The neuro-prognostic value of the ion shift index in cardiac arrest patients following extracorporeal cardiopulmonary resuscitation
2023-09-19GannanWangZheWangYiZhuZhongmanZhangWeiLiXufengChenYongMei
Gannan Wang ,Zhe Wang ,Yi Zhu ,Zhongman Zhang ,Wei Li ,Xufeng Chen ,Yong Mei,
1 Department of Emergency, the First Affiliated Hospital of Nanjing Medical University, Nanjing 210029, China
2 Key Laboratory of Emergency and Trauma of Ministry of Education, College of Emergency and Trauma, Hainan Medical University, Haikou 571199, China
BACKGROUND: The ion shift index (ISI) as a prognostic indicator that can show the severity of hypoxic-ischemic injury.We aimed to evaluate the performance of the ISI in predicting unfavorable neurological outcomes at hospital discharge in cardiac arrest (CA) patients following extracorporeal cardiopulmonary resuscitation (ECPR) and to compare its performance to other prognostic predictors.METHODS: This was a retrospective observational study including adult CA patients treated with ECPR between January 2018 and December 2022 in a tertiary hospital.Data regarding clinical characteristics and laboratory parameters were collected from medical records.The ISI was determined based on the first available serum electrolyte levels after ECPR.The primary outcome was unfavorable neurological status at hospital discharge,defined as Cerebral Performance Categories 3-5.Comparisons of the characteristics between the two groups were made using the X2 test for categorical variables and the t-test or non-parametric Mann-Whitney U-test for continuous variables,as appropriate.Correlation analysis was performed using Spearman’s rank correlation coefficient.A two-tailed P-value <0.05 was considered statistically significant.RESULTS: Among the 122 patients involved,46 (37.7%) had out-of-hospital CA,and 88 had unfavorable neurological outcomes.The ISI was significantly higher in the unfavorable outcome group than in the favorable outcome group (3.74 [3.15-4.57] vs.2.69 [2.51-3.07],P<0.001).A higher ISI level was independently related to unfavorable outcome (odds ratio=6.529,95% confidence interval 2.239-19.044,P=0.001).An ISI level >3.12 predicted unfavorable outcomes with a sensitivity and specificity of 74.6% and 85.2%,respectively (P<0.001).The prognostic performance of ISI (area under the curve [AUC]=0.887) was similar to that of other predictors,such as gray-to-white matter ratio (AUC=0.850,P=0.433) and neuronspecific enolase (AUC=0.925,P=0.394).CONCLUSION: ISI may be used as a prognostic biomarker to predict neurological outcomes in CA patients following ECPR.
KEYWORDS: Cardiac arrest;Ion shift index;Extracorporeal cardiopulmonary resuscitation
INTRODUCTION
Cardiac arrest (CA) is the leading cause of morbidity and mortality worldwide.[1,2]It has been reported that approximately 9.1% of individuals with out-of-hospital CA(OHCA) and 18.8% of patients with in-hospital CA (IHCA)survive to hospital discharge.[3]Despite the main advances in cardiopulmonary resuscitation (CPR) practice over the past few decades,the rate of survival with favorable neurological outcomes after CA has remained poor.[3]Extracorporeal CPR (ECPR) can be initiated to restore perfusion,taking the limit of hypoxic-ischemic brain injury and allowing for the possible identification and treatment of the underlying causes of CA as its goal.[4]ECPR may be considered a rescue therapy for selected patients when conventional CPR (CCPR) fails.[5]A meta-analysis suggested that when compared to CCPR,ECPR produced more survivors at hospital discharge,and among those survivors,more were neurologically intact.[6]Early neuro-prognostication after CA would help clinicians choose a proper therapy strategy and perform early assessment of outcomes for patients.[7]
Various serum biomarkers,such as neuron-specific enolase (NSE) and S-100β protein,appear to have prognostic value in the prediction of unfavorable outcomes after CA.[8]However,no consensus has been reached on a threshold value .[9]The ion shift index (ISI) is recommended as a prognostic indicator of ischemic injury severity,def ined as the ratio between the ion concentrations of intracellular fluid (ICF),including serum potassium,magnesium,and phosphate,and those of extracellular fluid (ECF),namely,serum calcium.[10]The present study was designed to assess the prognostic value of the ISI in the prediction of unfavorable neurological outcomes at hospital discharge in comatose CA patients following ECPR and to compare the power to other prognostic predictors.
METHOD
Study population
A retrospective observational study of adult (age≥18 years old) refractory OHCA and IHCA patients who underwent ECPR from January 2018 to December 2022 in a tertiary hospital was conducted.According to the inclusion criteria of ECPR implementation,[11]eligible patients were treated with veno-arterial extracorporeal membrane oxygenation (ECMO) through the femoral vein and artery if return of spontaneous circulation (ROSC) was not achieved more than 10 min after CCPR.Among these,the following patients were excluded: (1) those whose ECMO support duration was less than 12 h;(2) those who experienced CA due to electrolyte/acid-base disturbances,such as hyperkalemia/hypokalemia or diabetic ketoacidosis;(3)those whose levels of serum electrolytes within 6 h following ECMO pump-on were not available;(4) those who had preexisting medical conditions that might affect the levels of serum electrolytes,such as chronic kidney disease;(5) those who received potassium,magnesium,calcium or sodium bicarbonate ahead of blood sampling;or (6) those whose information about CA characteristics and other prognostic predictors were incomplete.
This study was approved by the Ethics Committee of the First Affiliated Hospital of Nanjing Medical University(2020-SR-226).
Data collection
Clinical data,including age,sex,comorbidities,CA location,witnessed status,bystander CPR,etiology of CA,initial rhythm,resuscitation duration (from CCPR to ECMO pump-on),Glasgow Coma Scale (GCS) score after ECPR,and ECMO duration,were systematically collected from patients’ medical records.Laboratory data were obtained within 6 h after ECMO pump-on,including serum electrolytes(potassium,magnesium,phosphate and calcium),hemoglobin,pH,lactate,glucose,albumin,alanine aminotransferase(ALT),aspartate aminotransferase (AST),total bilirubin,and creatinine.The levels of serum electrolytes were detected by an automatic biochemical analyzer (AU5400,Olympus,Japan) at the hospital laboratory.The ISI was obtained by the following equation[9]:
The available prognostic predictors,including clinical examination,gray-to-white matter ratio (GWR) through brain computed tomography scan and serum NSE,were evaluated so that the prognostic performance of ISI can be compared with that of other prognostic predictors.The indicators of unfavorable neurological outcome were considered when either of the following appeared:pupillary/corneal reflex absence,absent motor response or extensor posturing to external stimuli (GCS-motor response [GCS-M]≤2).Excluding the effects of sedatives or neuromuscular blocking drugs,pupillary/corneal ref lexes and GCS-M should be confirmed at least 72 h after CA.Moreover,the GWR at the level of the basal ganglia was obtained using the method mentioned in our previous study.[12]The highest values of serum NSE within 72 h after CA were collected for neuro-prognostication.[13]
Outcome
The primary endpoint of our study was neurological status at hospital discharge,which was assessed according to the Cerebral Performance Category (CPC) score.[14]An investigator blinded to the study hypothesis determined the CPC score by reviewing electronic medical records.The patients were classified into either a favorable neurological outcome (CPC 1-2) group or an unfavorable outcome (CPC 3-5) group.
Statistical analysis
Continuous variables are presented as the mean±standard deviation (SD) or median with interquartile range (IQR) depending on their normality,which was assessed by the Kolmogorov-Smirnov test.Categorical variables were described as frequencies with percentages(%).Comparisons of the characteristics between the two groups were made using the χ2test for categorical variables and thet-test or non-parametric Mann-WhitneyU-test for continuous variables,as appropriate.Correlation analysis was performed using Spearman’s rank correlation coefficient.A multivariate logistic regression model was constructed by variable selection following a backward stepwise procedure.Variables withP<0.10 in the univariate analysis (i.e.,OHCA,resuscitation duration,ALT,pH,lactate,and ISI) were included in the multivariate regression model.Variables that were closely related to those already included in the model were excluded.The results of the logistic regression analysis were summarized using odds ratios (ORs) and 95% confidence intervals (95%CIs).Receiver-operating characteristic (ROC) curves were plotted to determine the performances of ISI alone,the multivariate logistic regression model (i.e.,ISI in combination with other predictors),individual electrolytes in the index (potassium,magnesium,phosphate,and calcium),lactate,and those of other indicators in predicting unfavorable neurological outcome (GWR and NSE).The area under the curve (AUC)of ISI and those of other variables were calculated and compared by using DeLong’s test.[15]The optimal cutoffvalues of variables were determined on the basis of the maximal sensitivity and specificity.All statistical tests were processed using SPSS (version 23.0,SPSS Inc.,USA) and MedCalc (version 20,MedCalc Software Ltd.,Belgium)software.A two-tailedP-value <0.05 was considered statistically significant.
RESULTS
Clinical and laboratory characteristics
A total of 135 adult CA patients who underwent ECPR were enrolled during the study period.Among them,13 patients were excluded,as described in Figure 1,and 122 patients were included in our study.Forty-six (37.7%)patients experienced OHCA.According to the CPC score at hospital discharge,34 patients (27.9%) were in the favorable neurological outcome group,and 88 (72.1%) were in the unfavorable outcome group.The clinical and laboratory characteristics of the involved patients are presented in Table 1.
Prognostic factors related to unfavorable neurological outcome
In the univariate analysis,OHCA,initial non-shockable rhythm,resuscitation duration,ALT,pH,lactate,and ISI were related to an unfavorable neurological outcome at hospital discharge.In the multivariate logistic regression analysis (Table 2),a higher ISI level was independently related to unfavorable outcome at hospital discharge (OR6.529,95%CI2.239-19.044,P=0.001).
Prognostic performance of ISI
Spearman’s correlation analysis showed that the level of ISI was significantly correlated with resuscitation duration(r=0.408,P<0.001) and lactate (r=0.431,P<0.001).The prognostic performances of variables in the prediction of unfavorable neurological outcome are summarized in supplementary Table 1 and Figure 2.An ISI level >3.12 predicted unfavorable outcomes with a sensitivity and specificity of 74.6% and 85.2%,respectively (P<0.001).The AUC of ISI was 0.887 (95%CI0.817-0.956),which was significantly greater than that of individual electrolytes included in the index as well as that of lactate (P<0.05).Moreover,the AUC of ISI was comparable to that of other predictors,such as GWR (0.850,95%CI0.783-0.918,P=0.433) and NSE (0.925,95%CI0.876-0.975,P=0.394).
Prognostic performance of ISI in combination with other predictors
The AUC of the multivariate logistic regression model involving ISI was 0.945 (95%CI0.899-0.990),which was significantly higher than that of ISI alone (P<0.001). ISI in combination with other predictors (OHCA,initial nonshockable rhythm,resuscitation duration,ALT,pH,and lactate) showed a more promising prognostic performance.
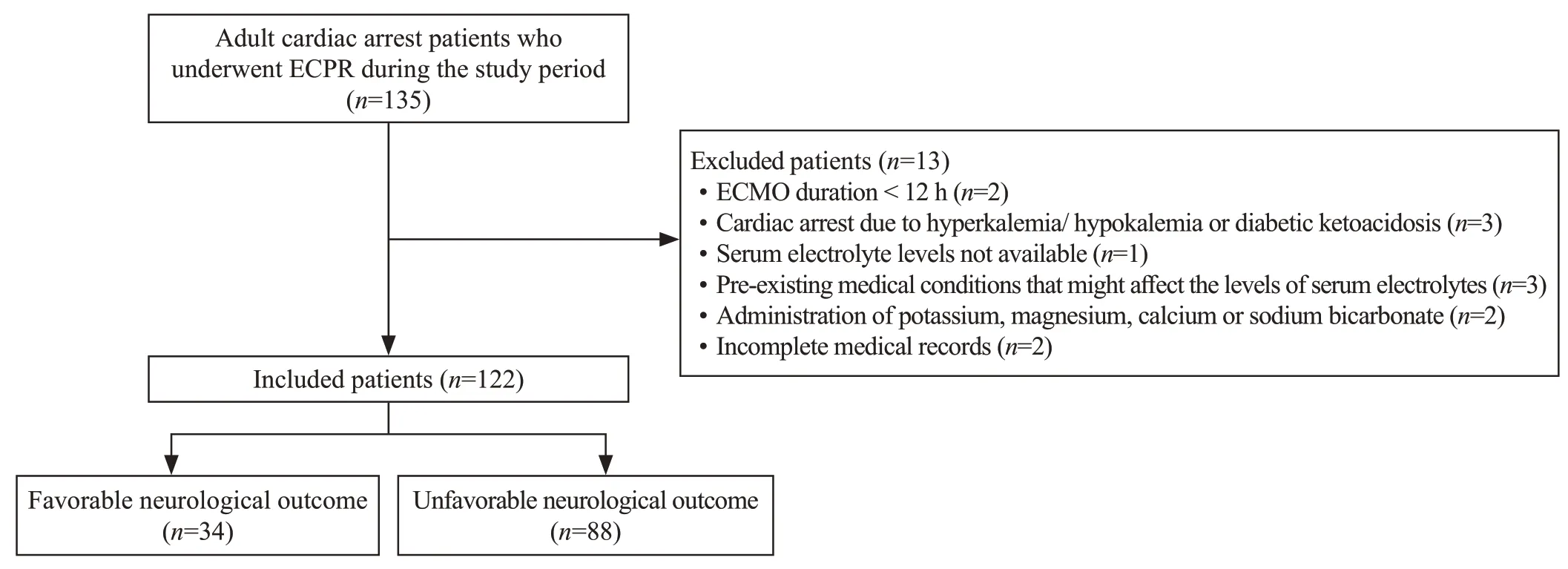
Figure 1.Flow chart of patient enrollment.ECPR: extracorporeal cardiopulmonary resuscitation;ECMO: extracorporeal membrane oxygenation.
DISCUSSION
ECPR is an invasive and resource-intensive therapy that requires highly specialized equipment and personnel and is expensive.Therefore,accurate prognostication is necessary to avoid an improper withdrawal of life-sustaining treatment in patients still having the possibility of a neurologically meaningful recovery and to avoid excessive treatment in those patients undergoing a severe and irreversible neurological injury.[16]Several approaches,including electrophysiological tests,neuroimaging,and serum brain-specific biomarkers,have been applied to accurately predict the outcomes of CA survivors.However,the application of these tools is not available during the early hours after ROSC.
Electrolyte disturbances are common in CA survivors.The maintenance of cellular ion homeostasis is achieved by membrane-bound energy-dependent ion pumps.Hypoxic-ischemic injury due to CA leads to cell membrane dysfunction and homeostasis loss.[9]The depletion of highenergy phosphate in the process of ischemia results in failure of the ion pumps that are used to keep ionic gradients across cell membranes.As a result,ion shifts between the compartments of ICF and ECF occur.In the early stage of hypoxia,when there is no inhibition of the sodiumpotassium-adenosine triphosphate (ATP) pump or cell injury,ATP breakdown leads to rapid production of phosphate,and the potassium and magnesium ions in the ICF flow out.This is followed by the inf low of calcium,sodium,and chloride ions in the ECF and a further loss of magnesium and potassium ions in the cytoplasm in accordance with ion pump dysfunction and cell injury.[17]In the irreversiblestage of cell injury,the increased permeability of the cell membrane causes the inf lux of extracellular calcium,and as a result,the damage to the cytoskeleton and mitochondria deteriorates,which finally leads to cell death.[18]
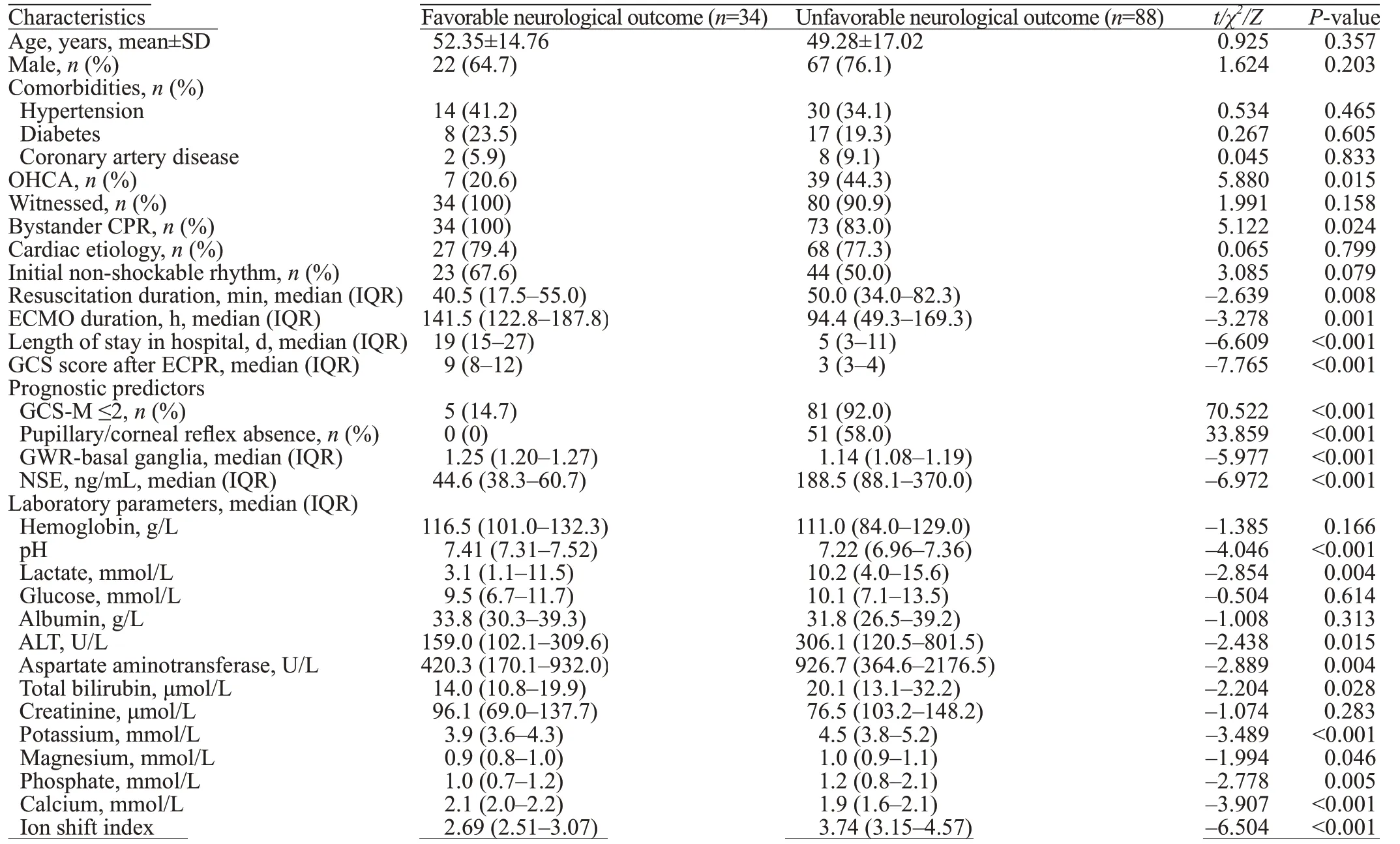
Table 1.Clinical and laboratory characteristics of enrolled patients
Electrolyte levels have been studied as predictors of outcome and cell injury severity.Previous studies demonstrated that mono-electrolyte levels,such as potassium and phosphate,were significantly associated with outcomes among CA survivors.[19]However,because the denominator and numerator in the ratio alter in opposite directions,ISI may be better in reflecting the extent of ion shift after ischemia than a single electrolyte level.In previous studies,it was shown that a higher ISI was related to unfavorable neurological outcomes in CA survivors,[10,17]suggesting that the ISI may be a new alternative choice for assessing prognosis.Similar to those findings,our study demonstrated that the ISI was significantly higher in the unfavorable neurological outcome group than in the favorable outcome group in an ECPR setting.An ISI level >3.12 predicted unfavorable outcome with a sensitivity of 74.6% and a specificity of 85.2%.In addition,the ISI had significantly better prognostic power in the prediction of unfavorable outcome than mono-electrolyte levels,indicating the advantage of ISI as a prognostic indicator compared to a single electrolyte.
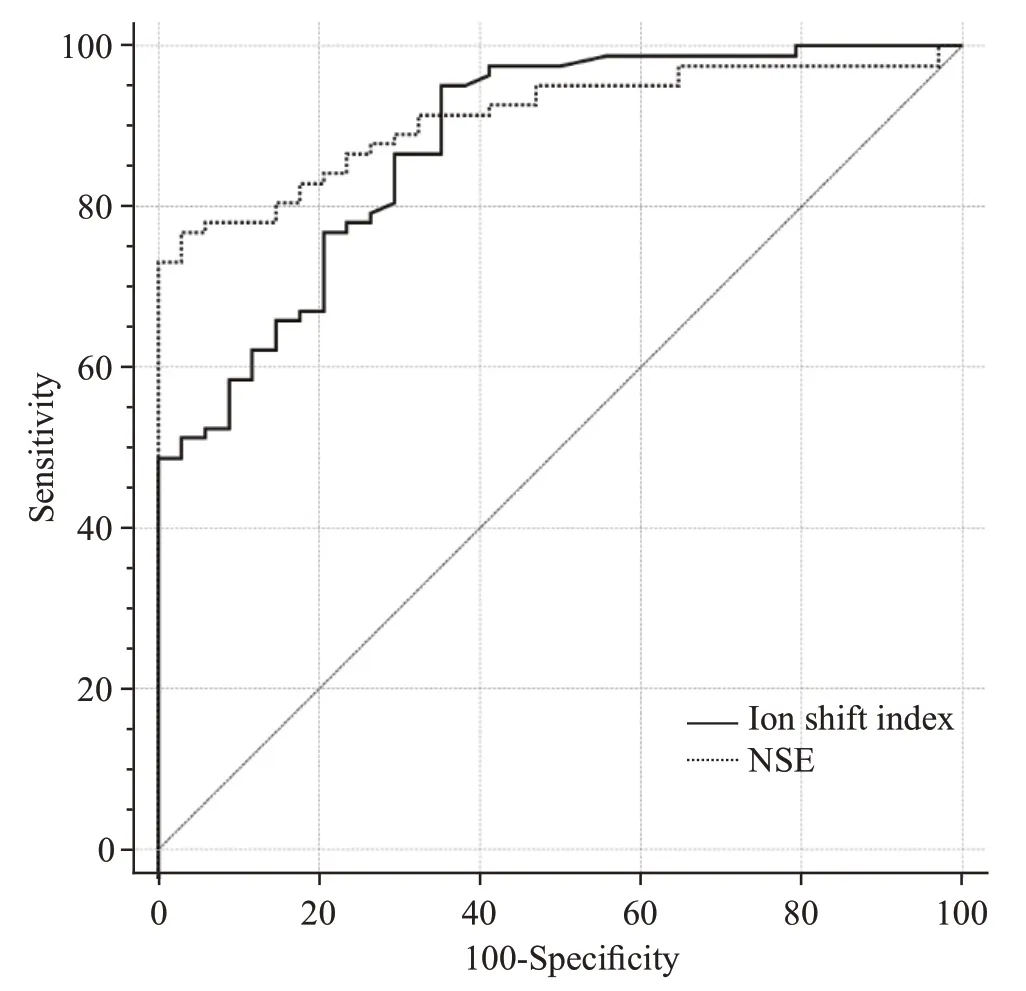
Figure 2.Receiver-operating characteristic curves for the ion shift index and NSE in predicting unfavorable outcome.NSE: neuronspecific enolase.
The levels of lactate have been traditionally chosen as a biomarker of hypoxic-ischemic damage and are a known predictor related to outcomes in CA survivors.[20]In the present study,ISI showed significantly better predictive power than lactate.Furthermore,current guidelines suggest that prognostic predictors,i.e.,reduced GWR on brain CT as well as high values of NSE within 72 h after CA should be applied in predicting unfavorable neurological outcomes.[21]Our study demonstrated that ISI exhibited comparable prognostic performance to GWR and NSE in predicting neurological outcomes at hospital discharge in CA patients following ECPR,indicating that the ISI level could be used as an objective prognostic biomarker that can be available early after ECPR.Apart from that,the calculation of ISI is relatively easy and only needs information on serum levels of electrolytes,which can be promptly determined in most hospital laboratories.
In this study,the multivariate analysis revealed that higher ISI levels were significantly associated with unfavorable outcomes,and the multivariate model involving the ISI and other significant indicators presented an enhanced prognostic performance compared to the ISI alone.These findings suggested a possible role for ISI in conjunction with other predictors instead of ISI alone.ISI could provide additional prognostic information and could be used in combination with other indicators (cl inical examination,neurophysiology,and neuroimaging) to predict outcome after CA.Further studies that combine the ISI with other variables to predict neurological outcomes in CA survivors are needed.
Limitations
There are several limitations in our study.First,this was a retrospective study of ECPR patients from a single center with a relatively small sample size.Some CA variables(witnessed status and initial non-shockable rhythm) showed no significant differences between the two groups.Further prospective multicenter studies are needed to enhance the generalizability of these findings.Second,the serum total calcium level was involved in the ISI calculation,as most of the patients had no available data on ionized calcium levels.It might have some effect on the results since the concentration of total calcium may not precisely embody the physiologic changes after ECPR.Third,the serum electrolyte levels and other prognostic factors were accessible to treating physicians and might have interfered with clinical decision-making,which may possibly result in a self-fulfilling prophecy.Fourth,although this study excluded patients who had pre-existing chronic kidney disease and those who had experienced CA secondary to electrolyte/acid-base disturbances,other medical conditions,such as parathyroid disease and chronic diarrhea,as well as medications,including furosemide and spironolactone,may lead to pre-CA electrolyte derangements and could affect the results.Finally,the endpoint was neurological status at hospital discharge in this study.Longer-term endpoints should be determined for more accurate prediction.
CONCLUSIONS
A higher ISI level was independently related to unfavorable neurological outcome at hospital discharge.ISI in combination with other prognostic indicators could be used as an alternative approach in the prediction of neurological outcomes in CA patients following ECPR.
Funding:This study was supported by the Key Laboratory of Emergency and Trauma (Hainan Medical University),Ministry of Education (KLET-202202).
Ethical approval:The study protocol was approved by the Ethics Committee of the First Affiliated Hospital of Nanjing Medical University (2020-SR-226).
Conflicts of interest:The authors have no conflicts of interest to declare.
Contributors:GNW and ZW contributed equally to this work and share first authorship.GNW and YM proposed and designed the study.YZ,ZMZ and WL analyzed and interpreted the data.GNW and ZW wrote the primary draft of the manuscript.XFC and YM revised the manuscript.All authors read and approved the final version of the manuscript.
杂志排行
World journal of emergency medicine的其它文章
- Emergency department approach to monkeypox
- A prospective cohort study on serum A20 as a prognostic biomarker of aneurysmal subarachnoid hemorrhage
- Mendelian randomization study to investigate the causal relationship between plasma homocysteine and chronic obstructive pulmonary disease
- Cardiopulmonary prognosis of prophylactic endotracheal intubation in patients with upper gastrointestinal bleeding undergoing endoscopy
- Effects of mesencephalic astrocyte-derived neurotrophic factor on sepsis-associated acute kidney injury
- Synchronized ventilation during resuscitation in pigs does not necessitate high inspiratory pressures to provide adequate oxygenation
