Innovative immunosuppression in kidney transplantation: A challenge for unmet needs
2022-07-29MaurizioSalvadoriArisTsalouchos
Maurizio Salvadori, Aris Tsalouchos
Maurizio Salvadori, Department of Renal Transplantation, Careggi University Hospital, Florence 50139, Italy
Aris Tsalouchos, Division of Nephrology, Santa Maria Annunziata Hospital, Florence 50012, Italy
Abstract Due to the optimal results obtained in kidney transplantation and to the lack of interest of the industries, new innovative drugs in kidney transplantation are difficult to be encountered. The best strategy to find the new drugs recently developed or under development is to search in the sections of kidney transplantation still not completely covered by the drugs on the market. These unmet needs are the prevention of delayed graft function (DGF), the protection of the graft over the long time and the desensitization of preformed anti human leukocyte antigen antibodies and the treatment of the acute antibody-mediated rejection. These needs are particularly relevant due to the expansion of some kind of kidney transplantation as transplantation from non-heart beating donor and in the case of antibody-incompatible grafts. The first are particularly exposed to DGF, the latter need a safe desensitization and a safe treatments of the antibody mediated rejections that often occur. Particular caution is needed in treating these drugs. First, they are described in very recent studies and the follow-up of their effect is of course rather short. Second, some of these drugs are still in an early phase of study, even if in well-conducted randomized controlled trials. Particular caution and a careful check need to be used in trials launched 2 or 3 years ago. Indeed, is always necessary to verify whether the study is still going on or whether and why the study itself was abandoned.
Key Words: New drugs; Unmet needs in kidney transplantation; Delayed graft function; Long-term outcomes; Kidney inflammation; Anti-human leukocyte antigen antibodies
INTRODUCTION
Little progress has been made over the past decade in the development of new therapeutic measures in clinical kidney transplantation, chiefly because of a lack of interest by industries and providers and because most centers have reached optimal outcomes with the drugs used today[1]. However, a strategy may be adopted to identify new immunosuppressant drugs in kidney transplantation.
New immunosuppressant drugs may be found looking for identified unmet therapeutic needs.
These new drugs may also be adopted as new immunosuppressive treatments or new strategies for special kidney transplantation scenarios such as ABO incompatibility, non-heart-beating donor (NHBD) transplantation and transplantation from high-risk donors.
Drugs for unmet therapeutic needs
These drugs may be categorized as follows: (1) Therapy for ischemia-reperfusion injury (IRI) that results in delayed graft function (DGF); (2) Therapy to preserve optimal kidney function over the long-term; and (3) Therapy for desensitization and antibody-mediated rejection (ABMR).
THERAPY FOR DGF
DGF refers to acute kidney injury (AKI) occurring in the first week of transplantation that cannot not be ascribed to acute rejection[2].
DGF is associated with increased immune activation, complement activation and release of damageassociated molecular patterns, such as hypomethylated DNA, hyaluronic acid, heparin sulfate, fibrinogen and heat shock proteins. Consequently, nuclear factor κB is activated and induces inflammatory cytokines such as interleukin (IL)-1, IL-6, tumoral necrosis factor alpha and interferon beta[3].
Due to this complex mechanism, although several drugs to treat DGF have been tried, many of them failed to prove their effectiveness. Indeed, DGF has also been called the graveyard of drugs for transplantation.
However, new drugs have recently emerged and they are still in randomized controlled trials (RCTs) to control DGF.
Anti-apoptotic strategies
Apoptosis plays an important role in shaping DGF. Indeed, the pro-apoptotic gene p53 is activated by hypoxia and induces cell cycle arrest and apoptosis[4].
QPI-1002 also known as 15 NP, is a short interfering RNA that inhibits the expression of p53. The results of a phase I/II clinical trial in kidney transplant recipients demonstrated beneficial effects on IRI/DGF in humans[5]. Additionally, two studies reported good results in mice[6,7]. However, the RCT was terminated in 2018 without positive results because of a lack of documented efficacy.
Pegylated carboxyhemoglobin
Carbon monoxide (CO) is involved in regulating endothelial cell survival and proliferation. It also plays roles in protecting against DGF through IRI, vessel relaxation and inhibition of proinflammatory responses[8-10]. The infusion of pegylated carboxyhemoglobin delivers CO to organs. CO is a very powerful anti-apoptotic substance and has anti-inflammatory effects. In animal studies, CO is extremely effective in both cold and warm ischemia.
The use of pegylated carboxyhemoglobin is currently the object of a phase 2/3 study to analyze the efficacy and safety of SANGUINATE for reducing the DGF rate in patients receiving a kidney transplant[11,12]. In a recent study by Thuillieret al[13], 3 oxygen transporters, HBOC-201, BbV and M101, were tested in organ preservation[13-15].
Relaxin
In DGF, relaxin (RLX) has an anti-inflammatory effect by reducing the expression of intracellular adhesion molecule 1, inducing the expression of Notch 1 in macrophages and reducing neutrophil adhesion through increased synthesis of nitric oxide[16-18]. Additionally, RLX causes vasodilatation through increased NO production and inhibition of endothelin 1 production[19]. Two studies[18,20] documented improved renal function, histologic improvement in damaged tissue after DGF, and a reduced number of apoptotic cells.
Hepatocyte growth factor
ANG-3777, formerly BB3, is a hepatocyte growth factor mimetic that binds to its transmembrane tyrosine kinase receptor, cMET[21]. In preclinical studies, ANG-3777 was renoprotective in a variety of animal models of AKI, exerting anti-inflammatory and regenerative effects and preventing tubular cell apoptosis, epithelial to mesenchymal transition and fibrosis[22,23]. In a randomized, placebo-controlled phase 2 trial on oliguric patients after kidney transplantation, patients treated with ANG-3777 had a larger increase in urine output, a greater reduction in C reactive protein and neutrophil gelatinaseassociated lipocalin and a higher estimated glomerular filtration rate (eGFR)[24]. More recently, Vincentiet al[25] started the Graft Improvement Following Transplant (GIFT) trial, which is a phase 3 trial on the hepatocyte growth factor mimetic ANG-3777 in kidney transplant recipients with DGF. The aim of GIFT is to generate data to advance the treatment of DGF. In addition, the authors stress that a significant factor is that ANG-3777 may also be effective when administered after AKI-related DGF.
Complement inhibition
Complement activation plays a significant role in IRI, which causes and precedes DGF. The most studied among the complement inhibitor drugs to minimize DGF has been Mirocept (APT 070), which inhibits C3/C5 convertases and C1 esterase inhibitors.
Mirocept, still in a phase 1 trial (ISRCTN49958194)[26], is a potent membrane-localizing complement inhibitor and may be administeredex vivoto the donor kidney prior to transplantation. However, a recent dose finding study in animals[27] documented that a high dose of Mirocept might be needed to achieve adequate complement inhibition. More promising results have been obtained with C1 esterase inhibition.
This drug may also be administered as a donor pretreatment strategy in high-risk recipients (NCT02435732)[28], but the trial results are still unknown. Better results have been obtained by administering C1 esterase inhibitors to recipients of kidneys from high-risk donors or in the case of donation after circulatory death (DCD)[29-31]. A recent study from Huanget al[32] studied the three-year outcomes of patients treated with C1 esterase inhibitors to avoid DGF in a randomized controlled study. The study found that the treatment was associated with a lower incidence of graft failure.
Table 1 summarizes representative drugs in the categories described above used to prevent DGF and their targets.

Table 1 Therapies targeting delayed graft function in kidney transplantation
Improving perfusion techniques
Improving perfusion techniques is not drugs in the sense of the word but rather a different strategy to prevent IRI and DGF by improving kidney perfusion at the time of kidney transplantation.
In a recently published study, Urbanelliset al[33] documented that continuous normothermicex vivokidney perfusion significantly improved early kidney function compared with hypothermic anoxic machine perfusion and static cold storage (SCS) in a porcine kidney auto-transplantation model.
A more interesting study was performed by Niemannet al[34]. The authors documented that reducing the body temperature by 2 °C of the deceased donor achieved a significant reduction in DGF rates and that the effect was more significant in the extended criteria donors.
Finally, in a recent review[35], it was documented that active oxygenation during hypothermic machine perfusion is the most beneficial in cases involving the use of DCD kidneys when applied starting from kidney procurement until transplantation. Active oxygenation improves preservation and subsequent early graft function.
THERAPY TO PRESERVE RENAL FUNCTION
These drugs may be divided into the following categories: (1) Therapy to avoid nephrotoxicity, usually by elimination of calcineurin inhibitors (CNIs); (2) Therapy to control inflammation and fibrosis (principally when inflammation overlaps fibrosis); and (3) Therapy to prevent donor-specific antibodies (DSAs) and treat chronic ABMR (cABMR).
Therapy to avoid nephrotoxicity induced by CNIs
Until recently and even today, the two main strategies for a CNI-free regimen have been as follows: Mammalian target of rapamycin inhibitor-based immunosuppression; belatacept based immunosuppression.
Several studies have documented the efficacy of everolimus therapy in conjunction with low-dose CNIs[36-39]. The study by Pascualet al[36] “the Advancing renal TRANSplant eFficacy and safety Outcomes with eveRoliMus based regimen (TRANSFORM)” was a randomized open label, two-arm study with 2037de novokidney transplant recipients recruited in 186 centers worldwide. Everolimus efficacy was demonstrated, but the administration of low-dose tacrolimus (TAC) was needed.
The complete withdrawal of CNIs is difficult to achieve and is only appropriate for low-risk patients and donors and for living donors, and in the absence of DSAs[40].
The use of belatacept or other agents blocking the costimulatory pathways is the other method to avoid CNIs.
The blockade of CD28/cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4) on T effector lymphocytes and CD80/CD86 on antigen presenting cells (APCs) was the first pathway to be targeted in the trials BENEFIT and BENEFIT-EXT[41,42] . Independent of well-preserved kidney function, the use of belatacept in a subset of patients was associated with an increased number of severe rejections[43,44] and an increased number of opportunistic infections[45] , including cytomegalovirus[46]. In addition a correlation between the incidence of post-lymphoproliferative disease and Epstein-Barr virus seronegative patients in the belatacept group was found[47].
These drawbacks are related to the fact that belatacept, which binds to CD80 and CD86 on APCs, blocks not only the T effectors that represent the positive signal but also the regulatory T (Tregs) that constitute the inhibitory signal (Figure 1).

Figure 1 Block of co-stimulation with Belatacept. APC: Antigen presenting cell; T eff: T effector; T reg: Regulatory T cells; PDL1: Programmed cell death receptor ligand 1; CTLA4: Cytotoxic T-lymphocyte-associated antigen 4.
In 2015, a report showed that the blockade of CD28 on effector T cells without inhibition of Treg cells prolonged survival in a nonhuman primate kidney transplant model. In this way, effector cells can be inhibited without inhibiting Tregs because selective CD28 blockade allows inhibitory signalsviaCTLA-4 and programmed cell death ligand-1 to remain intact while blocking T cell activation by CD28[48] (Figure 2).

Figure 2 Block of co-stimulation with anti CD28. APC: Antigen presenting cell; T eff: T effector; T reg: Regulatory T cells; PDL1: Programmed cell death receptor ligand 1; CTLA4: Cytotoxic T-lymphocyte-associated antigen 4.
Selective targeting of the CD28 antigen on T cells might be a more effective immunosuppressive therapy than belatacept, since this blockade leaves the inhibitory signal of CTLA-4 intact and may preserve Treg functions[49-51].
Currently, two monovalent antibodies, FR104 and lulizumab-pegol are under development for clinical application. These antibodies have antagonistic activity against CD28 alone[52,53]. To date, an RCT has been conducted at the University of California to modulate Tregs with combinatorial treatment with CD28 and IL-6 receptor antagonists[54] (Figure 3). The addition of an IL-6 receptor antagonist (tocilizumab) aims to further stimulate Treg cells and exert an anti-inflammatory effect. In the CTOT24 trial, after induction with thymoglobulin, steroids are administered from the beginning, lulizumab is started at the beginning and then continued weekly through day 77, belatacept is started on day 84 and administered every 4 wk, tocilizumab is started at the beginning and continued every 2 wk through day 168, and everolimus is started on day 14 and administered twice daily.

Figure 3 CTOT24 trial.
A different way to block costimulation is to block the interaction between CD40 and CD40 L. A first attempt was made to block the CD 40 receptor, but the studies were interrupted because of a number of thromboembolic complications[55,56]. This was because CD40 L is also expressed on platelets, which causes thromboembolic complications.
In 2014, Okimuraet al[57] reported that ASKP 1240, a fully human antibody targeting human CD40, had a potent immunosuppressive effect that did not interfere with platelets.
Recently, in a phase 1b study, the safety and efficacy of bleselumab, a fully human anti-CD40 monoclonal antibody, was documented by Vincentiet al[58]. The results were confirmed by a phase 2, randomized, open label, noninferiority study by Harlandet al[59].
Novartis claimed to have developed another anti-CD40 monoclonal antibody (CFZ-533, Iscalimab). The antibody was characterized by several studies[60,61] . The antibody is the object of an RCT inde novorenal transplantation[62] to demonstrate comparable efficacy to and better renal function than TAC inde novoCNI-free kidney transplantation.
Until recently, it was believed that the main cause of kidney injury over time after transplantation was primarily due to CNI nephrotoxicity.
The first study questioning this opinion was the DeKAF study by Gastonet al[63] . The study documented that the decline in kidney function was not only due to CNI nephrotoxicity but also due primarily to the presence in the recipient of DSAs and the consequent activation of the humoral response[64]. Indeed, long-term graft survival was lower in patients with DSAs in the serum and C4d, a marker of immune response activation on the glomerular capillary wall. The role of DSAs and ABMR was further documented by Sellaréset al[65] and Lefaucheuret al[66]. A separate study documented that bothde novoand pre-existing DSAs caused ABMR and reduced graft survival[67].
A more recent study by Stegallet al[68] examined 575 surveillance biopsies of kidney transplants from living donors on low-dose TAC therapy and found that 82% of patients whose grafts survived 10 years were affected by inflammatory lesions not related to CNI toxicity or to immunological mechanisms.
Preserving renal function requires other therapies in addition to safely reducing or withdrawing CNIs.
Therapy to control inflammation and fibrosis not related to immunological causes
Several factors, such as hyperuricemia, glucose intolerance, arterial hypertension, dyslipidemia and infection, may induce an inflammatory state in kidney transplant patients[69]. In addition, chronic hypoxia mediated by IL-1 and IL-6, angiotensin II and transforming growth factor beta may result in the accumulation of extracellular matrix, which can lead to interstitial fibrosis. In particular, several studies[70-72] document that IL-6 leads to allograft injury by acute inflammation, adaptive cellular/humoral responses, innate immunity and fibrosis. All these studies indicate that IL-6 is a mainstay in inducing inflammation and allograft injury.
Several drugs have been proposed to control the graft inflammatory state, including low-dose aspirin, statins, renin-angiotensin inhibitors, and xanthine-oxidase inhibitors, but no prospective trial with these drugs has been conducted in kidney transplantation. The only drug object of an RCT is the IL-6R inhibitor.
Currently, available agents for IL-6 signaling inhibition include monoclonal antibodies against IL-6 or IL-6R and Janus kinase inhibitors. The most often studied is tocilizumab, an IL-6R blocker. In a study conducted by Chandranet al[73], IL-6 blockade with tocilizumab increased Tregs and reduced T effector cytokines in renal graft inflammation. Tocilizumab-treated patients showed an improved tubulointerstitial Banff score and an increased Treg frequency.
Therapy to control chronic humoral rejection
Important advances have been made in the treatment of ABMR, but less effective treatments are available to control cABMR, which is a slowly progressing disease in which grafts are primarily injured byde novoDSAs[74].
Until recently, attempts to treat cABMR had been limited to a combination of plasmapheresis and intravenous immunoglobulins (IVIGs)[75] and rituximab (RTX)[76,77]. Recently, proteasome inhibitors such as bortezomib[78] and carfilzomib[79] have also been studied, but these drugs were not as effective as anticipated.
In addition, complement inhibitors such as C1 inhibitors (C1-INH) and eculizumab, failed to control cABMR[80,81] probably because antibodies may injure the endothelium in a complement-independent pathway. Better results have been obtained with the use of IL-6R or IL-6 inhibitors.
In a previous study, Shinet al[82] documented the efficacy of tocilizumab in blocking monocyte activation in anin vitromodel, to inhibit the inflammatory cascade induced by alloantibodies. In a more recent study, Shinet al[83] documented a beneficial effect of tocilizumab on cABMR owing to a reduction in antibody production by B cells.
Similarly, Choiet al[84] documented a reduction in DSAs and cABMR and stabilization of renal function in patients with cABMR, DSAs and transplant glomerulopathy treated with tocilizumab. A phase 4 RCT in patients with cABMR was recently designed[85].
Clazakizumab is a humanized monoclonal antibody directed against IL-6. In a study by Dobereet al[86], clazakizumab reduced DSAs and demonstrated beneficial effects on cABMR and renal function.
THERAPY FOR DESENSITIZATION AND ACUTE ABMR
Desensitization and treatment of ABMR are the two faces of the same coin. It has already been discussed how DSAs play a relevant role in inducing AKI and graft failure. DSAs may already be present before transplantation, or they may appearde novoafter kidney transplantation. In both conditions, they may cause ABMR.
Desensitization is the treatment to reduce or, when possible, completely eradicate DSAs before or at the time of transplantation. Treatment of ABMR includes powerful drugs aimed at controlling this severe complication.
To better understand the mechanism of action of these drugs, Figure 4 represents how DSAs are formed and where the immunosuppressant drugs may act[87]. Naïve CD4+ T cells recognize the antigen presented by APCs. Activated CD4+ cells process antigens, which are presented to naïve B cells. Costimulatory molecules mediate the presentation through CD80/86 and CD28. B cell maturation and development into B-memory cells and plasma cells (PCs) is regulated by cytokines (principally IL-6 and IL-21), B cell activating factor (BAFF) and a proliferation-inducing ligand that interact with B cell maturation antigen. PCs produce antibodies that bind to donor-specific human leukocyte antigen (HLA) molecules, activate complement and initiate injury leading to ABMR. Agents capable of interfering with this complex system are numerous and act at different levels.

Figure 4 Drugs acting at different levels to control the antibody formation. BLyS: B Lymphocyte stimulating factor; mAb: Monoclonal antibody; C1-INH:C1 inhibitors; NK: Natural killer; Cp: Complement; FcyR: FcyReceptor; MAC: Membrane attacking complex; MHC: Major histocompatibility complex; IL: Interleukin.
Several studies and reviews have described the drugs used in desensitization and in the treatment of ABMR[88-93].
Novel agents will be discussed in this chapter. New agents acting on costimulatory signals have already been discussed[48,49,57,59]. Similarly, anti-IL-6/IL-6R agents have been discussed[83-86].
Obintuzumab is a type 2 anti-CD20 antibody that induces more robust B cell depletion than RTX. To date, the drug has been evaluated in a phase 1b study to induce desensitization[94].
Belimumab belongs to the anti BAFF family. The drug is effective in treating systemic lupus erythematosus[95] but less effective in treating ABMR[96] due to possible infective complications. Proteasome inhibitors such as bortezomib and carfilzomib act on PCs, but are not as effective as anticipated. Carfilzomib has been studied in desensitization in a nonhuman primate model[97].
Drugs acting directly on PCs target CD38. Several studies or case reports have documented the efficacy of daratuzumab in the treatment of ABMR[98-100]. Isatuximab is effective on PCs and other immune cells, such as Tregs and Bregs. This fact may limit its applicability in the treatment of ABMR[101].
Inebilizumab is a humanized anti-CD19 monoclonal antibody approved for neuromyelitis optica[102].
An RCT with inebilizumab for pretransplant desensitization[103] was suspended due to the coronavirus disease pandemic.
Finally, another fully human monoclonal antibody, anti-CD38, is the object of an RCT for the treatment of ABMR[104].
In ABMR, the activation of the complement cascade is triggered by ligation of the C1 complex to HLA antigens that are bound by DSAs. Several drugs are capable of blocking complement activation (Figure 5). The C1 complex is activated upon antibody binding. The humanized monoclonal antibody BIVV009 (sutinlimab) targets its enzymatic subcomponent C1 s and this therapy blocks C4 and C2 cleavage and the formation of C3 convertase.
A phase 1 study with this drug[105] was concluded, and Eskandaryet al[80] studied 10 kidney transplant recipients with ABMR. Repeated biopsies documented a reduction in C4d deposition even if DSA levels and microvascular inflammation were unchanged.

Figure 5 Principal drugs affecting complement. C1-INH: C1 inhibitor; MAC: Membrane attacking complex.
C1-INH regulates several pathways that contribute to complement activation and cause ABMR.
In 2015, in a phase I/II placebo-controlled trial, Voet al[106] reported the efficacy of C1-INH in the prevention of ABMR in HLA-sensitized patients. Later, Montgomeryet al[107] in a randomized controlled pilot study, documented the efficacy of C1-INH in controlling ABMR. More recently, two more studies are ongoing to document the efficacy of human plasma C1 esterase inhibition as an addition to the standard of care for the treatment of ABMR[108,109].
The humanized monoclonal antibody eculizumab binds to C5 with high affinity and prevents C5 convertase-mediated cleavage to C5a and C5b. In the past, several studies documented the efficacy of eculizumab in treating ABMR[110-112]. Recently, other studies documented the efficacy of eculizumab in treating and preventing ABMR[113,114]. Antibody removal is another therapeutic technique that may be applied primarily to desensitize patients with preformed DSAs before transplantation. Until recently, antibody removal and/or inhibition have been performed by plasmapheresis and IVIGs. Recently, it was documented that imlifidase (IdeS), a recombinant cysteine protease derived from Streptococcus pyogenes, rapidly cleaves IgG in the lower hinge region to a Fab fragment and a dimeric Fc fragment[115] (Figure 6). In addition to eliminating HLA antibodies, Geet al[116] demonstrated that IdeS is a potent inhibitor of antibody-dependent cell cytotoxicity. A drawback of IdeS treatment is antibody recurrence after the interruption of the treatment. Incorporation of plasmapheresis and RTX to this treatment may overcome this drawback.
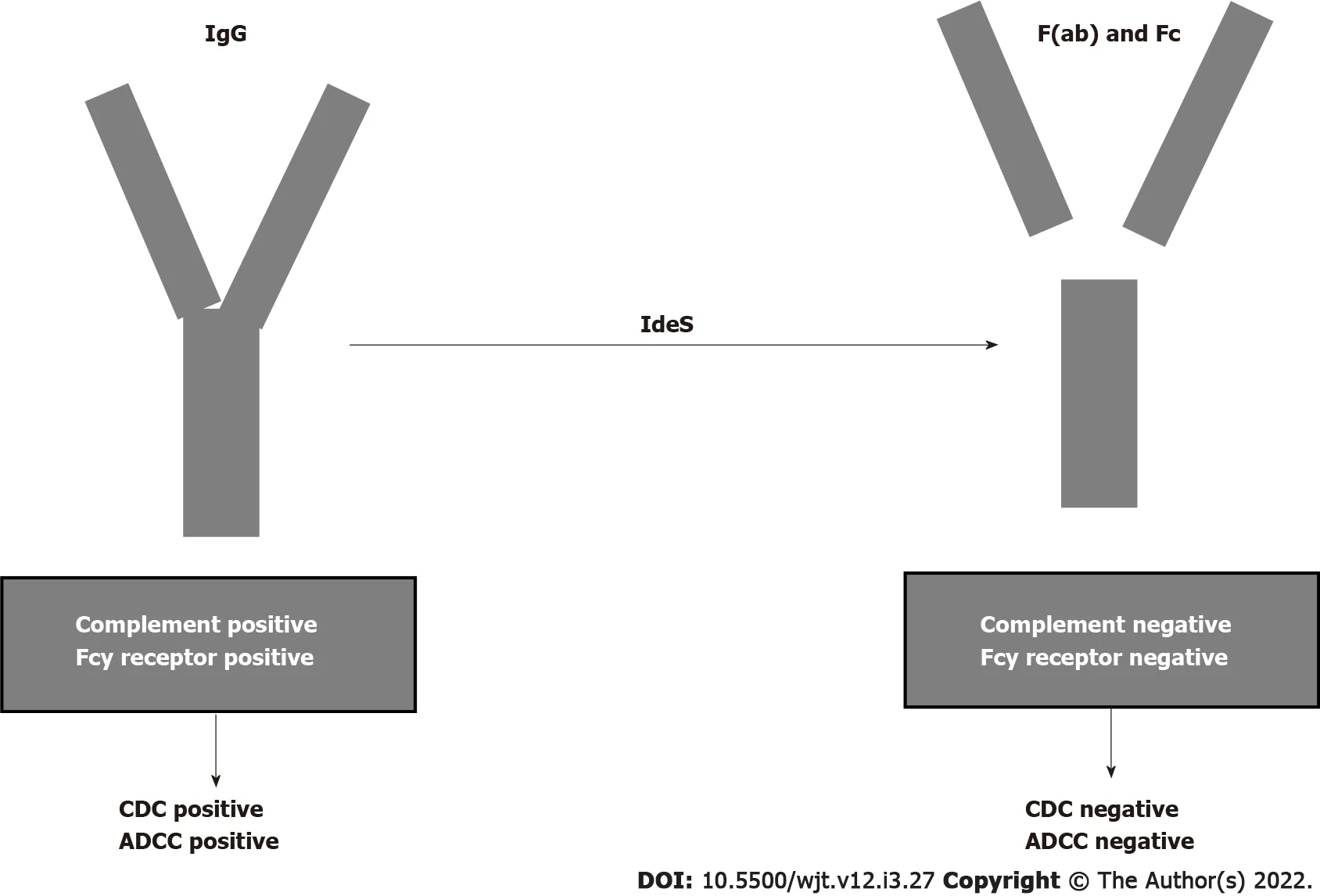
Figure 6 Cleaving intact immunoglobulin G by imlifidase. CDC: Complement dependent cytotoxicity; ADCC: Antibody dependent cell cytotoxicity; F(ab):Fragment ab; Fc: Fragment c; Ides: Imlifidase; IgG: Immunoglobulin G.
An international phase 2 trial was conducted in five transplant centers[117] for desensitization of cross-match-positive, highly sensitized kidney transplant recipients. Antibody rebound occurred 3-14 d after lipopolysaccharide administration, but graft survival at six months was 88.9%. The study conclusion was that IdeS converted positive cross matches to negative cross matches and achieved the transplantation of high-sensitized patients with optimal results at 6 mo.
In a more recent study, Kjellmanet al[118] documented that lipifidase treatment administered to 39 cross-match-positive patients accomplished a 3-year graft survival of 93% with an ABMR incidence of 38% in the first month post-transplantation.
CONCLUSION
Lack of interest by industries and optimal outcomes reached by the drugs used to date has resulted in little progress in finding new drugs. However, examining unmet needs in the field of kidney transplantation may help us to find new drugs. Needs not optimally covered by current drugs are control of DGF, improvement of the long-term immunosuppression with graft outcomes reduced by chronic damage and the control of desensitization and ABMR. The control of these needs is of outmost importance, considering the expanding numbers of new kinds of kidney transplantation as transplantation from older donors and from NHBDs and transplantation from antibody-incompatible donors.
In the first kind, controlling or reducing DGF is essential; in the latter kind, the reduction of antibodies against HLA is essential.
DGF may be controlled either with optimal management of the donor before or during kidney removal or with drugs attempting to target one of the multiple pathways involved in causing the IRI that is conducive to DGF.
New drugs are also emerging to control or reduce the antibody serum level. Several steps are involved in antibody generation and for each of those steps new drugs will be found.
In addition, drugs are able to reduce the nephrotoxicity induced by the long-term use of CNIs and to control kidney inflammation that may contribute to a worse graft outcome.
The majority of these drugs have been very recently found and are still in RCTs. Therefore, trials with novel agents require a careful approach and these new agents in transplantation face many challenges, but may provide a hopeful pipeline in this issue.
FOOTNOTES
Author contributions:Salvadori M and Tsalouchos A contributed equally to the manuscript; Salvadori M designed the study, performed the last revision and provided answers to the reviewers; Tsalouchos A collected the data from literature; Salvadori M and Tsalouchos A analyzed the collected data and wrote the manuscript.
Conflict-of-interest statement:Salvadori M and Tsalouchos A do not have any conflict of interest in relation to the manuscript, as in the attached form.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Italy
ORCID number:Maurizio Salvadori 0000-0003-1503-2681; Aris Tsalouchos 0000-0002-8565-4059.
S-Editor:Wang JJ
L-Editor:A
P-Editor:Wang JJ