Herbal medicine in treatment of dysmenorrhea:a systematic review
2022-10-14HamidrezaSheikhRoshandelRominaNegariNamaghiFatemehGhadimiZohrehPourAhmadSajjadGhasemzadehNedaMoghariZadehRoksanaMirkazemi
Hamidreza Sheikh Roshandel,Romina Negari Namaghi,Fatemeh Ghadimi,Zohreh Pour Ahmad,Sajjad Ghasemzadeh,Neda Moghari Zadeh,Roksana Mirkazemi*
1Research Institute of Nutritional Sciences and Traditional Medicine Ta'm Asrar,Tehran,Iran.2Farzanegan Nik Andish Institute for the Development of Knowledge and Technology,Tehran,Iran.3Faculty of Nutrition,Tabriz University of Medical Science,Tabriz,Iran.4Department of Cultural Sociology,Faculty of Humanities,Islamic Azad University Kish International,Kish Island,Iran.5Emam Hossein Hospital,Iran Medical Science University,Tehran,Iran.
Abstract Objective:Herbal medicine has been a standard treatment for primary dysmenorrhea in different cultures and countries,and multiple studies have shown its possible positive effect on pain relief.This systematic review of the literature was conducted to assess different types of herbal medicine used to treat primary dysmenorrhea and evaluate the effectiveness of these medicines.Methods:This study systematically reviewed published articles on herbal medicine treating primary dysmenorrhea for 10 years(2011–2021),using Preferred Reporting Items for Systematic Reviews and Meta-Analyses(PRISMA)guidelines.In February 2022,international credible scholarly databases were searched.Also,the references of selected articles were hand searched to find relevant studies.Based on the search syntax,the search guideline was first defined for the PubMed database and was later revised according to each database’s specific framework of search method.The studies were included if they were either clinical trials or Quasi-Experimental,published in English or Persian between 2011 to 2021.Grey literature,unfinished studies,and studies without well-defined primary dysmenorrheal participants were excluded.Results:Seventy-three studies investigated the effectiveness of a total of 44 plants and plant combinations(35 single plants and 9 combinations of plants)on primary dysmenorrhea of which only one study did not report a significant positive effect.Ginger was the most investigated plant.Eight studies assessed the effects of ginger alone,and four studied the combination of ginger with other plants,all of them showed significant effects but one study.Nine studies investigated the effects of either fennel or its combination,five studies were on chamomile and three studies were related to lavender.Overall,all of them,except one,reported the positive effect of herbal medicine on primary dysmenorrhea.Conclusions:Different herbal medicine has been used to treat primary dysmenorrhea,significantly reducing pain intensity or duration or bleeding severity or duration.
Keywords:primary dysmenorrhea;herbal medicine;plant;plant extracts;clinical trial;systematic review
Highlights
1.This study systematically reviewed published articles on herbal medicine in treating primary dysmenorrhea for a duration of 10 years(2011–2021).
2.In this investigation,the studies that were the clinical trial or Quasi-Experimental,published in English or Persian in duration between 2011 to 2021 and did not be Grey literature,unfinished studies,or related to second dysmenorrheal were included.
3.Overall,73 articles were investigated and the effect of herbal medicine on primary dysmenorrhea was categorized into five groups;reduction in pain intensity,pain duration,menstrual bleeding,bleeding duration and alleviating dysmenorrhea symptoms.
4.Different herbal medicine has been used for treatment of primary dysmenorrhea,which showed significant effect on reducing pain intensity or duration or bleeding severity or duration.
Background
Dysmenorrhea is defined as severe and frequent cramps and pain in the lower abdomen during menstruation.It sometimes causes low back pain,pain radiating down the legs,nausea,fatigue,headache,irritability,dizziness,vomiting,diarrhea,weakness and even fainting.There are two categories of dysmenorrhea:primary and secondary.Primary dysmenorrhea is not due to any physical causes or organic disease;secondary dysmenorrhea is caused by pelvic pathology[1,2].
Although primary dysmenorrhea is a common problem in women of reproductive age,which usually begins in adolescence,it remains underreported,underdiagnosed and undertreated in many cases,even if it leads to activity restriction[3,4].
The cause of primary dysmenorrhea is unknown,but the hyper-production of uterine prostaglandins,particularly of PGFand PGFis believed to be responsible.Dysmenorrhea can have multiple risk factors,including heavy and long-lasting menstrual bleeding,nulliparity,smoking,anxiety,depression,“younger age,low body mass index(BMI),perimenstrual somatic complaints,pelvic infections,previous sterilization,somatization,psychological disturbance,genetic influence and a history of sexual assault[2,5,6].”
Some studies estimated the prevalence of dysmenorrhea between 28% and 71.7% globally,while others reported an even higher rate[6].They indicated that between 16% and 91% of women of reproductive age have dysmenorrhea and 2% to 29% experience severe pain[7].
Severe menstrual pain restricts women’s daily activities and may even force them to miss work or school[8].Also,the adolescents who had dysmenorrhea reported less concentration in class,restricted social activities,and poor school performance[9].Dysmenorrhea also has a negative impact on their mood and causes depression and anxiety[2].
The mainstay of treatment for primary dysmenorrhea is pain relief.Non-steroidal anti-inflammatory drugs(NSAIDs),oral contraceptives and progestins are among the conventional treatments,of which consumption of NSAIDs can have some side effects[2,10].
A systematic review in 2015 showed that although NSAIDs are very effective for treating dysmenorrhea,they have some adverse effects including indigestion,headaches and drowsiness[11].In addition,patients who have a history of“gastroduodenal ulcer,gastrointestinal bleeding,or gastroduodenal perforation”probably should avoid taking NSAIDs[4].
Another systematic review in 2009 indicated that oral contraceptive pills could also have adverse side effects,including nausea,headaches,weight gain,abdominal pain,bloating,anxiety,loneliness and acne[4,12].Also,oral contraceptive pills cannot be prescribed to people trying to get pregnant[13].So now,many women prefer not to use conventional treatment and seek alternative therapies to relieve their menstrual pain.Multiple studies have been conducted on alternative therapies including herbal medicine,dietary supplements,dietary changes,exercise,transcutaneous electrical nerve stimulation,acupuncture,heat and spinal manipulation[4].
Some studies have shown that thiamine,pyridoxine,magnesium,vitamin E and fish oil can effectively treat primary dysmenorrhea.Also,the low-fat vegetarian diet is associated with symptom reduction.Another investigated hypothesis is the role of exercise in decreasing primary dysmenorrhea symptoms[4].
Herbal medicine has been a standard treatment for primary dysmenorrhea in different cultures and countries,and multiple studies have been conducted and shown its possible positive effect on relieving pain[14–18].
This systematic review of the literature was conducted to assess different types of herbal medicine used to treat primary dysmenorrhea and evaluate the effectiveness of these medicines.
Methods
This study aimed to systematically review published articles on the effectiveness of herbal treatment on reducing the pain of primary dysmenorrhea,using Preferred Reporting Items for Systematic Reviews and Meta-Analyses(PRISMA)guideline[19].
Search strategy
In February 2022,international credible scholarly databases,including Google Scholar,Magiran and PubMed were searched.Also,the references of selected articles were hand searched to find relevant studies.
Based on the search syntax,the search guideline was first defined for the PubMed database and was later revised according to each databases’specific framework of search method.
The following keywords in both English and Persian were used:“primary dysmenorrhea”,“herbal remedy”,“herbal medicine”,“plant”,“plant extracts”,“clinical trial”.
Eligibility criteria
The studies were included if they were either clinical trials or Quasi-Experimental,published in English or Persian in the last decade(between 2011 to 2021).
Gray literature,studies published in languages other than English or Persian,studies that only their abstracts were available and unfinished studies,and studies that focused on second dysmenorrhea were excluded.
There were no exclusion criteria related to the age range of the study participant suffering from primary dysmenorrhea in their menstrual cycle.The studies including patients without well-defined primary dysmenorrheal were excluded.
Selection process
First,based on the title and abstract of the articles,two reviewers independently selected the articles that met the inclusion criteria.Studies were classified into three categories:“excluded”,“included”,or“probable”.The articles that both reviewers did not qualify for the study were excluded.The two reviewers then reviewed the full text of the articles categorized as“probable”and a list was prepared.The list was examined,and the disputes were assigned to the included or excluded categories based on the vote of the third expert.
Data collection process
The included studies were independently reviewed for quality and validity by two reviewers,and the studies without quality and validity were excluded.For the final review,all selected articles were carefully studied.The following data were extracted and entered in the information extraction form:title,authors,year of publication,name of the magazine,study design,participants,instruments,study place,settings,reported indicators which were the primary and secondary outcomes/variables of the study.
Study risk of bias assessment
A methodologist reviewed all articles based on the international guidelines for reporting such as CONSORT CARE,PRISMA,STROBE and the articles with low validity were excluded.
Two independent reviewers conducted the eligibility,quality assessment,and data extraction stages of the systematic review and sought the opinion of a third reviewer in case of a difference of opinion.
Reporting bias assessment
The risk of bias was investigated according to the Cochrane quality assessment checklist.
Statistical method
Excel software was used for data extraction and simple descriptive analysis was used to analyze the data.
Result
Search of studies
Seventy three included studies investigated the effectiveness of a total of 44 plants and plant combinations(35 plants and 9 combinations)on primary dysmenorrhea(Figure 1)of which only one study did not report positive results(Table S1)[20–92].
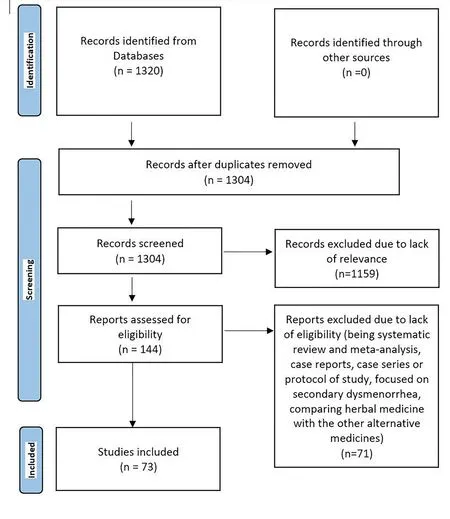
Figure 1 PRISMA flow diagram of selection of publications related to systematic review of herbal medicine in treatment of dysmenorrhea
In 48 of the studies,the investigated plant was significantly effective in reducing primary dysmenorrhea symptoms.However,in one study,the investigated plant was less effective than the nonsteroidal anti-inflammatory drugs administered to the control group(Table S1)[41].
Nearly 93%(63 of 73)of the studies investigated the effects of herbal medicine on the severity of pain and reported positive results.Only 12 out of 73 studies investigated dysmenorrhea symptoms in general.
Characteristics of included literature
Ginger was the most investigated plant.Eight studies assessed the effects of ginger alone,and three studied the combination of ginger with other plants.Only one study that investigated the“effect of eight-week high-intensity interval training and ginger supplementation on primary dysmenorrhea in nonathletic female students”did not report a significant positive effect[20].
Seven studies investigated the effects of ginger alone reported a significant decrease in the severity of the pain(Table S2)[21–27].
Nine studies investigated the effects of either fennel or its combination with other plants on primary dysmenorrhea.Five studies that used fennel as a single plant reported a significant decrease in the severity of the pain(Table S2)[46–50].
Five studies were on chamomile(2 only on chamomile and 3 on its combination with other plants).The two studies on chamomile showed it could reduce pain intensity and menstrual bleeding.The studies that investigated the“fennel,chamomile,and ginger combination”and“chamomile and ginger”combination showed these combinations could effectively ease dysmenorrhea symptoms overall(Table S2)[38,51].
Three studies indicated lavender could effectively reduce pain intensity(Table S2)[28,30–31].
Three studies assessed the effect of cinnamon:two only on cinnamon and one investigated the effect of its combination with ginger.All three reported a significant decrease in the intensity and duration of the pain,and one showed a successful alleviation of dysmenorrhea symptoms(Table S2)[39,65–67].
Studies of Teucrium Polium showed it could influence decreasing pain duration and intensity and menstrual bleeding duration(Table S2)[54,55,73,74].
Based on this systematic review,Ginger,Lavender,Prasaplai,Wheat germ,Melissa officinalis,Eryngo(Eryngium caucasicum Trautv),Dill(Anethum graveolens),Papaya leaf,Thymus vulgaris,Fennel,Glycyrrhiza glabra L.(G.glabra),Stachys Lavandulifolia,Uzara(Xysmalobium undulatum),Rose damascene,Rosaceous,Rose,Cinnamon,Nigella sativa,Achillea Millefolium,Valerian,Vitagnus,Teucrium Polium,Geranium,peppermint(Mentha piperita),Rosemary,Olive,Curcumin,Chamomile,Crocus sativus(saffron),Turmeric,Mint,and Sesame(sesamum indicum),alongside the combinations of“Melissa officinalis and Salvia officinalis”,“Cinnamon-ginger”,“Dangguijagyag-san”,“Fennelin and vitagnus”,“GeGen”,and“Matricaria chamomile and Achillea millefolium”are all effective in reducing the pain associated with primary dysmenorrhea(Table S2).
Lavender,Wheat germ,Fennel,Salix,Rhubarb(Rheum emodi),Cinnamon,Fenugreek Seed,Mint,and Commiphora myrrha,and the combinations of“Chamomile-ginger”,“Dangguijagyag-san”,and“Fennel,Chamomile and Ginger”can be effective on overal dysmenorrhea symptoms(Table S2).
Ginger,Cinnamon,Nigella sativa,Teucrium Polium,and Rosemary,and the combination of“Melissa officinalis and Salvia officinalis”,“Cinnamon-ginger”,and“Valerian and ginger”can decrease the duration of the pain associated with primary dysmenorrhea(Table S2).
Vitagnus,Rosemary,and Chamomile can decrease menstrual bleeding,and only one study showed that Teucrium Polium could reduce the menstrual bleeding duration(Table S2).
Assessment of risk of bias
The risk of bias was investigated according to the Cochrane quality assessment checklist[93].Table S3 shows the assessment results.
Discussion
Primary dysmenorrhea is a common problem around the world[3].NSAIDs,oral contraceptives,and progestins are among the conventional and most commonly used drugs for treatment[2].However,some women prefer alternative and natural treatments due to their adverse effects.This study was conducted to assess different types of herbal medicine used to treat primary dysmenorrhea and their effectiveness,based on published articles from 2011 to 2021.
The data indicated that ginger could reduce the intensity of primary dysmenorrhea symptoms.Another meta-analysis of randomized clinical trials in 2015 showed the same results.Consumption of 750 mg–2,000 mg ginger capsules in the first 3–4 days of the menstrual cycle could lower the severity of pain[94].
This review showed that fennel could also result in a decrease in pain severity.The results from other studies showed similar results[95,96].However,one study reported that fennel increased menstrual bleeding[96].
In this review,only one study indicated that Dangguijagyag-san could be effective in reducing the pain intensity and symptoms of primary dysmenorrhea.Another review in 2020 indicated that compared to western medication,placebos and other herbal medicines,Dangguijagyag-san has sound effects on reducing the pain associated with primary dysmenorrhea[97].
This systematic review confirms that lavender reduces the pain intensity(3 studies)and other symptoms of primary dysmenorrhea(1 study).In three of these studies,lavender was used for aromatherapy and in one as a massage oil.Another study in 2019 on the effect of aromatherapy with lavender also showed it could ease the symptoms of primary dysmenorrhea[98].
In the present review,two studies were found on the positive effect of rose damascene on reducing pain severity via oral consumption and self-massage.However,a meta-analysis in 2021 found that rose damascene used via massage,inhalation,vapor diffusion,or oral intake did not affect menstrual pain and anxiety.However,it reduced headaches,fatigue,and bloating associated with primary dysmenorrhea[99].
According to the results of this review,chamomile can reduce pain intensity and menstrual bleeding.Another review in 2021 showed similar results[100].
Conclusion
Different herbal medicine has been used to treat primary dysmenorrhea,significantly reducing pain intensity or duration or bleeding severity or duration.