]. Jinet al[17] found that elevated serum CRE level was a risk factor for gastrointestinal failure, and the results of this study were consistent with these findings.
The APACHE II scoring system consists of a total score of three components: Acute physiology, age, and chronic health status. It is widely applied in the assessment of critically ill patients, and is also a commonly used scoring system to judge the severity of acute pancreatitis[18,19]. An APACHE II score > 15 indicates a poor prognosis, and patients with higher scores have severe disease[20]. Greenberget al[21] showed that the higher the APACHE II score within 72 h of admission in SAP patients, the higher the death rate. The findings of the present research indicated that patients in the AGI group had higher APACHE II scores than those in the non-AGI group. It is suggested that SAP patients with AGI are morecritically ill and have a higher risk of death. The complexity of gastrointestinal function also lies in its internal dynamic changes. Disorder and translocation of intestinal flora is another potential mechanism for the occurrence of AGI.Intestinal flora activate the immune response through the lymphatic system, leading to the occurrence and even deterioration of MODS[22]. This research found a higher percentage of patients with AGI than with non-AGI, which was similar to the findings of Laterreet al[23]. It is suggested that MODS is closely related to SAP complicated by AGI.
研究显示:精神科护士一年内遭受工作场所暴力发生率为57.0%~99.0%[2,12-13]。本次调查显示:我院精神科护士1年内遭受工作场所暴力发生率为75.3%。精神科护士遭受工作场所暴力高的原因为:①精神病病人大多存在思维、行为异常,受幻觉、妄想影响,随时可能出现冲动伤人行为,而护士与病人接触机会最多,遭受暴力危害最直接[14];②在护士职业道德影响下,护士对病人暴力行为常采取忍让态度,处于较为被动地位,不能有效控制暴力;③精神科保护性约束或隔离措施的使用与暴力发生密切相关[15],护士在执行保护性约束和隔离措施时,经常遭受病人暴力。
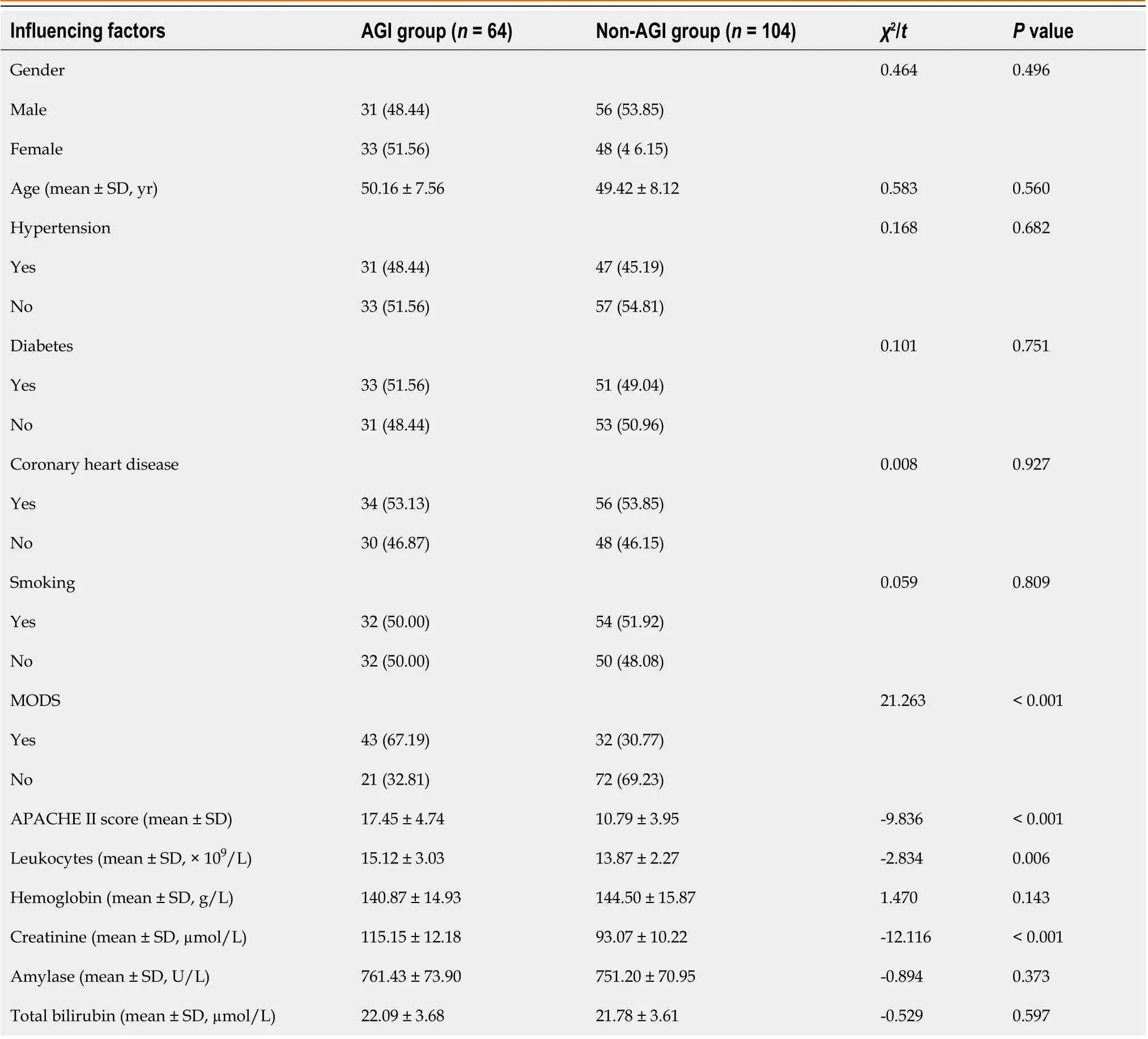
Table 1 Comparison of clinical and laboratory data between the two groups, n (%)
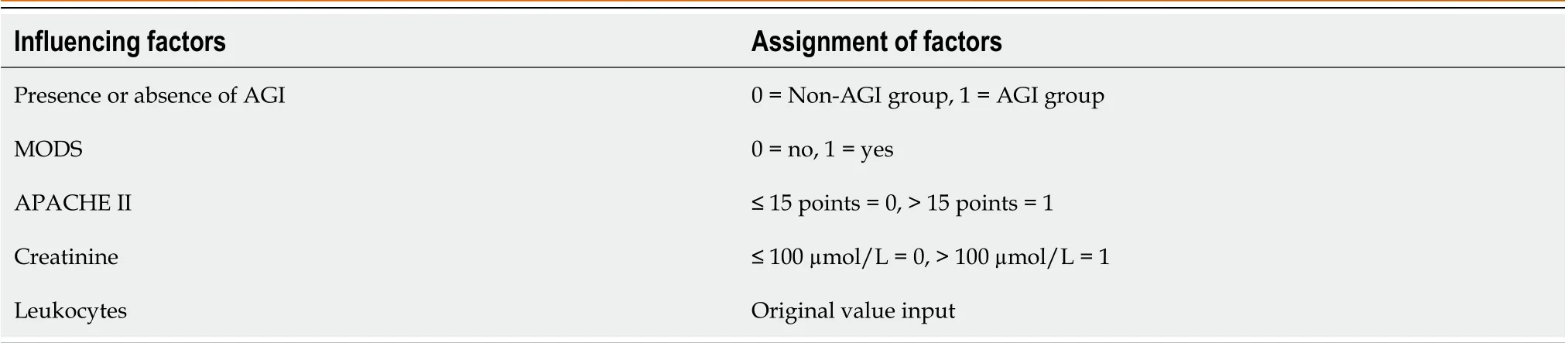
Table 2 Factor assignment for logistic regression analysis
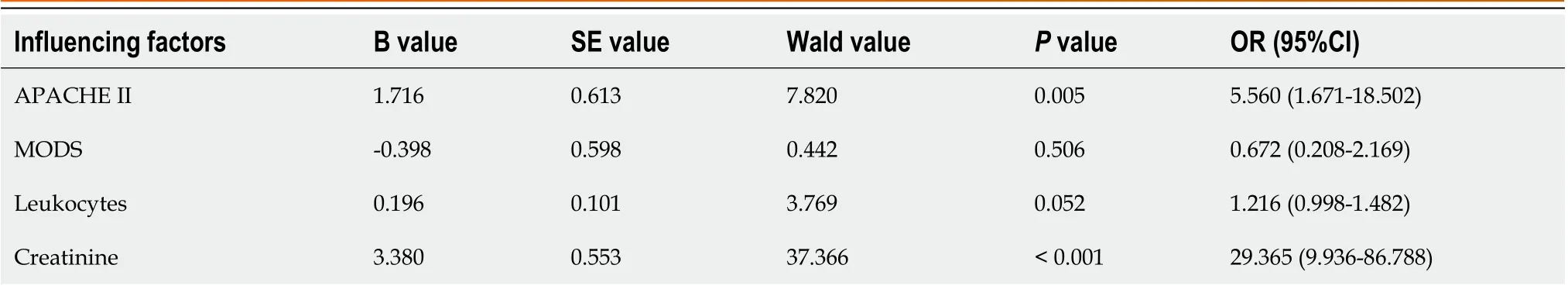
Table 3 Logistic regression analysis of severe acute pancreatitis patients with acute gastrointestinal injury
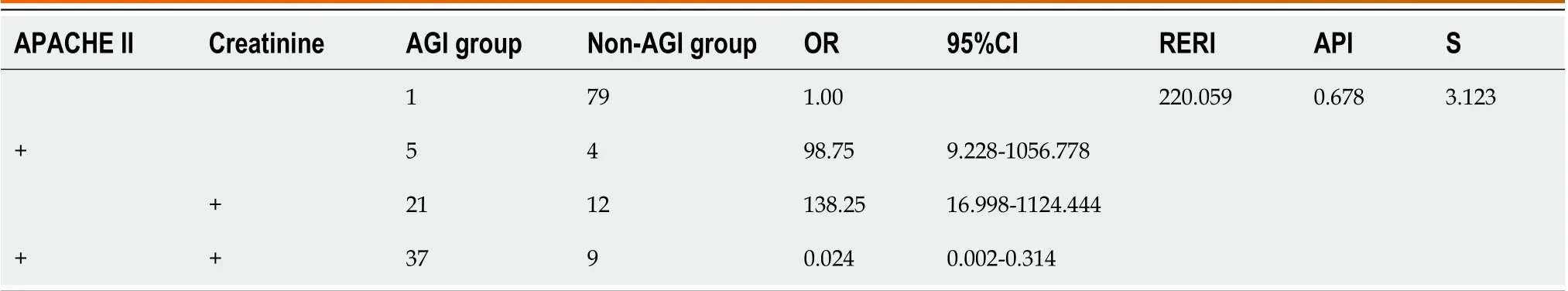
Table 4 Interaction of creatinine and acute physiological and chronic health scoring system II score on acute gastrointestinal injury in severe acute pancreatitis patients
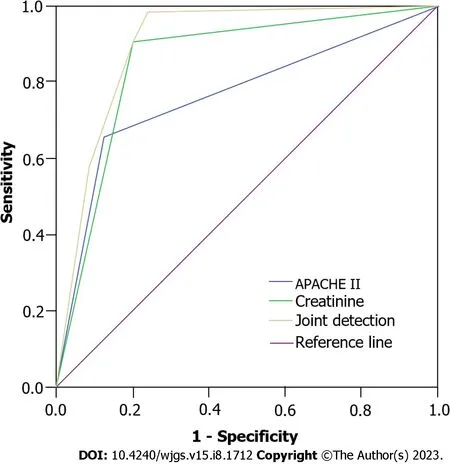
Figure 1 Receiver operating characteristic curve analysis of acute physiological and chronic health scoring system II, creatinine and joint detection. APACHE II: Acute physiological and chronic health scoring system II.
From the interaction study of risk factors, it was found that there was a statistically positive interaction between the APACHE II score and CRE level in SAP patients with AGI. The RERI of the interaction effect between high APACHE II score and elevated CRE level was 220.059, indicating that the risk of AGI increased by 220.059 times. The API was 0.678%and S was 3.123, indicating that 0.678% of AGI in these patients was caused by the coexistence of increased APACHE II score and increased CRE level, and the coexistence of both was 3.123 times that of AGI induced by the existence of either factor alone. Therefore, APACHE II score > 15 and CRE level > 100 µmol/L can lead to AGI in SAP patients. The changes in gastrointestinal function should be closely monitored, and timely and effective treatment should be provided to control the development of the patient's disease, reduce the body's inflammatory response, and avoid the involvement of other organs.
The present research was conducted to investigate the risk factors of SAP complicated by AGI and analyze the interaction between these risk factors. In this way, measures to prevent the incidence of AGI were implemented to improve the prognostic outcome of patients with SAP. However, the sample size in this study was limited, and the results may be biased to some extent. It is necessary to expand the sample and conduct a multicenter study to further confirm the risk factors of AGI in SAP patients.
CONCLUSION
An APACHE II score > 15 and CRE level > 100 µmol/L are both independent risk factors for SAP complicated with AGI,and there is a positive interaction between them. Therefore, in SAP patients with AGI, attention should be paid to managing the risk factors of AGI in SAP patients, and timely and effective interventions should be carried out to reduce the incidence of AGI and to improve the prognosis of SAP patients.
ARTICLE HIGHLIGHTS

FOOTNOTES
Author contributions:Chen JH designed and performed the research and wrote the paper; Zhang YA designed the research and supervised the report; Zhang MF designed the research and contributed to the analysis; Du WC supervised the report.
Institutional review board statement:This study was approved by the Medical Ethics Committee of Longyan First Affiliated Hospital of Fujian Medical University (Approved No. LYREC2023-k016-01).
Informed consent statement:This was a retrospective study and was exempt from informed consent according to Institutional policy.
Conflict-of-interest statement:The authors declare no conflicts of interest for this article.
Data sharing statement:The data used for this study can be obtained from the corresponding author upon request.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORCID number:Jian-Hui Chen 0009-0002-3734-7676; Mei-Fen Zhang 0009-0001-4005-7453; Wen-Chao Du 0009-0006-0826-8409; Yan-An Zhang 0009-0003-2341-6789.
S-Editor:Wang JL
L-Editor:A
P-Editor:Ji MX
猜你喜欢
杂志排行
World Journal of Gastrointestinal Surgery的其它文章
- Is endoscopic mucosal resection-precutting superior to conventional methods for removing sessile colorectal polyps?
- Knowledge, attitude, and practice of monitoring early gastric cancer after endoscopic submucosal dissection
- Changing trends in gastric and colorectal cancer among surgical patients over 85 years old: A multicenter retrospective study, 2001-2021
- Enhanced recovery nursing and mental health education on postoperative recovery and mental health of laparoscopic liver resection
- Effects of ultrasound monitoring of gastric residual volume on feeding complications, caloric intake and prognosis of patients with severe mechanical ventilation
- Regional differences in islet amyloid deposition in the residual pancreas with new-onset diabetes secondary to pancreatic ductal adenocarcinoma
