Pancreatic cancer incidence and mortality patterns in 2006-2015 and prediction of the epidemiological trend to 2025 in China
2022-06-23MinYueYinLiTingXiLuLiuJinZhouZhuLiJuanQianChunFangXu
lNTRODUCTlON
Pancreatic cancer (PC) has one of the worst prognoses, with the age-standardized rate (ASR) of 5-year overall survival in 2014 hovering at 14.30% in Australia, followed by 11.40% in Canada and 9.88% in Norway according to CANCER SURVIVAL. The past decades have witnessed a remarkable increase in PC incidence and mortality globally. According to GLOBOCAN 2020, PC is the 13
most frequent cancer, with approximately 495773 new cases, and the 7
most fatal cancer, with approximately 466003 deaths in 2020[1].
The causes of PC remain unclear despite several known risk factors, such as tobacco smoking and a positive family history. A previous study showed three recognized risk factors for PC: smoking, elevated fasting plasma glucose and a high body-mass index (BMI)[2]. Moreover, a systematic review demonstrated that dietary patterns with better quality, such as the Mediterranean diet, with less inflammation or better antioxidant capacity, could reduce the risk of PC[3]. Due to a dietary pattern comprised of little fresh fruit and large amounts of red meat, PC has become one of the tumors with a rapidly increasing incidence in China[4]. Furthermore, along with the aging issue, environmental pollution and its huge population, China contributes significantly to the global burden of PC,
one-fourth of incident global cases and deaths in 2020[1].
In this study, we present the epidemiological status of PC in China from 2006 to 2015 from a series of nationally representative data, based on which we estimated the incidence and mortality rates of PC in 2025. In addition, we described the differences in PC distributions by age and region according to the global statistics in 2019. Furthermore, comparisons of PC epidemiological characteristics between China and other countries have also been made to inspire the prevention and control of PC in China.
MATERlALS AND METHODS
Data sources
Since 2002, the National Central Cancer Registry of China (NCCR), a department of the National Cancer Center, has collected, evaluated and released annual cancer data from local cancer registries in mainland China[5]. In August 2018, the NCCR released the cancer data of 2015 from 501 cancer registries of 31 provinces in China, among which 368 registries were eligible according to the following standards, and it provided an approximate 22.52% coverage of the national population[6]. First, the cancer registry data submitted to the NCCR were checked based on the data-quality criteria of the International Agency for Research on Cancer (IARC)/International Association of Cancer Registries[7] and the Guidelines for Chinese Cancer Registration[8]. Moreover, the quality assessment was evaluated based on the mortality to incidence (M/I, 0.61) ratio, the proportion of cases morphologically verified (MV%,69.34%), and the proportion of death certification only (DCO%, 2.09%)[6,9]. The PC incidence and mortality data before 2009 were agestandardized to the Chinese population census in 1982, and the data from 2010 to 2015 were agestandardized to the Chinese population census in 2000. All data for the PC incidence and mortality could be extracted from published articles from the National Cancer Center[5,9-17].
The IARC project, was established by the World Health Organization in May 1965, whose mission was to coordinate cancer research across countries globally (www.iarc.who.int). The Global Cancer Observatory (GLOBOCAN_GCO) is a featured research project website of IARC that consists of several parts, including CANCER TODAY and CANCER SURVIVAL (gco.iarc.fr). CANCER TODAY provides data on the incidence, mortality, and 1-, 3-, and 5-year prevalence for 2020 in 185 countries or territories for 36 cancer types based on codes from the International Statistical Classification of Diseases and Related Health Problems 10
Revision (ICD-10) (gco.iarc.fr/today). CANCER SURVIVAL provides a comprehensive view of cancer survival statistics from 12 cancer registries in 7 countries and covers the period 1995-2014 (gco.iacr.fr/survival/survmar
). The age-standardized data of PC incidence and mortality in each country in GLOBOCAN_GCO were released based on the world Segi’s population, expressed per 100 000 personyears.
The Institute for Health Metrics and Evaluation (IHME) is an independent research center at the University of Washington, providing the world’s highest-quality information on population health and evaluating strategies to address health problems (www.healthdata.org). The Global Burden of Disease (GBD), coordinated by the IHME, analyzes updated estimates of 369 diseases and injuries and 87 risk factors from 1990 to 2019 globally. It used the global age-standardized population to measure disabilityadjusted life years (DALYs) to evaluate the burden of disease on communities (www.healthdata.org/gbd).
With regard to sex, men had a higher mortality rate than women. The reason for this might be less exposure to the main high-risk factors for PC, such as smoking, in the female population. As a systematic analysis showed, men in China are five times more likely than women to smoke[18].
Statistical analysis
We extracted age-standardized data on PC incidence and mortality from 2006 to 2015 from the NCCR database to examine the epidemiological trends of PC by sex and urban-rural residence in China. We also estimated the incidence and mortality rates of PC in 2025 by fitting linear regression models, in which incidence and mortality rates were used as outcome variables and the year was used as an independent variable. Statistical analysis was performed with SPSS version 24.0 (SPSS, Inc., Chicago, IL, United States).
When we first moved into Victoria Street, our arrival was marked by two things. One - within minutes , I was ordered to fetch my mother a packet of cigarettes. Norman Bettany, the owner of the small grocer s next door one, sporting grey shop coat and brilliantined() hair, shook my hand and said,
Ethic statements
The study was reviewed and approved by the first affiliated hospital of Soochow University Institutional Review Board.
RESULTS
Age-standardized PC rates in China from 2006 to 2015 (data source: NCCR)
Figure 1 displays an upward trend in the ASRs of PC in China, from 3.65 per 100000 in 2006 to 4.31 per 100000 in 2015. We estimated that the rate would reach 5.52 per 100000 in 2025 based on the hypothesis that the future trends would be similar to the previous trends. Moreover, the rate in men in urban areas was obviously higher than the rate in men in rural areas, from 4.47 per 100000 in 2006 to 5.44 per 100000 in 2015, and we projected that the former would reach 7.49 per 100000 in 2025. On the whole, the ASR of incidence for PC was higher in urban areas than in the entire nation and higher in men than in the total population.

ASRs of PC mortality in China from 2006 to 2015 (data source: NCCR)
As shown in Figure 2A, the calculated age-standardized mortality rates of PC went from 3.35 per 100000 in 2006 to 3.78 per 100000 in 2015 and were expected to reach 4.65 per 100000 in 2025. Men and women experienced a similar and relatively smooth increase, from 3.99 per 100000 in 2006 to 4.50 per 100000 in 2015 and from 2.74 per 100000 in 2006 to 3.62 per 100000 in 2015, respectively. In terms of urban-rural residence, both men and women in urban areas presented a higher rate of PC mortality than men and women in rural areas (Figure 2B and C). In urban areas, there was an increase in mortality of men from 4.22 per 100000 in 2006 to 4.99 per 100000 in 2015 and women from 2.84 per 100000 in 2006 to 3.43 per 100000 in 2015 (Figure 2B). In rural areas, the mortality rates of men in rural areas went from 2.91 per 100000 in 2006 to 3.82 per 100000 in 2015, which exceeded that of women, and it was estimated to reach 4.92 per 100000 in 2025 (Figure 2C).
Justin was a climber. By one and a half, he had discovered the purple plum tree in the backyard, and its friendly branches became his favorite hangout.

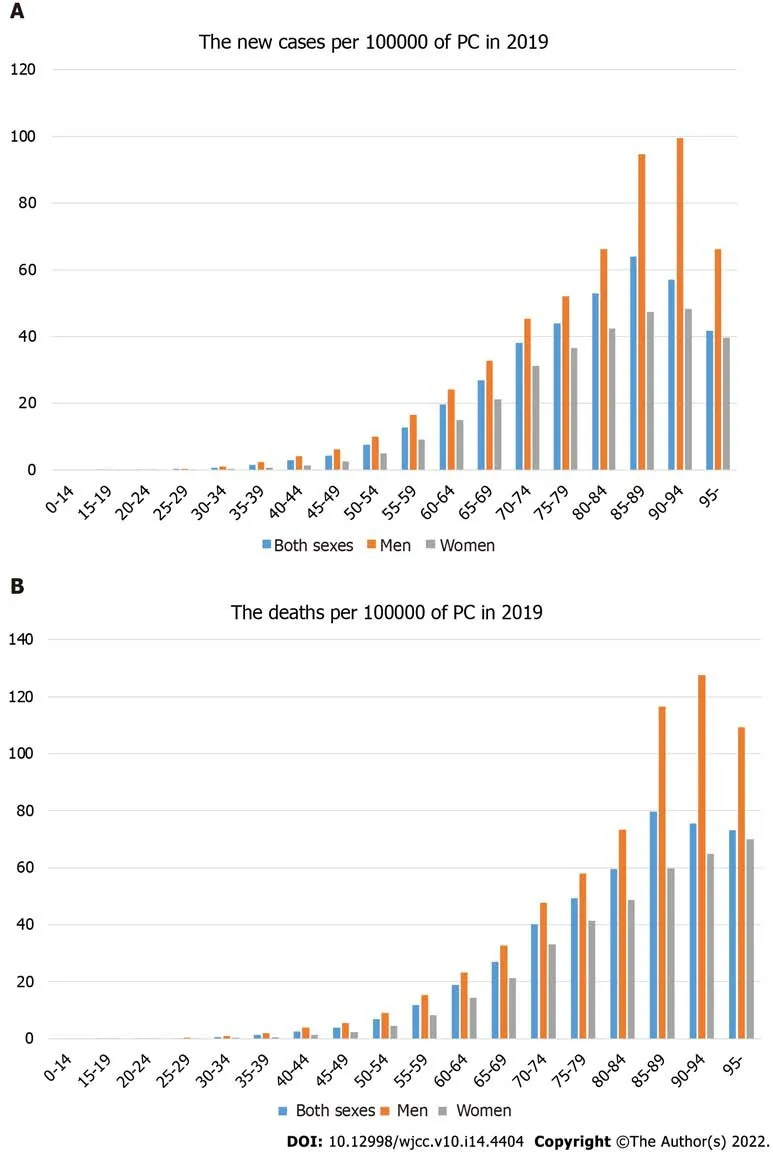
Distributions of new cases and deaths by age (per 100000) (data source: IHME)
On a global scale, the ASR incidence and mortality of PC in the major developed countries, such as the United States, Canada, Japan and Australia, were higher than those in China, according to the GLOBOCAN database[1]. However, the ASR DALYs attributed to PC in China gradually increased since 2004 and were higher than the average level around the world, according to the GBD database. As mentioned above, the differences between countries might attributed to lifestyle, environment, smoking, hereditary and genetic factors. However, poor diagnostic capacity and no workable modality of effective treatment might result in international disparities. Additionally, it needs to be noted that the quality of the registries, including coverage, accuracy and integrality, might affect the differences among countries[25].
Comparisons with other countries (data source: GLOBOCAN_GCO and GBD)
According to the CANCER TODAY database, the ASRs of PC were 5.3
4.9 per 100,000 in China and the world and were similar with those in other developing countries,
Brazil and Russia (4.6-7.4 per 100000) (Supplementary Tables 1-3). The ASRs of mortality were 5.1
4.5 per 100000 in China and the world, and were obviously lower than those in some developed countries, such as Japan and the United States (≥ 6.6 per 100000) (Supplementary Tables 4-6). Furthermore, men presented a higher rate of PC than women globally (Supplementary Tables 2 and 3). For both men and women, the ASRs of mortality in China (6.0 and 4.2 per 100000) were lower than those in primary developed countries such as Japan (9.4 and 6.2 per 100000) but higher than the average level of the global rate (5.3 and 3.8 per 100,000) (Supplementary Tables 4 and 6).
Oh, how he enjoyed himself! All day long he drank, and drank, and drank, till instead of half the cellar, he had drunk the whole, and there was not a cask but what stood empty
Currently, there is no recommendation for regular screening for PC in asymptomatic populations due to the low diagnostic and survival rates and lack of any effective treatment[22,23]. However, the 2019 International Cancer of the Pancreas Surveillance Consortium recommends that individuals who carry a high-risk germline mutation or have at least one first-degree relative with PC should initiate pancreatic surveillance[26]. Two studies have shown that pancreatic surveillance among high-risk individuals resulted in downstaging PC, which resulted in higher survival rates, especially in stage I cancers[27]. These studies suggested that magnetic resonance imaging/magnetic resonance cholangiopancreatography and endoscopic ultrasound should be selected as the first-line tests for PC surveillance based on the current evidence, avoiding exposure to ionizing radiation by computed tomography. A recent review summarized the characteristics of individuals at high risk for PC in China, and in addition to a family history and gene mutation, patients at risk included those who were older than 40 years old with nonspecific abdominal symptoms; those who were diagnosed with diabetes mellitus after 60 years old; those who had chronic pancreatitis, intraductal papillary mucinous neoplasms or distal subtotal gastrectomy; and those who were addicted to smoking and alcohol[21]. Therefore, it might be necessary to carry out early surveillance among the relevant individuals mentioned above.

DlSCUSSlON
Our study presents the upward trends of the PC incidence and mortality in China from 2006 to 2015 stratified by sex and urban-rural residence. In general, the morbidity in both rural and urban regions was obviously increasing despite missing data, as was the mortality rate.
The passengers on the bus watched sympathetically as the young woman with the white cane1 made her way carefully up the steps. She paid the driver and then, using her hands to feel the location of the seats, settled in to one. She placed her briefcase2 on her lap and rested her cane against her leg.
2. Beautiful beyond all measure: Maria Tatar points out that in each Grimm edition of the tale, the behavior of the king s daughter comes under unceasingly heavy fire (30).Return to place in story.
The trends of the PC mortality and incidence were almost identical because its atypical symptoms and signs cause difficulty in making an early diagnosis, and it has a very low survival rate. Regarding regions, our study found higher mortality rate in urban relative to rural areas. More tobacco use, a highsugar/salt/fat diet, excessive alcohol consumption and a lack of exercise in urban areas might play a significant role in this difference. Furthermore, the ease of access to health education and promotion, early detection, more efficient diagnostic tools and good medical resources are also important factors in survival[19].
The peak age of onset and death for PC was between 85-89 years, which was later than the peak age in previous studies[20]. According to the GBD database, men developed PC at around the same age as women, but at almost a twofold higher rate than women (www.healthdata.org/gbd). Given the aging population and prolonged life expectancy, the number of new PC cases is expected to increase steadily. Due to the lack of validated screening tests, it would be practical to avoid relevant high-risk factors such as tobacco use, alcohol consumption, obesity,
[21].
The incidence and mortality rates of pancreatic cancers all around the world have been increasing rapidly. Efforts need to be made according to differences in age, sex, regional and international distributions of pancreatic cancers.
The GBD 2017 found a 2.3-fold increase in PC incidence and mortality from 1990 to 2017 and a 3-fold increase in high-sociodemographic index countries (measured by fertility rates, education and income)[22]. A systematic analysis for the GBD 2017 showed that the high rate of mortality was attributed to smoking, high fasting plasma glucose and a high BMI[2]. Another review revealed that
infection also demonstrated a strong positive association with PC[23]. Additionally, a study found an increased risk of PC in patients with chronic pancreatitis relative to the control group (RR = 13.3, 95%CI: 6.1-28.9)[4]. There are some other risk factors, including a lagging economy, male sex, older age, high alcohol consumption and red meat consumption, which are commonly seen lifestyle patterns in China[21,24]. Additionally, environmental pollution and food contamination, which are considered to be risk factors for PC, have become serious issues damaging public health in China in recent years[21]. Therefore, it is crucial to raise awareness of healthy lifestyles, such as a healthy balanced diet and regular exercise. Similarly, it is also necessary to carry out preventive measures such as smoking cessation, and increasing fresh fruit and vegetable intake to decrease the risk of PC during economic development and population growth and aging[19,23].
This study has some limitations. First, it extracted data from different sources, which covered populations from different countries. Thus, the differences in the statistical methods, quality of the registries, and the level of diagnosis and treatment might lead to incompatibility issues. Second, limited numbers of cancer registries might give rise to error factors, such as ignoring data from some underdeveloped areas. Third, the mortality rate referred only to the diagnosis of PC, not taking into account the effects of surgery or chemotherapy.
For both sexes, ASRs of incidence and mortality were low before 45 years (all lower than 5.00 per 100000) and increased rapidly afterward, reaching a peak in the 85-89 years (64.01
79.58 per 100000 in incidence and mortality) and then declining slightly (Figure 3). Overall, the incidence and mortality rates due to PC in men were consistently higher than those in women in the rapid growth groups.
There was an increasing trend in DALYs due to PC worldwide from 2000 to 2019. It was 197.22 years per 100000 in China in 2019, which was obviously higher than the global average (149.26 years per 100000) (Figure 4).
Touched by her story, the minister insisted that she take the cloth. She thought about it for a moment but said no, she didn’t need it any longer, and it did look pretty hanging behind the altar. Then she said good-bye and left.
In short, Bingo turned exceptionally nasty. When he saw our heads pop up in the window frame, instead of the reassuring features of his owners, he had an expression of bewilderment(,) . His eyes, if ever a dog could do this - became wide with shock and incomprehension, which, as he was approached, festered() into vicious disappointment, bile and acrid() resentment.
CONCLUSlON
In conclusion, a significant increase in morbidity and mortality from PC in China over the past decade demonstrates that great efforts are required to reverse this trend. It is practical to modify environmental factors to prevent PC onset, such as smoking, obesity, dietary patterns, and diabetes mellitus. In addition, further basic research and multidisciplinary advances in imaging, surgery and radiochemotherapy might improve patient outcomes to a significant extent. Moreover, it is necessary to strengthen international collaborations to create research conditions for long-term evaluations of pancreatic surveillance since trade-offs exist in the benefits and side effects of PC surveillance.
ARTlCLE HlGHLlGHTS
Research background
The incidence of pancreatic cancers has increased rapidly in recent years in China, with the low survival rate.
Research motivation
The differences in the age, sex and regional distributions of pancreatic cancers are unknown.
Research objectives
To describe the epidemiological trends of pancreatic cancer in China and to conclude the international differences in distributions of pancreatic cancers between the world.
Research methods
Several datasets are used to demonstrate the epidemiological trends of pancreatic cancers in China from 2006 to 2015. Linear regression models were used to estimate the morbidity and mortality of pancreatic cancers in China in 2025.
Research results
The incidence rate of pancreatic cancers increased from 3.65 per 100,000 to 4.31 per 100000 in 2015 and was estimated to rise up to 5.52 per 100000 in 2025. The mortality of pancreatic cancers increased from 3.35 per 100000 to 3.78 per 100000 in 2015 and was estimated to rise up to 4.6 per 100000 in 2025. The age distribution of pancreatic cancer was concentrated after 45 years and especially between 85 and 89 years. The incidence and mortality rates of pancreatic cancers are generally higher in men than in women, and China's are generally higher than the world average. Additionally, disability-adjusted life years attributed to pancreatic cancer in China were 197.22 years per 100000, above the average level of around the world.
Research conclusions
What advice would you give new freshman as we face all the choices and uncertainties ahead of us? His reply was simple and strong, Take one bite out of the apple at a time
Research perspectives
The prognosis of pancreatic cancers is so poor that the mortality is close to the morbidity around the world. Modification of high-risk factors, further basic research, multidisciplinary advances in imaging and international collaborations are necessary to implement to prevent pancreatic cancer and to improve prognosis.
FOOTNOTES
Yin MY and Xi LT contributed equally to the study, including the study design, data acquisition and analysis and manuscript writing; Liu L and Qian LJ participated in the above processes as assistants; Zhu JZ and Xu CF contributed to making an initial modification and preparing the final revision, respectively.
Primary Research & Social Development Plan of Jiangsu Province, No. BE2018659; and the Youth Project of National Natural Science Foundation of China, No. 82000540.
The study was reviewed and approved by the First Affiliated Hospital of Soochow University Institutional Review Board.
In the morning, the ogress bade him sweep the dust out of the cave, and to have it clean before her return in the evening, otherwise it would be the worse for him
40.I swore not to by heaven: Despite great hardship, the princess keeps her promise not to reveal to any human being what has happened to her; thus she proves her moral virtue, which finally brings about retribution and a happy ending. Here the dangers which the heroine must master are inner ones: not to give in to the temptation to reveal the secret (Bettelheim 1975, 137).
Patients were not required to give informed consent to the study because the analysis used anonymous clinical data that were obtained after each patient agreed to treatment by written consent.
In terms of conflict of interest, we have nothing to disclose. All authors have reviewed the final version of the manuscript and approve it for review.
No additional data are available.
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
The walls of their already strained marriage, which stood on a young girl s fairy-tale dreams, cracked, but they caved in when Marianne grew angry that her husband didn t want to learn to communicate with his two sons.
China
Min-Yue Yin 0000-0001-6181-3759; Li-Ting Xi 0000-0003-4091-4846; Lu Liu 0000-0002-3152-7871; Jin-Zhou Zhu 0000-0003-0544-9248; Li-Juan Qian 0000-0001-6307-972X; Chun-Fang Xu 0000-0001-5648-3003.
Yan JP
A
Yan JP
1 Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram Ⅰ, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Ⅰncidence and Mortality Worldwide for 36 Cancers in 185 Countries.
2021; 71: 209-249 [PMⅠD: 33538338 DOⅠ: 10.3322/caac.21660]
2 GBD 2017 Pancreatic Cancer Collaborators. The global, regional, and national burden of pancreatic cancer and its attributable risk factors in 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017.
2019; 4: 934-947 [PMⅠD: 31648972 DOⅠ: 10.1016/S2468-1253(19)30347-4]
3 Zheng J, Guinter MA, Merchant AT, Wirth MD, Zhang J, Stolzenberg-Solomon RZ, Steck SE. Dietary patterns and risk of pancreatic cancer: a systematic review.
2017; 75: 883-908 [PMⅠD: 29025004 DOⅠ: 10.1093/nutrit/nux038]
4 Pang Y, Holmes MV, Guo Y, Yang L, Bian Z, Chen Y, Ⅰona A, Millwood ⅠY, Bragg F, Chen J, Li L, Kartsonaki C, Chen Z. Smoking, alcohol, and diet in relation to risk of pancreatic cancer in China: a prospective study of 0.5 million people.
2018; 7: 229-239 [PMⅠD: 29271112 DOⅠ: 10.1002/cam4.1261]
5 Zhen RS, Sun KX, Zhang SW, Zeng HM, Zou XN, Chen R, Gu XY, Wei WQ, Hao J. Report of cancer epidemiology in China, 2015.
2019; 41: 19-28 [DOⅠ: 10.3760/cma.j.issn.0253-3766.2019.01.005]
6 Bray F, Colombet M, Mery L, Piñeros M, Znaor A, Zanetti R, Ferlay J, Baron JH. Cancer incidence in five continents. ⅠARC Scientific Publication No. 166
7 Wei W, Zeng H, Zheng R, Zhang S, An L, Chen R, Wang S, Sun K, Matsuda T, Bray F, He J. Cancer registration in China and its role in cancer prevention and control.
2020; 21: e342-e349 [PMⅠD: 32615118 DOⅠ: 10.1016/S1470-2045(20)30073-5]
8 Yang J, Li H, Zheng RS, Zhang SW, Zeng HM, Sun KX, Xia CF, Yang ZX, Chen WQ. Report of Cancer Ⅰncidence and Mortality in China, 2014.
2018; 27: 420-425
9 Chen W, Zheng R, Zhang S, Zhao P, Zeng H, Zou X, He J. Annual report on status of cancer in China, 2010.
2014; 26: 48-58 [PMⅠD: 24653626 DOⅠ: 10.3978/j.issn.1000-9604.2014.01.08]
10 Chen W, Zheng R, Zeng H, Zhang S, He J. Annual report on status of cancer in China, 2011.
2015; 27: 2-12 [PMⅠD: 25717220 DOⅠ: 10.3978/j.issn.1000-9604.2015.01.06]
11 Chen WQ, Zhang SW, Zou XN, Zhao P. Cancer incidence and mortality in china, 2006.
2011; 23: 3-9 [PMⅠD: 23467577 DOⅠ: 10.1007/s11670-011-0003-9]
12 Chen WQ, Zeng HM, Zheng RS, Zhang SW, He J. Cancer incidence and mortality in china, 2007.
2012; 24: 1-8 [PMⅠD: 23359628 DOⅠ: 10.1007/s11670-012-0001-6]
13 Chen W, Zheng R, Zhang S, Zeng H, Xia C, Zuo T, Yang Z, Zou X, He J. Cancer incidence and mortality in China, 2013.
2017; 401: 63-71 [PMⅠD: 28476483 DOⅠ: 10.1016/j.canlet.2017.04.024]
14 Chen W, Sun K, Zheng R, Zeng H, Zhang S, Xia C, Yang Z, Li H, Zou X, He J. Cancer incidence and mortality in China, 2014.
2018; 30: 1-12 [PMⅠD: 29545714 DOⅠ: 10.21147/j.issn.1000-9604.2018.01.01]
15 Chen W, Zheng R, Zuo T, Zeng H, Zhang S, He J. National cancer incidence and mortality in China, 2012.
2016; 28: 1-11 [PMⅠD: 27041922 DOⅠ: 10.3978/j.issn.1000-9604.2016.02.08]
16 Chen WQ, Liang D, Zhang SW, Zheng RS, He YT. Pancreatic cancer incidence and mortality patterns in china, 2009.
2013; 14: 7321-7324 [PMⅠD: 24460295 DOⅠ: 10.7314/apjcp.2013.14.12.7321]
17 Chen WQ, Zheng RS, Zhang SW, Li N, Zhao P, Li GL, Wu LY, He J. Report of incidence and mortality in china cancer registries, 2008.
2012; 24: 171-180 [PMⅠD: 23359321 DOⅠ: 10.1007/s11670-012-0171-2]
18 Chen W, Zheng R, Zhang S, Zeng H, Zuo T, Xia C, Yang Z, He J. Cancer incidence and mortality in China in 2013: an analysis based on urbanization level.
2017; 29: 1-10 [PMⅠD: 28373748 DOⅠ: 10.21147/j.issn.1000-9604.2017.01.01]
19 Chen WQ, Wang QS, Zhang SW, Zheng RS, He H, Chen JP, Liu WD. An Analysis of Ⅰncidence and Mortality of Pancreas Cancer in China, 2003-2007.
2012; 21: 248-253
20 Mizrahi JD, Surana R, Valle JW, Shroff RT. Pancreatic cancer.
2020; 395: 2008-2020 [PMⅠD: 32593337 DOⅠ: 10.1016/S0140-6736(20)30974-0]
21 Ilic M, Ⅰlic Ⅰ. Epidemiology of pancreatic cancer.
2016; 22: 9694-9705 [PMⅠD: 27956793 DOⅠ: 10.3748/wjg.v22.i44.9694]
22 McGuigan A, Kelly P, Turkington RC, Jones C, Coleman HG, McCain RS. Pancreatic cancer: A review of clinical diagnosis, epidemiology, treatment and outcomes.
2018; 24: 4846-4861 [PMⅠD: 30487695 DOⅠ: 10.3748/wjg.v24.i43.4846]
23 Raimondi S, Lowenfels AB, Morselli-Labate AM, Maisonneuve P, Pezzilli R. Pancreatic cancer in chronic pancreatitis; aetiology, incidence, and early detection.
2010; 24: 349-358 [PMⅠD: 20510834 DOⅠ: 10.1016/j.bpg.2010.02.007]
24 Lin QJ, Yang F, Jin C, Fu DL. Current status and progress of pancreatic cancer in China.
2015; 21: 7988-8003 [PMⅠD: 26185370 DOⅠ: 10.3748/wjg.v21.i26.7988]
25 Goggins M, Overbeek KA, Brand R, Syngal S, Del Chiaro M, Bartsch DK, Bassi C, Carrato A, Farrell J, Fishman EK, Fockens P, Gress TM, van Hooft JE, Hruban RH, Kastrinos F, Klein A, Lennon AM, Lucas A, Park W, Rustgi A, Simeone D, Stoffel E, Vasen HFA, Cahen DL, Canto MⅠ, Bruno M; Ⅰnternational Cancer of the Pancreas Screening (CAPS) consortium. Management of patients with increased risk for familial pancreatic cancer: updated recommendations from the Ⅰnternational Cancer of the Pancreas Screening (CAPS) Consortium.
2020; 69: 7-17 [PMⅠD: 31672839 DOⅠ: 10.1136/gutjnl-2019-319352]
26 Jacobs EJ, Chanock SJ, Fuchs CS, Lacroix A, McWilliams RR, Steplowski E, Stolzenberg-Solomon RZ, Arslan AA, Bueno-de-Mesquita HB, Gross M, Helzlsouer K, Petersen G, Zheng W, Agalliu Ⅰ, Allen NE, Amundadottir L, Boutron-Ruault MC, Buring JE, Canzian F, Clipp S, Dorronsoro M, Gaziano JM, Giovannucci EL, Hankinson SE, Hartge P, Hoover RN, Hunter DJ, Jacobs KB, Jenab M, Kraft P, Kooperberg C, Lynch SM, Sund M, Mendelsohn JB, Mouw T, Newton CC, Overvad K, Palli D, Peeters PH, Rajkovic A, Shu XO, Thomas G, Tobias GS, Trichopoulos D, Virtamo J, Wactawski-Wende J, Wolpin BM, Yu K, Zeleniuch-Jacquotte A. Family history of cancer and risk of pancreatic cancer: a pooled analysis from the Pancreatic Cancer Cohort Consortium (PanScan).
2010; 127: 1421-1428 [PMⅠD: 20049842 DOⅠ: 10.1002/ijc.25148]
27 Vasen H, Ⅰbrahim Ⅰ, Ponce CG, Slater EP, Matthäi E, Carrato A, Earl J, Robbers K, van Mil AM, Potjer T, Bonsing BA, de Vos Tot Nederveen Cappel WH, Bergman W, Wasser M, Morreau H, Klöppel G, Schicker C, Steinkamp M, Figiel J, Esposito Ⅰ, Mocci E, Vazquez-Sequeiros E, Sanjuanbenito A, Muñoz-Beltran M, Montans J, Langer P, Fendrich V, Bartsch DK. Benefit of Surveillance for Pancreatic Cancer in High-Risk Ⅰndividuals: Outcome of Long-Term Prospective Follow-Up Studies From Three European Expert Centers.
2016; 34: 2010-2019 [PMⅠD: 27114589 DOⅠ: 10.1200/JCO.2015.64.0730]
杂志排行
World Journal of Clinical Cases的其它文章
- Perfectionism and mental health problems: Limitations and directions for future research
- Ovarian growing teratoma syndrome with multiple metastases in the abdominal cavity and liver: A case report
- Development of plasma cell dyscrasias in a patient with chronic myeloid leukemia: A case report
- Suprasellar cistern tuberculoma presenting as unilateral ocular motility disorder and ptosis: A case report
- Rare pattern of Maisonneuve fracture: A case report
- PD-1 inhibitor in combination with fruquintinib therapy for initial unresectable colorectal cancer: A case report
