Successful treatment of acute carotid artery injuries
2023-02-07YifengPanZhenjieLiuLibinZhangZhiweiGaoBingChen
Yi-feng Pan, Zhen-jie Liu, Li-bin Zhang, Zhi-wei Gao, Bing Chen
Department of Vascular Surgery, the Second Affiliated Hospital of Zhejiang University School of Medicine, Hangzhou 310009, China
Vascular injuries can lead to severe consequences, and in particular, carotid artery injury caused by combat, traffic accidents or other external forces is extremely harmful. As the neck has a complex anatomical structure and a relatively small local space, carotid artery injury is usually complicated by neural and spinal injuries, presenting challenges during emergency rescue. The hazards of carotid artery injury, in addition to shock and death induced by acute blood loss, include overlong cerebral ischemia due to trauma-induced thrombus detachment or vascular occlusion, and patients may have serious nerve damage after life-saving measures, thus affecting their quality of life. Hence, timely and effective treatment are key factors associated with the prognosis of patients. In this study, 7 patients with carotid artery injury were enrolled for a retrospective analysis, and the diagnosis and treatment experience was summarized.
METHODS
The ethics committee of our institution granted ethics approval of this study and waived the requirement for written informed consent. In total, 7 consecutive confirmed carotid injury patients who were treated with surgery at our department between January 2015 and January 2021 were enrolled. There were 5 males and 2 females, with a median age of 48.8 years.
The data collected included age, sex, causes of injury, brief medical history, duration of intensive care, antiplatelet therapy, and National Institutes of Health Stroke Scale (NIHSS) score.
RESULTS
Among the 7 patients, 5 patients had common carotid artery injuries, one internal carotid artery injury, and one external carotid artery injury. There were 5 cases caused by traffic accidents or sharp instruments and 2 cases of iatrogenic carotid artery injury. The average duration from injury to hospital admission was 9.4 (3-24) h, and 3 patients were transferred to our hospital after tracheal intubation. Six patients had relatively stable hemodynamics and underwent necessary imaging examinations preoperatively. One patient was directly transferred to the operating room for exploration of hemorrhagic shock (Table 1).

Table 1. Demographics, treatment, and outcome of patients with carotid artery injury
Patient 1 had a traffic-accident-induced open injury at the junction of the right root of the neck and chest wall (zone I and zone II). The patient’s vital signs were stable. Computed tomographic angiography (CTA) showed right common carotid artery occlusion and multiple vertebral fractures. Hybrid surgery was performed: (1) cerebral angiography assessed the right common carotid artery occlusion, intracranial circulation, circle of Willis, and posterior circulation condition; (2) intraoperative exploration revealed acute thrombosis and intimalrupture at the bifurcation of the internal and external carotid arteries, and we re-constructed the common and internal carotid arteries with the autogenous saphenous vein via interposition bypass. Finally, the carotid artery was re-examined by CTA after surgery (Figure 1).
Patient 2, with a sharp-instrument-induced carotid artery rupture at zone II, was in hemorrhagic shock and transferred to the hospital with tracheal intubation and compression of the wound. Emergency exploratory surgery revealed a knife incision proximal to the left internal carotid artery and a dissected internal jugular vein. The internal carotid artery and internal jugular vein were repaired at the first stage since an arteriovenous fistula had formed during compression (supplementary Figure 1).
Patient 3 experienced a knife stab injury in the right retroauricular mastoid region (zone III). Massive hematomas at the cranial base and posterior pharyngeal wall, extending toward the mediastinum along the posterior pharyngeal wall, resulted in severe deviation of the trachea. Tracheal intubation and wound hemostasis were performed outside the hospital. The patient underwent hybrid surgery in the emergency department: (1) the vascular integrity and the rupture and bleeding site were assessed with digital subtraction angiography (DSA); (2) covered stents were implanted into the common and internal carotid arteries to ensure the intracranial blood supply and to block external carotid artery bleeding; (3) the superficial temporal artery, occipital artery, facial artery, and internal jugular vein were ligated separately through the anterior edge of the sternocleidomastoid muscle, followed by one-stage debridement of the neck hematoma to relieve airway compression (supplementary Figure 2).
Four patients underwent endovascular treatment. Specifically, two patients experienced iatrogenic common carotid artery injury during internal jugular vein catheterization (supplementary Figures 3 and 4). Two traffic-accident patients had blunt injuries of the common carotid artery complicated with pseudoaneurysm. All injuries were located in zone I; the covered stents were implemented to repair the common carotid artery injury (supplementary Figures 5 and 6).
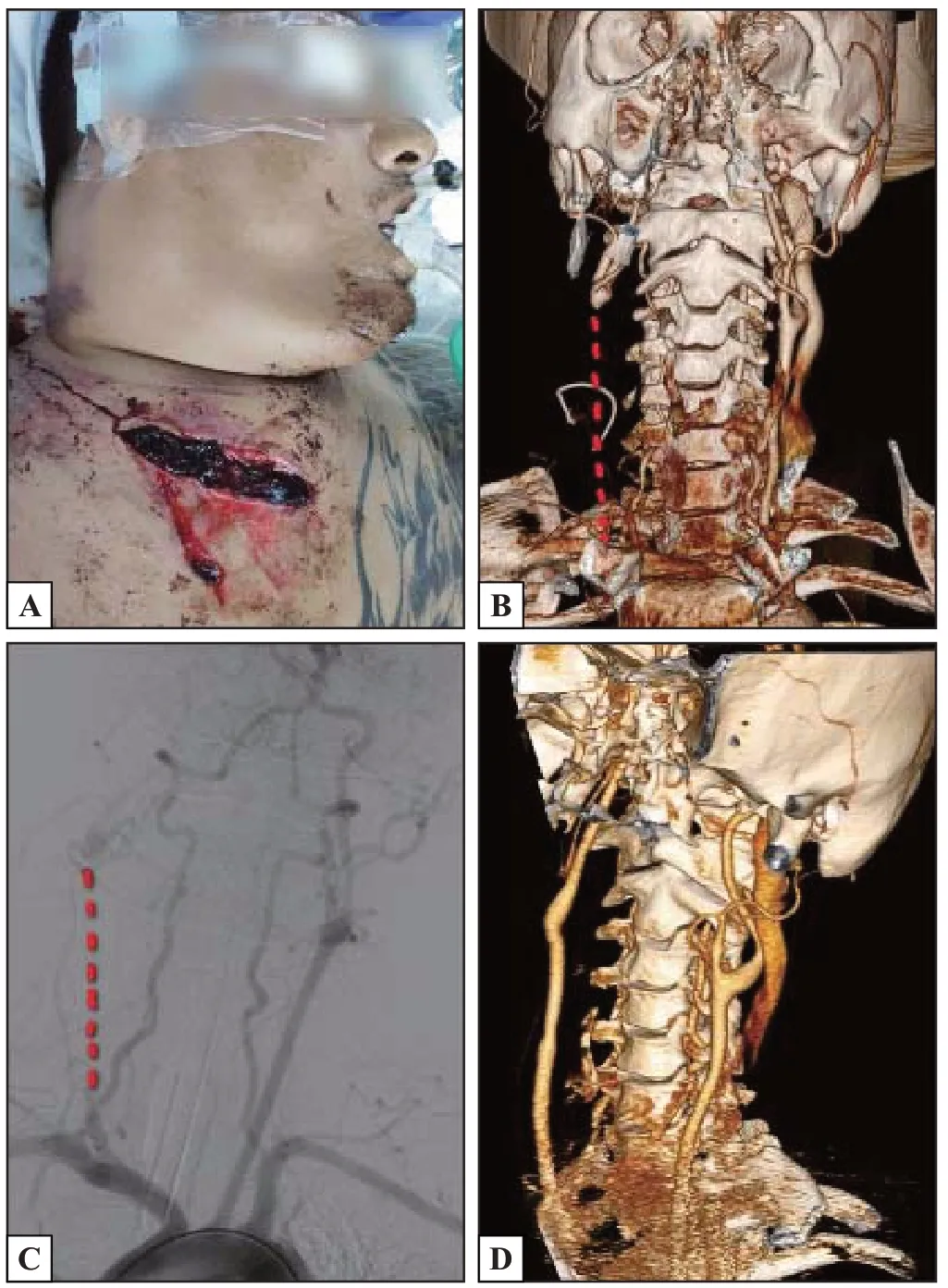
Figure 1. Clinical images of the patient 1. A: open injury at the junction of the right root of the neck and the chest wall; B and C: right common carotid artery occlusion by CTA and DSA; D: reconstruction of the right common and internal carotid arteries with the autogenous saphenous vein. CTA: computed tomographic angiography; DSA: digital subtraction angiography.
All patients received oral antiplatelet drugs (aspirin 100 mg/d, with/without clopidogrel 75 mg/d) after surgery.
All patients were successfully rescued, without perioperative mortality, hemiplegia or aphasia. Among them, 1 patient presented with an open injury at the right chest wall complicated by a brachial plexus injury, in addition to carotid artery injury. Two patients with open injuries involving the neck exhibited postoperative hoarseness, most likely attributed to injuries to the glossopharyngeal and hypoglossal nerves due to hematoma compression and trauma. The hoarseness resolved after a 12-month follow-up, without other residual neurological symptoms.
DISCUSSION
Carotid artery injuries can be divided into closed injuries and open injuries. Open injuries are at higher risk because: (1) active bleeding causes cervical hematoma to compress the airway, resulting in asphyxia and cerebral ischemia; and (2) open injuries are always associated with injuries of peripheral veins, airways, or nerves. In addition, the mortality rate for open injuries is up to 33%.[1]P revious experience indicates that surgical exploration is preferred for open injuries involving the carotid artery. However, surgical exploration showed limited clinical benefit and many related complications. According to the current consensus, the emergency surgical indications of carotid artery trauma are active hemorrhage, progressive hematoma, hemorrhagic shock, severe subcutaneous emphysema, and airway compression.[2-5]Generally, patients with stable hemodynamics receive a preoperative evaluation, including vital signs, physical examination of the nervous system, carotid artery ultrasound, and CTA, to determine the location and extent of carotid artery injury, intracranial blood supply and whether it is accompanied by spinal, tracheal, or esophageal injuries.
For patients whose nervous system is not assessable, preoperative imaging examinations are especially important. Ultrasonographic assessments for the carotid artery have limited reliability since they are only applied to zone II neck injuries and are influenced by dressings or hematomas. CTA of the carotid artery is with 90% sensitivity and 100% specificity in diagnosing penetrating carotid artery injury, and it is also valuable for the diagnosis of complicated fractures of the skull base or maxillofacial bone.[6]A s an invasive examination, carotid artery DSA is an irreplaceable method for carotid artery injury; its detection rate is higher than that of CTA for blunt carotid artery injury. S uperselective angiography of the carotid artery can clarify an injury form and identify the bleeding site and neighboring artery injuries; the bleeding can be endovascular balloon occlusion or vascular embolization if necessary. Additionally, superselective angiography rapidly assesses the compensation of the contralateral carotid and bilateral vertebrobasilar arteries for the injured side for decisionmaking regarding the placement of a carotid artery shunt for the reconstruction of the injured carotid artery. Such methods are especially critical for some patients whose preoperative CTA of the carotid artery cannot be utilized.
The neck comprises three zones: zone I (from the clavicle to the cricoid cartilage), zone II (from the cricoid cartilage to the submandibular triangle), and zone III (from the region above the angle of mandible to the cranial base). Injuries in different zones should be treated based on v arying principles.[7]For example, a zone II carotid artery injury can be quickly exposed via neck dissection; therefore, surgical exploration and repair are usually recommended. With regard to zone I and zone III carotid artery injuries, the proximal and distal blood vessels are hard to dissect and expose; injury sites can only be exposed using median sternotomy or mandibular subluxation, which are fairly intractable. Hence, carotid artery injuries in these two zones are more frequently treated via endovascular surgery or a hybrid surgery that combines endovascular surgery with open surgery. Recently, some scholars have proposed treatment principles for carotid artery injuries based on the “TOPIC” classification; that is, carotid artery injuries are classified in detail based on the time window, openness, injury site, injury degree, cerebral blood supply, and neurologic function, serving as the basis for diversified treatments.[8]
C oncerning appropriate drug treatment for spontaneous carotid dissection, anticoagulation or antiplatelet therapy should be started in time to prevent further thromboembolic events.[9,10]These two types of drugs show similar efficacy in reducing nervous dysfunction without increasing the risk of stroke.[11,12]However, traumatic cases need to take a more interdisciplinary approach and specific considerations regarding treatment. Patients’ risks, complications, and injuries should be considered for drug therapy. In the present study, 5 patients with carotid artery reconstruction, whether using a covered stent or autologous vein or carotid artery repair, were treated with anticoagulation combined with antiplatelet therapy. Two patients did not receive anticoagulation therapy for combined injuries with a high risk of bleeding.
Carotid artery injury is a critical condition that progresses rapidly and is refractory to treatment; therefore, such injuries often result in death or serious complications if not treated properly in a timely manner. For such patients, the specific cause of injury should be investigated, and the severity of injury, both systemic and local, should be evaluated quickly. Moreover, imaging examinations, e.g., carotid artery ultrasound and CTA, should be conducted when possible to further determine the severity of the injury and the presence or absence of comorbid injuries. F or patients with unstable vital signs, emergent surgical exploration should be employed. Hybrid surgery can be employed to define the injury site and intracranial blood supply and to quickly control bleeding and recover cerebral blood supply, providing certain advantages in the treatment of complicated carotid artery injuries.
Funding:None
Ethical approval:This study was approved by the Ethics Committee of the Second Affiliated Hospital of Zhejiang University School of Medicine. Written informed consent from patients was waived because of the retrospective design and the anonymous nature of data collection.
Confl icts of interest:The authors have no confl icts of interest to declare that are relevant to the content of this article.
Contributors:YFP collected the patient’s clinical data and wrote the paper. ZWG and BC contributed equally to this study. All authors have read and approved the manuscript.
All the supplementary files in this paper are available at http://wjem.com.cn.
杂志排行
World journal of emergency medicine的其它文章
- Patient care during interfacility transport: a narrative review of managing diverse disease states
- Endothelial cell metabolism in sepsis
- Nutritional status and prognostic factors for mortality in patients admitted to emergency department observation units: a national multi-center study in China
- Prolonged dual antiplatelet therapy after drug-eluting stent implantation improves long-term prognosis for acute coronary syndrome: five-year results from a large cohort study
- Efficacy and safety of remimazolam-based sedation for intensive care unit patients undergoing upper gastrointestinal endoscopy: a cohort study
- Glutamine supplementation attenuates intestinal apoptosis by inducing heat shock protein 70 in heatstroke rats
