Acute kidney injury due to bilateral malignant ureteral obstruction: Is there an optimal mode of drainage?
2023-01-08RabeaAhmedGadelkareemAhmedMahmoudAbdelraoufAhmedMohammedElTaherAbdelfattahIbrahimAhmed
Rabea Ahmed Gadelkareem,Ahmed Mahmoud Abdelraouf,Ahmed Mohammed El-Taher,Abdelfattah Ibrahim Ahmed
Abstract There is a well-known relationship between malignancy and impairment of kidney functions,either in the form of acute kidney injury or chronic kidney disease.In the former,however,bilateral malignant ureteral obstruction is a surgically correctable factor of this complex pathology.It warrants urgent drainage of the kidneys in emergency settings.However,there are multiple controversies and debates about the optimal mode of drainage of the bilaterally obstructed kidneys in these patients.This review addressed most of the concerns and provided a comprehensive presentation of this topic from the recent literature.Also,we provided different perspectives on the management of the bilateral obstructed kidneys due to malignancy.Despite the frequent trials for improving the success rates and functions of ureteral stents,placement of a percutaneous nephrostomy tube remains the most recommended tool of drainage due to bilateral ureteral obstruction,especially in patients with advanced malignancy.However,the disturbance of the quality of life of those patients remains a major unresolved concern.Beside the unfavorable prognostic potential of the underlying malignancy and the various risk stratification models that have been proposed,the response of the kidney to initial drainage can be anticipated and evaluated by multiple renal prognostic factors,including increased urine output,serum creatinine trajectory,and time-to-nadir serum creatinine after drainage.
Key Words: Acute kidney injury;Kidney;Malignancy;Percutaneous nephrostomy;Ureteral obstruction;Ureter
INTRODUCTION
Acute kidney injury (AKI) is defined as an increase in serum creatinine (SCr) of ≥ 0.3 mg/dL (≥ 26.5 μmol/l) within 48 h or ≥ 1.5 times from the baseline within 7 d[1,2].Classically,this biochemical definition is practically translated into a rapid deterioration of kidney functions within hours or days.It is a reversible pathology when properly managed in a timely manner.According to the positional relationship between the original pathology and the kidney of the affected patient,AKI has classically been classified into prerenal (hypovolemic),renal (intrinsic),and postrenal (obstructive;Po-AKI) AKI[2-4].The latter class represents a urological emergency when the patient presents with disturbed kidney functions,such as an elevated SCr level.The underlying pathology of Po-AKI is the obstruction of the two kidneys or one kidney in patients with a solitary functioning kidney.
The obstruction can occur at any point along the course of the ureters.This obstruction can be caused by either benign causes such as urolithiasis or malignant causes such as bladder cancer.Kidney obstruction with elevated function warrants drainage of the kidneys as fast as possible.Methods of drainage include placement of ureteral stents or percutaneous nephrostomy (PCN) tubes.Currently,there has been no consensus on the optimal mode of drainage (method and laterality) in these cases[5,6].Malignant ureteral obstruction (MUO) represents a more complex entity than the benign ureteral obstruction (BUO) in the field of AKI because the former has a mechanical factor (the obstruction) and a metabolic factor (the malignancy).
These variables have generated many controversies on the different aspects of the management of patients with AKI due to malignant bilaterally obstructed kidneys (BOKs).They may affect the decisionmaking for the mode of drainage,uncertainty of renal responses after drainage,benefits in the management of the underlying disease,and effects on patient quality of life (QoL) with the different methods of drainage[6-8].In this commentary review,we addressed these different aspects in patients with Po-AKI due to MUO.The relevant recent literature from the last two decades was reviewed for the available approaches of drainage of BOKs in patients with MUO.The scope of the review was to clarify the efficiency of these approaches and the differences and similarities between them.
DESCRIPTION OF SUMMARIZED LITERATURE
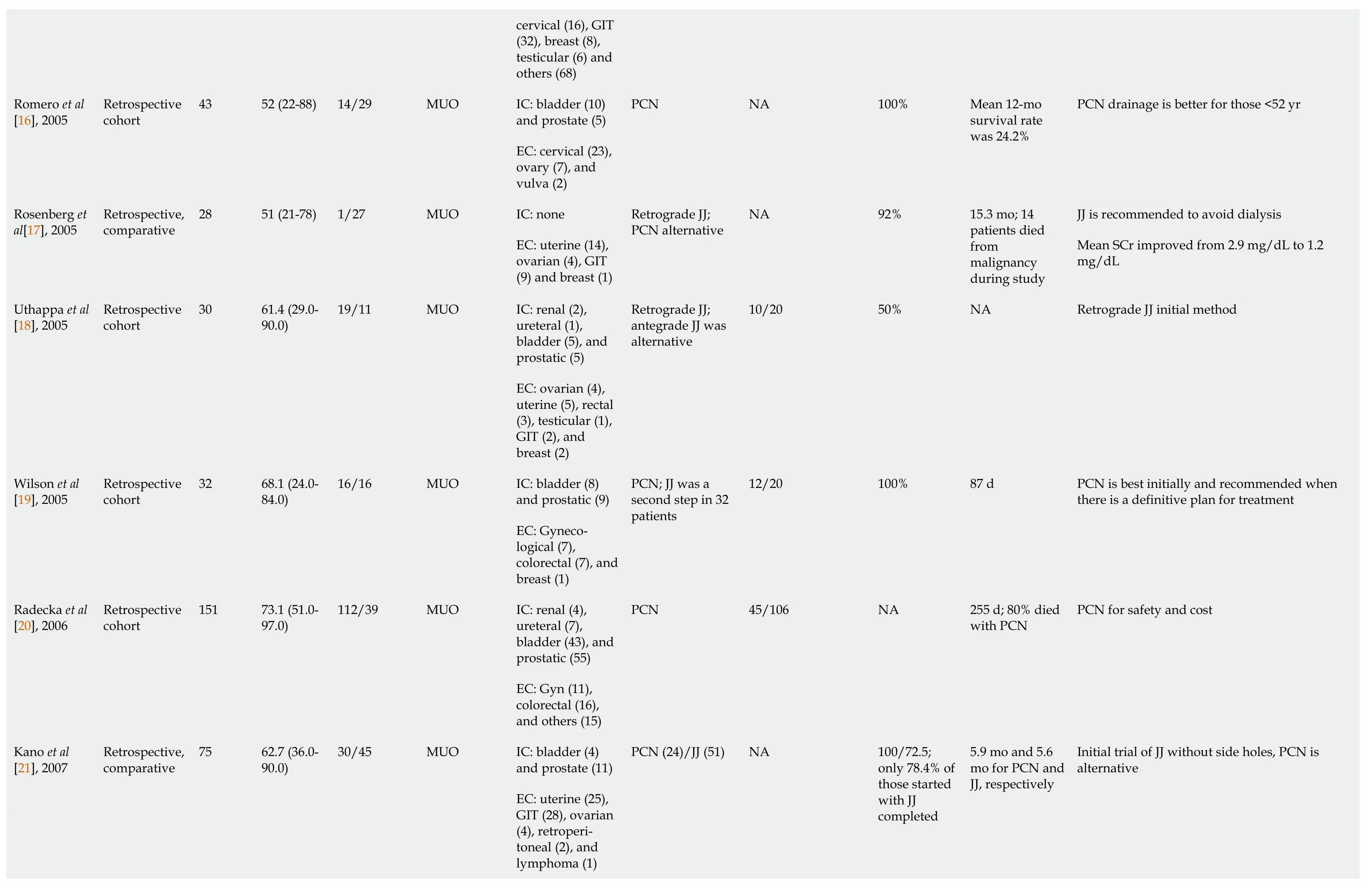
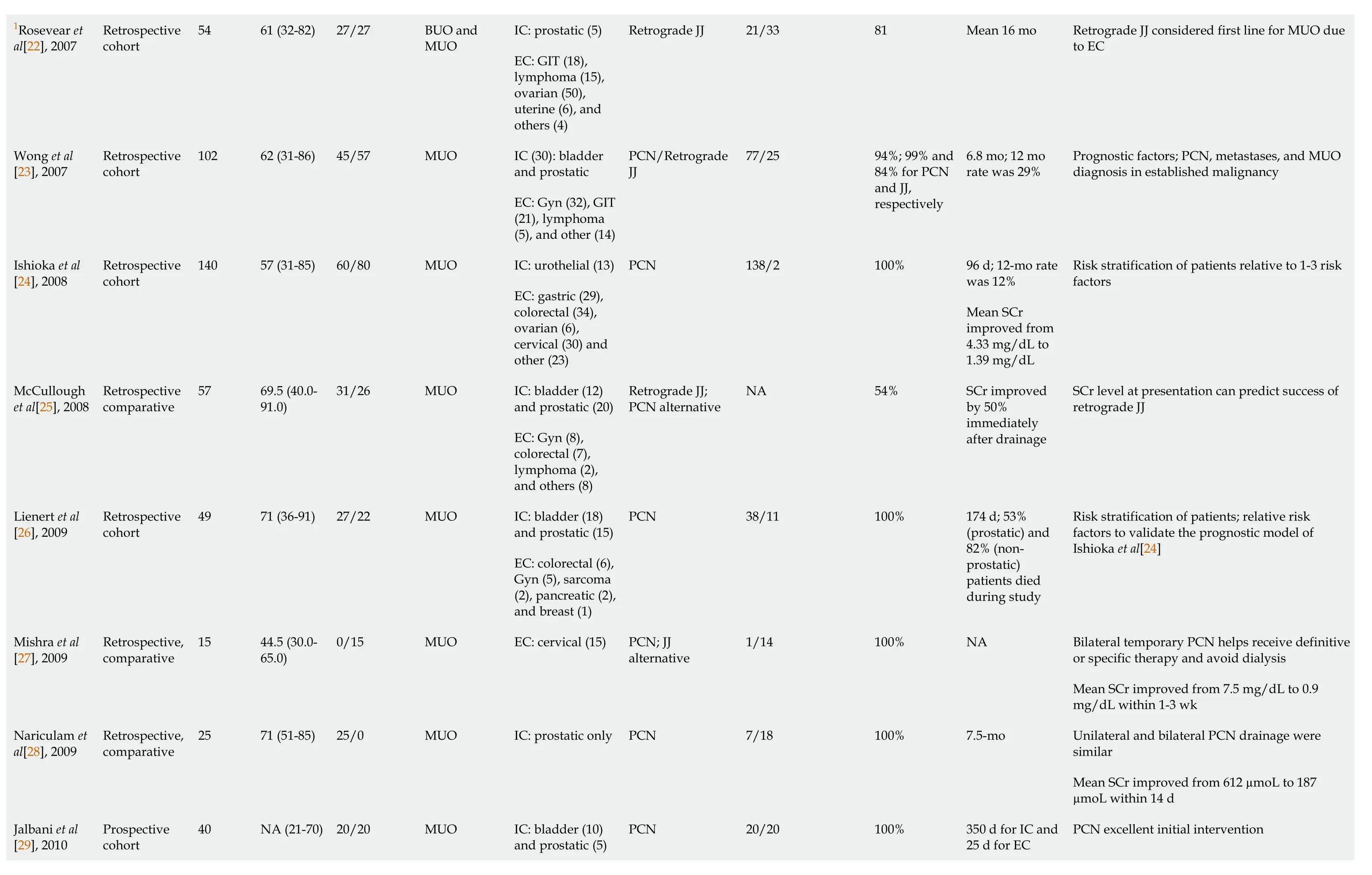
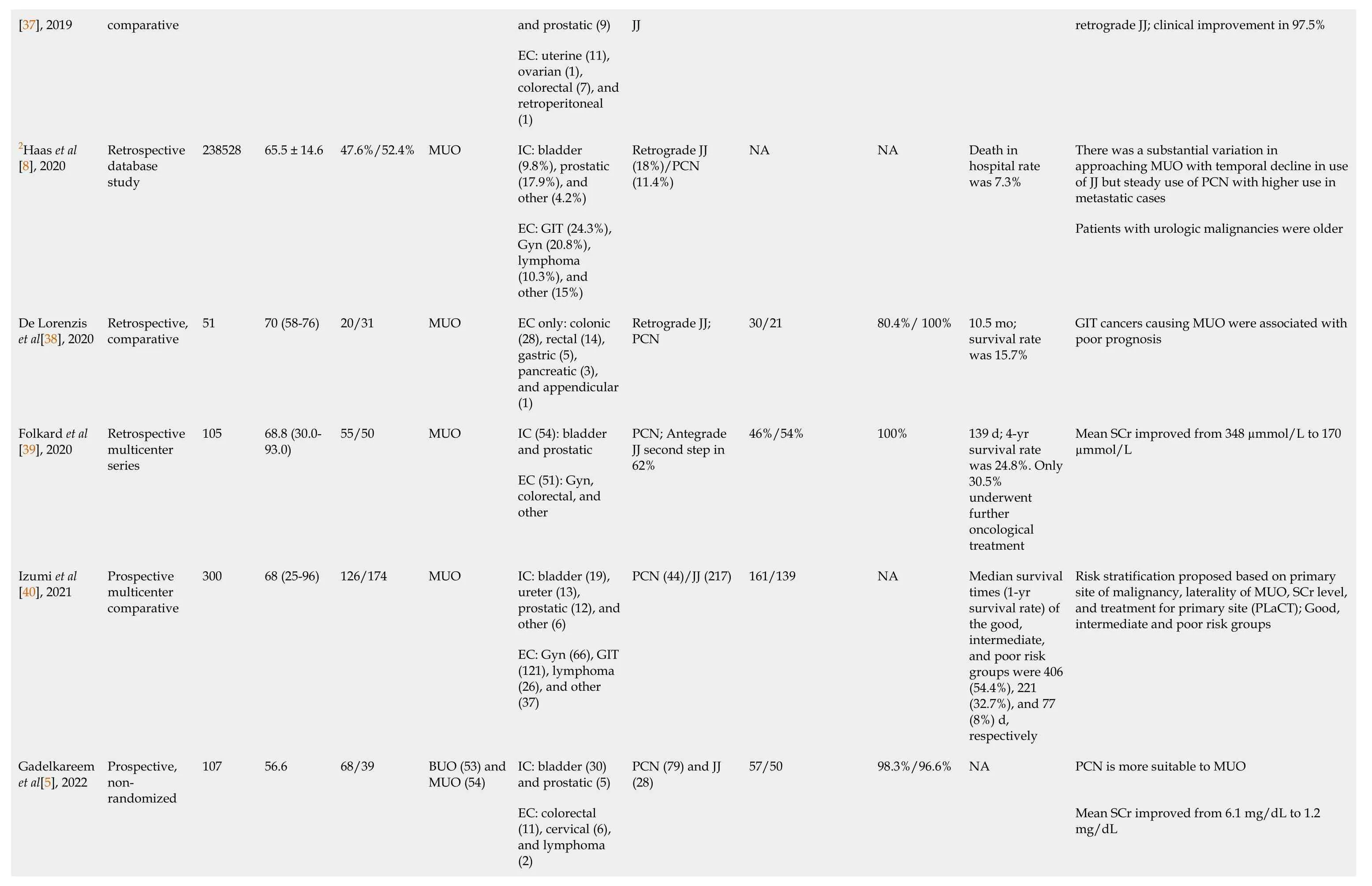
The relevant findings from the literature are summarized as relevant findings per study (Table 1) and as a comparison of the technical and practical characteristics (Table 2).In Table 1,36 studies were reviewed and listed in a chronological manner,including five retrospective studies published from 2000 to 2004[9-13],but one of them included patients with BUO and MUO[9].In 2005,however,another study included patients with BUO and MUO[14],while there were another five studies that included patients with only MUO[15-19].Only one study was found suitable in 2006,including 151 patients with MUO[20].In 2007,three retrospective studies were reviewed with various numbers of patients[21-23].However,five retrospective studies were found in 2008 and 2009[24-28],and three of them had comparative designs[25,27,28].In 2010,the first prospective study was published within the time frame of this review[29].Between 2011 and 2015,we included four retrospective studies[30-33],and only one of them had a comparative design[32].Also,between 2016 and 2019,only four studies were reviewed[34-37],but they included two comparative studies[36,37] and one prospective study[34].Furthermore,we included three studies published in 2020[8,38,39],one comparative study in 2021[40],and three studies in 2022[5,41,42].Table 1 included only four prospective studies[5,29,34,40],one large data base study[8],and two multicenter studies[39,40].Regarding the comparative data presented in Table 2,they were formulated from the studies listed in Table 1[9,12-14,17,21,33] and from other relevant studies[43,44].Many prognostic and risk stratification models have been proposed so far[23,24,26,40].They are based on variables from the patient and underlying pathology.However,the sharp stratification of these patients and solid guidelines have not been settled yet[24,26,30,34,40].These reviewed findings will be addressed and discussed in the different sections of this review.
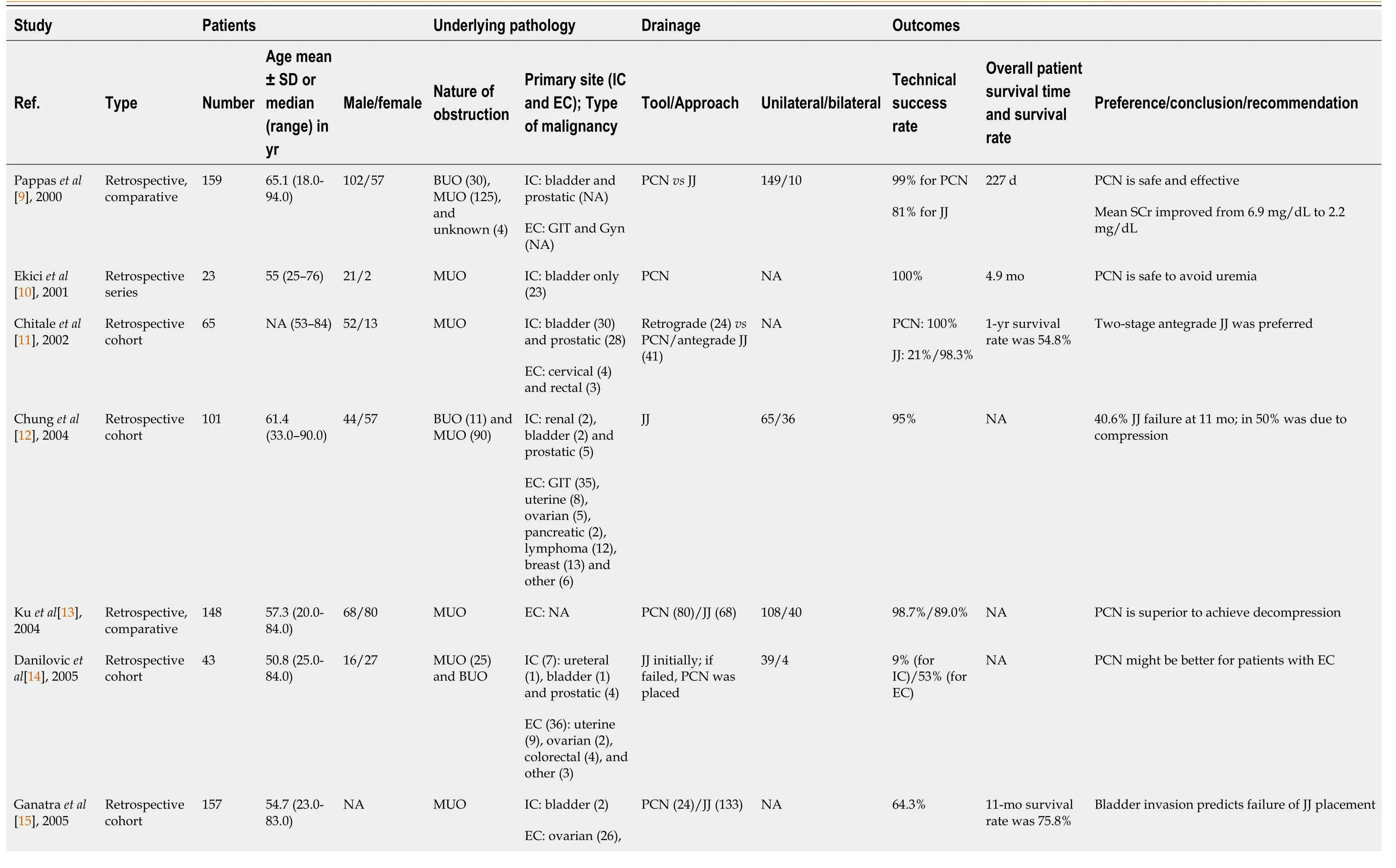
Table 1 Summary of studies of reporting drainage of bilaterally obstructed kidneys due to malignant ureteral obstruction during the period of 2000-2022

INCIDENCE
The incidence of AKI has been estimated by The National Institute for Health and Care Excellence as 13%-18% of people admitted to the hospital[45].It mainly involves the elderly and has a mortality rate of 10%-80%[45,46].Globally,AKI affects over 13 million people per year and results in 1.7 million deaths.Four in five cases of AKI occur in the developing world[47,48].Po-AKI represents 5%-10% of all AKI cases[49].However,it can represent up to 22% of AKI cases among the elderly[50] and 7.6% of the intensive care patients.Po-AKI due to MUO may represent up to 10% of cases with Po-AKI and 18% of patients with malignancy diagnosed within 1 year[51].
PATHOPHYSIOLOGY
Etiological classification of Po-AKI
Po-AKI is caused by urinary tract obstruction,when this obstruction affects the both functioning kidneys,a solitary kidney,or an only-functioning kidney.Relative to the origin of the obstructing pathology,the mechanism and causes of ureteral obstruction are classified into extraluminal compression,stenosis due to a mural pathology,and intraluminal lodgments.The three most common causes of renal obstruction in adults are urinary stones,malignancy,and iatrogenic benign strictures[6,7].Hence,these causes are either malignant or benign pathologies.The benign causes include urinarytract stones,ureteral strictures,and retroperitoneal fibrosis[7].However,the malignant causes include both urological and extraurological malignancies[5,6].The urological carcinomas of the urinary bladder[10,52] and prostate cancer[18] are the most common causes of MUO.The extraurological malignancies include colorectal cancer[5],cervical and uterine cancers[27],adnexal cancers,and systemic malignancy such as lymphoma and metastases (Table 1)[5,51].

Table 2 Comparison between the drainage of kidneys with malignant ureteral obstruction by percutaneous nephrostomy vs double-J stent approach
Pathophysiological mechanisms of Po-AKI with MUO
Obstruction-based mechanisms:There are multiple intrinsic pathophysiological mechanisms of AKI with BOKs,including hemodynamic instability,microcirculatory disorders (such as endothelial dysfunction and microvascular thrombosis),inflammation,tubular cell injury,renal venous congestion,tubular obstruction,and auto-immune processes[53].Reductions in renal blood flow represent a common pathologic pathway for decreasing the glomerular filtration rate in all these mechanisms[54].However,the most likely explanation is that one adopting an occurrence of alterations in the glomerulotubular dysfunction due to urine flow obstruction[55].In the early hours of obstruction of the kidney,the intraluminal pressure is transferred to the renal tubules and to Bowman’s space[55].The transferred pressure results in a decreased filtration pressure in the glomerular capillary walls.After 2-3 h of obstruction,a prostaglandin-mediated myogenic change in the afferent arterioles increases the renal blood flow,which normalizes within 5 h.
After 1 d,the renal and intraglomerular blood flow decreases as a result of the intrarenal production of thromboxane A2 and angiotensin II.These products are strong vasoconstrictors of the afferent and efferent arterioles and contribute to the reduction of the glomerular filtration rate[55].Thromboxane A2 and angiotensin II cause contraction of the mesangial cells,decreasing the glomerular surface area that is used for filtration.After 2 d,increased thromboxane A2 reduces kidney plasma by 60%.With persistence of obstruction,more losses occur in the tubular brush epithelia and renal blood flow[56].In addition,alterations in physiological sodium and water reabsorption are noted.Sodium absorption increases in the proximal tubules,but this increase is associated with a more significant decrease in sodium absorption in the juxtaglomerular nephrons.Furthermore,there is a reduction in the medullary ability to concentrate urine to only 350–400 mOsm[51,55,57].This decrease in tonicity results in a drop in water absorption in the descending part of the loop of Henle.Metabolic acidosis and hyperkalemia are common in Po-AKI due to many factors,representing a failure of renal acidification.This occurs with the inability to excrete potassium and hydrogen,which is explained by distal renal tubular acidosis and Na-K-ATPase failure,resulting in hyperkalemia[51].
Malignancy-based pathophysiological mechanisms:There is a well-established relationship between malignancy and impairment of renal functions.These intimate relationships have led to the evolution of a new branch of nephrology that is concerned with associations of cancer with the renal diseases.It is not only malignancy that affects kidney function by ureteral obstruction,but also various nephropathies are associated with its hematopoietic,chemotherapeutic and immunotherapeutic effects of different types of malignancy.These nephropathies manifest clinically as proteinuria,hematuria,hypertension,and cancer related-chronic kidney disease[58-60].
AKI in patients with malignancy is relatively common.According to a study conducted on 37000 malignancy patients over a 5-year period,27% of those patients developed AKI,and 7.6% of them developed severe AKI requiring dialysis.Also,the risk of AKI within the first year after a cancer diagnosis can be more than 18% in malignancy patients[51,61].The non-obstructive causes of AKI in patients with malignancy include sepsis due to low immunity and bad general conditions,direct kidney injury due to the primary malignancy,metabolic disturbances,and nephrotoxic effects of chemotherapies.In turn,AKI increases the risk of toxic effects from systemic chemotherapy,threatening their continuation[62].
The development of ureteral obstruction in the course of any malignancy is considered a sign of disease progression and reduces the median survival to <1 year[21,24,34].MUO is a bad event that is usually associated with advanced,and often,incurable stages of malignancy.Further,it is a definitive cause of urosepsis,acute pain,and uremic syndrome.Unilateral or bilateral MUO is due to extrinsic compression or direct infiltration by a local primary tumor or retroperitoneal lymphadenopathy.It may occur in patients with a previously diagnosed malignancy up to 84%.The median patient age at MUO diagnosis is usually high (Table 1),and the median time for development of MUO after the diagnosis of primary malignancy is variable[5,23].In comparison,the obstruction-based mechanisms seem to have a more favorable prognosis than the malignancy-based mechanisms.The effect of the benign mechanisms is usually unifactorial and reversible by a prompt drainage of the kidneys.In contrast,the malignancybased mechanisms are virtually multifactorial and irreversible in most instances[62].Hence,MUO is a modifiable risk factor of morbidity and mortality in patients with Po-AKI due to malignancy.Drainage of the obstructed kidneys can prevent the major sequelae of the obstruction-based mechanisms,promptly reversing the acute deteriorations of renal functions within days or weeks[5].
CLINICAL PRESENTATION
In Po-AKI,the clinical presentation includes the general manifestations of uremia and manifestations of urinary tract obstruction.The latter may include loin pain secondary to stretching of the urinary collecting system and hematuria caused by the obstructing malignancy[63].Decrease in urine output is a common presentation,but it is not specific to Po-AKI[41,51].Patients with Po-AKI may present with loin tenderness and fever when obstruction is associated with infection[51,57].
DIAGNOSIS
The initial laboratory evaluation should include measurement of blood gases and electrolyte levels,SCr,blood urea nitrogen,and complete blood count.Urinalysis may be requested in cases with a preserved urine output.Then,AKI could be diagnosed and staged according to KDIGO guidelines.In Po-AKI,the hallmark of diagnosis is the presence of hydronephrosis on abdominal ultrasonography (US) or computed tomography[41].Hydronephrosis can easily be demonstrated by the grey scale US where pelvicalyceal dilatation is recognized with or without disappearance of the renal papillae[51].After 3 to 4 wk of obstruction,diffuse thinning of the renal cortex and the medullary tissue is mostly recognizable.Moreover,Doppler US can evaluate the blood perfusion of the kidneys themselves by measuring the resistive index and ureteral obstruction by evaluation of the ureteral jets.The absence or decreased frequency of ureteral jets may indicate urinary obstruction.The severity of ureteric obstruction can be determined by evaluating all jet dynamics,including velocity,duration,and frequency[64].However,computed tomography is still the most diagnostic tool of Po-AKI due to benign and malignant causes[5].
MANAGEMENT
Initial measures of management
While the management of the prerenal and renal types of AKI is mainly supportive in nature,drainage of BOKs is the cornerstone of management of Po-AKI.However,the initial conservative management of patients with Po-AKI is mostly similar to that of the other types.It consists of resuscitation and correction of the metabolic imbalances[41].However,temporary drainage of BOKs is a mandatory and principal intervention,keeping the correction of the underlying cause to a time after recovery from AKI.
A urethral catheter placement can be performed in cases of bladder outlet obstruction such as benign prostatic hyperplasia,but PCN or double-J stent (JJ) are the usual methods in the cases of ureteral obstruction[2,4,65].Then,the broad-line goals of management are to correct the biochemical abnormalities such as severe metabolic acidosis and hyperkalemia,prevent further injury or progression to chronic kidney disease,and treat the underlying pathology[65].The management of hyperkalemia includes prevention of the life-threatening cardiac arrhythmias by administering calcium-based salts,support of shifting potassium into the cells,and enhancement of elimination of potassium through cation exchange resins[65,66].
Despite their fundamental roles,these pharmacological and conservative interventions may have a lower effect in the management of Po-AKI than in the management of the other types,relative to the role of drainage[51,57].Renal replacement therapy is considered in specific circumstances,such as the progression of complications in the severe cases with pulmonary edema,persistent hyperkalemia,and disturbed consciousness.This therapy is mostly in the form of intermittent hemodialysis,but peritoneal dialysis may be performed in a few circumstances[41,51,67].
Regarding the practical aspect of prioritizing dialysis over drainage,there is a perspective that underscores whether the degree of elevation of SCr alone is an indicator to resort to dialysis before drainage[41].It can be preferable to drain one or both kidneys whenever the patient can withstand the intervention for placement of a PCN[5].This might augment the chances of recovery with the conservative management and in those patients who may still warrant temporary dialysis after drainage.Despite the drainage efficacy,dialysis could also play an important role in the management of those patients,especially when drainage is not preferable,such as in patients with a very poor prognosis[52,68].
Drainage of BOKs
Currently,there is no consensus or well-established guidelines addressing the proper drainage of MUO,leading to wide variations in the practice patterns and preferences[5,69,70].However,relieving MUO prevents death from progressive renal failure and possibly prolongs the patient survival[20,24].There are two modalities for drainage of the kidneys with MUO: PCN and JJ.Both methods can cause considerable morbidity and reduce a patient’s health–related QoL.There are multiple studies that compared both of them and their impact on QoL in MUO because those patients are usually in late stages and their QoL is already impaired[9,71].The use of JJ for drainage of BOKs has many challenges,including higher invasiveness,need of anesthesia,liability of obstruction,and impossible placement due to complete obliteration of the ureteral lumen.These limitations are potentially present with antegrade and retrograde placement[72,73].These challenges led to the development of the JJ characteristics,ranging from the new materials to the pressure-based capabilities.JJ has different types,ranging from the conventional polymeric stents to the malignancy-specifically designed stents.Among the latter,there are 3 important types that have gained popularity in recent years and are used in MUO: tandem ureteric stent;metallic stent;and metal-mesh ureteral stents.Many studies have concluded very high rates of stent failure in MUO because the tumor or lymphadenopathy compresses the ureter against the indwelling stent,persistently obliterating the tube lumen and limiting the extraluminal flow[74,75].Also,the ureteral stent promotes mucous production from the urothelium and leads to urothelial sloughing.The lumen of a ureteral stent can become occluded with this debris[76-78].
Metallic ureteral stents gained superiority over the conventional JJ as they have a low occlusion rate,high success rate (60%) at 1 year,and low failure rate (15.4%)[79].Considering that the median survival time with extrinsic MUO is about 1 year[24,34],there is a high possibility that metallic stent replacement is unnecessary during a patient’s life.Tandem ureteric stent consists of a side-by-side ureteric stents within the ureter and can resist obstruction by providing a space in between the two stents that is difficult to compress.It has a success rate of approximately 87% at 2 years[80].It has a range of exchange from 6 mo to 1 year[76,80].Success rates ranged from 88% for the Allium stent to 65% for the Memokath 051.Resonance stent demonstrated the lowest migration rate (1%).Uventa showed the lowest obstruction rate (6%).A comparative study conducted by Chenet al[81] reported that metallic stents have longer indwelling time and are superior to conventional polymeric stents.There is a mean increase in functional duration of 4 mo,using the Resonance stent when it is compared to conventional polymeric stent[75].
Although PCN has a high success rate[13] and is considered safer than JJ[69],its need to carry an external bag could threaten the patient QoL[69].PCN seems to be more suitable for patients with advanced malignancy who may not have the candidacy for anesthesia or the ureteral patency to pass JJ.Also,they may have expected survival rates less than 12 mo that could be improved by PCN.However,the disturbance of their QoL is still the main concern,warranting estimation of the balance between the benefits and the risks[6,70].There are no clear advantages between the two forms of urinary diversion in MUO[6] (Tables 1 and 2).However,the type of urinary diversion depends on the experience of the urologist,the existing expertise,the availability of the armamentarium,the stage of malignancy,and the urgency of the diversion[82].In addition,it is dependent on the potential benefits of diversion at different parameters,including the radiological exposure,decrease in SCr,the overall complication rate,febrile episodes after drainage,tube exchange rate,and overall patient survival.Both drainage forms seem to have no advantage over each other in these variables[43].
However,despite the evidence-based recommendation by the recent meta-analyses in favor of the use of JJ rather than PCN in patients with MUO[43],there is an attitude that PCN is more commonly used than JJ for drainage of BOKS with MUO (Table 1).This attitude is noticeable in the single-center studies[5,8,83].Owing to the potential of placement of wide-caliber tubes and insertion of antegrade JJ[11,37],PCN may provide the chance of obtaining high drainage capacities[44].Also,PCN may become the only suitable method for drainage,especially in the elderly patients with advanced stages of malignancy who are not candidates for intervention[34,43],or have non-passable MUO[15,43].On the other hand,PCN may disturb the QoL more than JJ[6,19].This may be attributable to many potential unfavorable events with PCN such as the repeated slippage,obstruction,and urinary leakage.Hence,there should be a sufficient rationale to perform urinary diversion by PCN in patients with terminal stages of malignancy[6,57,84].If the evidence of the effect on QoL is absent,the potential survival benefit remains the individual factor that drives the decision,which should be PCN in patients with advanced malignancy[43,84].This may be attributed to the fact that most of these patients have no further oncological treatment chances following the diversion[39].
Laterality of drainage of BOKs with MUO has been addressed by some authors like Hyppoliteet al[85] who concluded superiority of bilateral over unilateral drainage.However,Nariculamet al[28]found no difference between unilateral and bilateral drainage.The combination of the tool and side of drainage in cases of BOKs is known as the mode of drainage.Despite the continuous research,the definition of the optimal mode of drainage of BOKs is still controversial,including the cases of MUO[5,43,70].We may adopt the perspective of performing unilateral drainage of BOKs,unless there are bilateral infections,pain,or non-improvement of SCr after unilateral drainage.In the latter situation,bilateral drainage can be performed consecutively[5].Similarly,the optimal mode of drainage of BOKs due to BUO is still controversial.In a recent survey study to evaluate the preferences of urologists and radiologists who may have the principal duties of interventions in cases of acute BOKs,the conclusion was to individualize the decision for each case with emergency indications for upper tract decompression by JJvsPCN[86].
PROGNOSTIC PARAMETERS AFTER DRAINAGE OF BOKS DUE TO MUO
Urine output
An increase in urine output is an early sign of renal recovery in patients with oliguric AKI.This is accompanied by a reduction in the level of high SCr,followed by a plateau period,and a subsequent fall in SCr[8,54].Usually,the increase of urine output is physiologic and self-limiting within the first 24 h after relief of obstruction.The kidneys try to normalize the internal environment of the body by fluid and electrolyte homeostasis within the early hours before returning to the normal status of the urine output[57].The post-obstructive diuresis means increased urine output after relief of BOKs.It is defined as increased urine output >200 mL for two consecutive hours or urine output >3000 mL per 24 h after relief of obstruction.When this diuresis becomes excessive or is prolonged,it becomes pathologic.It is attributed to the sudden release of the obstruction,which initiates reflex diuresis by multiple mechanisms,evoking the full capacity of the functioning nephrons[57].
There is a perspective that post-obstructive diuresis may be a sign of the acuteness of the condition and the magnitude of the renal power preserved.Also,it is believed that it is more common after drainage of BOKs due to BUO than those due to MUO[5].For example,an obstruction by a stone is related to its migratory potential that can be sudden and complete in comparison with an infiltrating malignancy that causes a gradual obstruction[6,7].However,this point of difference between BUO and MUO has not been sufficiently addressed in the literature.Despite its favorable prognostic values,the potential pathologic,metabolic,and circulatory risks of post-obstructive diuresis may threaten the patient’s life.Hence,it should be managed properly by oral or intravenous fluid compensation and management of the electrolyte imbalances that could ensue with excessive diuresis[57].
SCr trajectory
The rate of change of SCr over time in AKI is known as the creatinine trajectory.It can be applied in both the deterioration and recovery phases[1,5].The time factor in this topic reflects its practical importance in catching a cure in patients with MUO.SCr trajectory has attracted the attention in the management of patients with prerenal and renal AKI[87].However,it is still not recognizable in cases of Po-AKI.Our own work on this subject has not been published yet.The SCr trajectory is a potential parameter to understand AKI during both the renal dysfunction and recovery phases.The deterioration SCr trajectory may facilitate clinical classification and subtyping of AKI,using a different parameter rather than maximal SCr change.However,it mandates knowing a predeterioration or baseline SCr level,which is often lacking for most patients admitted in an emergency setting[1,88].On the other hand,based on SCr trajectory,the post-intervention classification facilitates understanding patient responses to early medical interventions.This could be provided by serial measures of SCr.Hence,the identification of AKI subclasses based on SCr trajectory has been proposed as a tool to improve the precision of risk stratification of patients with AKI[1,87,88].
The time-to-nadir SCr
The time needed to reach a nadir SCr or what is known as the time-to-nadir SCr after drainage of BOKs is another parameter of the responses of the kidneys to drainage.To the best of our knowledge,this parameter has not been sufficiently addressed in the literature of Po-AKI due to MUO.However,our work in this issue has revealed that large proportions of patients may fail to reach a normal nadir SCr due to the burden of malignancy.Also,the time-to-nadir in cases of MUO seems to be longer than that in the cases of BUO[5].Furthermore,the long time-to-nadir SCr may be associated with a low predrainage urine output and high body mass index.The rationale of measurement of the time-to-nadir SCr in patients with AKI is related to the magnitudes of benefits provided by early recovery,regarding the chance of cure or early management.This issue is still controversial in patients with MUO.The timeto-nadir SCr may be significantly shorter in patients with the potential to normalize SCr than in patients without normalized SCr levels after drainage[89].
Malignancy-related factors
The literature reports that some malignancies are statistically significant predictors of worse survival(Table 1).They include the unresectable or unsuitable malignancies for chemotherapy[83],gastropancreatic[90],hormonal-resistant prostate cancers,and those requiring hemodialysis before the procedure[16].Despite the successful drainage of BOKs in cases of MUO,the survival rate is still poor[23].The three significant factors that can predict a short survival time after PCN in patients with advanced stage malignancy are a low serum albumin before placement of PCN (3 g/dL or less),low grade hydronephrosis (Grade 1 or 2),and a large number of events related to malignant dissemination (3 or more).Patients who had only one variable had a 69% chance of 6-mo survival,those who had two variables had a 24% survival rate,and those with three variables had a 2% survival rate[6,26].Wonget al[23]identified other predictors as metastases,prior therapy,and diagnosis of MUO with a previously established malignancy.Despite developing these prognostic models,there should be a shared decisionmaking approach to perform invasive procedures like PCN and JJ,with a questionable degree of the effect on renal function recovery and the risk of complications.There should be a proper explanation of prognosis,subsequent treatment possibilities,and expected results before proceeding to these invasive maneuvers[42].
Current perspectives and future expectations to improve the poor prognosis
In the last decade,the literature has shown an extensive study of the predictors of the success and overall survival rates in patients with MUO.The common finding in this category of patients is the poor overall survival with advanced MUO[68,91].Many directions have been adopted in research to define the modifiable factors affecting the outcomes of drainage of BOKs in those patients.The main direction is studying the factors related to obstruction-based sequelae of MUO.Besides the type of malignancy,the occurrence of MUO and its degree and laterality were included as risk factors[92,93].Electrolytes and blood biochemical compounds such as serum albumin and hemoglobin levels have been found as independent factors[94,95].Hence,several prognostic models have been configured and published,initiating more debates on the optimal management approach[96-99].As an overview,the ongoing fact that seems to be verified with time is that not all patients gain benefits from drainage,and treatment should be individualized to each patient[95,100].Another direction is the improvement of the qualities and compression-bearing capabilities of the drainage tools,represented by the advances in manufacturing of JJ for MUO.In addition,the research has gone to outweighing the certainty of the benefits of interventions versus observation in those patients,considering disturbances of QoL as a principal factor in decision-making[101,102].
CONCLUSION
AKI due to MUO is a urological emergency,warranting immediate evaluation and management.The principal line of treatment is the drainage of the kidneysviaa placement of PCN or JJ.Despite the growing relevant literature,there is no consensus on the optimal approach.Several prognostic models have been attempted to stratify those patients relative to the potential risks and justify the interventions,but the controversies persist.Hence,the decision-making should be tailored to the patient stage and status rather than to strict guidelines.This selective approach may be attributed to the presence of many prognostic factors that should be considered during management,including the QoL and the anticipated benefit of drainage with a markedly reduced life expectancy of those patients.
FOOTNOTES
Author contributions:Gadelkareem RA and Abdelraouf AM designed the research,searched and collected the data,and wrote the paper;El-Taher AM and Ahmed AI contributed to design,writing and revision,and supervised the work;all authors revised and approved the paper.
Conflict-of-interest statement:The authors report having no relevant conflicts of interest for this article.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Egypt
ORCID number:Rabea Ahmed Gadelkareem 0000-0003-4403-2859;Ahmed Mahmoud Abdelraouf 0000-0002-7940-1573;Ahmed Mohammed El-Taher 0000-0001-7868-5749;Abdelfattah Ibrahim Ahmed 0000-0003-4643-4448.
S-Editor:Xing YX
L-Editor:Filipodia
P-Editor:Xing YX
