Speckle-tracking echocardiography for detecting myocardial dysfunction in sepsis and septic shock patients: A single emergency department study
2022-09-17XuanFuXueLinSamuelSeeryLinaZhaoHuadongZhuJunXuXuezhongYu
Xuan Fu, Xue Lin, Samuel Seery, Li-na Zhao, Hua-dong Zhu, Jun Xu, Xue-zhong Yu
1 Emergency Department, State Key Laboratory of Complex Severe and Rare Diseases, Peking Union Medical College Hospital, Chinese Academy of Medical Science and Peking Union Medical College, Beijing 100730, China
2 Department of Cardiology, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing 100730, China
3 Faculty of Health and Medicine, Division of Health Research, Lancaster University, Lancaster LA1 4YW, United Kingdom
KEYWORDS: Sepsis; Septic shock; Speckle-tracking echocardiography; Global longitudinal strain;Global circumferential strain
INTRODUCTION
Septic cardiomyopathy (SCM) is reversible myocardial depression, which occurs in the early stages of sepsis and septic shock, however, def initions and diagnostic criteria have yet to be unified.The echocardiographic parameters of left ventricular ejection fraction (LVEF) are routine measures and the clinical standard for assessing cardiac function. The threshold used to def ine “abnormal” is generally set according to an LVEF of between 40% and 50%.Even though LVEF measures are non-invasive and readily available, results largely depend upon loading conditions.LVEF is the fraction of chamber volume ejected in systole (stroke volume) in relation to the volume of the blood in the ventricle at the end of diastole (end-diastolic volume). LVEF is widely considered a predictor of mortality, although it does not provide an accurate subclinical assessment of contractility. This means that LVEF is less useful for those with sepsis or septic shock patients because “normal” LVEF readings can be observed even in those with impaired contractility.
Speckle-tracking imaging technologies enable us to track “speckle” displacement using two-dimensional (2D)echocardiographic images.This can be used to assess movement in the cardiac cycle or strain, which refers to the percentage of change in myocardial length/thickness compared to the initial length/thickness of the myocardium during contractions. These change percentages are measured longitudinally, radially, and across circumferential directions, providing further insights. This relatively new approach has an agreement with the current gold standard like cardiovascular magnetic resonance (CMR),which is feasible, repeatable, and accurate. It would appear that speckle-tracking echocardiography (STE) provides a more sensitive measure of contractility and can be used to overcome many shortcomings of LVEF readings.
Global longitudinal strain (GLS) has reduced interobserver and intraobserver variability, and is more sensitive and specific in identifying subclinical LV systolic dysfunction.GLS improves STE in terms of reproducibility and is considered easier for trainees to grasp. Over the past decade, studies have applied GLS technology to SCM and have found that strain measurements are not only more sensitive than conventional echocardiography, but also more accurate for patients with preserved LVEF,and could be used for diagnostics, prognostics, and longer-term followups.Few studies have explored the characteristics of myocardial function in the early stage of sepsis or septic shock or whether it is affected by infection severity such as shock state, which may be significant for sepsis or septic shock management. Therefore, it is necessary to understand whether early septic shock causes more strain changes than sepsis alone. It is also necessary to investigate the characteristics of strain parameters in sepsis and septic shock populations.
METHODS
Study setting
This is a cross-sectional study conducted in the Emergency Department (ED) of Peking Union Medical College Hospital. This facility is also the State Key Laboratory of Complex Severe and Rare Diseases. The study was conducted between 1June and 31December, 2021.The research protocol was approved by the Institutional Review Board (IRB) of Peking Union Medical College Hospital. Written informed consent was obtained from all patients (or their legal guardians) before being allowed to participate. The study was performed in accordance with the ethical standards established in the updated.
Participants
All patients who were admitted to the ED with acute infection were screened and diagnosed according to the standard definition, Sepsis 3.0(supplementary Table 1),for complete inclusion and exclusion criteria. Resuscitation and management strategies were implemented according to the Surviving Sepsis Campaign (SSC) guidelines.
Transthoracic echocardiography
Echocardiographic parameters were collected within 24 h of sepsis or septic shock diagnosis, and after the standard three-hour bundle determining in the SSC guidelines. Point-of-care transthoracic echocardiograms(TTE) were performed on patients with a supine position and from a left lateral position using a Mindray M9(Mindray Bio-Medical Electronics Co., Ltd., China).We adhered to image standards as recommended by the American Society of Echocardiography.All examinations were performed by certified emergency specialists under the supervision of a certif ied cardiologist.
LVEF was measured using both the Teichholz’s method(LVEF_Teich) which used M-mode, and Simpson’s biplane method (LVEF_SB) from the left four- to two-chamber apical views. The following measures were made to assess diastolic functions: early (E) and late (A) mitral inf low peak velocities, as well as early diastolic mitral annular velocity(e') which were acquired at the lateral mitral annuli with tissue Doppler imaging (TDI). Ratios for early trans-mitral flow velocity to the early diastolic mitral annular velocity(E/e') were calculated. Velocity-time integral (VTI) for the left ventricular outflow tract (LVOT) was measured using Doppler echocardiography to calculate stroke volume (SV)and cardiac output (CO). Cardiac preload was indirectly estimated by measuring the diameter of inferior vena cava(IVC) and inspiratory collapsibility index (CI).
2D-speckle-tracking and post-processing analysis
Imaging standards were set according to the consensus of the European Association of Cardiovascular Imaging and the American Society of Echocardiograph.GLS was calculated from the three standard apical perspectives, i.e.,two-, three-, and four-chamber views. Global circumferential strain (GCS) and global radical strain (GRS) were measured from parasternal short-axis views, from the left ventricular mitral valve, papillary muscles, to the apex. Images were obtained at a frame rate of 50–90 frames/s. By recording at least three consecutive cardiac cycles, the best single cardiac cycle was selected according to image quality and tracking quality. Images were rejected if they were of poor quality or if we could not track two or more adjacent segments.
Mindray TT-QA software (Mindray Bio-Medical Electronics Co., Ltd., China) was provided with the apparatus and can automatically trace a region of interest(ROI) using a point-and-click approach. Adjustments can also be made in accordance with the width of the ROI to achieve the best alignment. Thereafter, three apical images and two parasternal short-axis images were divided into six standard segments using the Mindray M9 apparatus.Meanwhile, the apical levels for parasternal short axes were divided into four segments. The corresponding number of time-strain curves were generated in each section, which jointly outlined the entire left ventricular wall. GLS, GRS,and GCS were the average systolic peaks of the segments,which were expressed as change percentages. Negative GLS and GCS values, as well as positive GRS values, were taken to represent myocardial contractility. All echocardiographic interpreters were blinded to all clinical data at the time of image analysis.
Clinical data
Glasgow Coma Scale (GCS) scores, Sequential Organ Failure Assessment (SOFA) scores, and Acute Physiology and Chronic Health Evaluation II (APACHE II) scores at the time of admission were collected. Data taken around the time of TTE were collected, including demographics, vital signs, hemodynamic, respiratory, laboratory results, and comorbidities. Sources of infection were identified using body fluid cultures, including blood, alveolar lavage fluid,urine, serous eff usion, cerebrospinal f luid, and wound swab.
Subgrouping
Subgroups were based on the criteria provided in Sepsis 3.0and through consensus for proposed values of analyzed SCM variables (cTnI and LVEF_SB).All participants were further subdivided according to the following three grouping standards: (1) septic shock, sepsis (without shock); (2) cTnI ≥99percentile upper reference limit (URL) 0.056 μg/L, cTnI <99URL 0.056 μg/L; (3) LVEF_SB ≥50%, LVEF_SB <50%.
Statistical analysis
Data were presented as means with standard deviations or as simple count data (or proportions), as indicated. The Student’s-test was performed to compare characteristics,laboratory tests, and echocardiographic parameters between groups when distribution was considered normal. Alternately,the Mann-Whitney-test was implemented when normal distribution was not evident.
Categorical data were compared using standard Chisquare tests. Bivariate correlations were summarized using a correlation matrix to assess relations between cardiac systolic and diastolic, hemodynamic indexes and myocardial injury markers. The R-value for indexes with obvious correlations in the heat map was calculated using Pearson’s or Spearman’s coeffi cients.
Statistical analysis was performed using R (version 4.1.2).Graphs were created using GraphPad Prism software (version 8.0.2) and MedCalc statistical software (version 20.023).The corrplot package in R was used to calculate correlation coefficients and consider the significance of each correlation in the heat-mapping algorithm. The two-tailed-value of 0.05 was set as the threshold for statistical signif icance.
RESULTS
Recruitment
A total of 132 consecutive adult patients who had been admitted to the ED for sepsis or septic shock were recruited.After exclusion, 60 patients were considered eligible for further analysis. Details of exclusion processes and subgroups are provided in Figure 1.
Patient characteristics
Demographics and clinical parameters are provided in supplementary Table 2. Age and gender distributions did not differ significantly between the three subgroups.The subgroups were well-balanced with regards GCS, comorbidities and in terms of the infection sources.
The patients with septic shock had a higher heart rate(HR) (=0.04) and norepinephrine (NE) doses (=0.01), as well as a lower systolic blood pressure (SBP) (=0.01) and diastolic blood pressure (DBP) (=0.01) compared to the patients with sepsis.
SOFA and APACHE II scores were significantly higher in the septic shock subgroup and in the LVEF_SB<50% subgroup (=0.01). Levels of partial pressure of arterial oxygen to fraction of inspired oxygen (P/F) were significantly lower in the septic shock subgroup (=0.03)and in the LVEF_SB <50% subgroup (=0.02).
Conventional echocardiographic data
Conventional echocardiographic parameters across subgroups have been provided in Table 1. Differences in LVEF_Teich, LVEF_SB, LVOT_VTI, LVOT_SV, LVOT_CO, E/A, e', E/e', and CI were not statistically significant between the septic shock and sepsis subgroups. However,LVEF_Teich and LVEF_SB decreased significantly in patients with cTnI ≥99URL compared to patients with cTnI<99URL (=0.03,=0.01, respectively). Additionally,LVEF_Teich, LVEF_SB, and LVOT_VTI significantly decreased in patients with LVEF_SB <50% compared to patients with LVEF_SB ≥50% (all=0.01).
Speckle-tracking echocardiographic data
STE parameters across subgroups have also been provided in Table 1. There were no significant differences in GLS, GCS GRS, or LVEF_STI between the subgroups of patients with septic shock and sepsis (all with>0.05).The analysis of GLS and GCS revealed that strain was significantly less negative in the subgroup of patients with cTnI ≥99URL compared to the patients with cTnI < 99URL (=0.02,=0.04, respectively). Additionally, GLS and GCS were signif icantly also less negative in the subgroup of patients with LVEF_SB <50% compared to the subgroup of patients with LVEF_SB ≥50% (both=0.01).

Figure 1. Flowchart for participant assignment. cTnI: cardiac troponin I; LVEF: left ventricular ejection fraction; SB: Simpson’s biplane; COPD:chronic obstructive pulmonary disease; 99th URL: 99 percentile upper reference limit.
The values of left ventricular systolic function assessed by GLS were significantly higher (which indicates poorer contractility) in the subgroup of patients with abnormal cTnI and LVEF_SB levels(–14.74%±4.21% in cTnI≥99vs. –17.11%±3.06% in cTnI<99URL,=0.02; –12.29%±2.61% in LVEF_SB<50% vs. –17.39%±3.12% in LVEF_SB≥50%,=0.01) compared to their counterparts. No significant differences were identified between septic shock and sepsis subgroups in this regard (–15.48%±3.43% vs.–16.59%±3.82%,=0.27) (supplementary Figure 1).
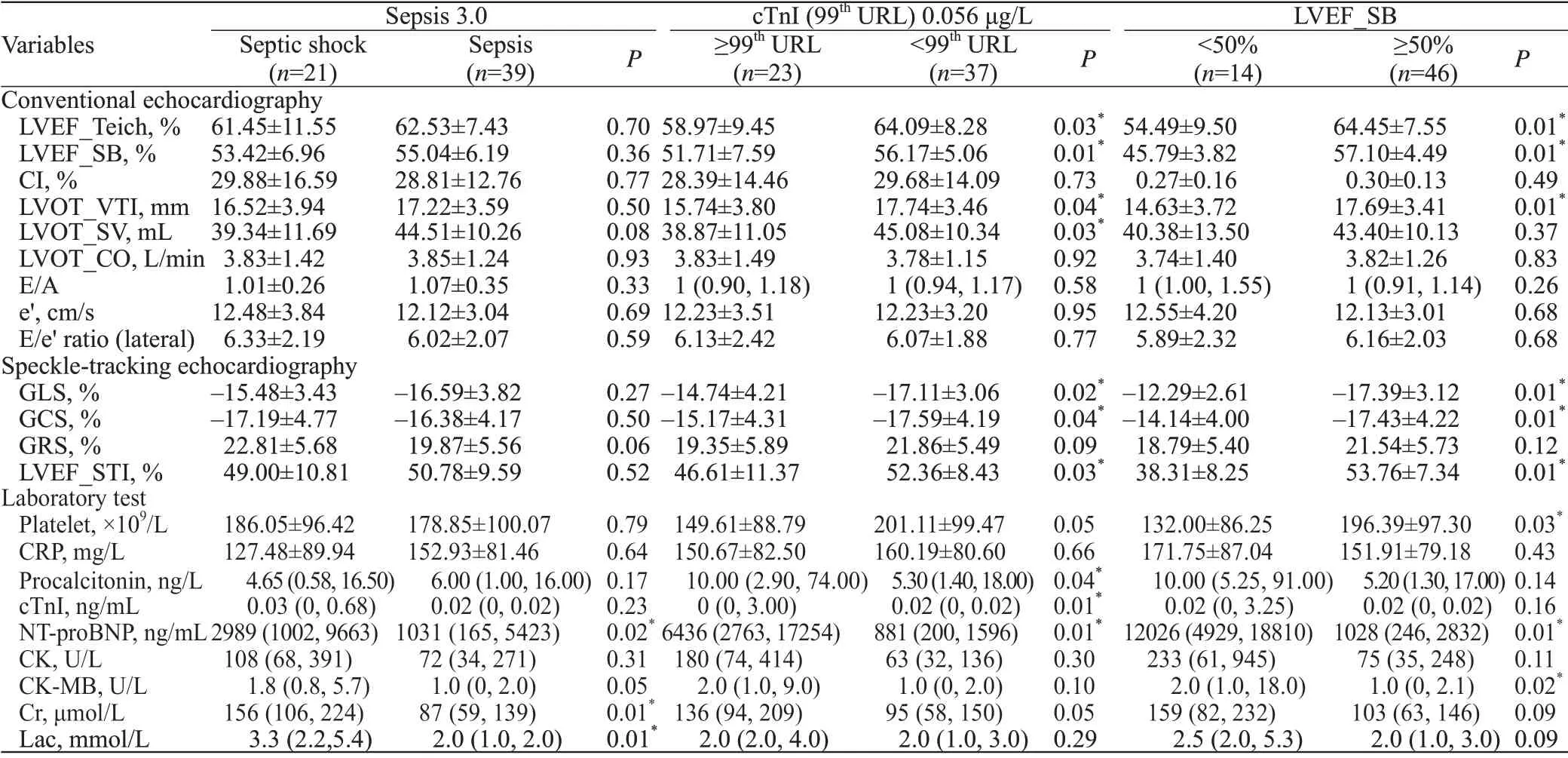
Table 1. Two-dimensional echocardiographic parameters and laboratory tests of the investigated groups
Laboratory tests
Laboratory test results are provided in Table 1.N-terminal pro-B-type natriuretic peptide (NT-proBNP)(=0.02), Cr (=0.01), and lactate (=0.01) levels were significantly higher in patients with septic shock compared to patients with sepsis.
In the subgroup of patients with cTnI ≥99URL, the level of procalcitonin (PCT) (=0.04) and NT-proBNP(=0.01) were signif icantly higher compared to patients with cTnI <99URL.
NT-proBNP and creatine kinase-myocardial band isoenzyme (CK-MB) levels were signif icantly higher in the patients with LVEF_SB <50% compared to patients with LVEF_SB ≥50% (=0.01,=0.02, respectively),while the platelet (PLT) count was signif icantly lower in the subgroup of same patients (=0.03).
Correlation between echocardiographic variables and laboratory tests
In the supplementary Figure 2 which provides a correlation matrix, contractility indices including LVEF_SB and LVEF_STI correlated with non-invasive hemodynamic parameter of LVOT_VTI to some degree and negatively correlated with strain indices, including GLS and GCS.
Cardiac injury indices including cTnI and NTproBNP positively correlated with GLS. There was also a negative correlation between GLS and LVEF_SB,LVEF_STI and LVOT_VTI.
Diastolic function indices including E/A, e', E/e' were not significantly associated with other echocardiographic variables or laboratory tests. Indices reflecting disease severity, such as SOFA and APACHE II scores, also did not appear significant in relation to echocardiographic variables.
The main correlations between investigated laboratory tests and echocardiographic parameters observed in the correlation matrix have been summarized. We found a signif icant negative correlation between GLS and LVEF_SB (= –0.69,<0.001) and a moderate correlation between GCS and LVEF_SB(= –0.39,=0.002), although there was no significant correlation between GRS and LVEF_SB (=0.199). In addition, there was a moderate correlation between GLS and GCS (= 0.47,<0.001).
For echocardiographic variables and serum biomarkers, GLS positively correlated with cardiac injury indices including both cTnI (=0.40,=0.002)and NT-proBNP (=0.44,=0.001). Both cTnI and NTproBNP were found to negatively correlate with LVEF_SB (= –0.36,=0.005;= –0.38,=0.003, respectively).Please see supplementary Figure 3 for further details.
DISCUSSION
This study attempted to gain insight into whether early septic shock causes more strain changes than sepsis alone.We also planned to investigate the characteristics of strain parameters in sepsis and septic shock populations. We found there was no significant difference in early strain parameters between patients with sepsis and septic shock(>0.05). However, we also found that strain parameters for GLS and GCS were significantly less negative (both<0.05) in subgroups of patients with abnormal troponin levels (cTnI ≥99URL) and LVEF values (LVEF_SB<50%). Additionally, we identif ied signif icant but moderate correlations between GLS and cTnI, NT-proBNP levels (both<0.05).
Previous studies carried out by Shahul et al,Lanspa et al,and Innocenti et alanalyzed echocardiographic findings for patients within 24 h of admission to intensive care unit (ICU), and found no association between septic shock and GLS or LVEF. Other studies found significantly lower GLS values in ICU patients with septic shock(<0.001).One might postulate that different time windows for measurements might cause diff erent results. In addition to participant characteristics, it is necessary to factor in context. The study conducted by Shahul et alfound a significant decrease of GLS in patients with septic shock(<0.001) only after 24 h in ICU, which may provide an explanation. Our study was conducted in an ED (rather than in an ICU) and therefore, conventional echocardiography and STE were performed after the initial three hours of resuscitation and once patients had been diagnosed with sepsis or septic shock. This may be the reason why we did not observe an association between shock and subclinical myocardial dysfunction. Further artif icial intelligence studies will likely provide more insight, although interconnected,national (and international) datasets are needed.
The underlying mechanisms involved in strain changes in sepsis and septic shock are not fully understood. While there is a possibility that microvascular contraction in the highly vulnerable subendocardial muscle layer may lead to ischemic injury, longitudinal f ibers are also highly prone to ischemia.Compared with other echocardiographic parameters, GLS provides insight into the systolic shortening of LV from the base to apex, and provides information on LV emptying and dilation, which appears to hold superior diagnostic strength.GLS has been proven more sensitive to early myocardial systolic abnormalities compared to conventional echocardiographic methods,and therefore could reflect the severity of the infection.However, this evidence comes from animal modelling which does not always apply to humans. Evidence has emerged that GLS has high clinical applicability and an overall GLS of greater than –18% is usually accepted as abnormal,but this cut-offhas yet to be validated because there is no offi cial consensus for the cut-off for SCM. Many studies have reported that a cut-off of –15%would be appropriate, although this may vary substantially within samples. Therefore, it would seem prudent to incorporate GLS into clinical practice as a supplementary parameter for LVEF, as this would help us to understand SCM.
Our study uncovered a suggestive effect of early troponin elevation rather than septic shock on myocardial dysfunction. Despite implementing more rigorous inclusion and exclusion criteria, we did not observe a significant difference in troponin levels between the sepsis and septic shock subgroups. However, under troponin-based subgroup analysis, we found that an abnormal troponin level can manifest with less negative GLS, GCS and lower LVEF.Previous researchhas found a strong correlation between cardiac troponin, infection severity, and sepsis prognosis.However, due to their lack of evaluation of cardiac function and morphology, there is no direct evidence around elevated troponin levels in relation to potential abnormal cardiac stress and injury. A previous study has included echocardiography and found that abnormal levels of troponin are related to sepsis-induced myocardial dysfunction,which has an independent prognostic value.In addition,we also observed a moderate correlation of troponin level with GLS and LVEF (=0.40,=0.002 and= –0.36,=0.005). This may enable us to identify global muscle dysfunction, simultaneously allowing us to better understand the pathophysiology of SCM. Therefore, the timing of echocardiography is important and should be considered with the rationalization of medical resources. We believe that it is necessary to carry out routine echocardiography early in the infection to understand abnormal troponin levels and STE to identify subclinical myocardial systolic dysfunction.
We included cardiac morphology analysis in this study, and found that NT-proBNP was related to cardiac performance. Circulating NT-proBNP was signif icantly higher in patients with septic shock, and in those with abnormal cTnI and LVEF_SB. There also appeared to be a modest correlation in NT-proBNP with both GLS (=0.44) and LVEF_SB (=0.38). This means that circulating NT-proBNP was likely related to septic shock occurrences.However, NT-proBNP is affected by fluid loading conditions, especially after resuscitation of sepsis or septic shock, and therefore we cannot recommend this biomarker for SCM analysis.
Strength and limitations
Compared with most clinical studies conducted in ICUs, this rather novel study is one of the few to include strain measurement in an ED setting. That is, we tried to advance the inspection time window to the end of initial resuscitation, after diagnosing sepsis or septic shock. This helps us respond to the conditions under which we conduct bedside echocardiographic assessment for patients at risk of SCM. Additionally, drawing on the evidence from previous relevant studies, we embedded very strict eligibility criteria to control for potential confounding factors and formulated criteria by excluding the effects of pre-existing cardiopulmonary disease, acute medical conditions other than infections, iatrogenic mechanical support, etc.
There were a number of limitations. Patients in the ED are usually assigned to final inpatient destinations within 48 hours, so we were unable to obtain dynamic changes in indicators during the course of the disease. Additionally,we could not rule out the possible evolution of left and right ventricular dysfunction. We also could not explore individual demographic or clinical factors, nor could we apply multivariate analysis to this sample because we had so few participants.
CONCLUSIONS
Evidence from this single ED study shows that myocardial dysfunction, such as lower LVEF or less negative GLS values in patients with sepsis or septic shock,is more affected by myocardial injury. The GLS may be incorporated into the mainstream clinical practice as a supplementary parameter for LVEF in patients with elevated troponin levels. Early screening and intervention for these patients may improve the prognosis, although we need to work together to develop larger datasets for modelling and to develop artif icial intelligence algorithms. Further research is needed to def ine cut-off values and to understand tachycardia and the hemodynamic eff ects in SCM patients.
None.
The research protocol was approved by the Institutional Review Board of Peking Union Medical College Hospital. Written informed consent was obtained from all patients(or their legal representatives) before being allowed to participate.All the authors declare that they have no conf licts of interest.
XF and JX: conceived and designed the study;XZY: study design assessment; XF: data acquisition; XF and LNZ:statistical analysis; FX: manuscript preparation; SS: manuscript editing; XL an HDZ: provided critical appraisal of the study; JX and ZXY: manuscript review. All authors read and approved the f inal manuscript.
All the supplementary files in this paper are available at http://wjem.com.cn.