Acute coronary syndrome on non-electrocardiogram-gated contrastenhanced computed tomography
2022-06-01ShuYoshihara
INTRODUCTION
Acute coronary syndrome(ACS)is a term used to refer to a range of conditions associated with acute myocardial ischemia and/or infarction,which are usually due to an abrupt reduction in the coronary blood flow[1].Chest pain characteristics,specific associated symptoms,electrocardiogram(ECG)abnormalities,and the levels of serum biomarkers of myocardial necrosis are essential for a diagnosis of ACS[1].However,rather than chest pain,some ACS patients present with atypical symptoms[2-4].A review of over 430,000 patients from the National Registry of Myocardial Infarction II with confirmed acute myocardial infarction(AMI)showed that one-third presented at the hospital with no chest pain[2].Patients such as these often present with symptoms including dyspnea alone,weakness,nausea and/or vomiting,palpitations,syncope,or cardiac arrest.The implications of absence of chest pain are important in terms of therapy and prognosis.The Registry report revealed that patients without chest pain were less likely to receive a diagnosis of a confirmed MI on admission,and were also less likely to receive thrombolytic therapy or primary percutaneous coronary intervention,and to undergo treatment with appropriate medical therapy.It is unsurprising that these differences were associated with increased in-hospital mortality[2].Therefore,it is sometimes difficult to achieve a definitive diagnosis of ACS,especially for patients who present with atypical symptoms,normal initial biomarkers of myocardial necrosis,and normal or nondiagnostic ECGs.Even in the presence of acute coronary ischemia,women,diabetics,and the elderly are more likely to present with atypical symptoms,and caution is required in evaluating possible ACS[2,3].The use of computed tomography(CT)in the emergency department(ED)has increased at a consistent exponential rate[5].Due to their greater temporal and spatial resolution,current multi-slice computed tomography(MSCT)systems are capable of rapid scanning that renders non-ECG-gated images with fewer cardiac motion artifacts.Although imaging of various cardiac diseases is superior with ECG-gated MSCT images,typically there is sufficient information provided in non-ECG-gated MSCT images of the thorax or abdomen to identify a number of incidental cardiac abnormalities like myocardial perfusion defect(MPD)of the left ventricle which may be related to the patient’s presenting symptoms[6].Consequently,clinically unrecognized ACS cases identified on CT performed for the indication of other diseases are increasing,especially in the ED.In this article,we present clinically unrecognized several ACS cases detected on routine non-ECG-gated contrast-enhanced CT performed in the ED for discriminating other pathologies.Non-ECGgated contrast-enhanced CT was performed using an 80-row MSCT scanner(Aquilion Prime,Toshiba Medical Systems,Tochigi,Japan).The scanning parameters were as follows:tube voltage,120 kV;tube current,mA modulation technique with a noise index of 12(maximum 500 mA);gantry rotation time,350 ms;reconstruction slice thickness,1mm.An intravenous bolus of nonionic contrast medium(55 kg < body weight;iopamidol 300 mg iodine/mL,55 kg ≥ body weight;iopamidol 370 mg iodine/ml)was delivered through a vein in the arm with a flow rate of 3.3 mL/s.The dose of contrast medium was appropriately 600 mg I/kg of body weight,to a maximum of 100 mL.The scanning delay was calculated by monitoring the contrast values that increased to 150 Hounsfield units in the descending aorta as the region of interest(25-30 s after injection).A second scan was performed 120 s after injection.When focal decrease of the left ventricular myocardial enhancement was visually found,a region of interest was manually set to measure CT attenuation values of the normal and hypoperfused myocardium.MPD was defined as a decrease of 20 or more Hounsfield units compared with the adjacent normal enhanced myocardium.
Of all the precious wives in the whole wide world, how did Mark get so lucky to marry the best one? He married you, Michelle, and he is so lucky! I am so proud of you, my little girl.
CARDIAC COMPUTED TOMOGRAPHY AND ACS
Progress in the technical development of cardiac CT enables rapid,accurate imaging of the cardiovascular system.With cardiac CT,it is necessary to use either prospective or retrospective ECG gating to synchronize the CT image with the ECG.In both methods,the waveform of the ECG is used to coordinate image reconstruction with the heart’s position in the chest[7].Recently,a large body of evidence has been published supporting early assessment of coronary artery stenosis by cardiac CT as an accurate,safe,and efficient rapid diagnostic strategy for ED patients with low-intermediate risk acute chest pain[8-11].As a result,the appropriate use criteria for cardiac CT designated detection of coronary artery stenosis by cardiac CT as appropriate for use in acute chest pain patients for whom the likelihood of ACS is low or intermediate[12].Moreover,identification of regional subendocardial or transmural hypoattenuation of the myocardium in cardiac CT provides incremental diagnostic value to detect ACS[13].Based on this novel evidence,the updated SCCT guidelines for the interpretation and reporting of coronary CT angiography have newly designated that myocardial CT enhancement patterns should be assessed during performance of cardiac CT[14].
NON-ELECTROCARDIOGRAM-GATED CONTRAST-ENHANCED CT AND ACS
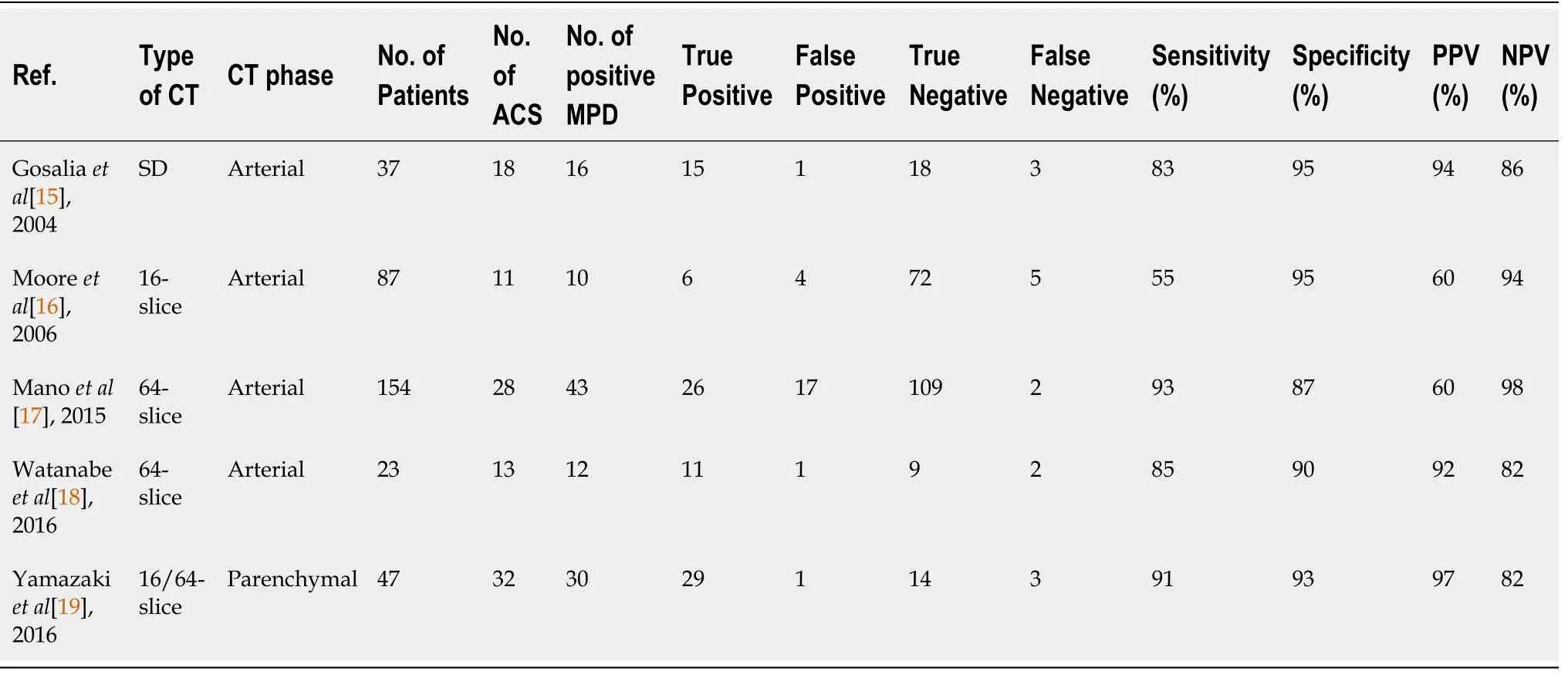
Recently,several reports have been published that suggest non-ECG-gated contrast-enhanced CT can detect ACS with high diagnostic accuracy(Table 1)[15-19].Mano
[17]evaluated the frequency of MPD on non-ECG-gated contrast-enhanced CT performed with a 64-slice CT scanner,which was done to assess aortic dissection or pulmonary embolism in 154 patients who had been admitted to the ED with acute chest pain and/or back pain.MPD was detected in 43 patients,26(60%)of whom were ultimately diagnosed with AMI.In the remaining 111 patients without MPD,only 2(2%)were ultimately diagnosed with AMI.They showed good diagnostic performance for MPD on non-ECGgated contrast-enhanced CT in predicting AMI with a sensitivity of 93% and a specificity of 87%.Watanabe
[18]evaluated the presence of MPD on non-ECG-gated contrast-enhanced CT using a 64-slice CT scanner in 23 patients who had been admitted to the ED with acute-onset chest pain and underwent emergent invasive coronary angiography.Of the 23 patients,13 were diagnosed with ACS and the remaining 10 were diagnosed with other conditions.MPD was detected in 11(85%)of the 13 ACS patients.They showed good diagnostic performance for MPD on non-ECG-gated contrastenhanced CT in predicting ACS with a sensitivity of 85% and a specificity of 90%.In comparison with the other studies using non-ECG-gated contrast-enhanced arterial phase CT imaging for detecting ACS,Yamazaki
[19]evaluated the ACS detection capability of using non-ECG-gated contrast-enhanced parenchymal phase CT imaging acquired with a 100-s scan delay.They showed good diagnostic performance for MPD visualized on non-ECG-gated contrast-enhanced CT during the parenchymal phase in predicting ACS with a sensitivity of 91% and a specificity of 93%.In non-ECG-gated contrastenhanced CT,the normal myocardium is usually blurry because reconstructed images are a mixture of the systolic and diastolic phases.Indeed,cardiac motion artifacts are recognized to be the most important factor to degrade diagnostic performance on non-ECG-gated contrast-enhanced CT[19].However,the frequency of false positive cases who were misjudged to have MPD without myocardial ischemia mainly due to cardiac motion artifacts was only 15%-20% in the previous reports[17,18].In cases with ACS,decreased regional myocardial wall motion due to acute myocardial ischemia will contribute to reduced motion artifacts and sharp visualization of the myocardial border.
IMPORTANT POINTS OF IMAGE INTERPRETATION IN DETECTING ACS ON NONELECTROCARDIOGRAM-GATED CONTRAST-ENHANCED CT
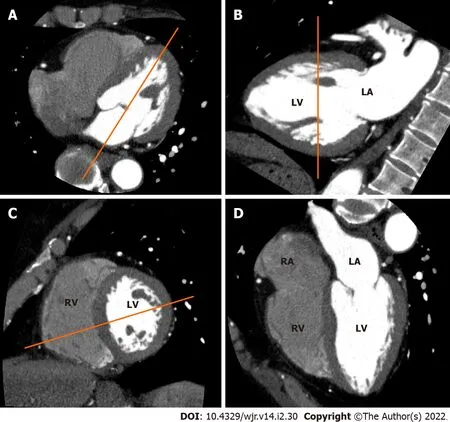
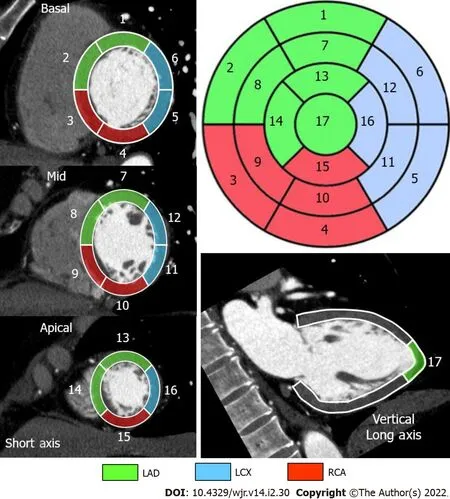
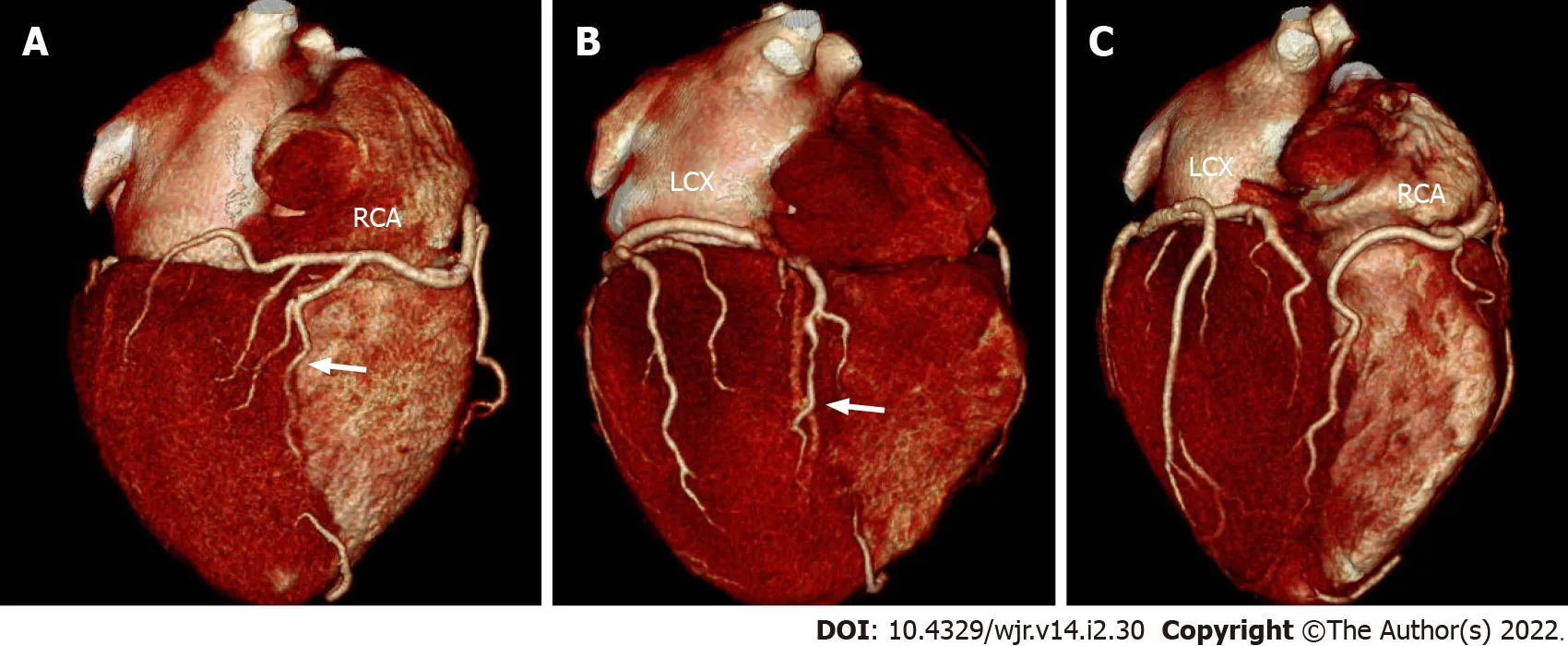
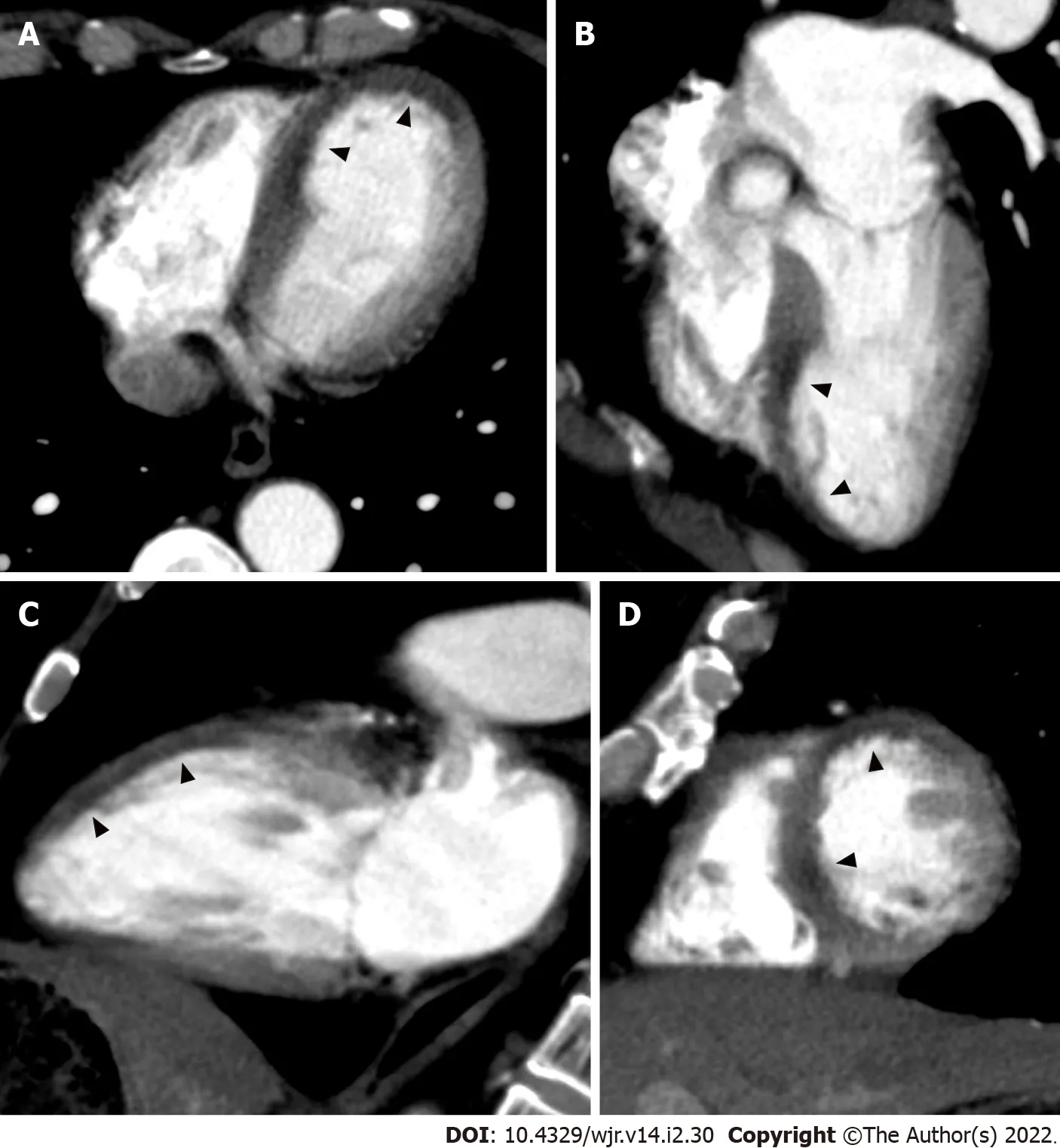
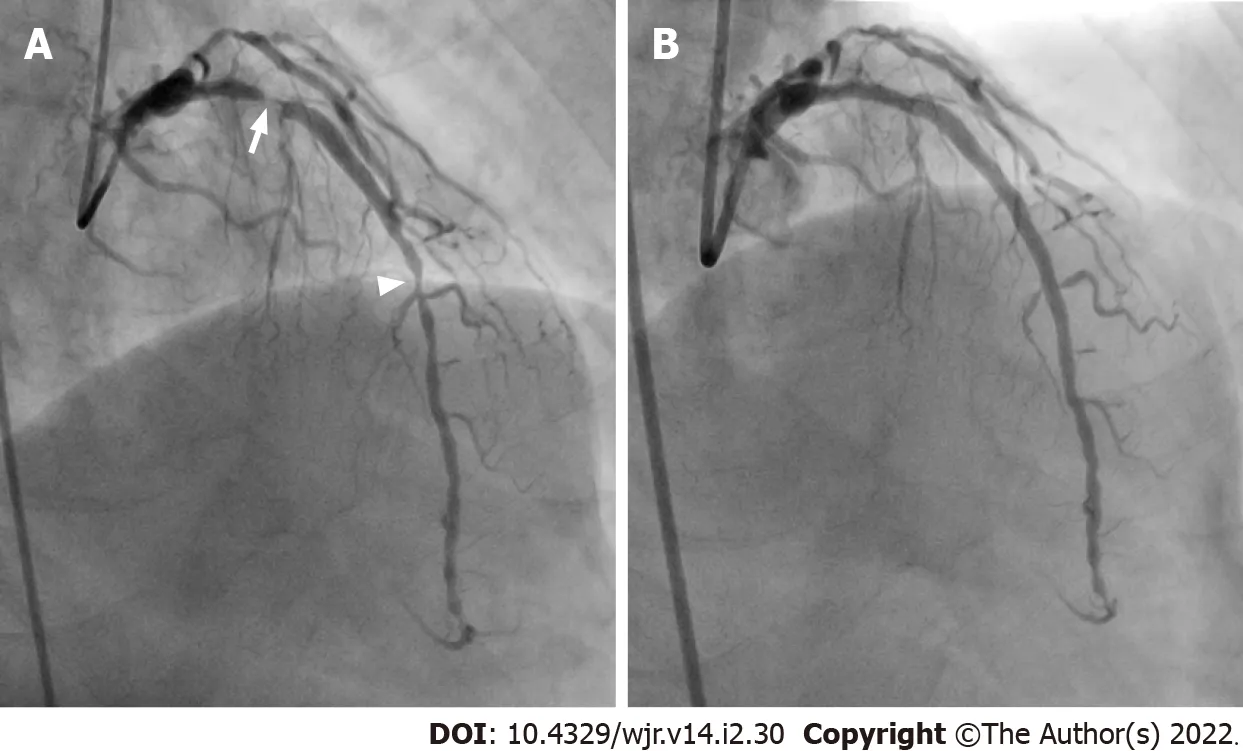
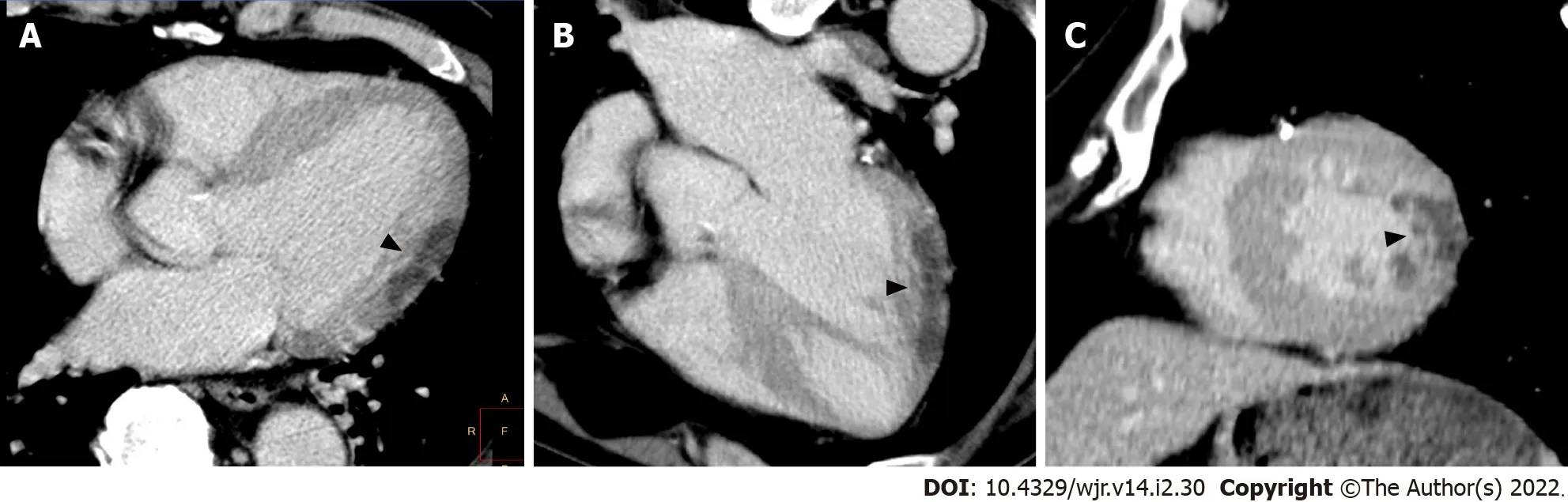
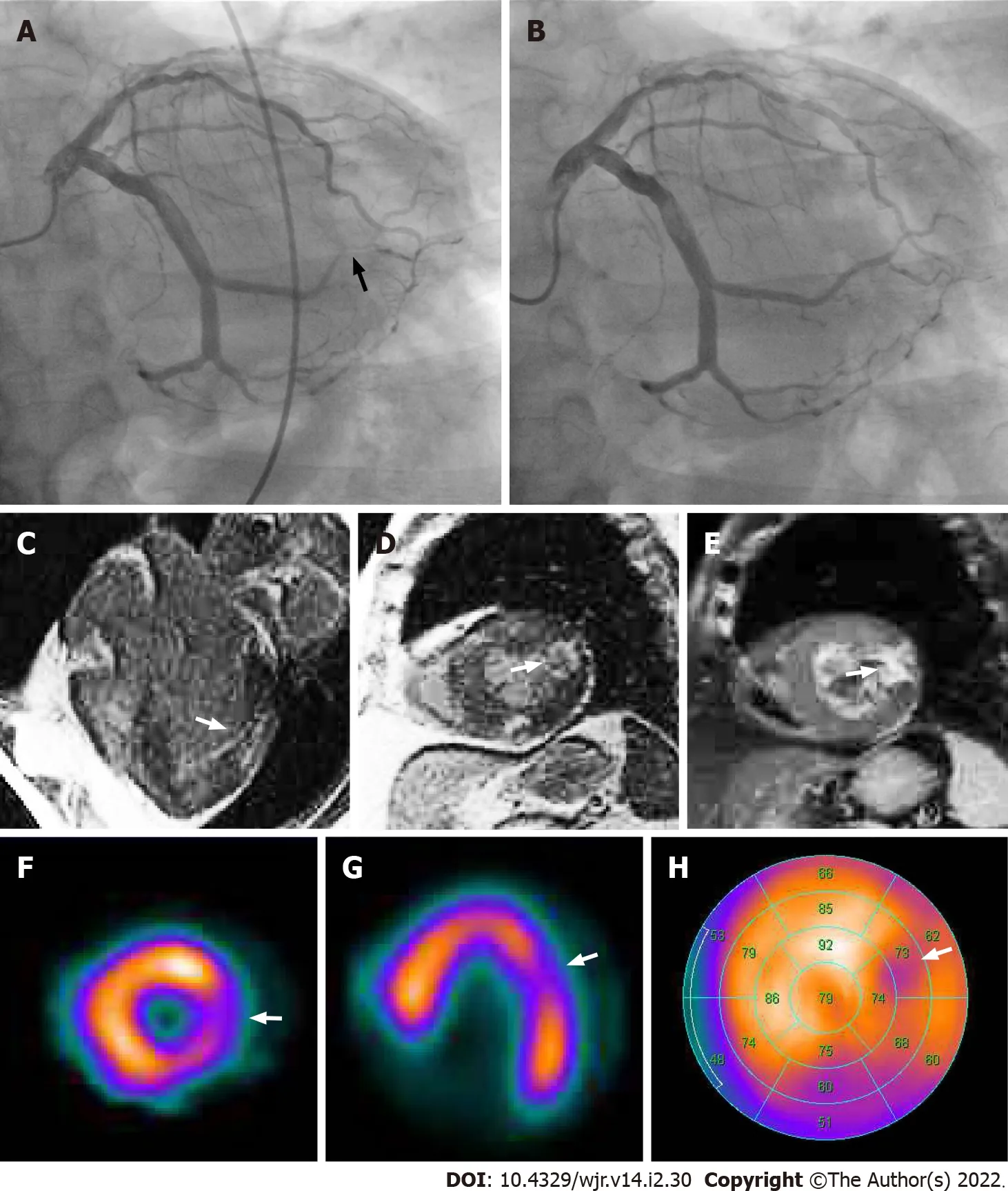
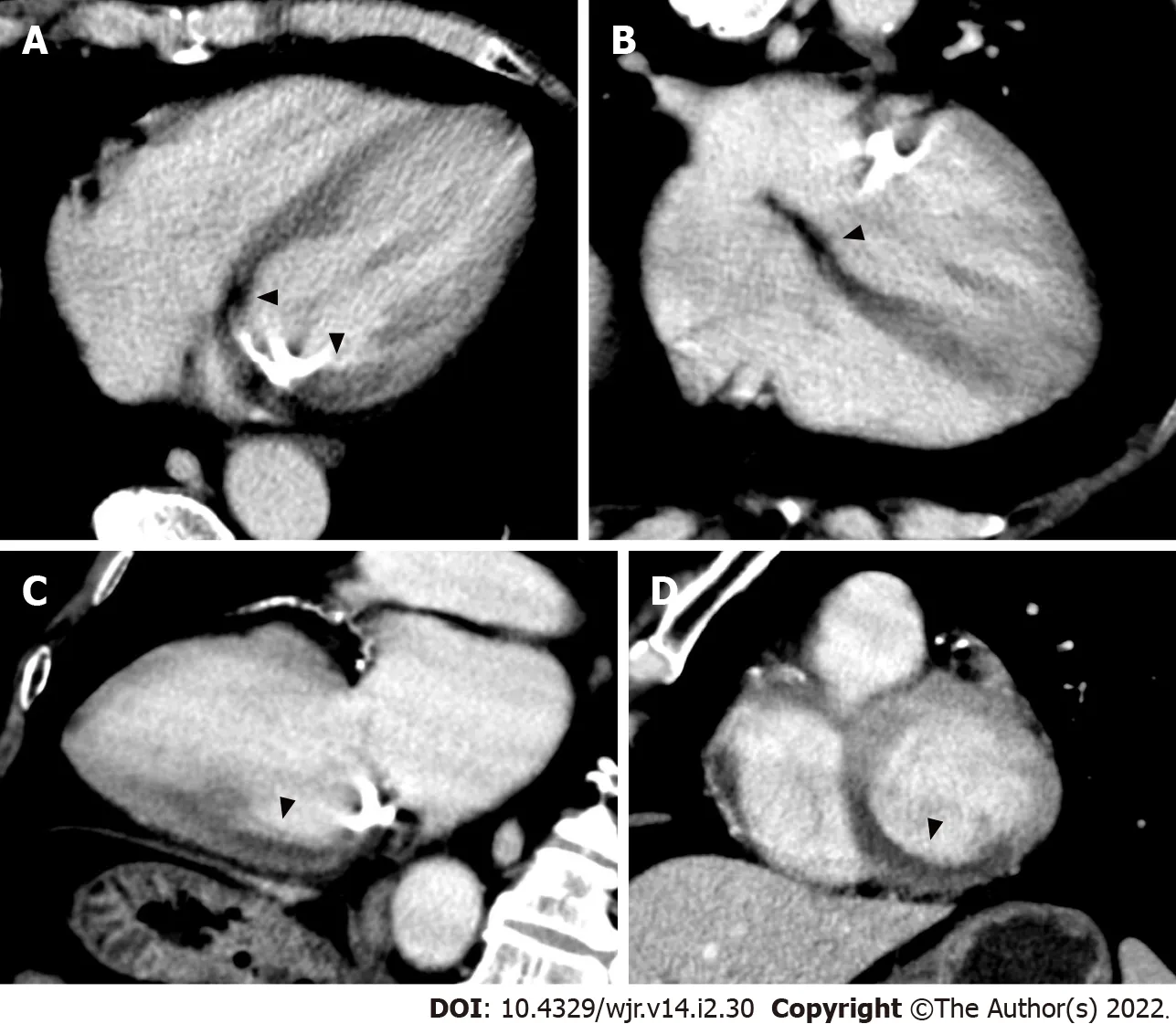
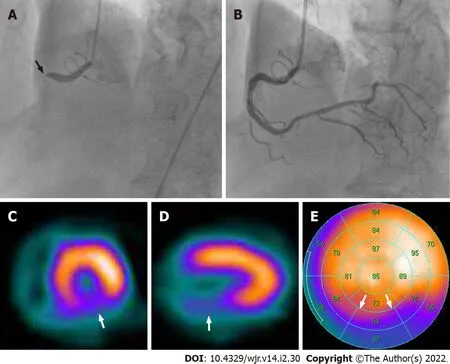
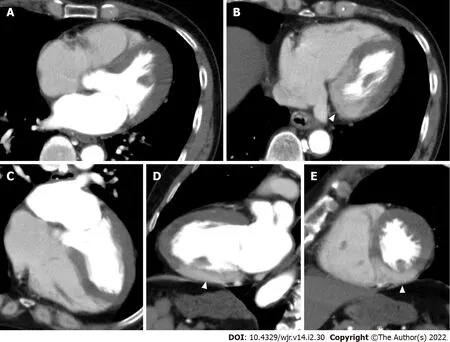
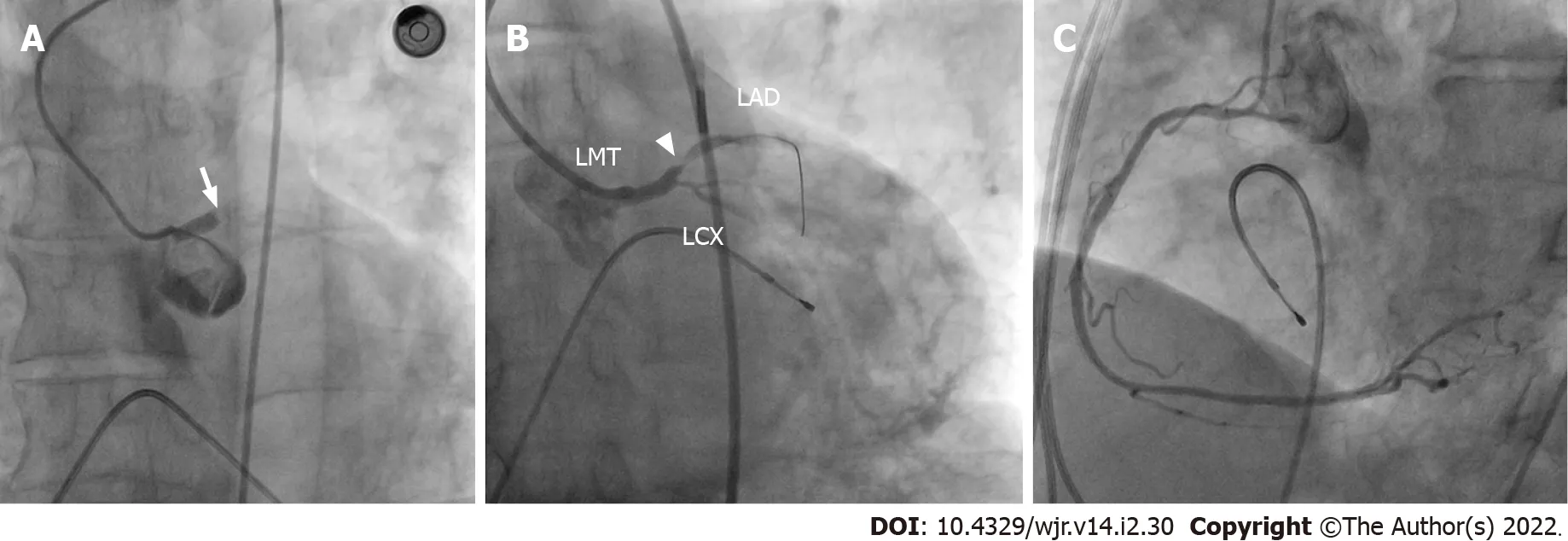
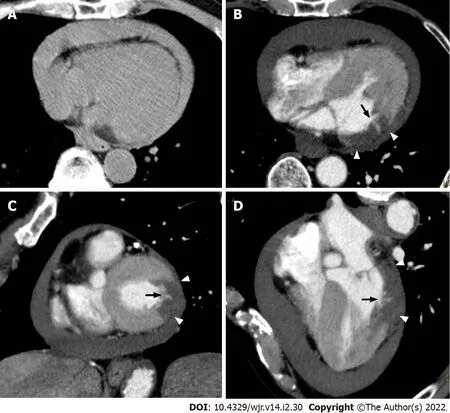
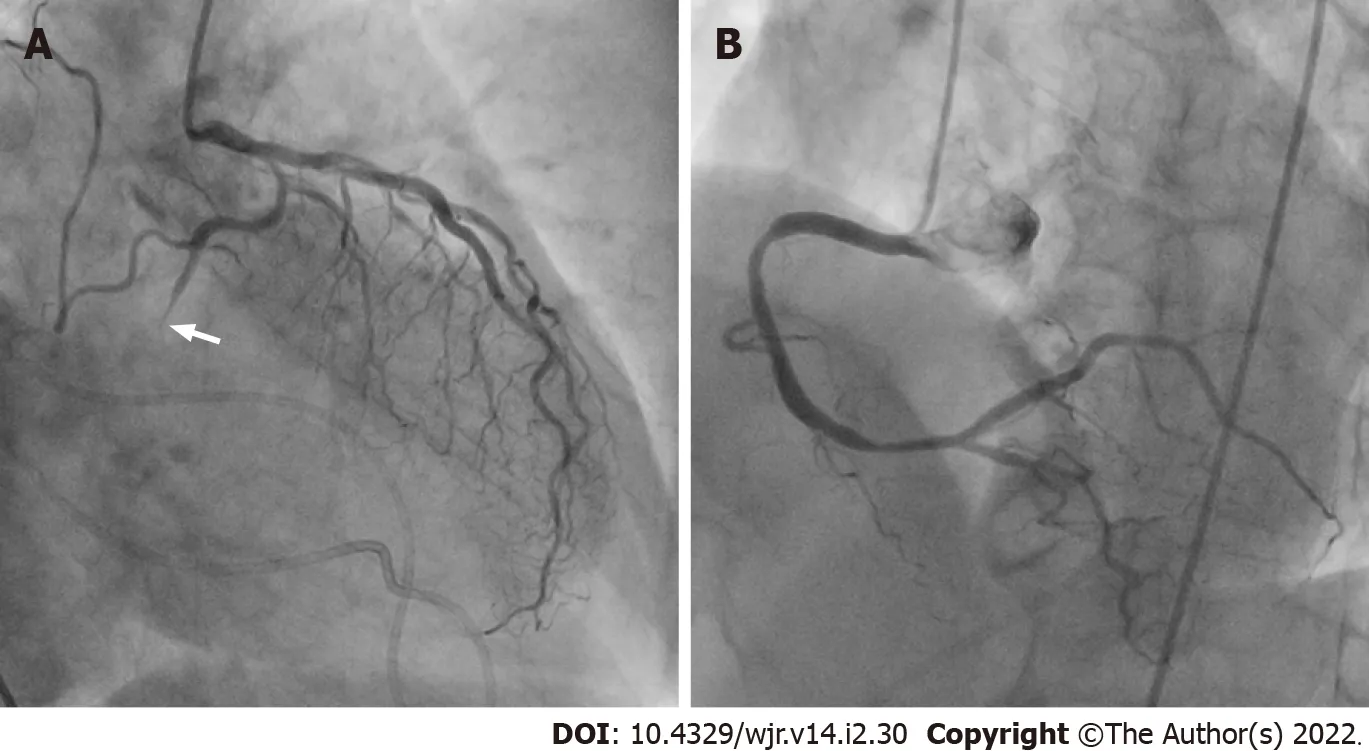
Vascular territories of the coronary artery
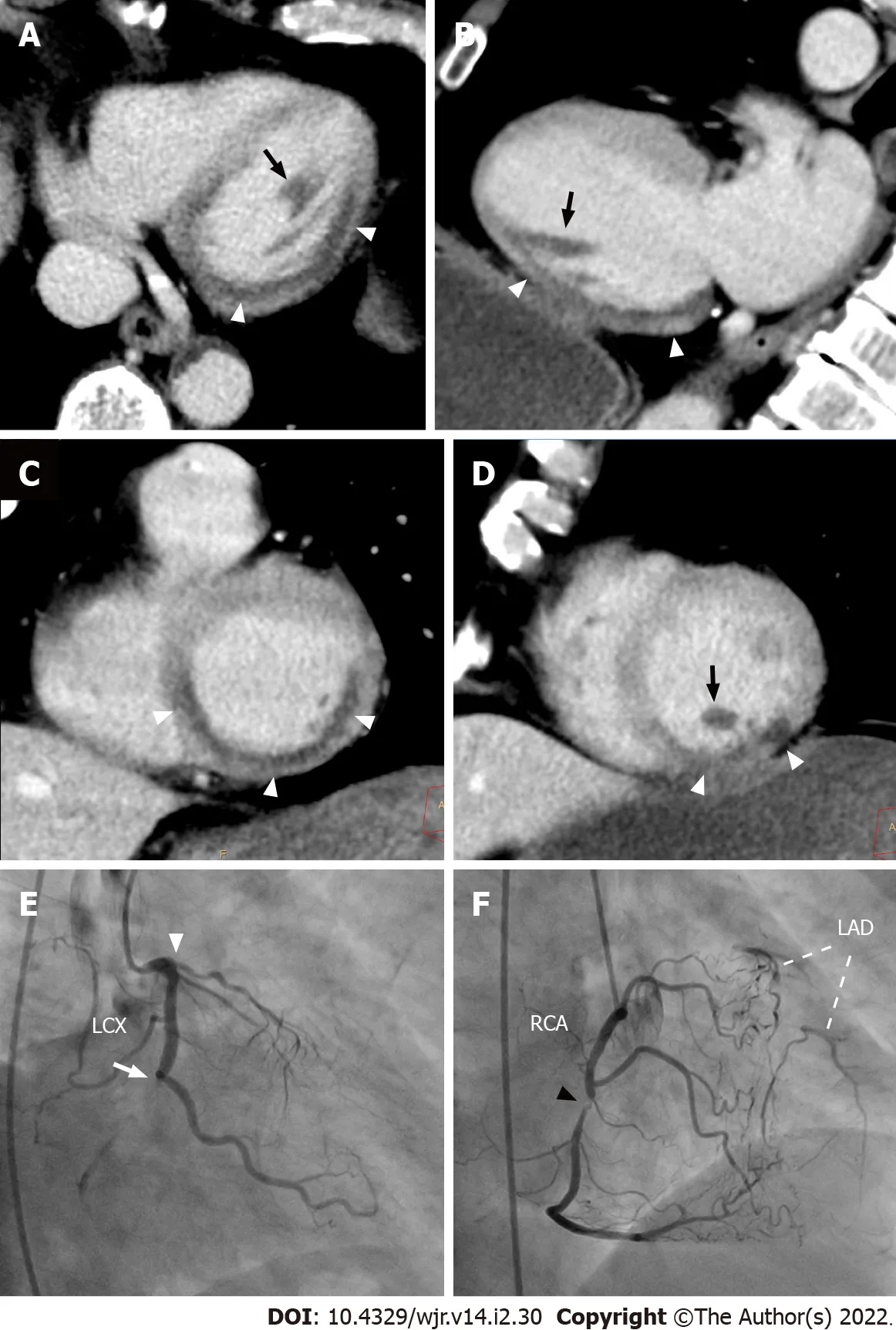
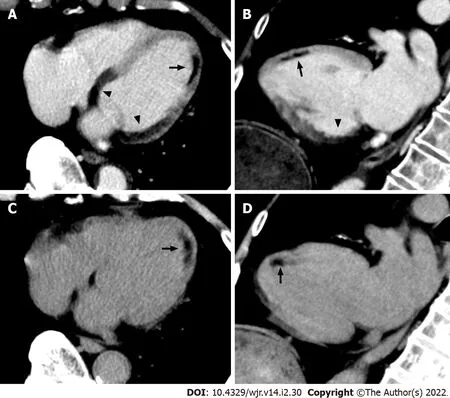
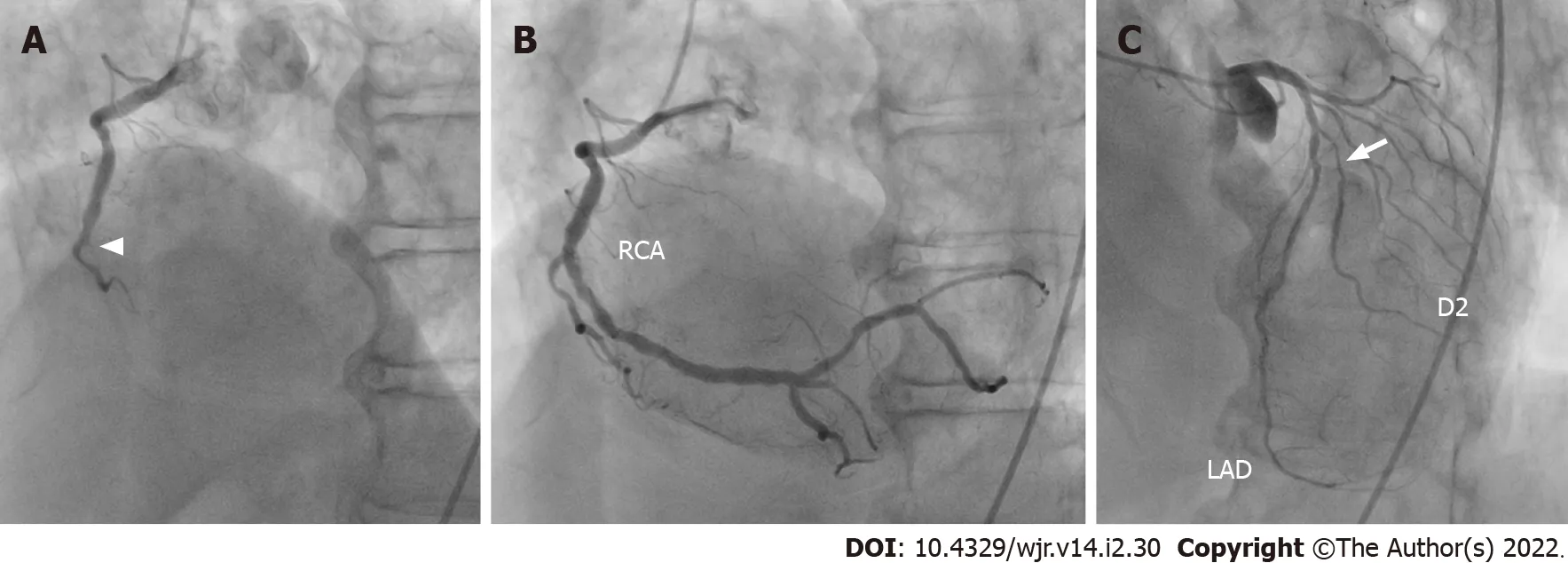
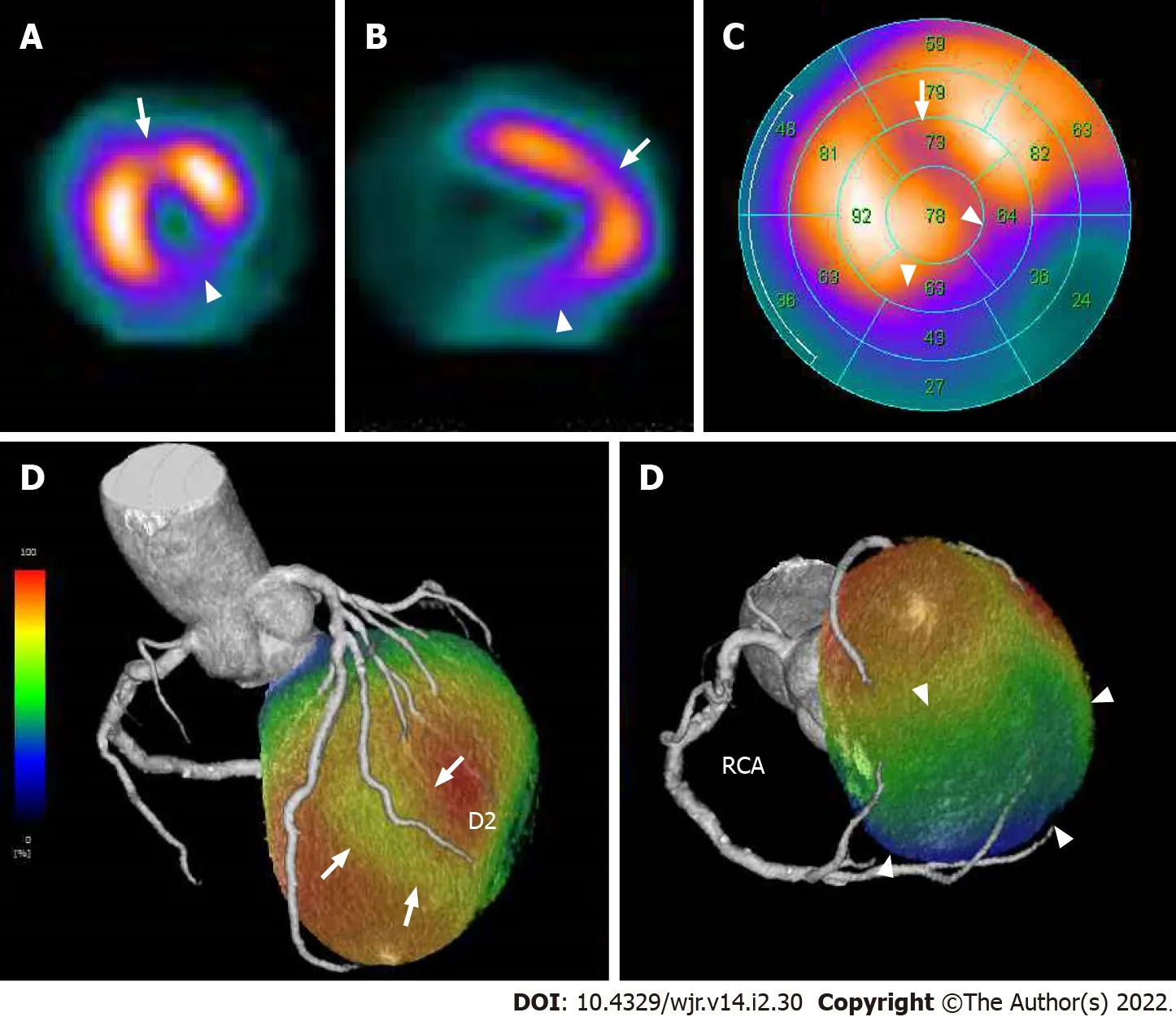
CT images are usually oriented and displayed using transaxial views,but these images do not cleanly transect the ventricle,atria,or myocardial regions supplied by the major coronary arteries.The American Heart Association(AHA)showed the cardiac plane definition and display for tomographic image modalities[20].Essentially,it has been suggested that,using any noninvasive method,the displays for evaluation of cardiac structures are presented in three orthogonal cardiac planes:horizontal long axis,vertical long axis,and short axis(Figure 1).Therefore,it is important to evaluate a suspicious findings of MPD detected in transaxial images by multiplanar reformatted cardiac plane images.To identify a culprit coronary artery and likely location of flow-limiting coronary stenosis,knowledge of the distribution of coronary blood flow in the AHA 17-segment model of the left ventricle is also important.Figure 2 shows the general assignment of the 17 myocardial segments to one of the three major coronary arteries[20].The apex,segment 17,which can be supplied by any of the three arterie,is where the greatest variability in myocardial blood supply occurs.Segments 1,2,7,8,13,14,and 17 are assigned to the left anterior descending artery(LAD)distribution,and segments 3,4,9,10,and 15 to the right coronary artery(RCA)when it is dominant.Generally,segments 5,6,11,12,and 16 are assigned to the left circumflex coronary artery(LCX).However,it should be noted that the coronary artery blood supply to the myocardial segments is variable.Coronary dominance is determined by the artery supplying the posterior descending artery(Figure 3).Among the general population,approximately 70%-80% is right-dominant(supplied by the RCA),5%-10% is left-dominant(supplied by the LCX),and 10%-20% is co-dominant(supplied by both the RCA and LCX)[21].In our experience,MPD territories demonstrated on non-ECG-gated contrast-enhanced CT agree with the results of invasive coronary angiography,radionuclide myocardial perfusion imaging,and cardiac magnetic resonance imaging with high accuracy(LAD:Figures 4 and 5,LCX:Figures 6 and 7,RCA:Figures 8 and 9).
Global myocardial ischemia
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial(CC BYNC 4.0)license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See:https://creativecommons.org/Licenses/by-nc/4.0/
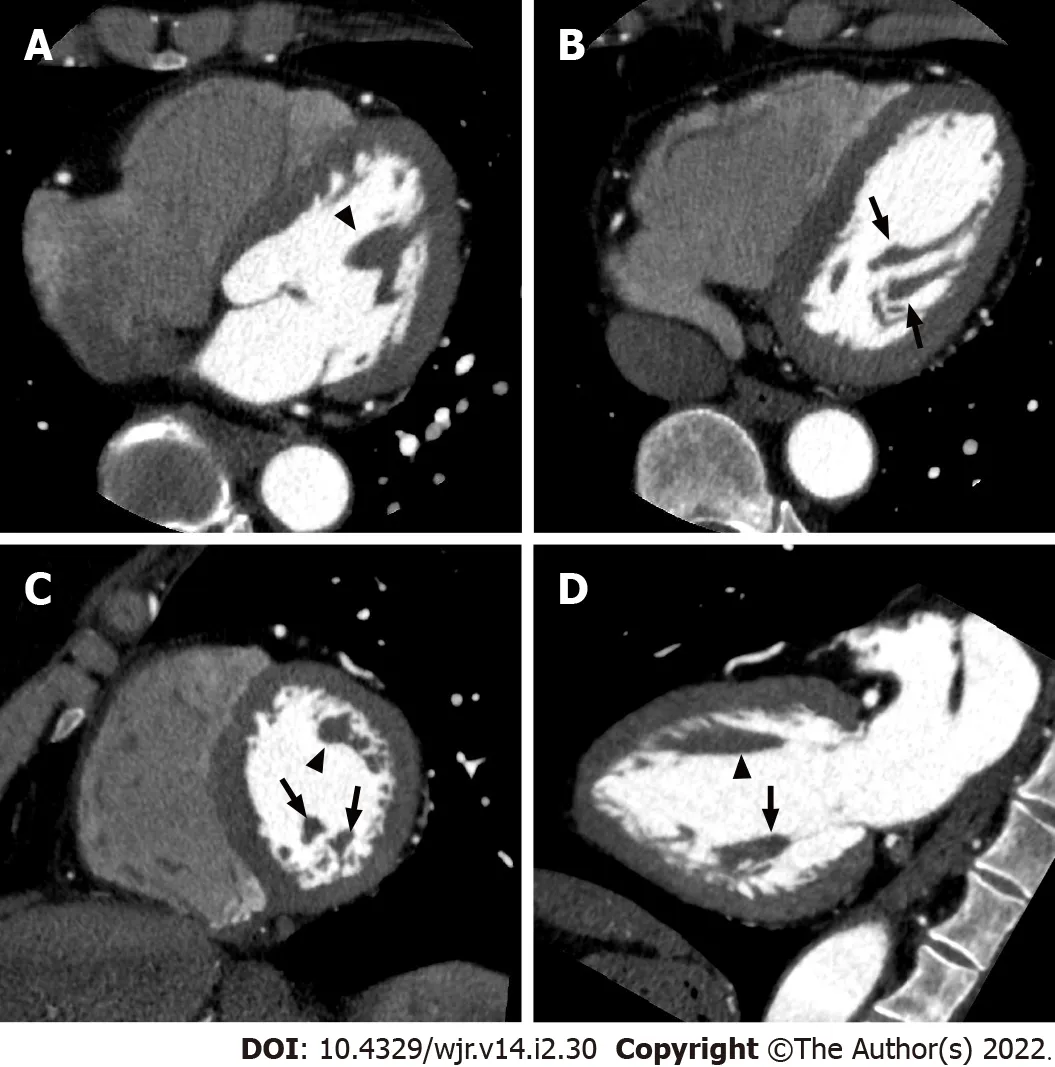
Hemopericardium
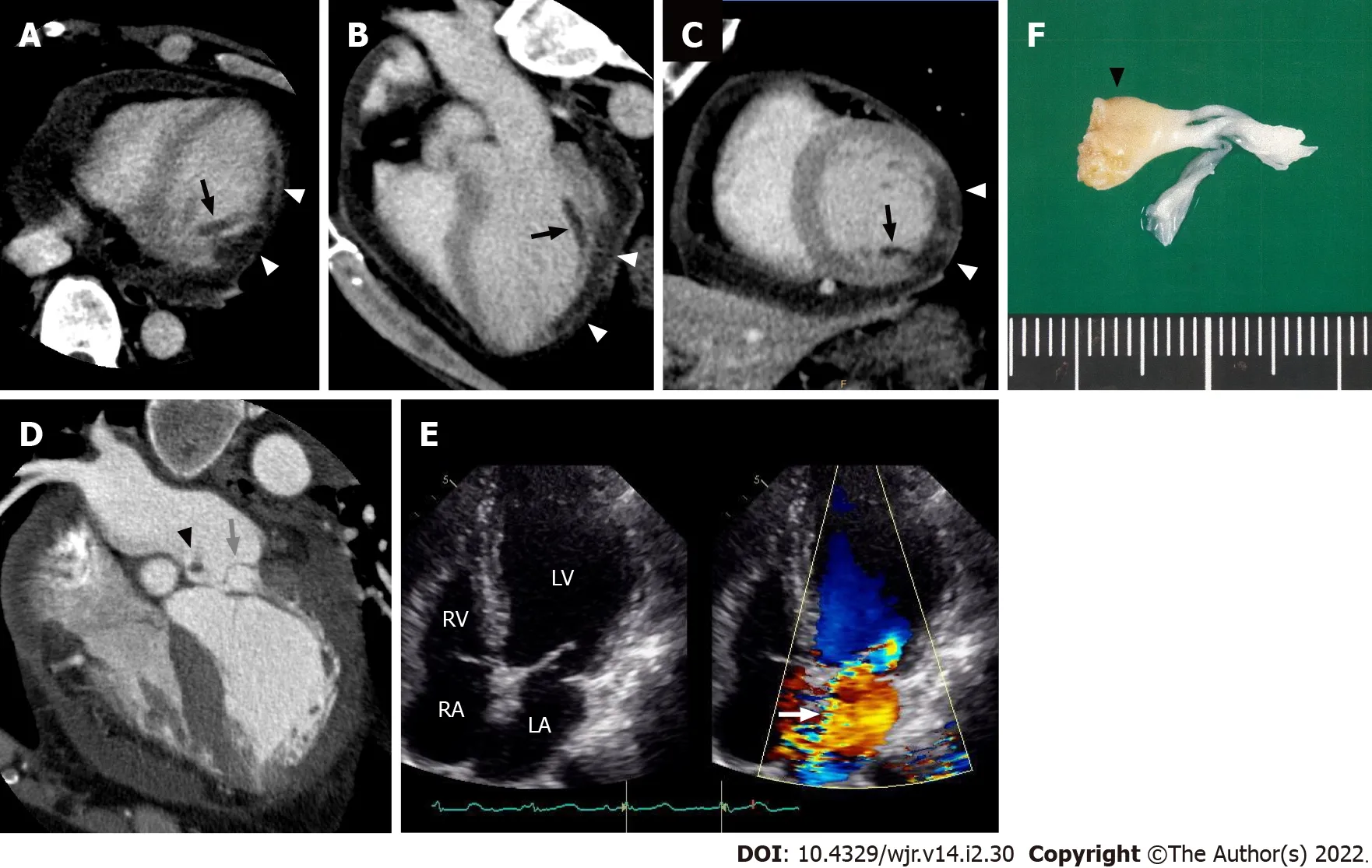
The papillary muscles are one of the components of the mitral valve apparatus[26].Two papillary muscles arise from the area between the apical and middle thirds of the left ventricular wall.Both the anterior and posterior mitral valve leaflets are attached
primary,secondary,and tertiary chordae to both anterolateral and posteromedial papillary muscles.The anterolateral papillary muscle is often composed of a single major muscle group,whereas the posteromedial papillary muscle usually comprises two or three major muscle groups(Figure 14).Left ventricular papillary muscles are particularly vulnerable to ischemia because they are perfused by the terminal portion of the coronary vascular bed.The anterolateral papillary muscle is supplied by the diagonal branches of the LAD and often by marginal branches from the LCX.In contrast,the supply to the posteromedial papillary muscle is
the posterior descending branch of the LCX or RCA(depending on dominance)[27].Necrosis of a papillary muscle is a frequent complication of MI and it should be recognized because it may lead to papillary muscle rupture,which is a rare but often-fatal mechanical complication.The posteromedial papillary muscle is particularly vulnerable to myocardial ischemia because of its single system of blood supply(Figure 15).The presence of MPD of the papillary muscle on contrast-enhanced CT is a finding suspicious of papillary muscle ischemia or necrosis,and detectable even in non-ECG-gated contrastenhanced CT(Figure 16).
Papillary muscle
Common causes of pericardial effusion include heart failure,renal failure,neoplasm,infection,and injury,including trauma and myocardial infarction[23].Pericardial fluid characteristics are reflected in the CT attenuation value.It is likely that a value closer to the value of water(0 Hounsfield units)is a simple effusion.A value greater than that of water density can be observed in conditions including malignancy,purulent exudate,and hemopericardium[23].Hemopericardium is induced by cardiac rupture,ruptured ascending aortic dissection,trauma,neoplasm,and as a consequence of cardiac surgery(iatrogenic)[24,25].Left ventricular free wall rupture is one of the complications of AMI that is often fatal.Acute rupture is usually fatal,but some patients with a small ventricular tear,which may be sealed temporarily by a clot or fibrinous pericardial adhesions,may progress to a subacute form allowing late survival.In cases with hemopericardium,the presence of MPD on contrast-enhanced CT is a finding highly suspicious of left ventricular free wall rupture and should be carefully checked.Accompanying myocardial defects are also detected even in non-ECG-gated contrast-enhanced CT(Figures 12 and 13).
Myocardial fat
Japan
CONCLUSION
Definitive diagnosis of ACS is sometimes difficult to achieve,especially in patients who present with atypical symptoms,normal initial biomarkers of myocardial necrosis,and normal or nondiagnostic ECGs.In order to avoid inappropriate management for this life-threatening event,clinicians should be
The authors declare that they have no conflicts of interest.
When the negro understood that he was being abused, he cried: Come along! I will put you into such a state that the birds of the air will weep for you
FOOTNOTES
Dogs had only played walk on parts in my family. As far as I was concerned the all defining object in a house was a television. There was one in Bill s house. It stood like a lonely, redundant sentinel() in a dank corner of his empty living room and seemed cold and unused. When I asked Bill what he watched, he answered that the set didn t work, it needed a new plug or some such, and he hadn t bothered to get it fixed. And what s more, he didn t miss it. To me this was unimaginable - how could a person have a TV and not use it?
aware that MPD is more commonly detectable even on routine non-ECG-gated contrast-enhanced CT performed in search of other pathologies.
Dana screamed for help. An airport supervisor3 appeared. He told Dana to get on the plane. Dana said that she was not moving until an ambulance arrived. The supervisor said her plane would leave without her. Dana said that she didn t care.
In a study that evaluated the presence of MPD on non-ECG-gated contrast-enhanced CT,Watanabe
[18]described a patient with AMI of the left main trunk who did not show MPD.In our experience,broad MPD induced by the occlusion of the left main trunk highlights the normally perfused myocardial enhancement in the RCA territory(Figures 10 and 11).Balanced ischemia is a well-known limitation of stress radionuclide myocardial perfusion imaging[22].MPD seen in radionuclide myocardial perfusion imaging results from the relative difference in radiotracer uptake of the left ventricular myocardium normalized to the most normal area with the highest radiotracer uptake.Therefore,in patients with ischemia that is relatively balanced among the three major vascular territories,this potentially results in a homogeneous radiotracer distribution in the myocardium,thus underestimating the severity of ischemia or even indicating a falsely normal result.MPD demonstrated on contrast-enhanced CT also reflects the relative difference in left ventricular myocardial contrast enhancement.Hence,it may be difficult to detect global myocardial ischemia as focal MPD on non-ECG-gated contrast-enhanced CT even in a rest condition.
Yoshihara S designed and performed all of this study and wrote the all of the revised manuscript.
CT attenuation values are quantitative,and they can be used to define a structure’s density or the iodine content after administration of iodinated contrast media.In a cardiac CT study,Nieman
[28]showed that CT attenuation values found in patients with long-standing(over 1 year)MI(-13 ± 37 HU)were significantly lower than in patients with acute(within 1 wk)MI(26 ± 26 HU)and normal hearts(73 ± 14 HU).Histologic analyses showed that myocardial fat at the site of a healed MI is common with a prevalence of 68%-84%[29,30].The presence of myocardial fat can be identified at the macroscopic level by CT,although a small amount of microscopic myocardial fat may be undetectable[31].Myocardial fat at the site of a MI is frequently observed as a subendocardial low attenuation in the distribution of the culprit coronary artery on both non-contrast and contrast-enhanced CT even in non-ECG-gated CT(Figure 17).Concomitant regional myocardial wall motion reduction in areas of old MI may support the clear visualization of the myocardial fat.The prevalence of left ventricular myocardial fat detected by CT increases as the infarct age becomes higher[32].Because it is important to differentiate ACS from OMI,in cases who present MPD on contrast-enhanced CT,CT-detectable myocardial fat associated with old MI should be excluded by comparison with non-contrast CT.In our experience,AMI of the RCA complicated with old MI of the diagonal branch was successfully distinguished by comparison with non-contrast CT in a non-ECG-gated CT examination(Figures 17-19).However,because OMI does not always show myocardial fat,it is difficult to differentiate ACS from OMI without CT-detectable myocardial fat only with usual contrast-enhanced computed tomography.
Shu Yoshihara 0000-0001-9294-3767.
Liu JH
A
The troll came rushing out, and was so angry and furious, and abused the king with all his might for bringing such a wretched fool with him, as he was sure that he could not pay the least bit of all the damage that had been done when he could not even pay off his old debt
Liu JH
1 Amsterdam EA,Wenger NK,Brindis RG,Casey DE Jr,Ganiats TG,Holmes DR Jr,Jaffe AS,Jneid H,Kelly RF,Kontos MC,Levine GN,Liebson PR,Mukherjee D,Peterson ED,Sabatine MS,Smalling RW,Zieman SJ;ACC/AHA Task Force Members.2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes:a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines.
2014;130:e344-e426[PMID:25249585 DOI:10.1161/CIR.0000000000000134]
2 Canto JG,Shlipak MG,Rogers WJ,Malmgren JA,Frederick PD,Lambrew CT,Ornato JP,Barron HV,Kiefe CI.Prevalence,clinical characteristics,and mortality among patients with myocardial infarction presenting without chest pain.
2000;283:3223-3229[PMID:10866870 DOI:10.1001/jama.283.24.3223]
3 Kosuge M,Kimura K,Ishikawa T,Ebina T,Hibi K,Tsukahara K,Kanna M,Iwahashi N,Okuda J,Nozawa N,Ozaki H,Yano H,Nakati T,Kusama I,Umemura S.Differences between men and women in terms of clinical features of STsegment elevation acute myocardial infarction.
2006;70:222-226[PMID:16501283 DOI:10.1253/circj.70.222]
4 Body R,Carley S,Wibberley C,McDowell G,Ferguson J,Mackway-Jones K.The value of symptoms and signs in the emergent diagnosis of acute coronary syndromes.
2010;81:281-286[PMID:20036454 DOI:10.1016/j.resuscitation.2009.11.014]
5 Larson DB,Johnson LW,Schnell BM,Salisbury SR,Forman HP.National trends in CT use in the emergency department:1995-2007.
2011;258:164-173[PMID:21115875 DOI:10.1148/radiol.10100640]
6 Shriki JE,Shinbane J,Lee C,Khan AR,Burns N,Hindoyan A,Wilcox A.Incidental myocardial infarct on conventional nongated CT:a review of the spectrum of findings with gated CT and cardiac MRI correlation.
2012;198:496-504[PMID:22357988 DOI:10.2214/AJR.11.7683]
7 American College of Cardiology Foundation Task Force on Expert Consensus Documents,Mark DB,Berman DS,Budoff MJ,Carr JJ,Gerber TC,Hecht HS,Hlatky MA,Hodgson JM,Lauer MS,Miller JM,Morin RL,Mukherjee D,Poon M,Rubin GD,Schwartz RS.ACCF/ACR/AHA/NASCI/SAIP/SCAI/SCCT 2010 expert consensus document on coronary computed tomographic angiography:a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents.
2010;55:2663-2699[PMID:20513611 DOI:10.1016/j.jacc.2009.11.013]
8 Goldstein JA,Chinnaiyan KM,Abidov A,Achenbach S,Berman DS,Hayes SW,Hoffmann U,Lesser JR,Mikati IA,O'Neil BJ,Shaw LJ,Shen MY,Valeti US,Raff GL;CT-STAT Investigators.The CT-STAT(Coronary Computed Tomographic Angiography for Systematic Triage of Acute Chest Pain Patients to Treatment)trial.
2011;58:1414-1422[PMID:21939822 DOI:10.1016/j.jacc.2011.03.068]
9 Hoffmann U,Truong QA,Schoenfeld DA,Chou ET,Woodard PK,Nagurney JT,Pope JH,Hauser TH,White CS,Weiner SG,Kalanjian S,Mullins ME,Mikati I,Peacock WF,Zakroysky P,Hayden D,Goehler A,Lee H,Gazelle GS,Wiviott SD,Fleg JL,Udelson JE;ROMICAT-II Investigators.Coronary CT angiography
standard evaluation in acute chest pain.
2012;367:299-308[PMID:22830462 DOI:10.1056/NEJMoa1201161]
10 Litt HI,Gatsonis C,Snyder B,Singh H,Miller CD,Entrikin DW,Leaming JM,Gavin LJ,Pacella CB,Hollander JE.CT angiography for safe discharge of patients with possible acute coronary syndromes.
2012;366:1393-1403[PMID:22449295 DOI:10.1056/NEJMoa1201163]
11 Cury RC,Feuchtner GM,Batlle JC,Peña CS,Janowitz W,Katzen BT,Ziffer JA.Triage of patients presenting with chest pain to the emergency department:implementation of coronary CT angiography in a large urban health care system.
2013;200:57-65[PMID:23255742 DOI:10.2214/AJR.12.8808]
12 Taylor AJ,Cerqueira M,Hodgson JM,Mark D,Min J,O'Gara P,Rubin GD;American College of Cardiology Foundation Appropriate Use Criteria Task Force;Society of Cardiovascular Computed Tomography;American College of Radiology;American Heart Association;American Society of Echocardiography;American Society of Nuclear Cardiology;North American Society for Cardiovascular Imaging;Society for Cardiovascular Angiography and Interventions;Society for Cardiovascular Magnetic Resonance,Kramer CM,Berman D,Brown A,Chaudhry FA,Cury RC,Desai MY,Einstein AJ,Gomes AS,Harrington R,Hoffmann U,Khare R,Lesser J,McGann C,Rosenberg A,Schwartz R,Shelton M,Smetana GW,Smith SC Jr.ACCF/SCCT/ACR/AHA/ASE/ASNC/NASCI/SCAI/SCMR 2010 appropriate use criteria for cardiac computed tomography.A report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force,the Society of Cardiovascular Computed Tomography,the American College of Radiology,the American Heart Association,the American Society of Echocardiography,the American Society of Nuclear Cardiology,the North American Society for Cardiovascular Imaging,the Society for Cardiovascular Angiography and Interventions,and the Society for Cardiovascular Magnetic Resonance.
2010;56:1864-1894[PMID:21087721 DOI:10.1016/j.jacc.2010.07.005]
13 Pursnani A,Lee AM,Mayrhofer T,Ahmed W,Uthamalingam S,Ferencik M,Puchner SB,Bamberg F,Schlett CL,Udelson J,Hoffmann U,Ghoshhajra BB.Early resting myocardial computed tomography perfusion for the detection of acute coronary syndrome in patients with coronary artery disease.
2015;8:e002404[PMID:25752898 DOI:10.1161/CIRCIMAGING.114.002404]
14 Leipsic J,Abbara S,Achenbach S,Cury R,Earls JP,Mancini GJ,Nieman K,Pontone G,Raff GL.SCCT guidelines for the interpretation and reporting of coronary CT angiography:a report of the Society of Cardiovascular Computed Tomography Guidelines Committee.
2014;8:342-358[PMID:25301040 DOI:10.1016/j.jcct.2014.07.003]
15 Gosalia A,Haramati LB,Sheth MP,Spindola-Franco H.CT detection of acute myocardial infarction.
2004;182:1563-1566[PMID:15150010 DOI:10.2214/ajr.182.6.1821563]
16 Moore W,Fields J,Mieczkowski B.Multidetector computed tomography pulmonary angiogram in the assessment of myocardial infarction.
2006;30:800-803[PMID:16954933 DOI:10.1097/01.rct.0000230001.15650.05]
17 Mano Y,Anzai T,Yoshizawa A,Itabashi Y,Ohki T.Role of non-electrocardiogram-gated contrast-enhanced computed tomography in the diagnosis of acute coronary syndrome.
2015;30:1-8[PMID:24221182 DOI:10.1007/s00380-013-0437-8]
18 Watanabe T,Furuse Y,Ohta Y,Kato M,Ogawa T,Yamamoto K.The Effectiveness of Non-ECG-Gated Contrast-Enhanced Computed Tomography for the Diagnosis of Non-ST Segment Elevation Acute Coronary Syndrome.
2016;57:558-564[PMID:27593539 DOI:10.1536/ihj.16-072]
19 Yamazaki M,Higuchi T,Shimokoshi T,Kiguchi T,Horii Y,Yoshimura N,Aoyama H.Acute coronary syndrome:evaluation of detection capability using non-electrocardiogram-gated parenchymal phase CT imaging.
2016;34:331-338[PMID:26883335 DOI:10.1007/s11604-016-0527-5]
20 Cerqueira MD,Weissman NJ,Dilsizian V,Jacobs AK,Kaul S,Laskey WK,Pennell DJ,Rumberger JA,Ryan T,Verani MS;American Heart Association Writing Group on Myocardial Segmentation and Registration for Cardiac Imaging.Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart.A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association.
2002;105:539-542[PMID:11815441 DOI:10.1161/hc0402.102975]
21 Angelini P.Coronary artery anomalies--current clinical issues:definitions,classification,incidence,clinical relevance,and treatment guidelines.
2002;29:271-278[PMID:12484611]
22 Berman DS,Kang X,Slomka PJ,Gerlach J,de Yang L,Hayes SW,Friedman JD,Thomson LE,Germano G.Underestimation of extent of ischemia by gated SPECT myocardial perfusion imaging in patients with left main coronary artery disease.
2007;14:521-528[PMID:17679060 DOI:10.1016/j.nuclcard.2007.05.008]
23 Wang ZJ,Reddy GP,Gotway MB,Yeh BM,Hetts SW,Higgins CB.CT and MR imaging of pericardial disease.
2003;23 Spec No:S167-S180[PMID:14557510 DOI:10.1148/rg.23si035504]
24 Haddadin S,Milano AD,Faggian G,Morjan M,Patelli F,Golia G,Franchi P,Mazzucco A.Surgical treatment of postinfarction left ventricular free wall rupture.
2009;24:624-631[PMID:20078707 DOI:10.1111/j.1540-8191.2009.00896.x]
25 Restrepo CS,Gutierrez FR,Marmol-Velez JA,Ocazionez D,Martinez-Jimenez S.Imaging patients with cardiac trauma.
2012;32:633-649[PMID:22582351 DOI:10.1148/rg.323115123]
26 Otto CM.Clinical practice.Evaluation and management of chronic mitral regurgitation.
2001;345:740-746[PMID:11547744 DOI:10.1056/NEJMcp003331]
27 Voci P,Bilotta F,Caretta Q,Mercanti C,Marino B.Papillary muscle perfusion pattern.A hypothesis for ischemic papillary muscle dysfunction.
1995;91:1714-1718[PMID:7882478 DOI:10.1161/01.cir.91.6.1714]
28 Nieman K,Cury RC,Ferencik M,Nomura CH,Abbara S,Hoffmann U,Gold HK,Jang IK,Brady TJ.Differentiation of recent and chronic myocardial infarction by cardiac computed tomography.
2006;98:303-308[PMID:16860013 DOI:10.1016/j.amjcard.2006.01.101]
29 Baroldi G,Silver MD,De Maria R,Parodi O,Pellegrini A.Lipomatous metaplasia in left ventricular scar.
1997;13:65-71[PMID:9039067]
30 Su L,Siegel JE,Fishbein MC.Adipose tissue in myocardial infarction.
2004;13:98-102[PMID:15033159 DOI:10.1016/S1054-8807(03)00134-0]
31 Kimura F,Matsuo Y,Nakajima T,Nishikawa T,Kawamura S,Sannohe S,Hagiwara N,Sakai F.Myocardial fat at cardiac imaging:how can we differentiate pathologic from physiologic fatty infiltration?
2010;30:1587-1602[PMID:21071377 DOI:10.1148/rg.306105519]
32 Ichikawa Y,Kitagawa K,Chino S,Ishida M,Matsuoka K,Tanigawa T,Nakamura T,Hirano T,Takeda K,Sakuma H.Adipose tissue detected by multislice computed tomography in patients after myocardial infarction.
2009;2:548-555[PMID:19442939 DOI:10.1016/j.jcmg.2009.01.010]
