Resuscitative endovascular balloon occlusion of the aorta in the treatment of severe hemorrhagic shock caused by upper gastrointestinal bleeding
2023-05-25YulinLiJunyangWangWenHanTaoSunKangLyuShanxiangXu
Yu-lin Li, Jun-yang Wang, Wen Han, Tao Sun, Kang Lyu, Shan-xiang Xu
Department of Emergency Medicine, the Second Affiliated Hospital of Zhejiang University School of Medicine, Hangzhou 310009, China
Hemorrhagic shock is a life-threatening disease often encountered in emergency departments (EDs).Hemorrhagic shock caused by extensive bleeding from multiple sites is often associated with high mortality and morbidity.In recent years, resuscitative endovascular balloon occlusion of the aorta (REBOA) has been widely used in traumatic hemorrhagic shock and is considered to be an effective resuscitation measure.[1]Some studies reported that REBOA was also effective for non-traumatic hemorrhage.[2,3]In this study, we report a case of hemorrhagic shock caused by acute upper gastrointestinal bleeding that was successfully treated and received REBOA to obtain a transition time.This report may provide feasible options for emergency physicians, gastroenterologists, or surgeons to more actively treat refractory gastrointestinal bleeding.
CASE
A 60-year-old male presented to the ED of our hospital complaining of melena for 1 d and had a few years of medication history of oral clopidogrel for treating coronary heart disease.Two weeks ago, the patient underwent duodenoscopic adenoma resection at a local hospital.The adenoma was 1.5 cm in size and was clamped with three titanium clips.There was no obvious postoperative discomfort.One day ago, the patient presented with massive melena, approximately 4,000 mL.He was unconscious, with a Glasgow Coma Scale (GCS) score of 8.In the ED, the patient developed hemorrhagic shock.His blood pressure was maintained at 81/45 mmHg (1 mmHg=0.133 kPa) with norepinephrine(0.45 μg/[kg·min]), and his heart rate was 135 beats/min.Endotracheal intubation was performed for assisted ventilation, and intravenous access was established for fluid resuscitation and transfusion of blood products.Then, the patient received approximately 1,100 mL of crystalline liquid, 1,200 units of prothrombin complex(PC), 400 mL of fresh frozen plasma, 2 units of red blood cells (RBCs), and 4 g of fibrinogen.However, the patient’s blood pressure was difficult to maintain and dropped to 65/42 mmHg, and his heart rate decreased to 65 beats/min (Figure 1).Considering that the situation was critical and the patient could have suffered cardiac arrest,we opted for the immediate use of REBOA.We inserted a 10F Coda balloon catheter (COOK Medical, USA) into the right femoral artery.The catheter was inserted 44 cm using surface positioning.The location of the balloon was confirmed to be in zone I using X-ray, and 8 mL of normal saline was injected into the balloon (Figure 2A).During this procedure, partial blockade was conducted to block the bleeding with an aortic balloon for a total of 71 min.The systolic blood pressure immediately rose to 85 mmHg, and the heart rate was 124 beats/min.One minute later, the systolic blood pressure of the patient was 135 mmHg.Bedside ultrasound was used to assess the blood flow below the balloon occlusion, and a weak pulse was palpable on both sides of the dorsum of the foot.Vasoactive drugs were gradually reduced, and laboratory tests revealed that hemoglobin was 39 g/L and lactic acid was 10.9 mmol/L.The patient was prepared for emergency endoscopy, and digital subtraction angiography (DSA) embolization and exploratory laparotomy were configured.Emergency gastroscopy showed a 1.5-cm rupture at the descending and horizontal parts of the duodenum with active bleeding.After using 5 more titanium clips, the patient’s blood pressure rose significantly, reaching a maximum of 155 mmHg(Figure 2B).The balloon was gradually released, and the patient’s systolic blood pressure decreased to 105 mmHg, then gradually to a minimum of 100 mmHg and remained stable thereafter.Emergency colonoscopy showed numerous dark red blood clots in the colon with no apparent active bleeding.During the whole process,8 units of RBCs, 800 mL of fresh frozen plasma, and a large amount of PC and fibrinogen were infused.

Figure 1.Schematic diagram of the treatment.INN: norepinephrine; REBOA: resuscitative endovascular balloon occlusion of the aorta; PC:prothrombin complex; FIB: fibrinogen; RBC: red blood cells; FFP: fresh frozen plasma.
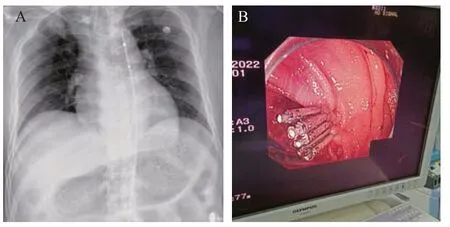
Figure 2.X-rays and DSA images.A: a 10F Coda balloon catheter inserted into the right femoral artery; B: during emergency gastroscopy,5 titanium clips used to stop the bleeding.
After the operation, the patient’s vital signs were stable,endotracheal intubation was removed the next day, and the patient was transferred to the gastroenterology ward.On the 5th day, the patient was discharged after successful resuscitation and treatment.
DISCUSSION
REBOA is an auxiliary measure to temporarily stabilize hemodynamics before carrying out deterministic hemostatic measures during hemorrhagic shock.REBOA is a transitional phase between temporary hemostasis and resuscitation.Although it is able to stabilize hemodynamics and temporarily control bleeding, it also puts the patient at risk for ischemia-reperfusion injury in the lower parts after blockage and restoration of blood flow.REBOA is mainly used in the resuscitation of hemorrhagic shock patients with severe trauma by temporarily controlling bleeding and stabilizing hemodynamics.A few studies have been performed on the application of REBOA in upper gastrointestinal bleeding,but only some related cases have been reported.In a recent case, REBOA was successfully used in a patient with cardiac arrest caused by upper gastrointestinal bleeding.Spontaneous circulation was restored,and hemostasis was successfully achieved by DSA embolization.[4]In a similar case of hemorrhagic cardiac arrest caused by hemorrhagic shock from a bleeding giant gastric ulcer, REBOA temporarily controlled the bleeding and quickly restored spontaneous circulation.As the bleeding could not be stopped endoscopically,emergency surgical exploration was performed to stop the bleeding.A recent retrospective study of REBOA in upper gastrointestinal bleeding showed significant hemodynamic improvement after balloon deployment in zone I in all cases, with a mortality rate of approximately 25%.[5]However, with the prolongation of the blocking time, the ischemia-reperfusion injury of the blocked distal tissue was significantly aggravated.Therefore,it has been proposed that partial balloon occlusion can significantly reduce ischemia-reperfusion injury in distal organs.[6]In a retrospective study of occlusion duration in Japan, 78 patients underwent partial REBOA for 58 min, and 37 patients underwent complete REBOA for 33 min.There was no difference in the 24-hour and 30-day mortality between the complete and partial REBOA groups.[7]This suggests that partial balloon occlusion has very broad clinical application prospects.Another study reported the use of a combination of complete and partial balloon occlusion at zone I of the aorta.[8]The combination of intermittent complete occlusion and partial occlusion has also been reported to have significant hemodynamic advantages in animal studies compared with partial balloon occlusion alone.That is, distal tissue perfusion is significantly more stable, with no difference in mortality and vasoactive drug use.[9]Our case was a patient with upper gastrointestinal bleeding, severe hemorrhagic shock with extremely unstable hemodynamics and critically low heart rate at the time, and impending cardiac arrest.In this case, we chose to implement partial REBOA to keep the cardiac afterload stable,maintain hemodynamic stability, and protect distal organs.This patient suffered no complications related to organ ischemia.Therefore, we performed REBOA in zone I of the aorta, and immediate hemodynamic improvement was observed; the heart rate increased, and cardiac arrest was successfully prevented.Abdominal contrast-enhanced computed tomography could not be performed because of the large amount of blood in his stool, unclear etiology, and hemodynamic instability.Emergency gastroscopy was performed immediately,and considering that the time required for endoscopic treatment and possible exploratory laparotomy may be longer than 30 min, we performed partial occlusion for 71 min.After gastroscopy, there was no distal organ ischemia-reperfusion injury.This suggests that partial balloon occlusion is a promising method of resuscitation for patients with severe hemorrhagic shock caused by upper gastrointestinal bleeding.
This may be the first report of partial balloon occlusion for upper gastrointestinal bleeding and the first time that partial balloon occlusion has been used to prevent cardiac arrest due to severe hemorrhagic shock from upper digestive bleeding.There were no ischemiarelated complications in the intestine and distal limbs reported after partial occlusion for 90 min.
CONCLUSION
REBOA could stabilize the hemodynamics of the patients and prevent cardiac arrest at the time of admission.Similar to traumatic hemorrhage, massive transfusion and partial REBOA might extend the occlusion duration of endoscopic hemostasis.More extensive use of REBOA in severe shock caused by upper gastrointestinal bleeding could be considered.
Funding:The study was supported by a grant from Health Commission of Zhejiang Province “optimization study on partial balloon occlusion of the aorta in traumatic hemorrhagic shock patients (2023KY774)”.
Ethical approval:The study was approved by the Ethics Committee of the Second Affiliated Hospital of Zhejiang University School of Medicine.
Conflicts of interest:The authors declare that there are no Conflicts of interest regarding the publication of this article.
Contributors:LYL and JYW contributed equally to this article.WH, TS, and KL: writing original draft; SXX: review and editing.All authors approved the final version.
杂志排行
World journal of emergency medicine的其它文章
- A 94-year-old patient with severe burns: a case report
- Pregnancy-related spontaneous coronary artery dissection after intravenous ritodrine infusion: a case report
- Twelve family members with tetramine poisoning after consumption of vegetables grown in polluted soils
- A rare case of purulent pericarditis secondary to subdiaphragmatic abscess
- Laryngeal mask airway bougie ultrasonography guided intubation in a morbidly obese patient with difficult airway
- Factors associated with the clinical outcomes of adult cardiac and non-cardiac origin cardiac arrest in emergency departments: a nationwide retrospective cohort study from China