Effects of different fresh gas flows and different anesthetics on airway temperature and humidity in surgical patients:a prospective observational study
2022-11-05IremGumusOzcanOzkanOnalAysunOzdemirkanAliSaltalMehmetSar
Irem Gumus Ozcan, Ozkan Onal,2, Aysun Ozdemirkan, Ali Saltalı, Mehmet Sarı
1 Department of Anesthesiology and Intensive Care, Selcuk University Faculty of Medicine, Konya, Turkey
2 Anesthesiology Institute, Department of Outcomes Research, Cleveland Clinic Main Hospital, Cleveland, OH, USA
Abstract This study was aimed to investigate the effects of different fresh gas (oxygen + air) flow rates and different anesthetics on airway temperature and humidity when using the same anesthesia machine in patients undergoing general anesthesia.In this prospective, observational study, 240 patients with American Society of Anesthesiologists (ASA) I–II between the age of 18–65 years to be operated under general anesthesia were enrolled and divided into two groups according to the fresh gas flow rate (3–6 L/min).Each of the two main groups was further divided into three subgroups according to the administered anesthetic gases and drugs.The resulting six groups were further divided into two subgroups according to whether the heat and humidity exchanger filter (HME) was attached to the breathing circuit, and the study was carried out on a total of 12 groups.The temperature and humidity of the inspired air were recorded every 10 minutes using an electronic thermo-hygrometer.The inspired temperature and humidity were greater in patients ventilated at 3 L/min compared to the 6 L/min group and in HME (+) patients compared to HME (–), regardless of the type of anesthetics.HME application makes the air more physiological for the respiratory tract by increasing the temperature and humidity of the air regardless of the anesthetic agent.This study was approved by Ethics Committee Review of Selcuk University Faculty of Medicine (No.2017/261) in September 2017, and was registered in the Clinical Trial Registry (identifier No.NCT04204746) on December 19, 2019.
Key words:airway; breathing systems; equipment; fresh gas; general anesthesia; heated humidifier; humidity; temperature
INTRODUcTION
Before the inhaled air reaches the lungs, it is heated and moistened in the nose and upper respiratory tract.This physiological protective mechanism is bypassed when endotracheal intubation is applied to the patient.Dry and cold compressed gases cause heat and humidity loss in the respiratory tract,1thus causing the destruction of the cilia and mucous membranes in the drying respiratory tract, resulting in reduced mucociliary transport and intense secretion.1-5
Therefore, when the patient is under general anesthesia, pulmonary problems such as decreased pulmonary compliance, decreased residual capacity, increased pulmonary shunt, and eventually hypoxemia and atelectasis may occur.Preserving the humidity and heat of respiratory gases is the key to preventing these complications.4,6,7
An anesthetic circle system includes two humidity and heat sources:rebreathing of the exhaled air that the patient heats and humidifies, and water vapor and heat formed by the exothermic reaction of the carbon dioxide (CO2) absorber.8The rate of fresh gas flow is the most important determinant of rebreathing.9Reventilated semi-closed systems can be used with low or high fresh gas flow rates according to demand and clinical experience.10,11There is no precise information about the optimal fresh gas mixture (oxygen + air) flow rate and ratio that should be applied in patients operated under general anesthesia.
Different fresh gas flow rates under general anesthesia are used in the authors’ hospital and globally.In this study, we aimed to investigate whether two different fresh gas flow rates, which are routinely applied in patients undergoing endotracheal intubation, affect the airway temperature and humidity.The primary outcome was to evaluate the effect of two different fresh-gas flow rates on airway temperature and humidity in intubated patients.The secondary outcome was to evaluate the effect of different anesthetic gases and drugs on airway temperature and humidity when intubated patients were under general anesthesia.
sUBJEcTs AND METHODs
study design
This prospective, randomized, single-blind, observational study was registered in the ClinicalTrials.gov (identifier No.NCT04204746) on December 19, 2019, and the study followed the relevant requirements of the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) statement (Additional file 1).Ethics Committee of Selcuk University Faculty of Medicine approval was taken (approval No.2017/261) in September 2017 (Additional file 2).The writing and editing of the article was performed in accordance with the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) Statement.After a signed informed consent was obtained, patients aged between 18–65 years, who were assessed to be at level I–II according to the rating scale of physical status by the American Society of Anesthesiologists (ASA) and underwent endotracheal intubation and general anesthesia were involved in the study between September 2017 and January 2018 at Selcuk University Faculty of Medicine Department of Anesthesiology and Reanimation.The evaluator was blind to the grouping.
Participants and study groups
Patients with the following conditions were excluded from the study:planned to emergency or trauma surgery, had a history of heart and thyroid disease, pulmonary parenchymal disease such as lung malignancy or chronic obstructive pulmonary disease, smoking, alcohol, or drug addiction, body mass index (BMI) greater than 30 kg/m2, fever and infection, used drugs that could affect thermoregulation, had more bleeding than expected (> 5 mL/kg), pregnancy or postpartum, mental insufficiency, and refused to participate the study.Patients were subjected to routine electrocardiography (DII and V5), peripheral oxygen saturation, non-invasive arterial blood pressure (systolic and diastolic), and axillary temperature monitoring.Fluid deficiencies were restored with room-temperature liquids according to the patient’s requirement.All patients were warmed with heater blankets that were placed under the patient and set to 40°C (Medwarm, Istanbul Medical, Istanbul, Turkey).While all of the patients included in the study were randomized by a resident physician (IGO) into study groups using a randomization application.Our study involved 12 groups with 20 patients in each group and a total of 240 patients (Figure 1).The patients were randomized into two main groups according to the applied fresh gas flow rate (3 and 6 L/min;n= 120).Each two main groups were randomized into subgroups according to the administered anesthetic gases and drugs as follows:sevoflurane + remifentanil (n= 40), desflurane + remifentanil (n= 40) or propofol + remifentanil (total intravenous anesthesia, TIVA;n= 40).These six subgroups were further randomized into two subgroups (n= 20) according to whether the heat and humidity exchanger (HME) filter (Disposet, Disposet Medical, Ankara, Turkey) was attached to the breathing circuit or not.
The inspired temperature (IT) and relative humidity (RH) of the inspired gases were measured using a quick reply thermohygrometer (Loobex Digital HTC-2, Loobex Medical, Istanbul, Turkey).A thermo-hygrometer climatic test chamber (NUVE, NUVE Medical, Ankara, Turkey) was used to calibrate the thermo-hygrometer.RH, IT, axillary body temperature, and end-tidal carbon dioxide measurements were recorded at 10, 30, 60, and 90 minutes.Inspired absolute humidity (IAH) according to the recorded values was calculated using the following formula:IAH:(3.939 + 0.5019T + 0.00004615T2+ 0.0004188T3) × RH/100.T indicates temperature.
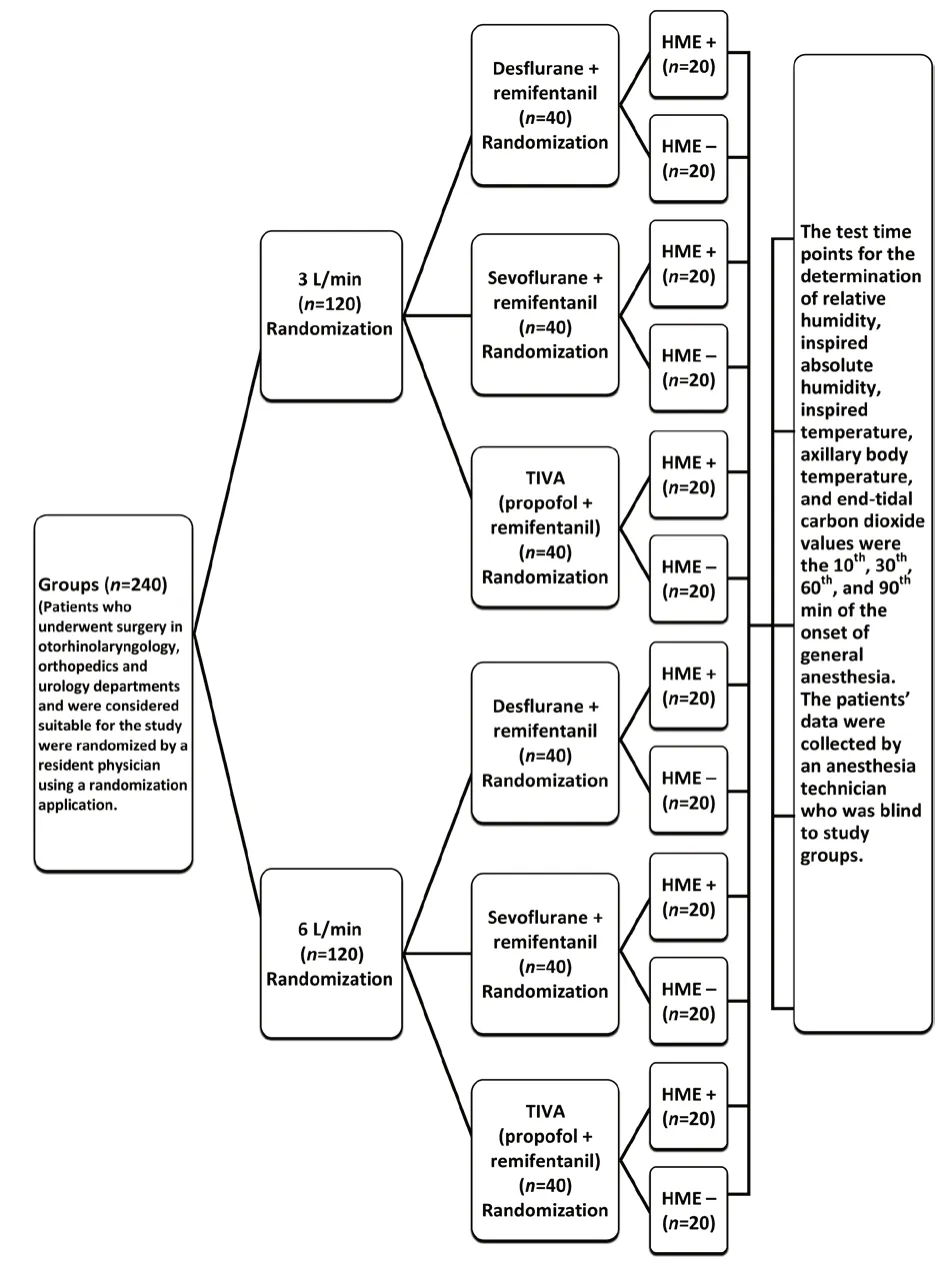
Figure 1:Assignment of patients included in the study according to study design.
Patients were under routine general anesthesia using the following for anesthesia induction:1–3 mg/kg propofol (Propofol, Fresenius Kabi, Istanbul, Turkey) 2–3 μg/kg fentanyl (Fentanyl, Johnson and Johnson, Istanbul, Turkey) and 0.5–1 mg/kg rocuronium (Esmeron, Merck Sharp Dohme, Istanbul, Turkey).Following the tracheal intubation, the lungs were mechanically ventilated for the whole operation period, and inhalation anesthesia was ensured with sevoflurane (Sevorane, Abbott, Istanbul, Turkey) (1.25–1.75%) and desflurane (Suprane, Baxter, Istanbul, Turkey) (5.5–6%) and TIVA was ensured with propofol (2%; Fresenius Kabi, Istanbul, Turkey) 5–8 mg/kg/hour and remifentanil (Ultiva, GlaxoSmithKline, Istanbul, Turkey) 0.25–0.5 μg/kg/min infusion in a mixture of oxygen with a ratio 2:1.Lung volume control was provided by an Aisys anesthesia workstation (Datex Ohmeda, Louisville, KY, USA).Respiratory rates were adjusted to keep end-tidal carbon dioxide concentrations between 30–35 mmHg.
Randomization
Patients enrolled in the study were randomly assigned in 1:1 ratio by the resident physician (IGO) using an application of number and letter random generator.All data were collected by an anesthesia technician who was unaware of the study groups and the type of device used in the intubation procedure.
statistical analysis
Study protocol, statistical analysis plan and raw data can be shared individually if there is a valid reason.The statistical methods of this study were reviewed by Assist.Prof.Adnan Karaibrahimoglu from Department of Bioistatician, Suleyman Demirel University.Statistical analysis of the study was performed using SPSS 20.0 software (IBM Inc., Armonk, NY, USA).Defined criteria for all variables were calculated.Categorical variables were presented using frequencies and percentages, and numerical variables were tabulated using mean ± standard deviation (SD) (median).The normal distribution suitability of the measured results was analyzed using the Kolmogorov-Smirnov test.Non-parametric tests were used for repeated measures and independent group comparisons as the majority of the measured results were not normally distributed.Friedman’s two-way analysis of variance, Mann-WhitneyUtest for two independent groups, and Kruskal-Wallis’s variance analysis for multiple groups were favored for comparing repeated measures.Bivariate repeated measures covariance analysis was applied to see the effects of demographic characteristics such as age, gender, and BMI.Tukey’s honestly significant differencepost hoccomparison methods were used for binary comparison and repeated covariance analysis for non-parametric methods.The determination of the relationships between variables was achieved by Monte Carlo corrected chi-square analysis.Statistical values ofP< 0.05 were considered significant.
REsULTs
A total of 240 patients in 12 groups, 150 (62.5%) male and 90 (37.5%) female, were included in the study; however, sex distribution according to anesthesia methods for the two different fresh gas streams was not statistically significant (3 L/min:P= 0.772; 6 L/min:P= 0.576).There were no differences in terms of age (P= 0.343), height (P= 0.823), weight (P= 0.530) and BMI (P= 0.203) for the HME (+) and HME (–) patients who received 3 L/min fresh gas flow and were under anesthesia composed of desflurane or TIVA.However, when the HME (–) group was compared with the HME (+) group in which patients received 3 L/min fresh gas flow and sevoflurane for anesthesia, body weight was statistically different (P< 0.05).
The IT and IAH values of the patients who received all three anesthesia methods were statistically different at each time interval (P< 0.05) and were higher in the HME (+) group using 3 L/min fresh gas flow (Figure 2).For the HME (+) and HME (–) groups in which patients received 3 L/min fresh gas flow and had anesthesia composed of desflurane, sevoflurane, or TIVA, there were statistically significant differences in IT and IAH values measured at 10, 30, 60, and 90 minutes (P< 0.001).Generally, the IT and IAH values increased over time (Figure 2).
While the weight and BMI values were significantly different (P< 0.05) for the HME (+) and HME (–) groups who received 6 L/min fresh gas flow and had anesthesia composed of desflurane, mean ages were similar.Weight and BMI were greater for the HME (+) group in which patients received 6 L/min fresh gas flow.There were no statistically significant differences in terms of age, weight, height and BMI between the groups who received anesthesia composed of sevoflurane and TIVA.IT and IAH values measured at 10, 30, 60, and 90 minutes were statistically different (P< 0.001) for all HME (+) and HME (–) groups in which patients received 6 L/min fresh gas flow and had anesthesia composed of desflurane, sevoflurane or TIVA.Greater IT and IAH values were obtained in the HME (+) group than the HME (–) group.Generally, as time increased, the measured values increased (Figure 2).
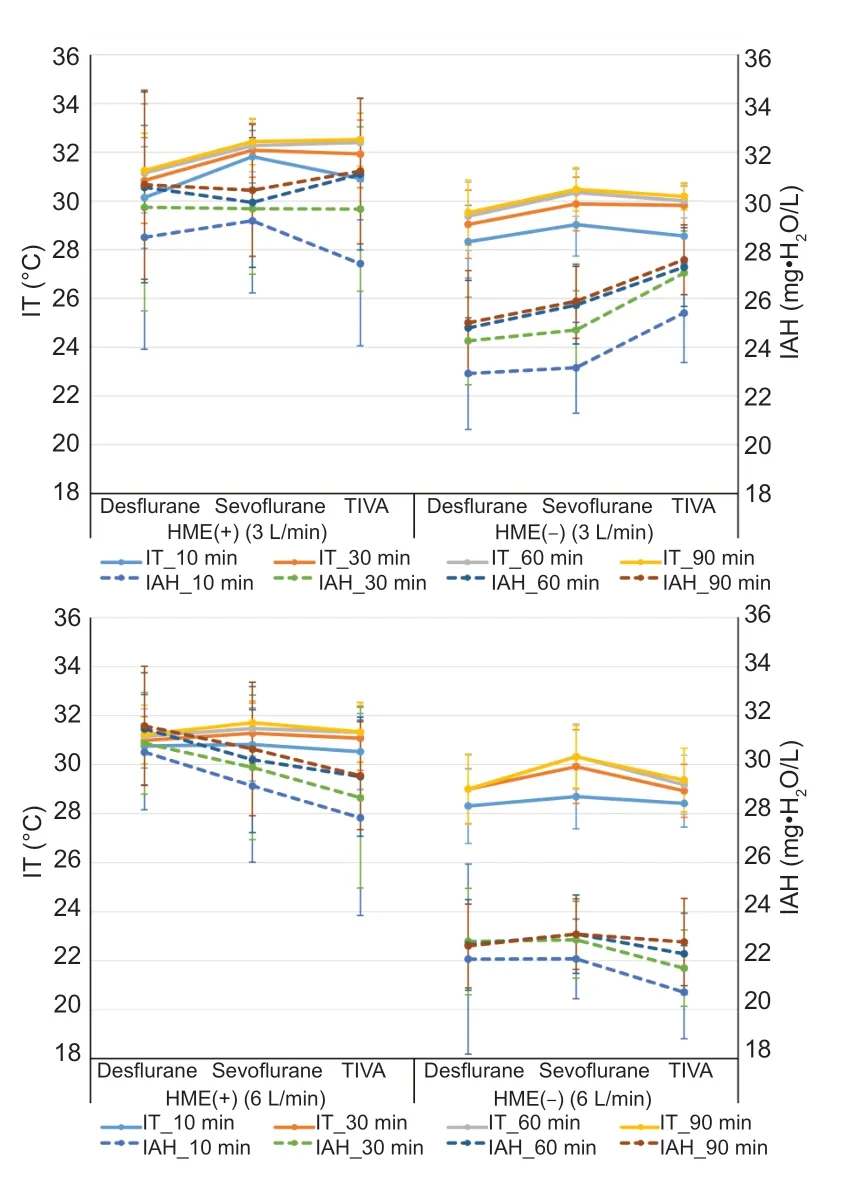
Figure 2:Comparison of groups in which patients received 3 and 6 L/min fresh gas flow under desflurane, sevoflurane, and TlVA anesthesia in terms of lT and lAH values, depending on whether HME (+) or HME (–).
Patients in the HME (+) and HME (–) groups who received 3 L/min fresh gas flow and had anesthesia composed of desflurane, sevoflurane, or TIVA were compared, and there was no statistically difference in terms of age (P= 0.58), weight (P= 0.387), height (P= 0.754) and BMI (P= 0.703).In the HME (+) group, the measured IT values were statistically different (P< 0.05).The measured IT values under desflurane anesthesia were lower than those under sevoflurane or TIVA anesthesia.There was no statistically difference in measured IAH values in the HME (+) group (Figure 3).
Patients in the HME (–) group who received 3 L/min fresh gas flow had measured IT values at 60 and 90 minutes were statistically different (P< 0.05).Measured IT values were higher in the patients under sevoflurane.Measured IAH values were statistically different at all times (P< 0.05), which were lowest in the group under desflurane, and higher in the groups under sevoflurane and TIVA (Figure 3).Patients in the HME (+) and HME (–) groups who received 6 L/min fresh gas flow and had anesthesia composed of desflurane, sevoflurane, or TIVA were compared (Figure 3).
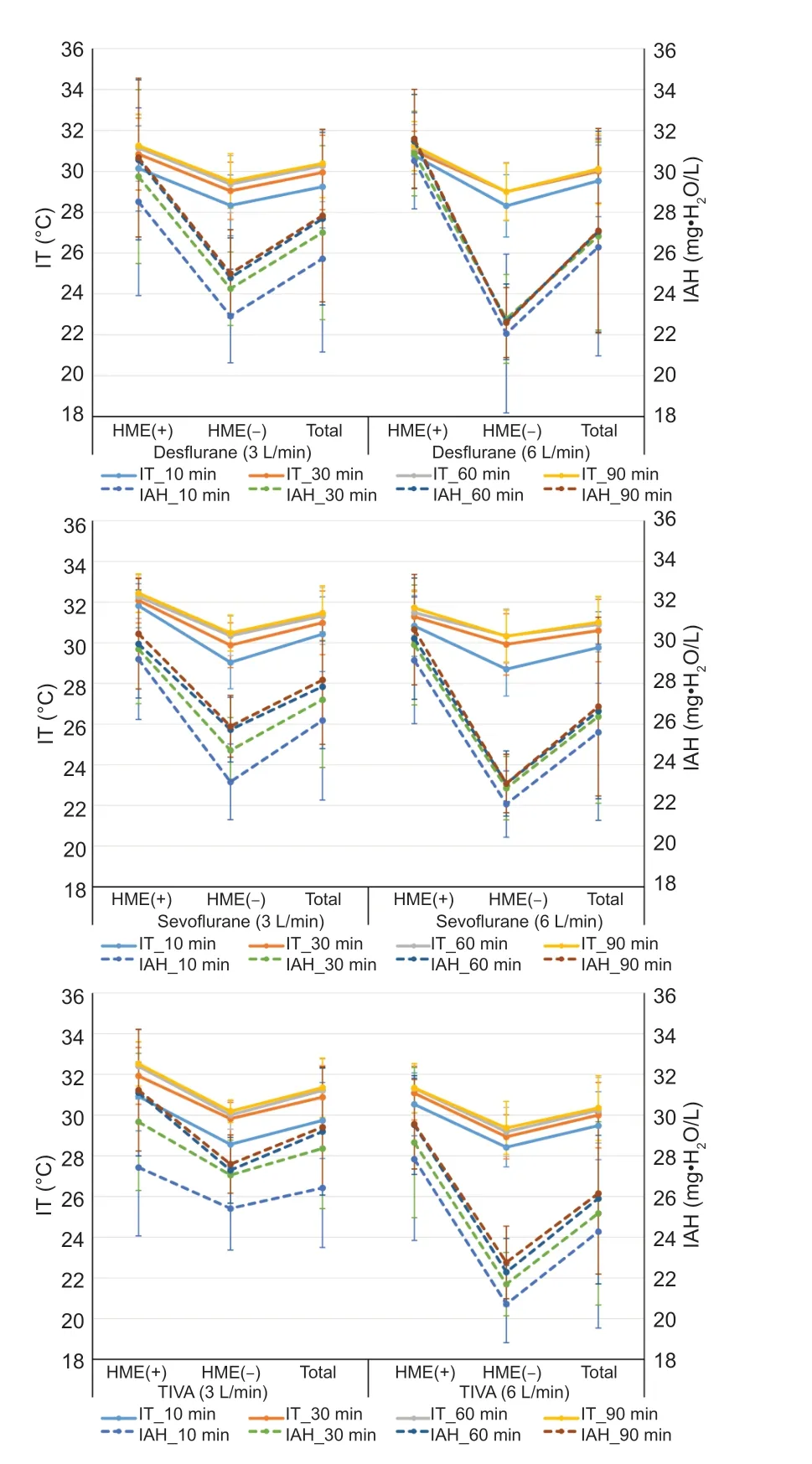
Figure 3:Comparison of patients under desflurane, sevoflurane, and TlVA anesthesia within their own groups in terms of lT and lAH values, depending on whether HME (+) or HME (–) and according to the application of 3 and 6 L/min fresh gas flow.
In the HME (+) group, compared with demographic characteristics, there was a statistical difference only in weight that was higher in the group under desflurane.There was no statistical difference in measured IT values in the HME (+) group, but measured IT values were higher for patients under sevoflurane.The measured IAH values at 90 minutes were statistically significant (P< 0.05).The measured IAH value was highest in the group under desflurane, and lower in the groups under sevoflurane and TIVA (Figure 3).
In the HME (–) group, only age that is one of the demographic characteristics was statistically different and it was lower in the sevoflurane group.Patients in the HME (–) group who received 6 L/min fresh gas flow had statistically significant measured IT values (P< 0.05) at 30, 60, and 90 minutes; the measured IT values were higher in the group under sevoflurane.Measured IAH values at 10 and 30 minutes were statistically different (P< 0.05), and these values were higher in the sevoflurane group (Figure 3).
Patients in the HME (+) and HME (–) groups who had anesthesia composed of desflurane, sevoflurane, or TIVA were compared according to fresh gas flow applications of 3 and 6 L/min (Figure 4).In the HME (+) group which desflurane anesthesia was applied, there were statistically differences in age (P= 0.036) and BMI (P= 0.03) characteristics and there were higher at group which 6 L/min fresh gas flow applied.When the fresh gas flow rates were compared for patients in the HME (+) group under desflurane, there was no statistical difference in terms of measured IAH (P= 0.074) and IT (P= 0.785) values.In the HME (–) group in which desflurane anesthesia was applied, there was no statistical differences in terms of age (P= 0.076), weight (P= 0.171), height (P= 0.896) and BMI (P= 0.3).When the fresh gas flow rates were compared for patients in the HME (–) group under desflurane, measured IAH measurements showed statistically significant differences (P< 0.05) at 30, 60, and 90 minutes, which were higher in the 3 L/min fresh gas flow group.In the HME (–) group under desflurane anesthesia, when the fresh gas flows were compared, there was no statistically differences in IT values.
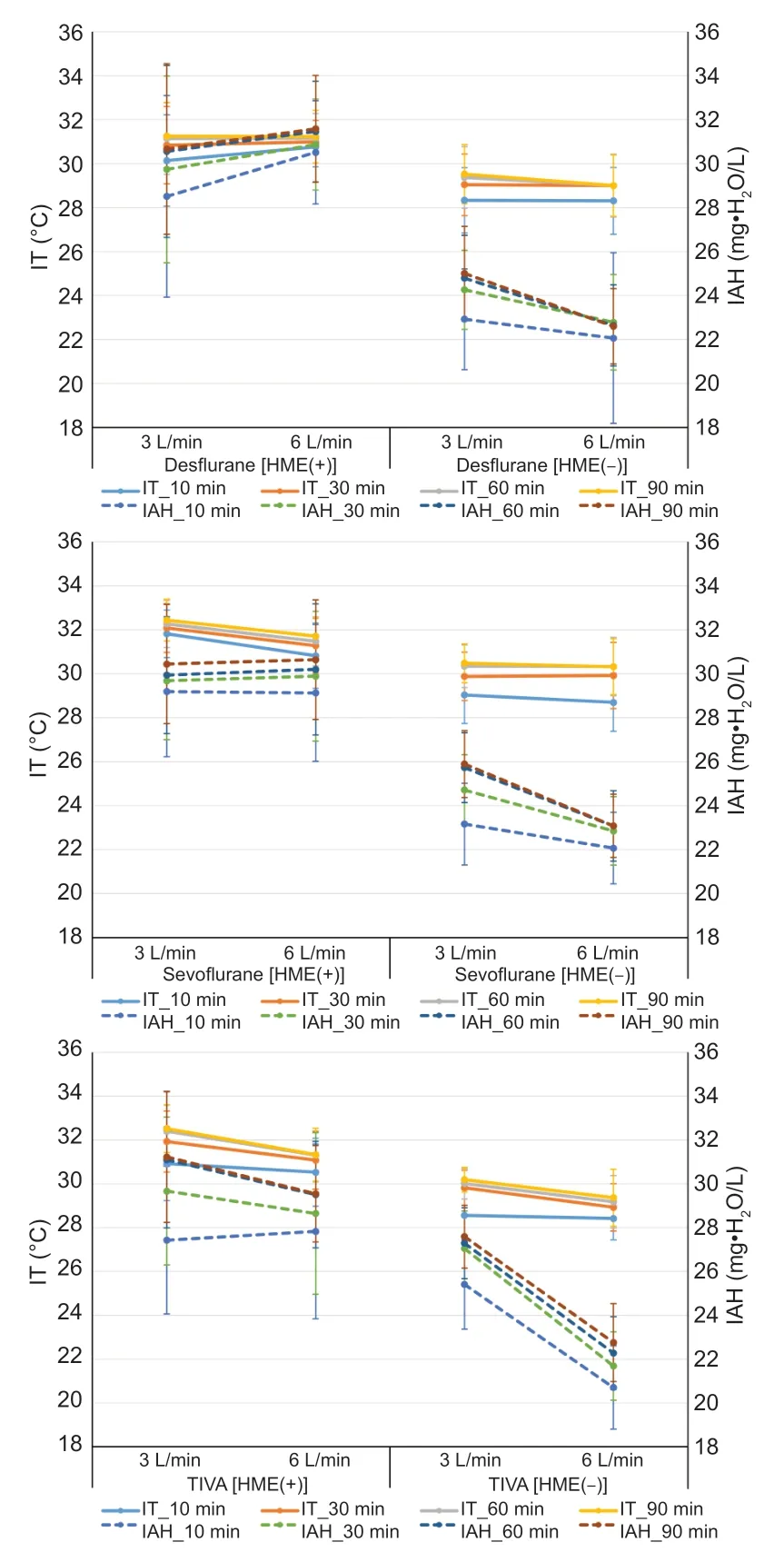
Figure 4:Comparison of patients under desflurane, sevoflurane, and TlVA anesthesia within their own groups in terms of lT and lAH values, according to the application of 3 and 6 L/min fresh gas flow and whether HME (+) or HME (–).
In the HME (+) group in which sevoflurane anesthesia was applied, there was statistically difference in BMI and it was higher at group which 6 L/min fresh gas flow applied.When fresh gas flow rates were compared for patients in the HME (+) group under sevoflurane, the measured IAH values were not different statistically; however the measured IT values had statistically significant differences (P< 0.05), and measured IT values were higher in the 3 L/min fresh gas flow group.In the HME (–) group which sevoflurane anesthesia was applied, there was a statistical difference in height which is one of the demographic characteristics and it was higher when 3 L/min fresh gas flow was applied.When the fresh gas flow rates were compared for patients in the HME (–) group under sevoflurane, the measured IAH values were statistically different (P< 0.05) at 30, 60, and 90 minutes, and the values were higher in the 3 L/min fresh gas flow group.In the HME (–) group under sevoflurane anesthesia, there was no statistically differences in IT values (Figure 4).
In the HME (+) and HME (–) groups which TIVA anesthesia was applied, there was no statistical difference in demographic characteristics.When fresh gas flows were compared for patients in the HME (+) group under TIVA, measured IT values at 30, 60, and 90 minutes and measured IAH values at 60 minutes were statistically different (P< 0.05); all values were higher in the 3 L/min fresh gas flow group.For patients in the HME (–) group under TIVA, IT and IAH values at 30, 60, and 90 minutes were statistically different (P< 0.05), and the values were higher in the 3 L/min fresh gas flow group (Figure 4).
DIscUssION
As the fresh gas flow during anesthesia increases, the humidity and temperature of the patient’s airway decrease.Low humidity and temperature can also lead to dysfunction in the epithelium of the patient's trachea and bronchi.The HME used in anesthesia respiratory circulation keeps the humidity and temperature of the patient’s airway near to the physiological values like low fresh gas flow rate.7,12-19There is no consensus on the sufficient temperature and AH of the inspired gas pending mechanical ventilation handling an endotracheal tube.12However, anesthesiologists generally determine the rate of fresh gas flow to patients according to their clinical experience, surgical requirements and habits; they do not care whether an HME is used or not.High fresh gas flows of 3 and 6 L/min are routinely used in the authors’ operating room.This study aimed to determine whether commonly employed fresh gas flows and the use or non-use of an HME affect the airway humidity rates and temperature values of patients under general anesthesia.The advantages of low fresh gas flow anesthesia include lower costs and preventing environmental pollution.Gas humidity levels are also higher in low fresh gas flows than other fresh gas flow techniques, and heat loss is minimized.20Thus, the physiological environment required for trachea and bronchus is better preserved.Heating the inhaled gases also provides an advantage in preventing postoperative hypothermia.
However, in the case of low-flow anesthesia, the inhalation of O2-depleted gas significantly reduces the concentration of O2in the inspected gas.This should be taken into account when adjusting the O2concentration.Hypoxia, CO2deposition, accumulation of harmful metabolites of volatile anesthetics, volatile anesthetic titration takes a long time are the disadvantages of low-flow anesthesia.For this reason, inspired O2, inhalation anesthetics and CO2concentration, airway pressure and exhaled volume should be monitored.9
Previous studies suggest that the minimum target for IAH of the inhaled gases to prevent respiratory tract dehydration is 20 mgH2O/L for short-term use in general anesthesia or 30 mgH2O/L for prolonged use in intensive care.3,4,21,22When working with minimal fresh gas flow (≤ 0.5 L/min), at least 20 mgH2O/L was reached at 60 and 120 minutes after the respiratory cycle was connected to the patient.Similarly, an inspiratory RH of at least 20 mgH2O/L was obtained in all studies with low fresh gas flow (0.6–1.0 L/min) 120 minutes after the respiratory cycle circuitry was applied to the patients.7,9,13,14,20-24When IAH values measured at 10, 30, 60, and 90 minutes were considered in this study, IAH levels of at least 20 mgH2O/L were reached under anesthesia in all HME (–) groups.The fact that all patients in the HME (–) groups reached the minimum humidity content despite high fresh gas flow rates shows that fresh gas flow rates of 3 and 6 L/min are reliable for operations that will last for 90 minutes and less.However, the epithelium of a patient’s air should be examined in a laboratory environment to reach a definite conclusion.Similar to most studies, inspiratory RH values in our study were close to 30 mgH2O/L independent of fresh gas flow when using an HME or time to connect to a patient’s respiratory circuit.Therefore, as also found in this study, when HME filters are used in adult patients, the choice of different fresh gas flows does not create significant differences in airway humidity content.In a study conducted with anesthesia machines (Drager Cato and Aestiva/5 Datex-Ohmeda) of different designs, a fresh gas flow of 0.5 L/min or 1 L/min was selected and compared with the inspired IAH values according to HME (+) and HME (–).14Anesthesia treatment was performed with 40%O2, 60% NO2mixture, and sevoflurane.With the Drager Cato machine, IAH values measured at 120 minutes for 0.5 and 1 L/min currents were different for the HME (+) and HME (–) groups; higher values were obtained in the fresh gas flow of 0.5 L/min.With the Datex Aestiva/5 machine, measured IAH values at a fresh gas flow rate of 0.5 L/min were found higher in both cases.However, the IAH measured by the Drager Cato machine for the HME (+) and HME (–) groups and at both flow rates was significantly higher than the IAH measured by the Datex Aestiva/5 machine.The authors noted that this result was compatible with the heating plate in the Drager Cato design.In contrast, this study used an Aisys anesthesia workstation (Datex Ohmeda), but did not record data at 120 minutes; measurements were limited to 90 minutes.In addition, this study included more patients than the other study.This study also used higher fresh gas flows of 3 and 6 L/min and different anesthesia methods.When the values at 60 minutes (which were measured in both studies) were compared, the IAH values obtained in the HME (+) group on the Drager Cato instrument were higher than the measured IAH values in all groups of our study.Measured IAH values obtained in the HME (–) group using the Drager Cato machine and 0.5 L/min fresh gas flow rate were higher in this study than in the HME (+) group.This result shows that the rates of fresh gas flow and the design of the anesthesia machine are more important than the use of an HME filter in terms of measured IAH values.The measured IAH values obtained with HME (–) and a 1 L/min fresh gas flow were higher than the other HME (–) groups.When the Datex Aestiva/5 instrument was used, the measured IAH values obtained when HME was used were similar to the values obtained in this study’s HME (+) groups.However, the measured IAH values in that study were significantly lower than the measured IAH values in this study’s HME (–) group.This result shows that the anesthesia machine used changed the humidity of the air in the patient and that the Aisys anesthesia machine used in this study moisturizes the patient’s air better than the Aestiva/5 machine.In another study using a Servo 900C (Siemens-Elema, Nurnberg, Germany) anesthesia workstation, fresh gas flow rates of < 1, 2, and 5 L/min were selected; HME (+) and HME (–) recipients for each of these groups were also compared.16At 60 minutes in the HME (+) group, the IAH values were similar and higher than in the HME (–) group.In HME (–) group, however, IAH values decreased as fresh gas flow rates increase.Similar to that study, the measured IAH values of the HME (+) groups receiving fresh gas flow rates between 3 and 6 L/min in the present study were not statistically different; close values were obtained.There was also a statistically significant difference in IAH values between the HME (+) and HME (–) groups in the present study; higher IAH values were obtained in the HME (+) group.The decrease in IAH caused by the increase of fresh gas flow in HME (–) groups was statistically significant in the present study.While the measured IAH values for the HME (+) group were similar in the Servo 900C study and the present study, higher IAH values for the HME (–) group were found in the present study.This result shows that the Aisys anesthesia machine used by the authors may be better at retaining airway humidity than the Servo 900C (Siemens-Elema) anesthesia machine.In another study using a Servo 900C anesthesia workstation, fresh gas flows of 1, 3, and 6 L/min were compared for anesthesia composed of isoflurane and a mixture of 60% NO2+ 40% O2.17The IAH values in the HME (+) groups in the present study were consistent with the values in the HME (+) groups of that study.In that Servo 900C study, while the IAH values measured in the HME (–) group decreased as the fresh gas flow amount increased, the IAH values obtained were lower than the IAH values in the present study.Another study investigated the effect on IT and IAH of using an HME on patients under isoflurane anesthesia with a 1 L/min fresh gas flow (0.5 L/min O2, 0.5 L/min NO2) and using a Drager Primus anesthesia workstation.18The measured IAH of the HME (+) group was similar to the IAH value obtained in the present study.The measured IAH value of the HME (–) group was similar to the IAH value obtained for the 6 L/min fresh gas flow group of the present study.These results show that the design of the anesthesia machine used is as important as the fresh gas flow rate and whether or not an HME is used.IAH values were reported in another study that used a Drager Fabius anesthesia workstation, TIVA anesthesia, and a 1 L/min fresh gas flow.19While that study used a 1 L/min fresh gas flow like the study that used a Drager Primus anesthesia workstation, it used TIVA anesthesia instead of isoflurane anesthesia.18When these two studies were compared, the values obtained in the HME (–) groups were the same, whereas the values obtained in the HME (+) groups were lower than in the study that used TIVA anesthesia.When that Drager Fabius/TIVA study was compared with the patients under TIVA in the present study, lower IAH values were found in the present study despite being administered at a lower fresh gas flow rate.This result shows that different anesthesia workstations, as well as TIVA and inhalation anesthesia, can achieve different IAH values.In another study used an Acoma CT-7FII (Acoma, Japan) anesthesia workstation, fresh gas flow rates of 2 and 4 L/min, and sevoflurane anesthesia.25In HME (–) groups using fresh gas flow rates of 2 and 4 L/min, the present study obtained lower values than the IAH values measured of the Acoma study for patients under sevoflurane.This difference may also be attributable to the difference in the anesthesia workstation.Another study using a Servo 900C anesthesia workstation and fresh gas flows rates of < 1, 2, 5 L/min reported that IT values were not statistically different for HME (+) patients.However, higher IT values were found compared to HME (–) groups.16At the same time, the IT values of the HME (–) group decreased further as the flow of fresh gas increased.A further study measured values when using a Servo 900C anesthesia workstation, anesthesia composed of a mixture of isoflurane and 60% NO2+ 40% O2, and fresh gas flows of 1, 3, and 6 L/min.17When the IT values for a 1 L/min fresh gas flow were compared to another study that used a Drager Primus anesthesia workstation, isoflurane anesthesia method and fresh gas flow of 1 L/min (0.5 L/min O2, 0.5 L/min NO2), the measured IT values for the Drager Primus anesthesia workstation were slightly lower.17,18This result suggests that anesthetic workstation design is as effective as using an HME.In our study, when using Servo 900C ventilator (Siemens-Elema) anesthesia workstation was compared with fresh gas flow of 3 and 6 L/min, with the same fresh gas flow, higher IT were obtained in groups without HME.In the HME (+) group, similar IT values were obtained.For the IT values of all groups in the present study, the presence of HME (+) and HME (–) showed statistically significant differences; higher IT values were obtained in HME (+) group.The IT values measured in groups with a fresh gas flow rate of 3 L/min were higher than the IT values measured in groups with a fresh gas flow rate of 6 L/min; thus, the use of an HME and a lower fresh gas flow rate increases the measured IT values.One study showed that low IAHs could be tolerated for short periods without causing dysfunction of the tracheobronchial epithelium.6For this reason, authors have shown that there is no need to use additional HME in respiratory circulation during short-term anesthesia.22However, authors showed that the airway mucosa of critically ill patients was less tolerant of thermal stresses and noted that this group of patients need higher IAH.6The concomitant viscousness of epithelial secretions can cause to retention of sputum and eventually make prone patients to ventilator-associated pneumonia or endotracheal tube blockage.26Therefore, using an HME in the respiratory tract is recommended in patients with respiratory tract dysfunction, especially during prolonged operations using high fresh flow or requiring long-term postoperative mechanical ventilation.22
In the early stages of the surgical procedure, HME, which properly moisturizes and warms the inhaled gases, has been shown to be advantageous in some studies.25In our study, the required minimum IAH value was obtained although no filter was used in 90 minutes lasting operations.Few studies have investigated patient postoperative respiratory outcomes.One study compared the effects of low (1 L/min) and high fresh-gas flow (3 L/min) rates on mucociliary clearance (using saccharin transit time) and pulmonary function.7In the high fresh gas flow group, postoperative forced vital capacity and forced expiratory volume were found to be significantly lower after one hour, and the saccharin clearance time was found longer than the low fresh gas flow group.It has been suggested that respiratory functions and mucociliary clearance were better preserved with low-flow anesthesia.The most important limitations of the present study are blindness, lack of randomization, and the failure to examine patient airway epithelium in a laboratory environment.Humidity and temperature measurements were predefined intermittently and limited to 90 minutes; longer duration effects were not assessed.Another limitation is that only 3 and 6 L/min fresh gas flows were compared; minimal and low fresh gas flows were not used.Also, IAH and IT measurements were not made at the isothermal saturation point.Finally, pediatric and geriatric patients were not included in the study.
In conclusion, humidity and temperature protection on the patient respiratory system depends on a variety of factors, including the amount of fresh gas, and use or no use of HME, the type of ventilator, the type of anesthetic drugs, respiratory system structure, and patient demographic characteristics.For patients with general anesthesia, a low fresh gas flow should be used and HME should be fitted.And further studies should be carried out to focus on different fresh gas flows and long-term procedures in different age groups.
Acknowledgements
We would like to thank Anesthesia Technician Esra Acar for collecting the data of the study.
Author contributions
Study conception and design, and data collection, analysis and interpreting:IGO, OO, MS, AO, AS; manuscript writing, and revision:IGO, OO, AO, MS.All authors approved the final version of the manuscript.
conflicts of interest
This study was presented at Department of Anesthesiology and Reanimation, Selcuk University Faculty of Medicine as a thesis by Dr.Irem Gumus Ozcan.The authors declare that they have no conflict of interests.
Open access statement
This is an open access journal, and articles are distributed under the terms of the Creative Commons AttributionNonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.©Article authors (unless otherwise stated in the text of the article) 2022.All rights reserved.No commercial use is permitted unless otherwise expressly granted.
Additional files
Additional file 1:STROBE checklist.
Additional file 2:Hospital Ethics Approval.
杂志排行
Medical Gas Research的其它文章
- Anesthesiologists and burnout:what are we missing?
- spuriously low end tidal carbon dioxide in capnometry:Nafion tube malfunction in end tidal carbon dioxide module blamed for near mishap!
- In vivo microelectrode monitoring of real-time hydrogen concentration in different tissues of rats after inhaling hydrogen gas
- Color change after tooth bleaching with ozone and 10% ozonized carbamide peroxide for in-office use
- Hydrogen-rich bath with nano-sized bubbles improves antioxidant capacity based on oxygen radical absorbing and inflammation levels in human serum
- Comparative analgesic, hemodynamic, pain and duration of sensory and motor block effects of dexmedetomidine, granisetron, and nitroglycerin added to ropivacaine in intravenous anesthesia for forearm surgeries:a randomized clinical study