Comparison of clinicopathological characteristics between resected ampullary carcinoma and carcinoma of the second portion of the duodenum
2022-11-29KoheiNishioKenjiroKimuraAkihiroMurataGoOhiraHirojiShinkawaShintaroKodaiRyosukeAmanoShogoTanakaSadatoshiShimizuShigekazuTakemuraAkishigeKanazawaShojiKuboTakeakiIshizawa
Kohei Nishio,Kenjiro Kimura,Akihiro Murata,Go Ohira,Hiroji Shinkawa,Shintaro Kodai,Ryosuke Amano,Shogo Tanaka,Sadatoshi Shimizu,Shigekazu Takemura,Akishige Kanazawa,Shoji Kubo,Takeaki Ishizawa
Kohei Nishio,Kenjiro Kimura,Go Ohira,Hiroji Shinkawa,Ryosuke Amano,Shogo Tanaka,Shigekazu Takemura,Shoji Kubo,Takeaki lshizawa,Department of Hepato-Biliary-Pancreatic Surgery,Osaka Metropolitan University,Osaka 5458585,Japan
Akihiro Murata,Shintaro Kodai,Sadatoshi Shimizu,Akishige Kanazawa,Department of Hepato-Biliary-Pancreatic Surgery,Osaka City General Hospital,Osaka 5340021,Japan
Abstract BACKGROUND Few studies compared the oncological and biological characteristics between ampullary carcinoma (AC) and cancer of the second portion of the duodenum (DC-II),although both tumors arise from anatomically close locations.AIM To elucidate differences in clinicopathological characteristics,especially the patterns of lymph node metastasis (LNM),between AC and DC-II.METHODS This was a retrospective cohort study of 80 patients with AC and 27 patients with DC-II who underwent pancreaticoduodenectomy between January 1998 and December 2018 in two institutions.Clinicopathological factors,LNM patterns,and prognosis were compared between the two groups.RESULTS The patients with AC and DC-II did not exhibit significant differences in 5-year overall survival (66.0% and 67.1%,respectively) and 5-year relapse-free survival (63.5% and 62.2%,respectively).Compared to the patients with DC-II,the rate of preoperative biliary drainage was higher (P = 0.042) and the rates of digestive symptoms (P = 0.0158),ulcerative-type cancer (P <0.0001),large tumor diameter (P <0.0001),and advanced tumor stage (P = 0.0019) were lower in the patients with AC.The LNM rates were 27.5% and 40.7% in patients with AC and DC-II,respectively,without significant difference (P = 0.23).The rates of LNM to hepatic nodes (N-He) and pyloric nodes (N-Py) were significantly higher in patients with DC-II than in those with AC (metastasis to N-HE: 18.5% and 5% in patients with DC-II and AC,respectively;P = 0.0432;metastasis to N-Py: 11.1% and 0% in patients with DC-II and AC,respectively;P = 0.0186)CONCLUSION Although there were no significant differences in the prognosis and recurrence rates between the two groups,metastases to N-He and N-Py were more frequent in patients with DC-II than in those with AC.
Key Words: Ampulla of Vater;Duodenum;Lymphatic metastasis pattern;Lymphatic metastasis station;Lymph node excision;Neoplasm;Pancreaticoduodenectomy
lNTRODUCTlON
Ampullary carcinoma (AC) accounts for 0.2% of all gastrointestinal cancers and 7% of all periampullary cancers[1].In contrast to other periampullary carcinomas,AC is associated with higher resection rates and better prognosis because of its earlier presentation due to the anatomical characteristics[2].The reported rates of resection and 5-year survival after resection of AC are approximately 50%[3] and 30%-52%[4,5],respectively,whereas primary duodenal cancer (DC) accounts for approximately 0.3% of all gastrointestinal cancers[6] and 30%-45% of all small intestinal cancers[7].The reported rates of resection and 5-year survival after resection of DC are 39%[8] and 37%-67%[9-12],respectively.The only curative treatment for both AC and DC,especially DC located in the second portion of the duodenum (DC-II),is surgical resection with regional lymph node dissection using pancreaticoduodenectomy.The National Comprehensive Cancer Network (NCCN) guidelines recommend pancreaticoduodenectomy withen blocremoval of regional lymph nodes for resectable DC-II and state that pyloric preservation is acceptable in the absence of a hereditary condition[13].In contrast,there are no NCCN guidelines for AC.The lymph node metastasis (LNM) patterns and the optimal range of lymph node dissection in DCII and AC remain controversial.The present study aimed to compare the oncological and biological characteristics between DC-II and AC.
MATERlALS AND METHODS
Eighty-four patients with AC and thirty-six patients with DC-II who underwent surgical resection in Osaka City University Hospital or Osaka City General Hospital between January 1,1998 and December 31,2018.After the exclusion of patients who underwent duodenal partial resection (n= 9) and papillectomy (n= 4),the remaining 80 patients with AC and 27 patients with DC-II who underwent pancreaticoduodenectomy were included in the present retrospective cohort study (Figure 1).All patients were followed for survival,and the median follow-up period was 36.5 (range,2.3-227.3) months.Recurrence was defined when the tumor was detected again by imaging modalities,such as enhanced CT.Surgical approaches included classical pancreaticoduodenectomy (Whipple procedure) in 50 patients (12 patients with DC-II and 38 patients with AC),subtotal stomach-preserving pancreaticoduodenectomy in 49 patients (14 patients with DC-II and 35 patients with AC),and pyloruspreserving pancreaticoduodenectomy in 8 patients (1 patient with DC-II and 7 patients with AC).As adjuvant chemotherapy,33 patients,including 8 patients with DC-II and 25 patients with AC,received S-1 (4 patients with DC-II and 14 patients with AC),tegafur-uracil (3 patients with DC-II and 8 patients with AC),and gemcitabine (1 patient with DC-II and 3 patients with AC).There were no definitive criteria for the administration of adjuvant chemotherapy.

Figure 1 Patient flowchart.
The demographic and clinical variables included age,sex,preoperative body mass index,preoperative modified Glasgow prognostic score,tumor size,gross appearance,preoperative biliary drainage,preoperative symptoms,preoperative serum carbohydrate antigen level,preoperative serum carcinoembryonic antigen level,operative procedure,duration of operation,volume of intraoperative blood loss,histological grade,Union for International Cancer Control (UICC) classification,LNM,lymphatic invasion,venous invasion,postoperative complications,and adjuvant chemotherapy.
The TNM classification and the pathological stage of all tumor specimens were determined using the 7th edition of the UICC TNM classification[14].Tumor differentiation was classified into well differentiated,moderately differentiated,poorly differentiated,and undifferentiated adenocarcinoma,according to the World Health Organization classification[15].Regional lymph nodes were classified into superior pancreaticoduodenal lymph nodes (N-SP),inferior pancreaticoduodenal lymph nodes (N-IP),pyloric lymph nodes (N-Py),hepatic lymph nodes (N-He),and superior mesenteric lymph nodes (N-SM) according to AJCC Cancer Staging 7thedition[16].The initial recurrent sites were classified into liver,lungs,distant lymph nodes,peritoneum,local,and others.
Statistical analysis
The clinicopathological factors were compared between the patients with DC-II and AC.Categorical variables were compared using theχ2or Fisher’s exact test.Continuous variables were compared using Mann-Whitney U tests.Survival was calculated using the Kaplan-Meier method,and comparisons between the groups were performed using the log-rank test.Pvalues of <0.05 were considered to indicate statistical significance.All statistical analyses were performed using JMP®version 12 (SAS Institute,Cary,NC,United States).
RESULTS
Comparison of overall survival and relapse-free survival between the patients with DC-II and AC
The 5-year overall survival (OS) rate was 66.0% in the patients with AC and 67.1% in those with DC-II (P= 0.80) (Figure 2A).The 5-year RFS rate was 63.5% in the patients with AC and 62.2% in those with DC-II (P= 0.88) (Figure 2B).

Figure 2 Survival curves of patients with cancer of the second portion of the duodenum (n = 27) and ampullary carcinoma (n = 80).
Comparison of the clinicopathological factors between the patients with DC-II and AC
Table 1 shows the results of the comparative analysis of the clinicopathological factors between the patients with DC-II and AC.Briefly,the rate of preoperative biliary drainage was significantly higher in the patients with AC than in those with DC-II (P= 0.042).Conversely,the rates of digestive symptomsi.e.,vomiting,nausea or abdominal pain (P= 0.0158),ulcerative-type tumor (P<0.0001),large tumor diameter (P<0.0001),and advanced tumor invasion (P= 0.0019) were significantly higher in the patients with DC-II than in those with AC.The LNM rate was 27.5% in the patients with AC and 40.7% in those with DC-II,without significant difference (P= 0.23).

Table 1 Comparative analysis of clinicopathological factors between patients with resected cancer of the second portion of the duodenum and ampullary carcinoma

17th edition of the Union for International Cancer Control TNM classification.AC: Ampullary carcinoma;BMI: Body mass index;CA19-9: Carbohydrate antigen 19-9;CD: Clavien-Dindo classification;CEA: Carcinoembryonic antigen;DC-II: Carcinoma of the second portion of the duodenum;mGPS: Modified Glasgow prognostic score;mod: moderately differentiated adenocarcinoma;muc: mucinous adenocarcinoma;pap: papillary adenocarcinoma;PD: Pancreaticoduodenectomy;poor: Poorly differentiated adenocarcinoma;PpPD: Pylorus-preserving pancreaticoduodenectomy;SSPPD: Subtotal stomach-preserving pancreatoduodenectomy;well: Well-differentiated adenocarcinoma.
Comparison of the affected sites and the frequency of LNM between the patients with DC-II and AC
Table 2 shows the results of the comparative analysis of the affected sites and the frequency of LNM to specific sites between the patients with DC-II and AC.In summary,the rates of LNM to the N-He and the N-Py were significantly higher in the patients with DC-II than in those with AC (metastasis to N-He: 18.5% and 5% in patients with DC-II and AC,respectively;P= 0.0432;metastasis to N-Py: 11.1% and 0% in patients with DC-II and AC,respectively;P= 0.0186).There were no significant differences in the rates of metastases to the N-SP,N-IP,and N-SM between the patients with DC-II and AC.
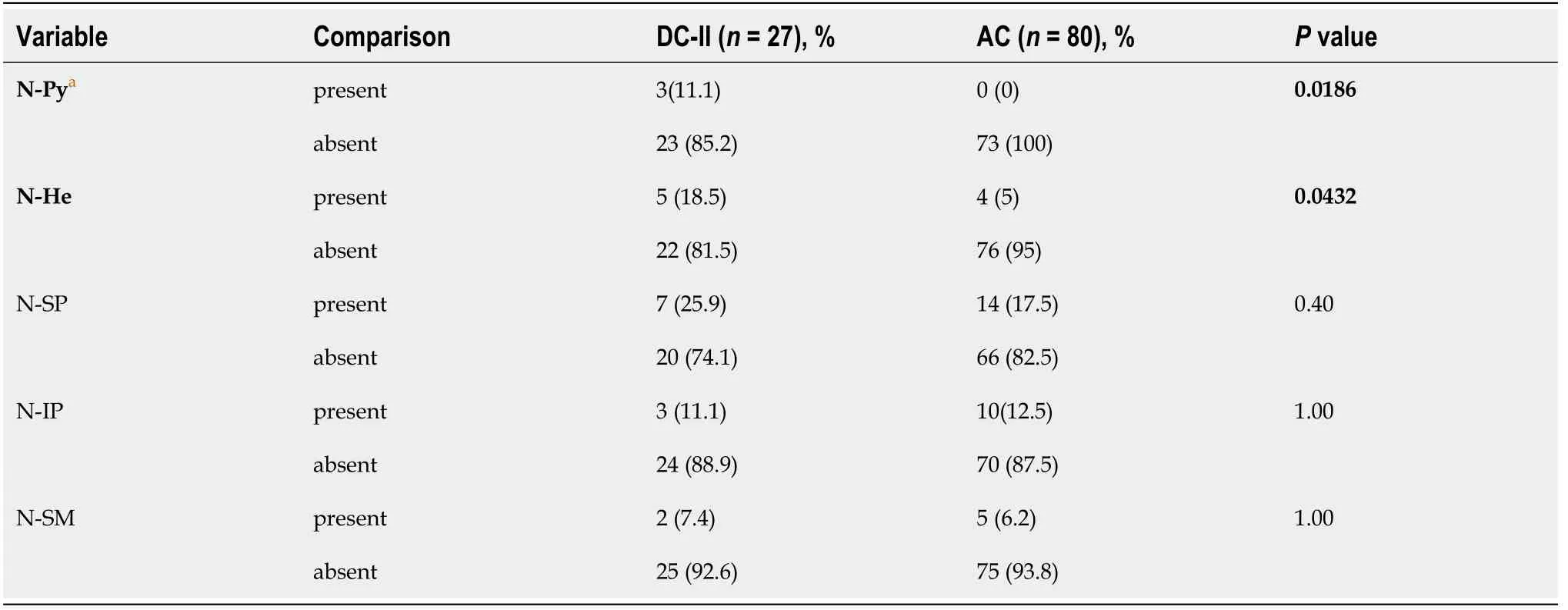
Table 2 Comparison of the sites and the frequency of lymph node metastasis between the patients with cancer of the second portion of the duodenum and ampullary carcinoma
Figure 3 shows the LNM distribution in patients with DC-II and AC.Briefly,LNM was found in 11 of the 27 patients (40.7%) with DC-II,including metastases to N-SP,N-He,N-Py,N-IP,and N-SM in 7 (63.6%),5 (45.5%),3 (27.3%),3 (27.3%),and 2 (18.2%) patients,respectively.Meanwhile,LNM was found in 22 of the 80 patients (27.5%) with AC,including metastases to N-SP,N-IP,N-SM,and N-He in 14 (63.6%),10 (45.5%),5 (22.7%),and 4 (18.2%) patients,respectively.Metastasis to N-Py was not found in any of the patients with AC (0%).
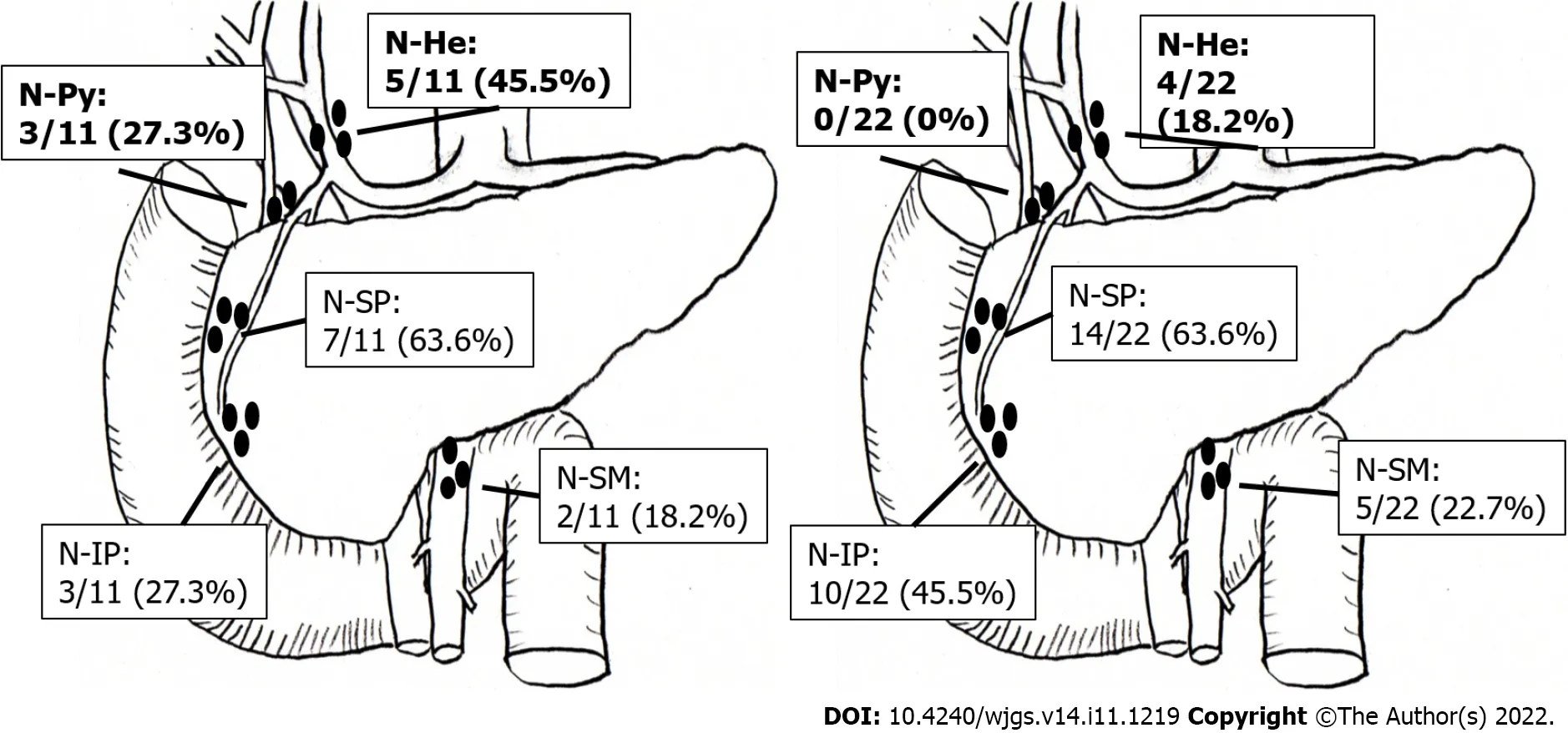
Figure 3 The distribution of lymph node metastasis in patients with cancer of the second portion of the duodenum (n = 11) and ampullary carcinoma (n = 22).
Analysis of the initial recurrent sites in patients with DC-II and AC
Table 3 shows the comparison of the initial recurrent sites of DC-II and AC.Initial recurrence was observed in 28 patients with AC and 10 patients with DC-II.Specifically,10 (35.7%),6 (21.4%),6 (21.4%),and 5 patients (17.9%) with AC experienced recurrence in distant lymph nodes,lungs,liver,and local sites,respectively.Meanwhile,5 (50%),3 (30%),and 2 (20%) patients with DC-II experienced recurrence in distant lymph nodes,lungs,and liver,respectively,with no local recurrence observed in any of the patients with DC-II.There was no significant difference in the recurrence pattern between the patients with AC and DC-II.

Table 3 Analysis of initial recurrent sites in patients with cancer of the second portion of the duodenum and ampullary carcinoma
DlSCUSSlON
The present study results indicated that metastases to N-He and N-Py were more frequent in patients with DC-II than in those with AC.The NCCN guidelines indicate that pancreatoduodenectomy withen blocremoval of regional lymph nodes,including retropancreatic,hepatic artery,inferior pancreaticoduodenal,and superior mesenteric lymph nodes,should be performed for resectable DC-II [13].Furthermore,the guidelines state that pyloric preservation is acceptable in the absence of a hereditary condition[13].The 7thedition of the UICC TNM classification of malignant tumors include N-Py as regional lymph nodes[14].Sakamotoet al[17] indicated that the rate of metastasis to N-Py and N-He was significantly higher in patients with duodenal bulbs tumors and DC-II than in those with tumors in the third or fourth portion of the duodenum.Katoet al[18] reported that metastasis was detected in infrapyloric lymph nodes in 11.4% of patients with DC in the 1st-4thportion,and the location of the LNM did not exhibit a significant correlation with the primary site of DC.In the present study,metastasis to N-Py was found in 11.1% of patients with DC-II.In contrast,there are no NCCN guidelines for AC,and the 7thedition of the UICC TNM classification of malignant tumors include N-Py in the regional lymph nodes in patients with AC[14].The General Rules for Clinical and Pathological Studies on Cancer of the Biliary Tract (6thedition) by the Japanese Society of Hepato-Biliary-Pancreatic Surgery include N-Py in the list of regional lymph nodes in patients with AC,although N-Py dissection is not mandatory[19].Kayaharaet al[20] reported that metastasis to N-Py was absent in patients with resected AC.Similarly,no patient with resected AC had metastasis to N-Py in the present study cohort.Muet al[21] reported that the rate of metastasis to N-Py was 2.5% in patients with AC.Leeet al[22] also reported that LNM of AC first spread to the posterior pancreaticoduodenal lymph nodes followed by spread to the anterior pancreaticoduodenal nodes,and metastasis to N-Py and N-He was limited in patients with AC.Several studies on AC reported that lymphatic spread mainly extended from the posterior pancreaticoduodenal region to the superior mesenteric lymph nodes[20,23,24].Furthermore,another study suggested that the papilla of Vater was derived from the ventral pancreas with not many communicating lymphatic vessels between the ventral and dorsal pancreas[25];therefore,it was speculated that most of the LNM of AC moved toward N-SMviathe inferior pancreaticoduodenal artery.However,we also speculated that lymphatic spread not only extended from the posterior pancreaticoduodenal region to the superior mesenteric node but also from the anterior pancreaticoduodenal region to N-Py and N-Heviathe gastric duodenal artery in DC-II.These anatomical considerations might be associated with the higher rates of metastases to N-He and N-Py in patients with DC-II than in those with AC.
In the current study,the rates of cases with large tumor diameter and advanced tumor invasion were higher in patients with DC-II than in those with AC.These differences might be due to the earlier appearance of symptoms,such as jaundice,in patients with AC than in those with DC-II,leading to the earlier diagnosis of AC.We did not observe significant differences in OS and RFS between the patients with AC and DC-II despite the more advanced tumor invasion observed in the patients with DC-II.These results might suggest that even in DC with more advanced tumor invasion than AC,the prognosis equivalent to AC could be obtained if pancreaticoduodenectomy with regional lymph node dissection as well as AC was performed.Riallet al[26] reported that the 5-year overall survival rate after pancreaticoduodenectomy was 37% in patients with AC and 51% in those with DC and that the prognosis of DC was significantly better than that of AC.Other studies reported that there was no significant difference in OS between the patients with resected AC and DC[27,28].However,these studies were small in scale and retrospective in design;therefore,large-scale cohort studies are warranted for the accurate comparison of prognosis between the patients with DC and AC.
The present study results also revealed that distant lymph nodes were the most common sites of initial recurrence in both DC-II and AC.Several studies reported that the most common site of recurrence was liver in patients with AC undergoing curative resection[29,30].Conversely,Cecchiniet al[31] reported that 45% of the patients with resected DC had recurrence and that the first sites of recurrence were distant,locoregional,and both in 21%,19%,and 5% of the patients.Onkendiet al[32] reported that approximately 60% of all recurrences were locoregional of paients with resected DC.However,these studies included segmental resection in addition to pancreaticoduodenectomy,which were considered as the cause of the high locoregional recurrence rate.In a study including patients undergoing pancreaticoduodenectomy for AC or DC,Bowitzet al[33] reported that the recurrence patterns of AC and DC were similar,with first recurrence to isolated distant sites in most patients with AC and DC (73.9%;AC,69.2%;DC,80.6%);the authors also reported that liver was the most affected distant site of recurrence (33.8%;AC,28.8%;DC,36.1%).In the present study,pancreaticoduodenectomy with regional lymph node dissection was performed in both the patients with AC and DC-II and the rate of recurrence at local sites such as the regional lymph nodes was lower than the rate of recurrence in distant lymph nodes.These results suggested that pancreaticoduodenectomy with regional lymph node dissection was effective not only in AC but also in DC-II.
The major limitations of the present study were the small sample size and the retrospective study design.Additionally,standard surgical procedures were not performed in some patients and the adjuvant chemotherapy indications and regimens were not standardized.Multicenter prospective studies with larger cohorts are necessary to clarify the prognosis and the LNM patterns in patients with DC-II and AC for the selection of appropriate surgical procedures with the best outcomes.
CONCLUSlON
There were no significant differences in prognosis and recurrence rate between the patients with DC-II and AC despite the more advanced tumor invasion in patients with DC-II than in those with AC.Metastases to N-He and N-Py were more frequent in patients with DC-II than in those with AC.
ARTlCLE HlGHLlGHTS
Research background
Few studies have compared the oncological and biological characteristics between ampullary carcinoma(AC) and cancer of the second portion of the duodenum (DC-II),although both tumors arise from anatomically close locations.
Research motivation
The lymph node metastasis (LNM) patterns and the optimal range of lymph node dissection in DC-II and AC remain controversial.
Research objectives
The present study aimed to elucidate differences in clinicopathological characteristics,especially the patterns of LNM,between AC and DC-II.
Research methods
This was a retrospective cohort study of 80 patients with AC and 27 patients with DC-II who underwent pancreaticoduodenectomy between January 1998 and December 2018 in two institutions.Clinicopathological factors,LNM patterns,and prognosis were compared between the two groups.
Research results
The rate of preoperative biliary drainage was significantly higher and the rates of digestive symptoms,ulcerative-type cancer,large tumor diameter,and advanced tumor stage were significantly lower in patients with AC than DC-II.There were no significant differences in prognosis,recurrence,and lymph node metastasis rates between the two groups,although hepatic and pyloric lymph node metastases were more frequent in DC-II than in AC.
Research conclusions
Although there were no significant differences in the prognosis and recurrence rates between the two groups,metastases to N-He and N-Py were more frequent in patients with DC-II than in those with AC.
Research perspectives
Lymph node dissection to N-He and N-Py may be omitted for AC,that is unlikely for DC-II.
FOOTNOTES
Author contributions:Nishio K designed the study and wrote the draft of the article.Kimura K and Kubo S contributed to interpretation of the data and the critical revision of the article content.All the other authors (Murata A,Ohira G,Shinkawa H,Kodai S,Amano R,Takemura S,Shimizu S,Kanazawa A and Ishizawa A) contributed to the data collection and interpretation and critically reviewed the article;All the authors have read and agreed to the article.
lnstitutional review board statement:This study was approved by the Ethics Committees of Osaka City University (approval No.2020-198) and Osaka City General Hospital (approval No.1910076) and was performed in compliance with the Declaration of Helsinki.
lnformed consent statement:All patients provided informed consent for using their data in this study according to the institutional regulations of the study sites.
Conflict-of-interest statement:All authors declare that they have no competing interests related to the manuscript.
Data sharing statement:No additional data are available.
STROBE statement:The authors have read the STROBE Statement - checklist of items,and the manuscript was prepared and revised according to the STROBE Statement - checklist of items.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Japan
ORClD number:Kohei Nishio 0000-0002-0480-7640;Kenjiro Kimura 0000-0001-9946-2624;Shogo Tanaka 0000-0002-5629-5691;Takeaki Ishizawa 0000-0002-9534-6973.
S-Editor:Liu JH
L-Editor:A
P-Editor:Liu JH
杂志排行
World Journal of Gastrointestinal Surgery的其它文章
- Preoperative blood circulation modification prior to pancreaticoduodenectomy in patients with celiac trunk occlusion:Two case reports
- Observational Study Development of a warning score for early detection of colorectal anastomotic leakage: Hype or hope?
- Disturbed passage of jejunal limb near esophageal hiatus after overlapped esophagojejunostomy following laparoscopic total gastrectomy
- Assessment of tumor markers CA 19-9,CEA,CA 125,and CA 242 for the early diagnosis and prognosis prediction of gallbladder cancer
- Recombinant human thrombopoietin treatment in patients with chronic liver disease-related thrombocytopenia undergoing invasive procedures: A retrospective study
- Comprehensive abdominal composition evaluation of rectal cancer patients with anastomotic leakage compared with body mass indexmatched controls