Prognostic diff erences of catestatin among young and elderly patients with acute myocardial infarction
2022-09-17WeixianXuYuanyuanFanYaoSongXinLiuHuiLiuLijunGuo
Wei-xian Xu, Yuan-yuan Fan, Yao Song, Xin Liu, Hui Liu, Li-jun Guo
Department of Cardiology, Peking University Third Hospital, Beijing 100191, China
KEYWORDS: Catestatin; Acute myocardial infarction; Elderly; Outcome
INTRODUCTION
Catestatin, an active peptide derived from chromogranin A (CgA), was initially discovered as an endogenous antagonist of the nicotinic cholinergic receptor, which inhibited catecholamine release from both chromaffin cells and noradrenergic neurons. Subsequently, catestatin was found to act as a potent vasodilator by stimulating histamine excretion from mast cells.Catestatin is a multifunctional neuroendocrine peptide that is closely related to many cardiovascular diseases.In metabolic syndromes,serum catestatin levels are decreased compared to control patients.Catestatin is responsible for hepatic/plasma lipid and insulin regulation, improving insulin sensitivity,reducing hypertension, and attenuating obesity in murine models. Lower catestatin level is a signif icant risk factor for hypertensive adult patients.Plasma levels of catestatin are higher in patients with heart failure than those in the healthy control group.Catestatin also reflects myocardial fibrosis and sympathetic overactivity during acute worsening of heart failure or acutely decompensated heart failure.The predictive value of plasma catestatin in chronic heart failure patients was also reported in a study conducted on 202 patients with chronic heart failure, in which catestatin was an independent and strong risk factor for all-cause mortality and cardiac death.For coronary artery disease (CAD),conf licting results have been recently reported with increased or decreased plasma levels of catestatin in patients with CAD. An early study showed that catestatin levels increased after acute myocardial infarction (AMI).Increased circulating catestatin levels have also been correlated with the occurrence of malignant arrhythmia,adverse events(death from cardiovascular causes, readmission with ACS or CHF),and left ventricular remodeling after AMI.In agreement with these results, we previously found that plasma catestatin levels decreased in patients with AMI and unstable angina compared to patients without a diagnosis of CAD, and there were no associations between catestatin and major adverse cardiac events (MACEs).Recent studies have reported that circulating levels of catestatin signif icantly decreased in patients with CAD compared with the healthy control group.Furthermore, serum catestatin concentration was inversely associated with the severity of atherosclerosis.
Studies focusing on the pathophysiological mechanisms report that catestatin suppresses plaque progression and preserves vascular elasticity by suppressing lipopolysaccharide(LPS)- or tumor necrosis factor-α (TNF-α)-induced expression of intercellular adhesion molecule-1 (ICAM-1) and vascular cell adhesion molecule-1 (VCAM-1) in human embryonic cells (ECs), suppressing the inflammation in human macrophages, the proliferation of human vascular smooth muscle cells (VSMCs), and the expression of collagen-1 and collagen-3, and by increasing elastin expression.Catestatin can be used to defend against oxidative stressinduced apoptosis by activating the beta 2 adrenergic receptor and protein kinase B (PKB/Akt) pathway in the ischemicreperfused myocardium.In cultured ECs, catestatin suppressed TNF-α-induced expression of inflammatory cytokines and adhesion molecules by activating angiotensinconverting enzyme 2 (ACE2).These multiple effects establish catestatin as a master regulator of cardiovascular functions.Catestatin might be used as a new biological marker for cardiovascular diseases; however, further studies are needed.
There have been no studies about the predictive value of catestatin for AMI in elderly patients. Our previous study found that catestatin levels were not associated with MACEs during a follow-up period of two years.However,outstanding questions still remain such as whether catestatin can predict MACEs if the follow-up period is longer or whether the predictive value of catestatin differs between young and elderly patients with AMI.
The present study aims to investigate the associations between plasma catestatin levels and long-term outcomes of AMI and the diff erences in the prognostic value of catestatin in young and elderly patients with AMI.
METHODS
Subjects
Patients with AMI who underwent emergency percutaneous coronary intervention (PCI) for the first time within 12 h after symptom onset between July 2012 and December 2013 at Peking University Third Hospital were enrolled in this series. AMI was diagnosed based on the universal definition of MI: troponin elevation in conjunction with ischemic symptoms, ischemic electrocardiogram changes, and imaging evidence. AMI included ST-segment elevation myocardial infarction(STEMI) and non-ST-segment elevation myocardial infarction (NSTEMI), according to the universal definition of myocardial infarction put forth by the European Society of Cardiology and the American Heart Association.
The exclusion criteria were as follows: patients whose symptom onset lasted more than 12 h; patients who underwent thrombolysis, unsuccessful PCI(Thrombolysis in Myocardial Infarction [TIMI] score from 0 to 2 at the end of the procedure), or emergency surgery; patients with rheumatic heart disease, severe valvular heart disease, chronic congestive heart failure,cardiomyopathy, deep venous thrombosis, acute pulmonary embolism, infection, systemic inf lammatory,tumor disease, documented renal failure, or clinical evidence of renal impairment.
The study protocol conformed to the ethical guidelines of theand was approved by the Institutional Review Board of the Peking University Third Hospital. Written informed consent was obtained before coronary angiography.
Assays for plasma catestatin
Blood samples for catestatin measurements were obtained from the antecubital vein without stasis in all patients before coronary angiography. Blood samples were collected in chilled ethylene diamine tetra acetate(EDTA) vacutainers containing 2,500 U/mL aprotinin,immediately centrifuged at 3,000 r/min for 10 min at 4°C, and stored at −80 °C until analysis. Plasma catestatin levels were measured using a catestatin ELISA kit (Phoenix Pharmaceuticals, USA), according to the manufacturer’s instructions. Measurements were obtained by trained technicians in the clinical laboratory of the hospital.
Medical data
The clinical and laboratory data of all subjects were collected from medical records. Clinical data included risk factors for coronary heart disease, such as age, sex,hypertension, dyslipidemia, diabetes mellitus (DM),smoking, and body mass index. Left ventricular ejection fraction (LVEF) was assessed by echocardiography using Simpson’s method during the first 24 h after admission to the cardiac care unit. Other laboratory indicators, such as routine blood tests and lipid and glucose levels, were also assessed.defined as<0.05. Statistical analysis was performed using SPSS (Version 19.0).
MACEs
All patients were followed-up every three months through clinical interviews or telephone calls to collect information regarding MACEs after discharge. Patients were followed-up until the first MACE within four years. If no MACEs occurred, the patients were followed up for four years after discharge. MACEs included cardiovascular death, recurrent AMI, re-hospitalization for heart failure, and revascularization. All MACEs were conf irmed using the medical records.
RESULTS
The final study included 165 patients, including 113 with NSTEMI and 52 with STEMI. There were 24 MACEs(16 readmissions for revascularization, three recurrent myocardial infarctions, and f ive rehospitalizations for heart failure) among 165 patients, including 102 young patients(<60 years old) and 63 elderly patients (≥60 years old). The MACEs group had lower catestatin levels than the non-MACEs group (0.74±0.49 ng/mL vs. 1.10±0.79 ng/mL,=0.033) and were older (59.0±11.4 years old vs. 53.2±12.8 years old,=0.036). The rate of MACEs was significantly higher in the elderly group than in the young group (23.8%[15/63] vs. 8.8% [9/102],=0.008). The proportion of females was higher in the elderly group than in the young group (=0.001). Elderly patients were more likely to have hypertension (=0.009), but were less likely to smoke(=0.001). The rates of dyslipidemia and DM were not signif icantly diff erent between the young and elderly groups.The counts of white blood cell (WBC) and platelet (PLT)were lower in the elderly group (=0.005,=0.009). The catestatin levels in the elderly group were not significantly higher than those in the young group (=0.069). There were no significant differences among the other indicators. The details were shown in supplementary Table 1.
As shown in Table 1, the young patients with MACEs had lower hemoglobin (=0.009) and lower LVEF(=0.004). The catestatin levels did not significantly differ
Statistical analysis
Descriptive statistics were used for all baseline variables, with means and standard deviations for normally distributed variables; medians and interquartile ranges for non-normally distributed variables; and rates and proportions for categorical variables. Student’s-test and Pearson’s Chi-square test were used to compare differences between the groups. Kaplan-Meier hazard analyses were plotted for AMI patients with low and high catestatin levels according to the median level (0.86 ng/mL). The association between catestatin and MACEs was assessed using Cox proportional hazards regression,in which confounders such as sex, hypertension,dyslipidemia, DM, smoking, and LVEF were also included. All analyses were carried out among young and elderly patients with a cut-off age of 60 years. All tests of signif icance were two-tailed. Statistical signif icance wasbetween the MACEs group and the non-MACEs group in the young group, while they were significantly lower in the elderly group (0.76±0.50 ng/mL vs. 1.31±0.77 ng/mL,=0.012). Other baseline characteristics were similar between the MACEs and non-MACEs groups.

Table 1. The diff erences of baseline clinical characteristics between MACE and non-MACE group respectively among young and elderly patients
MACEs were significantly different between low and high levels of catestatin (Kaplan Meier,=0.007)in the elderly group, but not in the young group (Kaplan Meier,=0.893) (Figure 1). In the Cox proportional hazards regression analysis to explore the predictors of MACEs among elderly patients, high catestatin was one of the independent factors (hazard ratio [] 0.19,95% confidence interval [] 0.06–0.62,=0.006) after adjustment for other risk factors (Table 2). However, in the young patients, LVEF, but not catestatin, was one of the independent factors (0.93, 95%0.88–0.98,=0.004) (Table 3).
DISCUSSION
In the present study, patients with lower plasma catestatin were more likely to have MACEs. Plasma catestatin levels were an independent factor for MACEs after adjusting for confounders. These findings were signif icant among elderly patients but not among young patients. The prognostic value of catestatin for MACEs among patients with AMI differed between the young and elderly groups.
Our findings are consistent with those of previous studies.Chen et alreported that serum catestatin concentration was lower in patients with CAD and that decreased circulating catestatin levels were inversely correlated with disease severity. Low plasma catestatin is a valuable prognostic parameter in predicting death from all causes and unplanned hospitalization in patients with heart failure with reduced ejection fraction at the two-year follow-up.In our previous study,patients with CAD also had lower catestatin levels. However,catestatin did not predict MACEs at the two-year followup. In the present study, when patients were dividedinto two groups (young or elderly patients), we found that catestatin was an independent factor for MACEs after adjusting for confounders among elderly patients during the four-year follow-up. Compared with low catestatin levels,high levels of catestatin reduced the MACE risk (0.19).

Table 2. The Cox regression model for MACEs among elderly patients
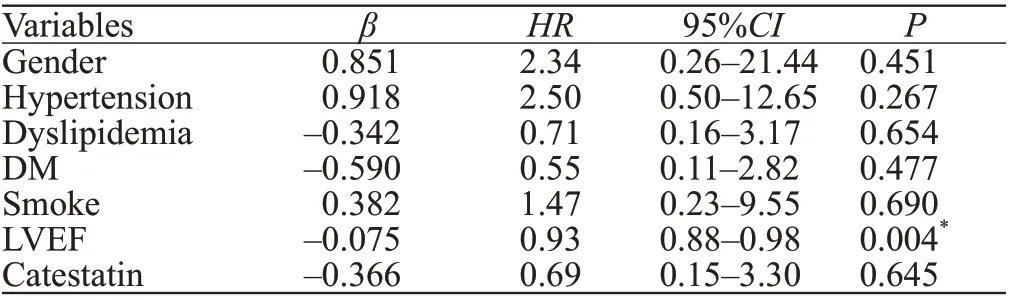
Table 3. The Cox regression model for MACEs among among young patients

Figure 1. The associations between catestatin and major adverse cardiovascular events (MACEs) among young and elderly patients. A: the MACEs were not signif icantly diff erent between low and high levels of catestatin among young patients (Kaplan Meier, P=0.893); B: elderly patients with lower catestatin levels were more likely to have MACEs (Kaplan Meier, P=0.007).
These data show that catestatin is a master regulator of cardiovascular function through multiple mechanisms.(1) Catestatin exerts vasodilatory effects through inhibiting catecholamine secretion, stimulating histamine release,and increasing nitric oxide (NO) release from vascular ECs.Catestatin infusion directly dilates blood vessels and reduces blood pressure.(2) Catestatin exerts anti-atherosclerotic effects. (3) Catestatin exerts protective effects against ischemia/reperfusion-induced myocardial dysfunction via the NO-dependent pathway in rats.Catestatin also exerts direct protective effects on rat cardiomyocytes undergoing ischemia/reperfusion by stimulating the phosphoinositide 3-kinase (PI3K)/protein kinase B (Akt)/glycogen synthase kinase 3β (GSK3β)pathway.(4) Catastatin reduces inf lammation through its role in tissue homeostasis by regulating immune cell infiltration and macrophage differentiation. Catestatin has been shown to reduce inflammation in various mouse models of diabetes, colitis, and atherosclerosis where catestatin treatment resulted in less infiltration of immune cells into affected tissues.(5) Catestatin plays an important role in angiogenesis by stimulating the migration and proliferation of ECs and contributing to ischemia-induced angiogenesis.Catestatin is associated with the development of coronary collateral circulation and chronic myocardial ischemia.A growing body of evidence suggests that catestatin may be an interesting therapeutic target for CAD treatment and/or diagnosis.
In the present study, age was an important factor affecting the predictive value of catestatin. Among elderly patients, high levels of catestatin can reduce the risk of MACEs, but not in young patients.Pathophysiological states can change with age, which may explain the conflicting results regarding reports of increased or decreased plasma levels of catestatin in patients with CAD. Other factors may also have contributed to the variance in the results of different studies. Catestatin changes with the time of onset of ischemia;therefore, the time point of the sample would lead to differences in catestatin levels. The types of CAD and concomitant diseases could also affect catestatin levels.
This study provides new insights into catestatin at different ages. However, there are some limitations to this study that need to be addressed. First, catestatin levels were measured at only one time point; therefore,dynamic changes in each patient were not obtained.Other indicators such as CgA and norepinephrine were not assessed in this study. Second, we did not examine the mechanism underlying the association between catestatin use and MACEs. Third, the sample size of this study was small. Prospective, large-sample trials are needed to investigate the associations and mechanisms between plasma catestatin and MACEs.
CONCLUSIONS
Elderly patients with lower plasma catestatin levels were more likely to have MACEs. Catestatin may be a novel marker for the long-term prognosis of AMI,especially in elderly patients. More eff orts to investigate the key roles of catestatin bioactivity and to detect its levels at different time points in various ages are necessary to thoroughly assess its pathophysiological function and value as a prognostic marker.
This work was supported by the National Natural Science Foundation of China (81400319).
The study protocol conformed to the ethical guidelines of the. The written informed consent to participate in the study were obtained from all participants. The study was approved by the Institutional Review Board of Peking University Third Hospital.
The authors have no conf licts of interest to declare.
WXX and YYF are the co-first authors. WXX,YYF, and LJG designed and carried out the study, wrote and revised the manuscript; YS and XL collected and analyzed data;HL analyzed the data and revised the manuscript. All authors reviewed the manuscript.