Alcohol intake is associated with a decreased risk of developing primary biliary cholangitis
2022-10-08JanineAdeleFrenchPaulGowStevenSimpsonYapKateCollinsJustinNgPeterAngusIngridvanderMei
Janine Adele French, Paul Gow, Steven Simpson-Yap, Kate Collins, Justin Ng, Peter W Angus, Ingrid A F van der Mei
Janine Adele French, Paul Gow, Kate Collins, Justin Ng, Peter W Angus, Department of Gastroenterology, Austin Hospital, Heidelberg 3084, Australia
Steven Simpson-Yap, Melbourne School of Population and Global Health, University of Melbourne, Carlton 3053, Australia
Steven Simpson-Yap, lngrid A F van der Mei, Menzies Institute for Medical Research, University of Tasmania, Hobart 7000, Australia
Abstract BACKGROUND Primary biliary cholangitis (PBC) is a chronic progressive liver disease of unknown aetiology characterised by immune-mediated destruction of small and medium-sized intrahepatic bile ducts. There are few well-established risk factors and epidemiological studies are needed to further evaluate the pathogenesis of the disease.AIM To evaluate the relationship between alcohol intake, smoking and marijuana use with PBC development.METHODS We conducted a prevalent case control study of 200 cases and 200 age (within a five year age band) and sex-matched controls, identified from the Victorian PBC prevalence study. We assessed lifetime alcohol intake and smoking behaviour (both tobacco and marijuana) prior to PBC onset and used conditional logistic regression for analyses.RESULTS Alcohol intake consistently showed a dose-dependent inverse association with case status, and this was most substantial for 21-30 years and 31-40 years (Ptrend < 0.001). Smoking was associated with PBC, with a stronger association with a longer duration of smoking [e.g., adjusted OR 2.27 (95%CI: 1.12- 4.62) for those who had smoked for 20-35 years]. There was no association between marijuana use and PBC.CONCLUSION Alcohol appears to have an inverse relationship with PBC. Smoking has been confirmed as an environmental risk factor for PBC. There was no association between marijuana use and PBC.
Key Words: Primary biliary cholangitis; Autoimmune liver disease; Epidemiology; Alcohol
lNTRODUCTlON
Primary biliary cholangitis (PBC) is a chronic progressive liver disease of unknown aetiology characterised by immune-mediated destruction of small and medium-sized intrahepatic bile ducts. It predominantly affects women in the fourth or fifth decade of life. The aetiology of PBC remains largely unknown but is thought to involve a complex interaction between genetic and environmental factors. Genetic factors are considered to play a role in disease onset due to higher concordance rates in monozygotic than dizygotic twins[1], and population studies that have shown higher incidence in first degree relatives of those with PBC[2]. Recurrent urinary tract infections[2-5] and smoking[2,3,5,6] have been the only risk factors that have been found to be consistently associated with disease development. However, these environmental factors combined appear insufficient to explain the pathogenesis, and it is likely that other environmental factors play a role in disease onset.
In this population-based case-control study, we examined whether alcohol intake, smoking tobacco and marijuana use were associated with the development of PBC.
MATERlALS AND METHODS
Participants
Cases:Cases were diagnosed with either definite or probable PBC. Definite PBC was defined as the presence of liver histology compatible with PBC, cholestatic liver function tests (elevation of serum alkaline phosphatase), and an anti-mitochondrial antibody titre of at least 1:40. Probable PBC was defined as patients fulfilling two of these three diagnostic criteria.
All gastroenterologists in the Australian state of Victoria were sent letters notifying them of the study and inviting them to ask their patients to participate. In addition, cases identified from the Victorian PBC prevalence study[7] were invited to participate (response rate 91%, 160/176). In total, 205 cases were recruited for this study, of which 200 were included in the final analysis. Three cases were excluded as they were not living in Victoria at the time of the study. Two cases were excluded as their histology revealed features of PBC/autoimmune hepatitis overlap syndrome.
Controls:Age and sex-matched controls were recruited from the electoral roll (12%) andviaan advertisement in Victorian newspapers and community-based websites (88%). The latter was utilised because the electoral role alone was unsuccessful in obtaining the required number of controls. Potential participants from the electoral roll were sent a letter of invitation and a consent form. Participants who responded to advertisements were sent a copy of the consent form prior to the appointment being made. Subjects were screenedviatelephone for a history of any liver disease, and seven potential participants were excluded for this reason. Two hundred controls were recruited for this study. Controls were matched 1:1 to the cases based on sex and age (within a 5-year age band) and linked by their grouping identification number for statistical analysis. French JA and Ng J conducted all interviews and measurements between 01 January 2015 and 31 October 2017.
Measures of alcohol intake
Pre-onset alcohol behaviours were queried by questionnaire, including frequency of alcohol intake per week (didn’t drink at all, < 1 d/wk, 1-2 days per week, 3-4 days per week, 5-7 days per week) as well as an average number of drinks per session (didn’t drink, 1-2 drinks, 3-4 drinks, ≥ 5 drinks) over the age periods 16-20 years, 21-30 years and 31-40 years. The frequency and average number of drinks were combined by using the mid-point value of each category and multiplying the two values to estimate average number of drinks consumed per week; these were categorised as 0, 1-5, 6-10, 11-20, and > 20 drinks/wk. A standard drink was defined as 10 g of alcohol content. Cases who had been diagnosed during the defined age periods, as well as their linked controls, were not included in the analysis of that specific age period or age periods that followed.
Measures of smoking and marijuana use
History of smoking (never smoked, ex-smoker), age of commencement, quantity of cigarettes smoked, smoking duration, and periods of non-smoking were queried by questionnaire prior to PBC diagnosis. Controls were given the age of PBC diagnosis of their matched case. History of marijuana use (never used, ex-user and current user) and frequency of marijuana use was also queried.
Other measures
Participants had their height and weight measured, and their body mass index (BMI) calculated. The questionnaire also included country of birth, self-reported ethnicity, level of education completed, history of urinary tract infection (if yes, number of urinary tract infections and at what age), past surgical history, other medical comorbidities and personal, and family history of liver disease and autoimmune diseases.
Statistical analysis
Differences in categorical characteristics between cases and controls were evaluated by Chi-square test, while differences in continuous variables between cases and controls were evaluated byt-test.
The associations of alcohol intake with case status were evaluated by conditional logistic regression, estimating an odds ratio (OR). Adjusted models were adjusted for country of residence, education, vitamin D supplement use, and smoking status. Further adjustment for current alcohol intake was undertaken to assess whether pre-onset alcohol associations were independent of subsequent alcohol behaviour, as these can be correlated. Tests for interactions were undertaken by including a product term of the predictor and interaction term. All analyses were done using STATA/SE 15.0 (StataCorp, College Park, TX, United States).
RESULTS
There was a female to male ratio of 10.8:1 and the mean age was 63.6 years for cases and 61.5 years for controls (Table 1). Average BMI was in the overweight range for both groups.
As would be expected given matching, there were no significant differences between cases and controls in either age or sex. As is typical for control groups, controls had a higher proportion with a higher educational level (P< 0.001), and they were more likely to be Australian-born (P< 0.001). Therefore, models were adjusted for educational level and whether the participant was born in Australia. There was no difference in ethnicity between cases and controls (Table 1). The mean time from PBC diagnosis to time of study was 12.6 years.
Alcohol intake
Alcohol intake, both frequency per week and average number of drinks per session, was significantly lower amongst cases throughout their life course. Alcohol intake consistently showed a dose-dependent inverse association with case status, which was strongest for the 21-30 age group and 31-40 age group (Ptrend< 0.001) (Table 2). PBC cases were also more likely to be non-drinkers (age group 21-30 years: OR 5.05 (95%CI: 2.53-10.09), age group 31-40 years: OR 3.64 (95%CI: 1.34-9.90), persisting on adjustment. The inverse associations between alcohol intake and case status remained upon adjustment for alcohol intake at the time of questionnaire, demonstrating that pre-onset alcohol intake is independently associated with PBC development. For patients with PBC and cirrhosis at the time of the analysis, the pre-PBC alcohol intake in each 10-year band for both total drinks per week and drinks per session did not impact Child-Pugh score at the time of analysis (Supplementary Tables 1 and 2).
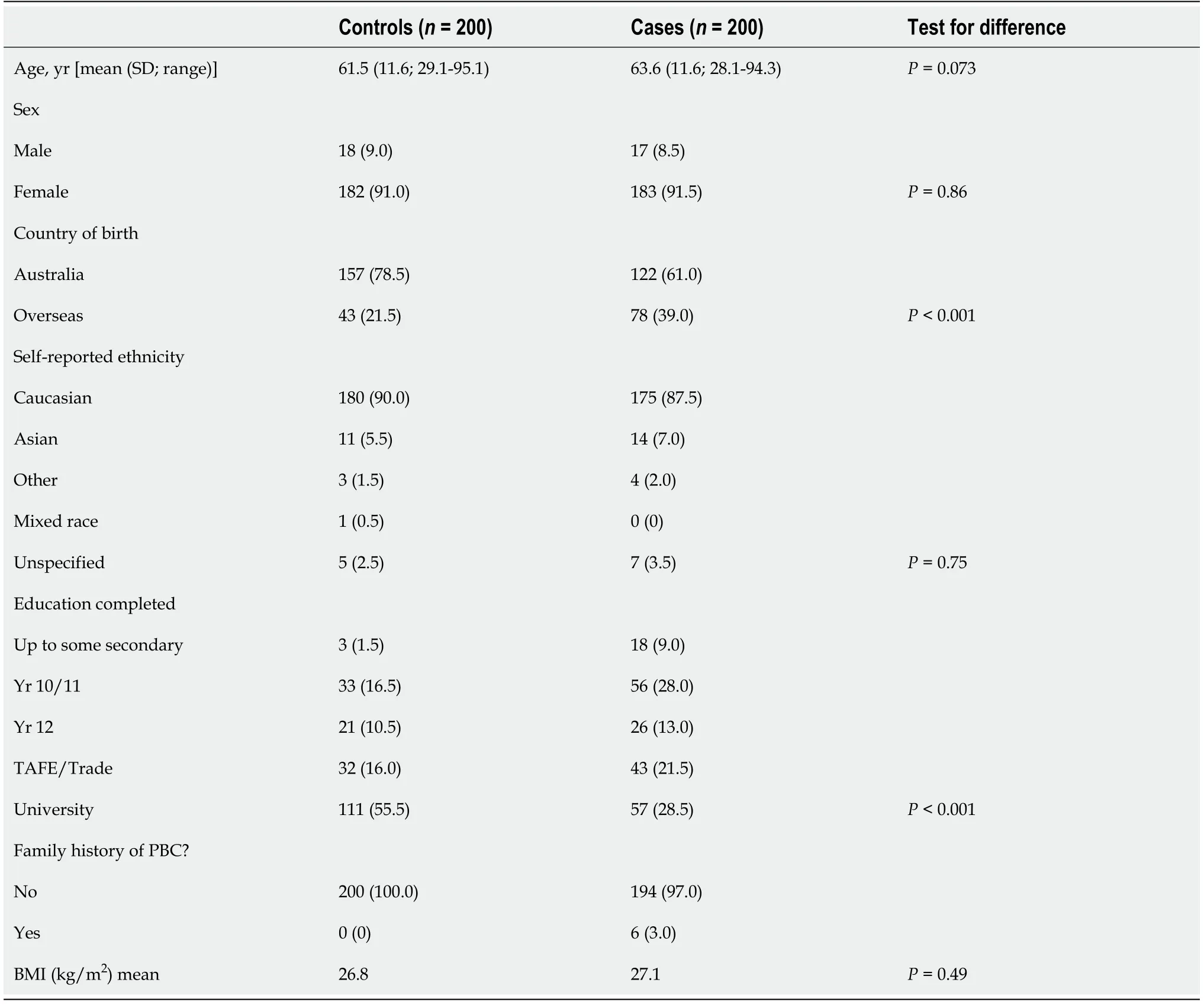
Table 1 Cohort characteristics of cases and controls
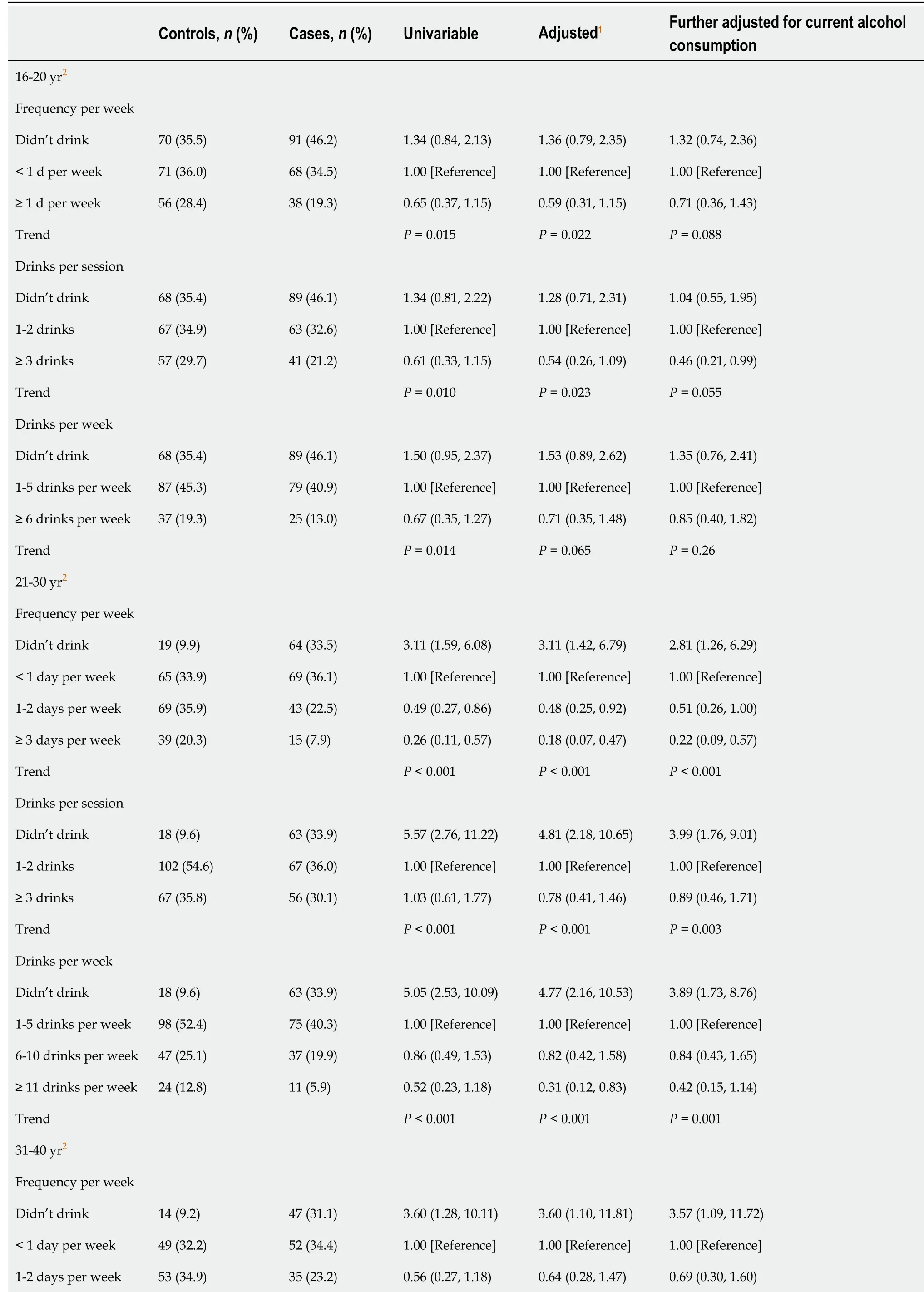
Table 2 Odds ratios for primary biliary cholangitis and alcohol intake (frequency per week, drinks per session, drinker per week) for different age spans
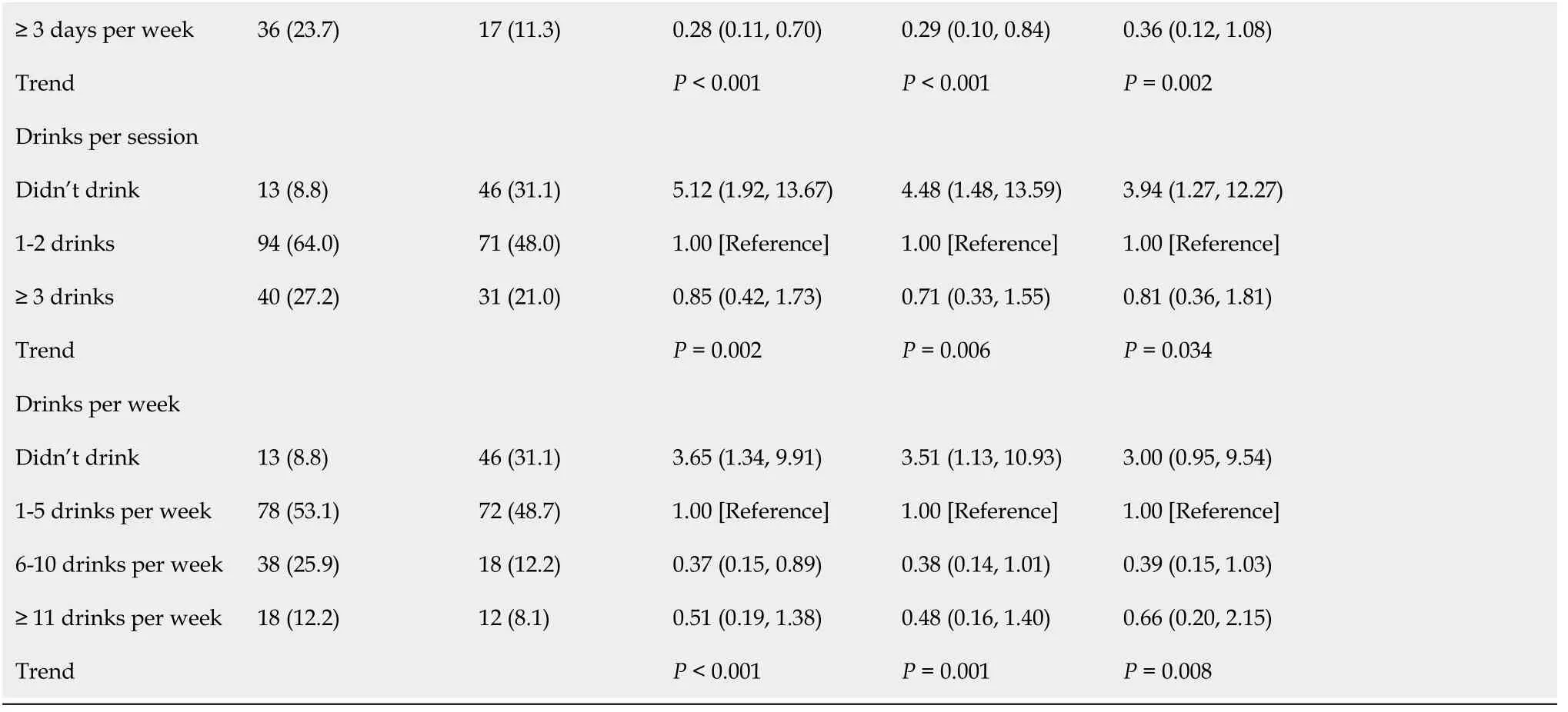
Associations with case status assessed by conditional logistic regression, grouped on the linkage identifier for matched cases and controls.1Adjusted models adjusted for whether participant was born in Australia, education completed, and whether participant had ever smoked.2Cases (and their linked controls) who had been diagnosed prior to each age span were excluded from analysis, including 1 case/control pair for 16-20 yr, 8 case/control pairs for 21-30 yr, and 47 case/control pairs for 31-40 yr.PBC: Primary biliary cholangitis.
Tobacco/marijuana
In the unadjusted analysis, smoking was significantly more common among cases, but the effect size reduced after adjustment [aOR1.42 (95%CI: 0.88-2.30)] (Table 3). The association was stronger for those who smoked for longer [aOR 2.27 (95%CI: 1.12-4.62) for those who had smoked for 20-35 years] [aOR 1.90 (95%CI: 0.68-5.30) for those who had smoked > 35 years].
In contrast to tobacco, there was no association with marijuana use and cases status, and this remained after adjustment for birthplace and educational level, as well as further adjustment for tobacco smoking. Small numbers precluded effective examination of the associations of the duration of marijuana use or the age of marijuana debut.
DlSCUSSlON
PBC is an increasingly common[7] potentially life-threatening cholestatic liver disease with a poorly defined aetiology. We identified a modest association with PBC for past smoking with an aOR of 1.42 (95%CI: 0.88-2.30), which did not quite reach significance. Our effect size is close to the pooled OR of 1.67 (95%CI: 1.4-1.92) identified in a meta-analysis of five case-control studies examining the association with PBC and smoking[8]. Importantly, our associations were stronger for those who smoked for longer [e.g., aOR 2.27 (95%CI: 1.12- 4.62) for those who had been smoking for 20-35 years]. This was also the case in a study in the United Kingdom, where an OR of 3.5 (95%CI: 1.9-6.3) was found for those who smoked for 20 years or more[6]. A more robust way of assessing dose-response would be to measure the history of smoking in pack years, which, unfortunately we were not able to perform in our study. We did not identify an association with marijuana use and the development of PBC.
This is the first study that has thoroughly evaluated the intake of alcohol in PBC cases from adolescence until the age of PBC diagnosis. Surprisingly, we found that alcohol has an inverse association with the development of PBC. Our study found that cases reported significantly less alcohol intake prior to PBC onset with dose-response associations, and compared to controls, cases were more likely to report that they never drank. For example, by age 21-30 years, a third of the cases said they never drank, and this was true for only 10% of the controls aOR 3.93 (95%CI: 1.74-8.89). Our associations remained after adjustment for country of birth, education level, and smoking, and remained after a further adjustment for current alcohol intake. The big question is whether this is a true finding or whether this could have resulted from recall bias due to the stigma surrounding the intake of alcohol. Those with established liver disease may be even more likely to underreport alcohol intake prior to disease onset. However, if this is a true observation, it has important implications with respect to modifiable risk factors.
There is minimal data in the literature on the association between alcohol and PBC. There have only been two previous case-control studies where this has been evaluated and alcohol was not the primary outcome measure in either of these studies. Gershwinet al[2] found no significant difference in alcohol intake between 1032 cases and 1041 controls when they evaluated those who had consumed ≥ 12/wk standard drinks over a lifetime. However, as this is a very rudimentary measure of lifetime alcohol intake, a more detailed lifetime assessment of alcohol intake is required to evaluate this further. They also found that 28% of prevalent cases were likely to have had ≥ 12/wk standard drinks in the year prior to interview compared with 50% of controls (unadjustedP< 0.0001)[2]. However, it is difficult to make a meaningful assessment of this data, as the alcohol intake period was after disease onset, where cases would have been advised to minimise alcohol intake.
Princeet al[3] compared data from more than 2400 controls with two groups of prevalent PBC cases; cases from a geographically defined epidemiology study (epidemiological casesn= 318) and from a survey of the national patient support group (foundation cases,n= 2258). They found that PBC cases from both groups were less likely to have regularly consumed alcohol over their lifetime compared with controls [OR 0.57 (95%CI: 0.39-0.83), OR 0.73 (95%CI: 0.61-0.79) for epidemiological and foundation cases respectively]. When males were excluded from the analysis, the significant difference did not persist for the foundation cases but did persist for the epidemiological cases[3]. Thus, there was a need for a more detailed study of alcohol intake prior to PBC onset.
Alcohol is thought to protect against autoimmune diseases such as rheumatoid arthritis[9,10], SLE[11,12], autoimmune thyroid disease[13], and Type I diabetes mellitus[14]. It has been suggested that moderate alcohol intake may have a protective effect on the immune system, compared with alcohol abuse or abstinence, and this may explain the protective effect on subsequent autoimmune disease development[13,15]. The mechanism as to how moderate alcohol prevents subsequent autoimmune disease development remains unclear. Potential mechanisms to explain the beneficial effects of moderate alcohol intake on the immune system function are; loss of natural killer cell activity[16], changes in immunoglobulin levels[17] and alterations in T helper 1 (Th1) and Th2 mediated immunity[18]. Thus, there is the possibility that alcohol could also be protective for PBC.
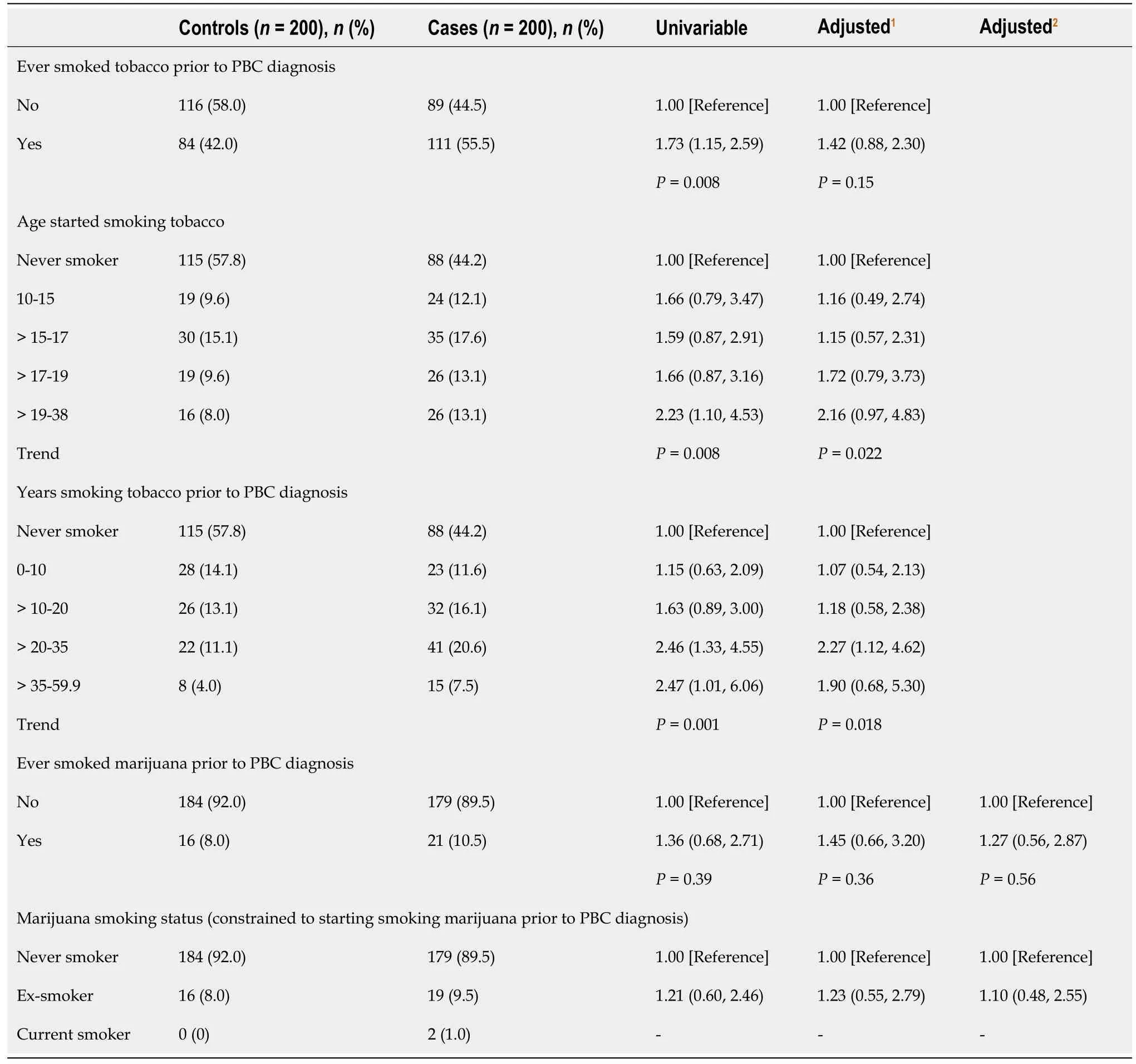
Table 3 Odds ratios for the association between tobacco and marijuana intake and primary biliary cholangitis development
This study has several strengths. The demographic characteristics of our case cohort were similar to other published PBC cohorts in Europe[19], and the United States[2], and the participation rate of the cases was high (91%). Therefore, it is likely that our cohort is representative of other PBC populations worldwide. Our control group was matched on age (within a five-year band), and sex and was obtained from the same geographical location as cases. A limitation of our study is the selection of controls - only 12% were recruited from the electoral roll, our intended source of recruitment for all controls, but this was not possible due to this limited response to invitation. Another potential limitation of our study is possible measurement error due to respondents summarising their frequency and quantity of alcohol intake over 10 year age intervals (except for the four-year interval of 16-20 years old). It is also possible that fatigue, a symptom in up to 80% of PBC patients[20], was significant enough prior to diagnosis to reduce or even prevent alcohol intake in PBC cases.
CONCLUSlON
Overall, we did not find that alcohol intake was a risk factor for PBC. Instead, we found that it was inversely associated, which raises the possibility that alcohol intake may be associated with a reduced risk of PBC, an important finding for a disease with few established risk factors. Due to the limitations of this study, this association requires replication in other PBC studies, preferably in cohort studies where the exposure is measured prior to disease onset.
ARTlCLE HlGHLlGHTS
Research background
Primary biliary cholangitis (PBC) is a chronic progressive liver disease of unknown aetiology characterised by immune-mediated destruction of small and medium-sized intrahepatic bile ducts. There are few well-established risk factors and epidemiological studies are needed to further evaluate the pathogenesis of the disease.
Research motivation
Recurrent urinary tract infections and smoking have been the only risk factors that have been found to be consistently associated with PBC development. However, these environmental factors combined appear insufficient to explain the pathogenesis, and it is likely that other environmental factors play a role in disease onset.
Research objectives
To analyze environmental factors such as smoking, marijuana and alcohol use, and the role they play in PBC development.
Research methods
A prevalent case control study of 200 cases and 200 age (within a five year age band) and sex-matched controls, identified from the Victorian PBC prevalence study. The associations of alcohol intake with case status were evaluated by conditional logistic regression, estimating an odds ratio.
Research results
For PBC development alcohol intake consistently showed a dose-dependent inverse association with case status, and this was most substantial for 21-30 years and 31-40 years. Smoking was associated with PBC, with a stronger association with a longer duration of smoking while there was no association between marijuana use and PBC.
Research conclusions
Our study found that alcohol intake may be associated with a reduced risk of PBC, an important finding for a disease with few established risk factors.
Research perspectives
The association of alcohol and risk reduction of PBC requires replication in other PBC studies,preferably in cohort studies where the exposure is measured prior to disease onset.
FOOTNOTES
Author contributions:French JA, Gow P, Angus PW and van der Mei IAF conducted the research design; French JA conducted the data acquisition; French JA, Simpson-Yap S and van der Mei IAF conducted the data interpretation and all authors were involved with the manuscript preparation; French JA, Simpson-Yap S, Ng J, van der Mei IAF, Angus PW and Gow P approved the final submitted draft; Collins K assisted with submission; Nil other authors/institutions other than those listed were involved with this study; all authors have approved the final version of this manuscript, including the authorship list.
lnstitutional review board statement:Ethical clearance was obtained from the Austin Hospital’s Health Research and Ethics Committee (HREC 2013/04859) and it complies with acceptable international standards.
lnformed consent statement:All study participants provided informed written consent prior to study enrollment.
Conflict-of-interest statement:Dr. French reports grants from Orphan Australia, grants from Austin Medical Research Foundation, during the conduct of the study.
Data sharing statement:No additional data are available.
STROΒE statement:The authors have read the STROBE Statement—checklist of items, and the manuscript was prepared and revised according to the STROBE Statement—checklist of items.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Australia
ORClD number:Janine Adele French 0000-0003-0630-5916; Paul Gow 0000-0001-6505-7233; Steven Simpson-Yap 0000-0001-6521-3056; Kate Collins 0000-0001-6357-3867; Peter W Angus 0000-0001-8505-2317; Ingrid A F van der Mei 0000-0001-9009-7472.
S-Editor:Gong ZM
L-Editor:A
P-Editor:Gong ZM
杂志排行
World Journal of Hepatology的其它文章
- Nutritional assessment in patients with liver cirrhosis
- Non-alcoholic fatty liver disease: ls surgery the best current option and can novel endoscopy play a role in the future?
- Therapies for non-alcoholic fatty liver disease: A 2022 update
- Βile acids as drivers and biomarkers of hepatocellular carcinoma
- Approach to persistent ascites after liver transplantation
- Positive autoantibodies in living liver donors
