Stomach cancer burden in China: Epidemiology and prevention
2023-05-14XinxinYanLinLeiHeLiMaomaoCaoFanYangSiyiHeShaoliZhangYiTengQianruLiChangfaXiaWanqingChen
Xinxin Yan ,Lin Lei ,He Li ,Maomao Cao ,Fan Yang ,Siyi He ,Shaoli Zhang,Yi Teng,Qianru Li,Changfa Xia,Wanqing Chen
1Office of Cancer Screening,National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital,Chinese Academy of Medical Sciences and Peking Union Medical College,Beijing 100021,China;2Department of Cancer Prevention and Control,Shenzhen Center for Chronic Disease Control,Shenzhen 518020,China
Abstract In 2020,stomach cancer was the fifth most commonly diagnosed cancer and the fourth leading cause of cancerrelated death worldwide.Due to the relatively huge population base and the poor survival rate,stomach cancer is still a threat in China,and accounts for nearly half of the cases worldwide.Fortunately,in China,the incidence and mortality rates of stomach cancer presented a declining trend owing to the change of individual life styles and the persistent efforts to prevent stomach cancer from the governments at all levels.Helicobacter pylori (H.pylori)infection,poor eating habits,smoking,history of gastrointestinal disorders,and family history of stomach cancer are the main risk factors for stomach cancer in China.As a result,by taking risk factors for stomach cancer into account,specific preventive measures,such as eradicating H.pylori and implementing stomach cancer screening projects,should be taken to better prevent and decrease the burden of stomach cancer.
Keywords: Stomach cancer;burden;China;risk factors;prevention
Introduction
Stomach cancer is a multi-step and multi-factorial disease with a complex process of progressive development,which is one of the fatal cancers worldwide.The etiology of stomach cancer is still not entirely clear.Environmental and dietary variables,Helicobacter pylori(H.pylori)infection,heredity,and precancerous state are among the risk factors for stomach cancer.The incidence of stomach cancer differs significantly between genders,age groups,nations or regions,and even periods within the same region(1).Males have a higher incidence and mortality rate for stomach cancer than females,with a male-to-female ratio of about 2:1 (2).Besides,stomach cancer is a serious problem in China,accounting for approximately 50% of all cases of stomach cancer worldwide (1).As a result,we summarize the data on stomach cancer epidemiology,prevention,and control in China in the hopes of providing a reference for stomach cancer strategy planning and aiding in the promotion of cancer control measures in China.
Global epidemiology of stomach cancer
The data on incidence,mortality and survival for the world and countries with a high incidence of stomach cancer are shown inTable 1.It is estimated that 1.1 million new cases of stomach cancer occurred globally in 2020,ranking fifth among all cancer types.The global stomach incidence varies widely,most markedly in Asia (0.8 million).China contributes the most incidence cases of stomach cancer,with 478,000 cases,accounting for 43.9% of all cases worldwide (1).Incidence rates for stomach cancer are two-fold higher for males than females (15.8 per 100,000vs.7.0 per 100,000),which is common all over the world (1,4).
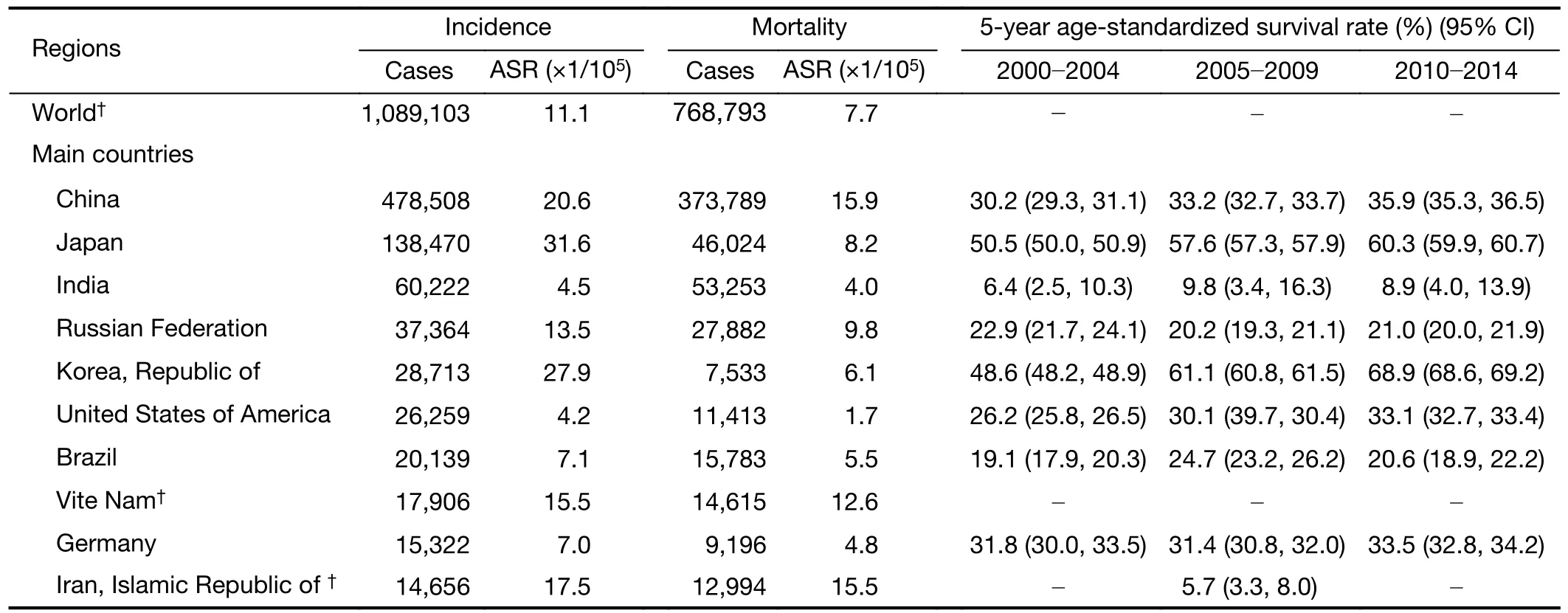
Table 1 Stomach cancer burden comparison by geography (world and main countries) (1,3)
There were about 768,793 deaths caused by stomach cancer internationally in 2020,which accounted for almost 7.7% of total cancer deaths.The global stomach mortality burden is remarkably similar to the incidence,with Asia also contributing the most (1,2).The estimated agestandardized mortality rate for stomach cancer in Asia was more than 5 folds that of Northern America (20.5 per 100,000vs.3.3 per 100,000) (1).Similar to the incidence rate of stomach cancer,the mortality rate of stomach cancer in males is twice that in females (11.0 per 100,000vs.4.9 per 100,000) (1,3),and similar results have also been found from the Global Burden of Diseases study (5).
Stomach cancer age-standardized five-year survival was generally between 20% and 40%,with wide variation globally (5).Survival rates were exceptionally high in Japan(60.3%) and the Republic of Korea (69.0%) in 2010-2014(Table 1).Following 2000,survival rates rose by 5% in Canada,the US,and several developed countries.In addition,5-year survival rates increased by 20% or more in China and the Republic of Korea (3).
Burden and trends of stomach cancer in China
Incidence
According to a study conducted by Zhenget al.,nearly 396,500 (276,300 males,120,200 females) new cases of stomach cancer were diagnosed in 2016 (6),which is the equivalent of more than 1,086 cases diagnosed each day.The overall crude rates and age-standardized rates (ASR) of incidence by the standard Chinese population for stomach cancers were 28.7 per 100,000 and 17.6 per 100,000,respectively (6).The incidence rate of males was 2.5 times higher than that of females (25.1 per 100,000vs.10.3 per 100,000) (6).Cancer incidence rates usually vary distinctly by region as a result of lifestyle diversity or environment.The ASR of stomach cancer incidence was the highest in Northwest China,followed by East and Central China,with South China having the lowest incidence rate (6).The incidence of stomach cancer was higher in rural areas than in urban areas (7) (Table 2).
Mortality
According to Zhenget al.,there were estimated nearly 288,500 death of stomach cancer in 2016 (6).The overall crude rates and age-standardized rates (ASR) of mortality by the standard Chinese population for stomach cancers combined were 20.9 per 100,000 and 12.3 per 100,000,respectively (6).The mortality rate of males was more than twice higher as that of females (17.8 per 100,000vs.7.1 per 100,000) (6).Regional differences in cancer mortality rates were also noticeable.The ASR of mortality stomach cancer combined was the highest in Northwest China,with South China having the lowest incidence rate (6).The mortality of stomach cancer was higher in rural areas than in urban areas (7) (Table 2).
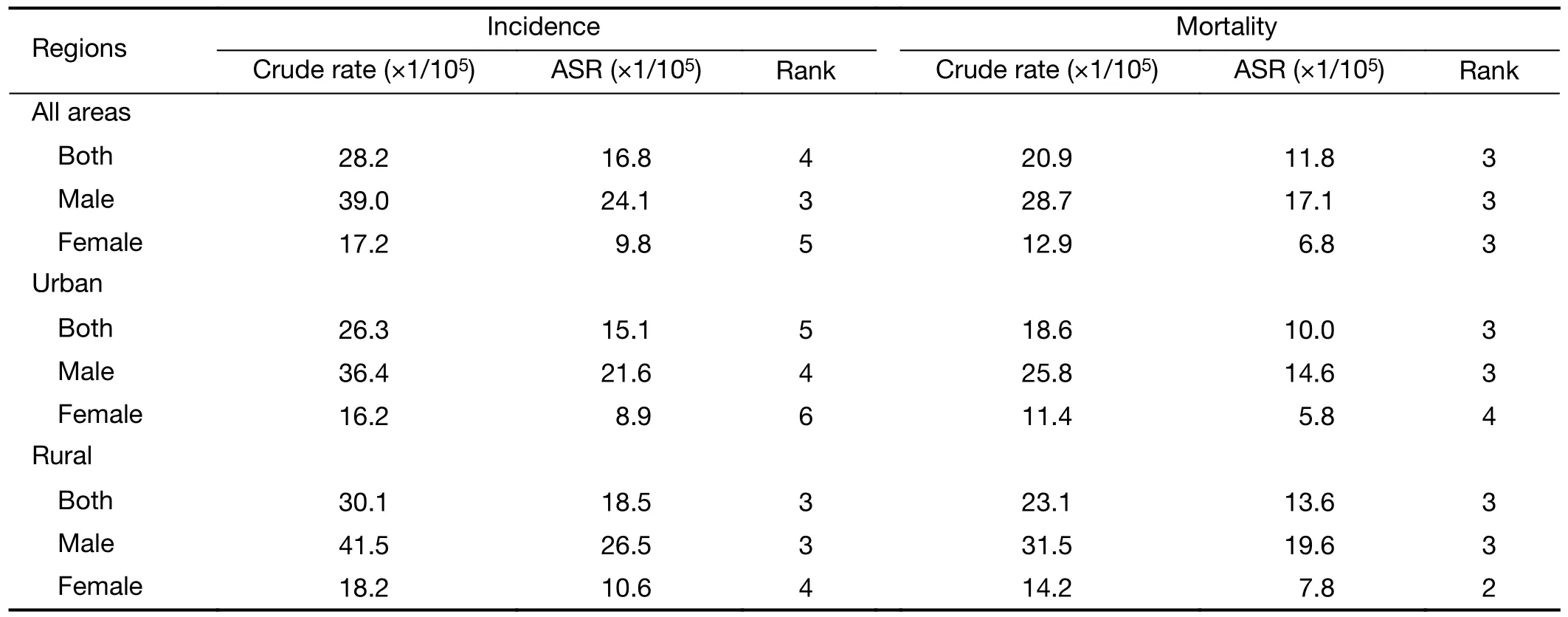
Table 2 Estimated stomach cancer cases,deaths,and corresponding rates by region and sex in China,2016 (7)
Age-specific and region-specific incidence and mortality
Stomach cancer incidence and mortality have a strong relationship with age.The age-specific incidence rate and mortality rate of stomach cancer were low before the age of 40 years,increased after the age of 40 years,and peaked above the age of 80-84 years.The age-specific incidence and mortality rates of males and females were similar to the overall population trend.The highest incidence and mortality rate of stomach cancer among males were 244.2 per 100,000 and 265.8 per 100,000 in age of 80-84 years,respectively,while in females the highest incidence and mortality rates were 122.1 per 100,000 in age of 80-84 years and 117.3 per 100,000 in age of over 85 years,respectively (7) (Figure 1).
Although the age-specific incidence and mortality rate of stomach cancer in urban and rural areas followed a similar trend,the age-specific burden in rural areas was much higher than that in urban areas.Whether in urban or rural regions,the incidence of stomach cancer increased rapidly from age of 55-59 years to peak at age of 80-84 years,and the mortality rate for stomach cancer similarly shows this pattern.In addition,until the age of 55 years,there was no noticeable difference in the incidence and mortality rate of stomach cancer in rural and urban areas,however,after that age,the incidence and mortality burden in the rural population was significantly higher than that in the urban people population (7) (Figure 1).

Figure 1 Age-specific incidence and mortality rates (per 100,000) for stomach cancer by region and sex in China in 2017.(A,B) Age-specific incidence rates in all region,urban and rural (A) and in both,male and female (B);(C,D) Age-specific mortality rates in all region,urban and rural (C) and in both,male and female (D).Data were extracted from the cancer registry annual report 2020 (7).
Trends
According to cancer registry data,the age-standardized incidence rate and mortality of stomach cancer remain decreasing (6).The age-standardized incidence rates of stomach cancer kept decreasing steadily during 2000-2016 in males and females,and the average annual percentage change (AAPC) of males and females were -3.0% [95%confidence interval (95% CI): -3.5%,-2.5%] and -2.9%(95% CI: -3.1%,-2.6%),respectively (6).There was a similar trend in mortality for stomach cancer with -3.4%(95% CI: -4.0%,-2.9%) in males and -4.2% (95% CI:-3.4%,-5.0%) in females (8).The studies based on Global Burden of Disease data similarly found that the incidence and mortality rates of stomach cancer were both decreasing in China (9-11),and the range of stomach cancer mortality dropped from the first to the third during 1990-2015 (10).
5-year survival rate
Zenget al.reported that approximately 35.1% of stomach cancer patients could survive over five years after diagnosis recently,and the male and female survival rates were similar (12).Stomach cancer survival rates have increased in rural region between 2003 and 2015.In 2003-2005,the survival rate in the urban regions was 7.6% higher than that in the rural region,but between 2012 and 2015,the gap shrunk to just 2.5% (12) (Table 3).The 5-year survival rate for those aged 0-64 years old was consistent and similar (>30%);however,it dropped sharply for those over 65 years old (12) .

Table 3 Estimated stomach cancer age-standardized 5-year survival rate by region and sex in China,2003-2015 (12)
Economic burden
The total expense of cancer in 2017 reached 304.8 billion Chinese Yuan (CNY),and the inpatient expense of cancer was 241.9 billion CNY.Inpatient expenses for stomach cancer accounted for a meaningful part of total cancer(about 10%) in 2017.Among all cancers,stomach cancer remained one of the top 3 contributors to cancer inpatient payments during 2008-2017 (from 5.50 billion CNY in 2008 to 23.84 billion CNY in 2017).Notably,after 2013,the pace of growth in hospital costs for stomach cancer began to noticeably slow down.In addition,among all the types of hospitals,inpatient expenses for stomach cancer were the highest for grade 3 general hospitals (13) (Table 4).
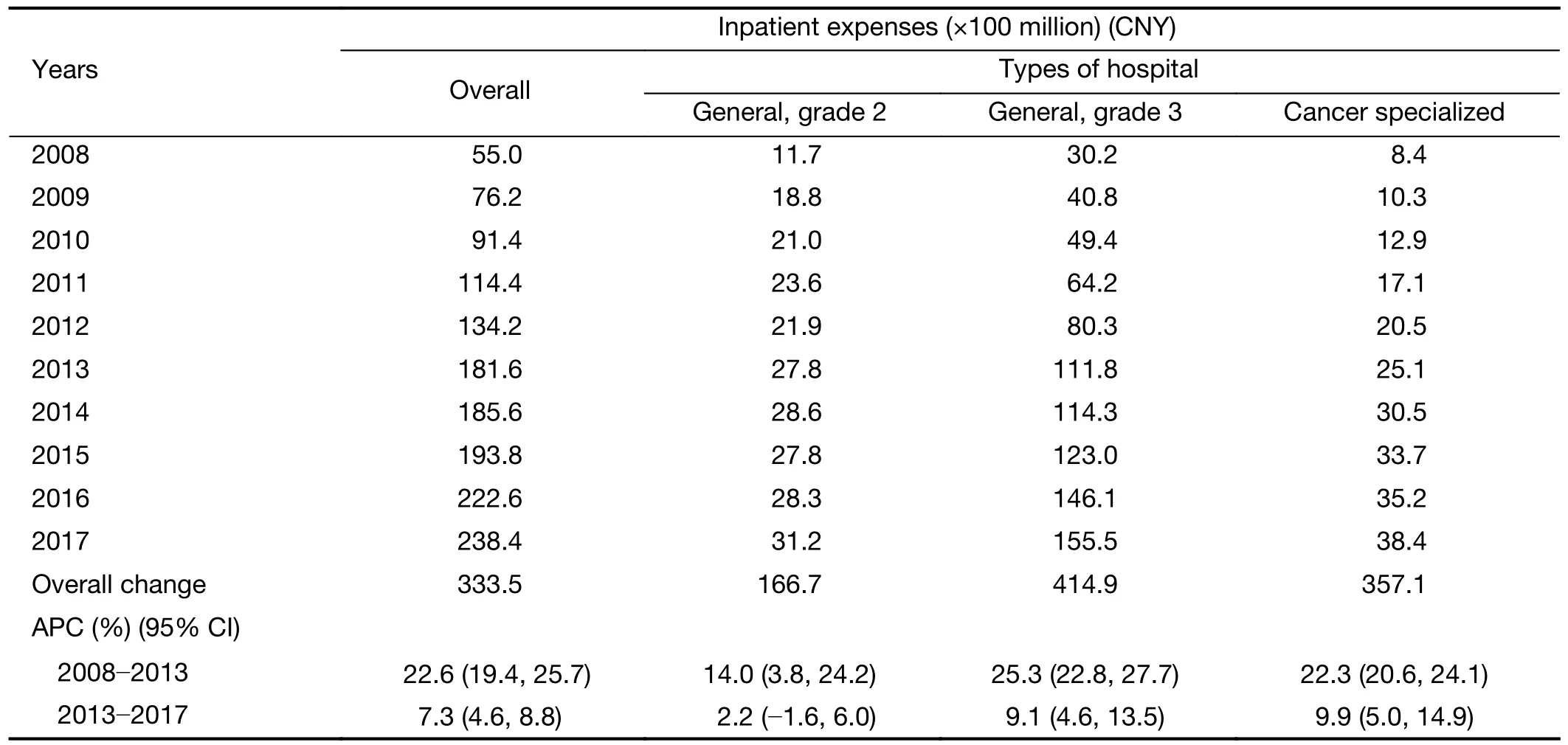
Table 4 Inpatient expenses of stomach cancer overall and by types of hospital in China during 2008-2017 (13)
According to a study on high-risk population by Liet al.,a more detailed direct cost of stomach cancer was reported.For the individuals,the average time cost was 804 U.S.dollars (USD),the average hospitalization cost was 19,876 USD,and the average out-of-pocket hospitalization cost was 10,605 USD.In addition,radiation treatment fees(2,716 USD) and medication fees for chemotherapy (6,518 USD) accounted for the largest overpaying average hospitalization costs per case.Besides,surgical fees for endoscopic treatment and radical resection were 724 USD (14).
Main risk factors of stomach cancer in China
H.pylori infection
H.pyloriis the most important infectious cause of stomach cancer worldwide.Previous studies have demonstrated thatH.pylori,high-risk human papillomavirus,hepatitis B virus,and hepatitis C virus are the four most important infectious pathogens,accounting for more than 90% of infectionrelated cancers globally.Among all these factors,H.pyloriaccounted for 40% (15).Eastern Asia,Latin America,the Middle East,and Eastern Europe are high-risk regions forH.pylori-attributable cancer (15).In China,H.pyloriinfection is a major factor contributing to stomach cancer and the rate ofH.pyloriinfection in China is 40.7%(16,17).A recent case-cohort study on adults aged 30-79 years from China Kadoorie Biobank cohort found thatH.pyloriinfection was responsible for 78.5% of non-cardia gastric cancer and 62.1% of cardia gastric cancer cases (18),and estimated that 74.5% of stomach cancers in China in 2018 were caused byH.pyloriinfection (18,19).Although antibiotics are not targeted drugs eradicatingH.pylori,antibiotics are still the main treatment forH.pylori.In addition,due to regional and population variations,it is crucial to take drug resistance,treatment effectiveness,side effects,and cost into account (20).However,it is gratifying that,in China,Zenget al.achieved a leading position inH.pylorivaccine studies by developing an oral recombinantH.pylorivaccine,which successfully completed the world’s first phase 3 clinical trial ofH.pylori.The study reported that 71.8% (95% CI: 48.2,85.6) of vaccinated subjects were protected againstH.pyloriinfection,indicating that the oral recombinantH.pylorivaccine was effective and safe (21).
Then little Gerda wept hot tears, which fell on his breast, and penetrated7 into his heart, and thawed8 the lump of ice, and washed away the little piece of glass which had stuck there. Then he looked at her, and she sang—
Life style
Abundant evidence has supported the association between stomach cancer and lifestyle risk factors.For example,according to a study based on the China Health and Nutrition Survey (CHNS),the lifestyle risk factors under investigation accounted for 59.8% of stomach cancer cases in China (22).
Dietary and eating habits
High sodium intake has been linked to stomach cancer reported by several studies (23-25).Based on CHNS,Wuet al.discovered that high sodium intake was associated with 16.6% of incident stomach cancers in 2011 (22).A case-control study with participants recruited in Shandong province found that the incidence risk of stomach cancer was 1.8 times [odds ratio (OR)=1.8;95% CI: 1.2,2.2] and 2.5 times (OR=2.5;95% CI: 1.2,3.6) for individuals with a daily salt intake of 3-5 g and more than 5 g than those with salt intakes of less than 3 g per day,respectively (26).According to previously published studies and systematic reviews,red and processed meat consumption may increase stomach cancer risk (27-31).From the Stomach Cancer Pooling (StoP) Project’s findings,an increased risk of stomach cancer was observed for the consumption of red(OR=1.2;95% CI: 1.0,1.5) and processed meat (OR=1.2;95% CI: 1.1,1.4) (32).A study based on CHNS data discovered that 14.1% and 7.7% of stomach cancer were attributable to high red and processed meat consumption,respectively (22).Consumption of pickled food,mold food,fried food and hot food is associated with the risk of stomach cancer (24,31,33).A meta-analysis of the Chinese population found that the risk of stomach cancer with frequent intake of pickled food,fried food,moldy food,and hot food was 2.7 (OR=2.7;95% CI: 2.1,3.5),1.8 (OR=1.8;95% CI: 1.4,2.4),2.6 (OR=2.6;95% CI: 0.9,7.7) and 2.3(OR=2.3;95% CI: 1.8,2.9),respectively (33).
Smoking
Tobacco consumption is one of the main risk factors for many cancer types.China is the largest producer and consumer of tobacco,and China has the world’s largest smoking population (34,35).Smoking is closely related to stomach cancer,and there were significant dose-response relations between stomach cancer,the amount smoked,and the degree of inhalation (31,33,36-39).A secondary analysis of a randomized clinical trial showed that smoking was associated with an increased risk of stomach cancer incidence (multivariable-adjusted OR=1.7;95% CI: 1.0,2.9) and mortality [hazard ratio (HR)=2.0;95% CI: 1.0,4.0] (40).According to a prospective study of 0.5 million adults,the multivariate-adjusted risk ratio (RR) for smokers with stomach cancer in females was 1.2 (95% CI: 0.8,1.8),which was greater in males 1.3 (95% CI: 1.2,1.6) (36).The incidence risk of stomach cancer among smokers who began smoking at age <20 years,20-24 years,and ≥25 years were 1.57,1.39,and 1.15 times higher than that in nonsmokers,respectively (Ptrend=0.0002).And for stomach cancer the RRs were 1.2,1.5 and 1.5 for those who smoked<15,15-24,and ≥25 cigarettes daily (Ptrend=0.0258) (36).
Alcohol consumption
Alcohol consumption is considered one of the risk factors for stomach cancer,but the relationship is not yet clear in China.Wuet al.found that alcohol consumption was attributable to 3.6% of stomach cancer (22).A metaanalysis,including 81 studies (68 case-control studies and 13 cohort studies) found that the combined OR for drinkers with stomach cancervs.non-drinkers was 1.20(95% CI: 1.1,1.3).However,this relationship between alcohol consumption and stomach cancer risk was only presented in case-control studies (OR=1.3;95% CI: 1.1,1.4),not cohort studies (OR=1.0;95% CI: 0.96,1.1) (41).In addition,alcohol consumption was not linked to stomach cancer risk in Chinese prospective cohort studies(40,42).According to a prospective cohort study in Chinese population,alcohol consumption was not a significant risk factor for stomach cancer (OR=1.1;95% CI: 0.7,1.7) (40).
Family history of stomach cancer
A family history of stomach cancer is associated with increased risks of stomach cancer,which has been reported by many studies (29,38,43-45).According to the study by Zhanget al.,stomach cancer risk increased in first-degree relatives with a history of stomach cancer (OR=4.3;95%CI: 1.7,11.1) in urban populations in China (38).A casecontrol study in areas of high-risk stomach cancer in China,found that individuals with a family history of gastric cancer had a higher risk of stomach cancer than those without a family history (OR=1.3;95% CI: 1.1,2.0) (44).A study based on Linxian general population reported that participants with a cancer family history had a 27% higher risk of stomach cancer incidence (HR=1.3;95% CI: 1.2,1.4],as well as a 26% higher risk of stomach cancer mortality (HR=1.3;95% CI: 1.1,1.4) compared with those without a family history (45).
Prevention and control for stomach cancer in China
Primary prevention
Primary prevention of stomach cancer refers to taking measures to reduce the exposure to risk factors by considering the etiology of stomach cancer with the aim of reducing the incidence and mortality of stomach cancer.It aims to reduce the incidence of stomach cancer.Stomach cancer is a type of cancer that develops over a number of stages under the influence of several factors.The important causes of stomach cancer includeH.pylori,poor lifestyle choices,and nutritional variables (16,46).
H.pylori eradication
Global consensus that treatment and eradication ofH.pyloriinfection can prevent the development of stomach cancer (21,47-50).In the Chinese consensus on the eradication ofH.pyloriand the prevention and control of stomach cancer (2019,Shanghai),the key points of view are consistent with international consensus,highlighting thatH.pyloriinfection is the leading cause of stomach cancer in China and that eradicatingH.pylorican reduce the incidence of stomach cancer in China.The consensus clearly definedH.pylorieradication as a primary prevention measurement for stomach cancer,which has a significant role in boosting the prevention of stomach cancer in China(16).In Chinese population,eradicatingH.pylorican prevent stomach cancer,and the preventive effect is closely associated with the length of follow-up.In 1995,a field intervention study in Linqu (Shandong province),a highrisk region of stomach cancer,first reported that eradicatingH.pyloricould markedly reduce the incidence of stomach cancer,and the incidence rate of stomach cancer decreased by 29%-52% after 8-22 years of followup (51).Relative studies on health economics indicated that the screening strategy withH.pylorieradication was proved cheaper and more effective than conventional strategies withoutH.pylorieradication in preventing stomach cancer in the Chinese population.(52).A study based on the Markov model found that the incidence of stomach cancer could be reduced by 35.5% from 2020 to 2035 throughH.pylorieradication among the general population in China(53).Moreover,H.pylorieradication would provide a longterm positive impact on the prevention and treatment of gastrointestinal illnesses such as peptic ulcer disease and non-ulcer dyspepsia (21).In addition,medical research institutions have made progress in developing the vaccine againstH.pylori.In 2009,China took the lead in the world to successfully develop an oral recombinantH.pylorivaccine with fully independent intellectual property rights,and the launch of the vaccine will be of great significance in reducing the prevalence ofH.pyloriinfection (20).
In China,the prevalence ofH.pyloriinfection has been decreasing in recent years (17),which may be attributed to the implementation of several policies.National and local media at all levels have actively publicized healthy policy documents such as the Health Literacy of Chinese Citizens-Basic Knowledge and Skills (54).And the key points of cancer prevention and treatment are popularized in the national anti-cancer week,which is held every year throughout the country to guide the public to establish the correct health concept and raise the awareness of stomach cancer prevention and control in the whole society.In addition,the Chinese Consensus on Family Based-H.PyloriInfection Control and Management for the first time proposed the prevention and control ofH.pyloriinfection by families,which will play an active and important role in reducing the spread ofH.pyloriin China (55).
Life style
Lifestyle changes reduce the incidence of stomach cancer radically.Since the official implementation of the Framework Convention on Tobacco Control in China in 2006,China has introduced some tobacco control policies one after another,and the smoking rate in China has decreased significantly.The China Reported Health Hazards of Smoking 2020 pointed out that the smoking rate of people aged 15 years and above in China was 26.6%in 2018,with a smoking rate of 50.5% for males and 2.1%for females (56).In addition,China has taken measures to improve high salt eating habits.The Healthy China Action(2019-2030) clearly states that the daily salt intake for each person should not be more than 5 g.The results of the nutrition and chronic diseases status of Chinese residents surveillance show that the health awareness of Chinese residents has gradually increased.In 2020,Chinese household salt reduction policy has shown some success.The daily cooking salt for each person is 9.3 g,a decrease of 1.2 g compared to 2015 (57).
Secondary prevention
Since various risk factors are associated with stomach cancer development,it is challenging to reduce the cancer burden by primary prevention only.Comparatively,secondary prevention for high-risk population has become an effective means of stomach cancer prevention and control,which is a key measure to reduce its mortality and long-term incidence.Secondary prevention of stomach cancer refers to early detection,early diagnosis and early treatment through screening or physical examination.
Stomach cancer screening
Many epidemiological studies have shown that screening for stomach cancer could effectively decrease cancer incidence and mortality through enabling early detection and treatment in at-risk populations.Stomach cancer screening and early diagnosis and treatment are secondary measures of cancer prevention and the primary focus of the current prevention of stomach cancer worldwide (58).In 1983 and 2002,Japan and South Korea,two countries with the highest burden of stomach cancer,conducted national stomach cancer programs (59,60).In order to effectively promote stomach cancer screening in China,a number of early diagnosis and treatment programs for stomach cancer have been carried out since 2005,with the support of the central government.The existing population screening programs in China include the Cancer Screening Program in Rural Areas initiated in 2005,the Cancer Screening Program in Huaihe River Areas in 2007,and the Cancer Screening Program in Urban Areas in 2012 (61).In addition to national stomach cancer screening programs,local governments and research institutions at all levels have launched various stomach cancer screening programs,such as the Gastrointestinal Cancer Center program initiated by the National Center for Clinical Research in Digestive Diseases,the National Center for Quality Control of Gastrointestinal Endoscopy and other institutions.These measures have been effective in improving the early diagnosis and survival rate of stomach cancer in China.
The current national screening programs for stomach cancer in China basically follow a modified high-risk population strategy,focusing on individuals aged 40-74 years (aged 40-69 years in rural areas and aged 45-74 years in urban areas).Then the high-risk individuals were screened by gastroscope.In a systematic review and metaanalysis of Asian countries,endoscopic screening may reduce the risk of death from stomach cancer (62).In China,stomach screening has been shown to effectively decrease the incidence of and mortality (8,63).According to Chenet al.,a recent large,multi-center populationbased study reported that the one-time endoscopic screening was effective in the prevention of upper gastrointestinal cancer in individuals aged 40-69 years in high-risk region in China,with 34% reduction in incidence and 62% reduction in mortality for non-cardia stomach cancer in the screened group compared with the control group (8).In addition,several Markov model studies showed that endoscopic screening for stomach cancer was cost-effective,with start age of 40 or 45 years in China(53,64).However,more prospective research and health economic studies are required to assist decision-makers in the specific start and stop age and interval of stomach cancer screening in China,and so that government may effectively support stomach cancer preventive and control programs.
Conclusions
Current epidemiological data indicate that stomach cancer remains the major factor threatening health in China.However,stomach cancer could be effectively avoided by taking primary prevention measures,such as eradicatingH.pylori,and secondary prevention measures,such as cancer screening.Given the large population of stomach cancer patients in China,the intervention against stomach cancer through primary and secondary prevention modalities,together with policies and governmental financial assistance,should continue to be emphasized and encouraged.
Acknowledgements
This study was supported by the National Natural Science Foundation of China (No.81974492);the National Natural Science Foundation of China (No.82273721) and the Sanming project of Medicine in Shenzhen (No.SZSM201911015).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
杂志排行
Chinese Journal of Cancer Research的其它文章
- When immunotherapy meets liver transplantation for hepatocellular carcinoma: A bumpy but promising road
- Transforming cancer cells for long-term living with cancer:An inspiring new approach
- Integrated strategies for chemotherapy cycles in nasopharyngeal carcinoma patients: Real-world data from two epidemic centers guiding decision-making
- Variant rs8400 enhances ALKBH5 expression through disrupting miR-186 binding and promotes neuroblastoma progression
- Exploration and optimization of surgical techniques for laparoscopic transhiatal lower mediastinal lymph node dissection for adenocarcinoma of esophagogastric junction: A prospective IDEAL 2a study with qualitative design
- Aqueous-soluble components of sporoderm-removed Ganoderma lucidum spore powder promote ferroptosis in oral squamous cell carcinoma