Endoscopic ultrasound-guided through-the-needle microforceps biopsy and needle-based confocal laser-endomicroscopy increase detection of potentially malignant pancreatic cystic lesions:A single-center study
2022-05-19CarlosRoblesMedrandaJuanOlmosMiguelPugaTejadaRobertoOleasJorgeBaquerizoBurgosMarthaArevaloMoraRaquelDelValleZavalaJoaoAutranNebelDanielCalleLoffredoHannahPitangaLukashok
lNTRODUCTlON
The incidence of pancreatic cystic lesions (PCLs) is rising mainly in elderly patients[1].Therefore,early detection of potentially malignant PCLs increases the possibility of a curative approach.Current American Gastroenterological Association guideline recommends magnetic resonance imaging (MRI) or magnetic resonance cholangiopancreatography (MRCP) to assess PCLs[2].For the same purpose,the revised Fukuoka guideline recommend computerized tomography (CT),MRI or MRCP,keeping endoscopic ultrasound guided fine-needle aspiration (EUS-FNA) for intraductal papillary mucinous neoplasm (IPMN) evaluation[3].Nevertheless,both guidelines showed an unsatisfactory pooled sensitivity for malignant PCLs of 64% and 59%,respectively[4].
EUS is the most sensitive diagnostic method for detecting potentially malignant pancreatic lesions with an 88.5% sensitivity;yet it holds a 52.9% specificity and a higher inter-observer variability.Thus,EUS alone has very low diagnosability capacity[5-7].Similarly,a considerable number of PCLs cannot be characterized by CT,MRI or MRCP alone[8,9].EUS-guided diagnostics techniques increase EUS accuracy for differentiating PCLs,namely:(1) EUS-FNA;(2) Contrast-enhanced EUS (CE-EUS);(3) Fiberoptic probe cystoscopy (cystoscopy);(4) EUS-guided through-the-needle direct intracystic micro forceps biopsy (mFB);and (5) EUS-guided confocal laser endomicroscopy (nCLE)[9].
EUS-FNA allows biopsy of suspicious lesions and cytological and biochemical cystic fluid analysis[7].Whereas,CE-EUS help to differentiate between solid
PCLs,by detecting enhanced septa or nodules present within cystic lesions[10].Through-the-needle fiberoptic probe cystoscopy requires a 19-gauge needle guided by EUS to locate and enter the PCL.Then,the preloaded fiberoptic probe is advanced,allowing visualization of the cyst content as cystic wall features[11].The microforceps device samples tissue from the cyst’s wall,septations,and/or mural nodules and thus increase cellular yield[12].Furthermore,nCLE characterizes PCLs type by imaging the intact cyst architecture,targeting abnormal areas and reducing unnecessary sampling of surrounding tissue,with a diagnostic accuracy of 80% to 95%[8].
Given the poor prognosis of malignant pancreatic lesions,determining the best diagnostic approach for early detection of potential malignancy among the variety of newly available EUS-related technology is essential.Therefore,we aimed to compare the accuracy of EUS for detection of potentially malignant PCLs when it is performed alone,EUS-FNA,CE-EUS or cystoscopy and associated with novel EUS-related techniques:mFB and nCLE.We hypothesize that EUS-guided through-the-needle mFB and nCLE may increase malignancy detection during EUS assessment of pancreatic cysts.
MATERlALS AND METHODS
Study design
The following is an observational,analytic,longitudinal,retrospective cohort and single-center study performed at the Instituto Ecuatoriano de Enfermedades Digestivas (IECED),a tertiary center in Ecuador.The study protocol and informed consent documents were approved by the institutional review board,and the study was conducted in accordance with the Declaration of Helsinki.Selected patients signed corresponding informed written consent for healthcare purposes.
Population selection
Records from patients older than 18 years of age who underwent EUS at IECED from January 2013 to March 2018 were extracted from the institutional database.Cases with non-pancreatic lesions were excluded.Patients were allocated to three cohorts:(1) Patients who had been evaluated
EUS alone;(2) Patients who had been evaluated with EUS-FNA,CE-EUS and/or cystoscopy;and (3) Those evaluated with novel EUS-related techniques:mFB and nCLE.
Endoscopic techniques malignancy criterion for pancreatic cystic lesions
Due to sparse cellularity of acquired specimens,several complementary clinical,radiological,and imaging techniques are required to achieve PCLs definitive diagnosis.PCLs with potential to progress to malignancy mainly IPMN,mucinous cystic neoplasms (MCN),and neuroendocrine tumors (c-NET) with cystic degeneration.Identifying malignancy features for these lesions with EUS,CE-EUS,cystoscopy,nCLE,FNA,and mFB include the following:
Demographic,clinic,endoscopic and histopathological and 24-mo follow-up data were obtained from the institutional database and phone calls when necessary.The study endpoint was to determine agreement between detection of potentially malignant in PCLs (EUS malignancy detection) and malignancy after 24-mo follow-up.EUS malignancy detection was defined based on procedure findings (EUS-alone,CE-EUS,cystoscopy and/or nCLE) reported on endoscopic records,as well as EUS-FNA and/or EUS-mFB aquired biopsy results when available.PCLs were classified as malignant (MCN,IPMN and c-NET) according to Fukuoka criteria.This data was recovered by two endoscopists (C.R.M.and H.P-L.).Malignancy after 24-mo follow-up was based on clinical outcomes,endoscopic surveillance,or surgical specimen histopathology when available.This data was recovered by two general practitioners (R.O.and J.B-B.) and a general surgeon (D.C-L.) who were blinded to information concerning to EUS malignancy detection.
A thick/hyper-enhancing wall/septum,enhancing solid component within a cyst,or an enhancing mural nodule favors malignancy criterion.Furthermore,there is a radiological correlation between pancreatic duct communication and IPMN diagnosis,but not MCN.Also,main duct type IPMNs hold a higher risk of malignancy transformation than branch duct type IPMNs (up to 68%
22%,respectively).MCN may show peripheral calcifications within multilocular septate lesions[3,14].
Independently,there was a positive statistical association and observed agreement for EUS malignancy detection with cystoscopy,mFB or nCLE,and 24-mo follow-up.EUS-FNA and CE-EUS exhibited a positive but nonsignificant association;whereas EUS alone only presented a negative significantly association [OR 0.066 (0.025-0.157;
0.001)] when considering the agreement between EUS malignancy detection and malignancy after 24-mo follow-up as an outcome.
Prone to malignancy lesions may depict epithelial or vascular patterns in nCLE[5,8,11,13,15].nCLE Epithelial patterns:MCN show epithelial borders with a flat mosaic appearance (single or multiple layers of epithelial bands).IPMN exhibit dark rings and papillary projections.c-NET portray a trabecular pattern (fibrous bands separating cells nests).nCLE Vascular patterns:MCN,IPMN and cystic-NET may show a branched pattern;IPMN and MCN may also display a rope-ladder pattern[5].
An offline interobserver analysis (IOA) of the EUS criteria (EUS borders,lobularity,wall,microcyst component,diagnosis,and level of confidence) was performed by three endoscopists (J.O.,R.V.and J.N.) using a randomly selected EUS image set (
=111 cases) collected by C.R-M.
IPMNs histologic examinations exhibit four possible morphologies:gastric (columnar cells lining papillae with basally located nuclei rich in apical mucin),intestinal (similar morphology to colonic villous adenomas with cigar shaped nuclei and variable apical mucin amount),pancreaticobiliary (more complex papillae composed of rounded nuclei cuboidal cells with some prominent nucleoli),and oncocytic (complex papillae lined with round cells with granular eosinophilic cytoplasm and prominent central nucleoli)[3,14].
MCNs also display low and high-grade dysplasia features.While bland mucin-containing epithelium honeycomb sheets are seen with low-grade MCNs,a complex papillary structure with smooth nuclear contour mucin-containing cells,inconspicuous nucleoli,and fine chromatin is found in high-grade MCNs.On histologic examination,MCNs show focally flat o cuboidal lining and tall mucin-containing epithelium,with a densely ovarian-type stroma wall that positively stains for progesterone/estrogen receptors,calretinin,and inhibin[3,14].
C-NET aspirate display classic endocrine morphology (pseudorosettes,isolated,and loosely cohesive groups of round/polygonal cells with finely stippled chromatin round nucleus)[5,11,14,15].Immunostains (chromogranin,CD10,vimectin,and β-catenin cytoplasmic expression) provide a definitive diagnosis[14].
Endoscopic techniques methods
Three experienced endosonographers (C.R-M.,J.O.,R.V.) performed all EUS evaluations,under general anesthesia with patients in the supine position and use of antibiotic prophylaxis.EUS procedures were performed with a linear-array video echoendoscope (EG-3870 UTK,Pentax Medical,Montalve,NJ,United States) attached to an ultrasound console (HI VISION Avius
,Hitachi Medical Systems,Steinhaus,Switzerland).Indication of EUS-related techniques was based on endosonographers discretion.Although more techniques are available to perform on larger cysts (>3 cm).
EUS-FNA was performed with a 19-gauge needle (Expect™ Slimline,Boston Scientific,Malborough,United States) (Figure 1A).The cystic fluid was examined for tumor markers (amylase,lipase,carcinoembryonic antigen levels).
To display cystic wall and nodule vascularization,4.8 mL of SonoVue
(Braccio,Milan,Italy) was used for CE-EUS.Cystic wall and nodule vascularization were defined as visible contrast enhancer bubble movement within the cystic wall,septum,and nodules (Figure 1B),and were referred for further diagnosis with EUS-FNA.
Examinations were performed by using a linear-array video echoendoscope attached to an ultrasound console,as previously described.A SOC fiber optic probe (Legacy SpyGlass
fiber optic,Boston Scientific,Marlborough,United States) was inserted through the 19-gauge needle into the cystic cavity to observe the intracystic wall and contents (Figure 1C).

The target lesion was identified under EUS and punctured with a 19-gauge FNA needle.With the needle inside the lesion,the stylet was removed,and the micro forceps (Moray™ micro forceps,STERIS,Mentor,United States) were inserted through the needle for tissue sampling.Two to three bites of biopsy specimens were taken with each pass of the micro forceps.The tissue acquisition was visually confirmed and directly placed on formalin containers for pathologic evaluation.
After EUS examination,patients were intravenously injected with 5 mL of 10% fluorescein (BioGlo
,Sofar Productos,Bogota,Colombia) 2 to 3 min before nCLE imaging.CLE was performed using the AQ-Flex nCLE miniprobe (Cellvizio,Mauna Kea Technologies,Paris,France).The probe was advanced through the locking device into the 19-gauge needle.The preloaded needle was advanced under EUS guidance into the PCL.The tip of the nCLE probe was placed in contact with the intracystic epithelium,and intracystic endomicroscopic images were captured (Video 1and Video 2).After image acquisition,the nCLE probe was withdrawn,and the PCL was aspirated.
Data abstraction
Presenting two out of the three following characteristics was considered as increased risk for malignancy criteria:main pancreatic duct dilation between 5-9 mm (10 mm high risk stigmata for malignancy),PCLs size>3 cm,and mural nodules presence[3,13].
A hard winter followed this summer. Snow-storms swept over landand sea, and there was difficulty in getting from one place toanother. How unequally things are distributed in this world! Herethere was bitter cold and snow-storms, while in Spain there wasburning sunshine and oppressive heat. Yet, when a clear frosty daycame, and Jurgen saw the swans flying in numbers from the seatowards the land, across to Norre-Vosborg, it seemed to him thatpeople could breathe more freely here; the summer also in this part ofthe world was splendid. In imagination he saw the heath blossom andbecome purple with rich juicy berries, and the elder-bushes andlime-trees at Norre Vosborg in flower. He made up his mind to go there again.
Interobserver agreement
EUS-FNA and EUS-mFB are resources for tissue sample extraction.For these techniques,cytology should be assessed in the context of radiological and clinical findings[3,11,14].Low and high-grade IPMN dysplasia should be distinguished as the latter may easily become invasive.Low-grade IPMN:may resemble normal gastric epithelium.High-grade IPMN may show a cell size ≤ 12 μm,hypo/hyperchromasia,background necrosis,nuclear irregularity,large single vacuolated cells,and increased nuclear to cytoplasmic ratio[14].
We described that pairing EUS,mFB,and nCLE,had a statistically significant improved detection of potentially malignant PCLs compared to any of the evaluated techniques alone.No adverse events were documented,and a 100% technical success rate was achieved.
Statistical analysis
Final database was consolidated and encrypted by M.A-M.Data analysis was performed by IECED Institutional Biostatistician (M.P-T.) using R v.4.0 (R Foundation for Statistical Computing,Vienna,Austria).A
-value<0.05 was considered statistically significant.
:We considered a 100% specificity of EUS + nCLE for the prediction of potentially malignant PCLs,with a 35% disease prevalence (6/31 mucinous cystic neoplasm and 5/31 IPMNs) for defining the sample size (16).We estimated a sample size of 25 patients for each cohort,with an α and β-error of 5% and 20% respectively,and an 80% statistical power.
:Numeric variables were described through the mean ± SD or median (minimummaximun range) in accordance with statistical distribution (Kolmógorov-Smirnov test).Categorical variables were described with frequency (%),and 95%CI when corresponding.Descriptions about techniques combination was summarized on a Venn Diagram (17).
:Observed agreement between EUS malignancy detection and malignancy after 24-mo follow-up was established.The statistical association between EUS alone or EUS with an additional endoscopic technique
the positive observed agreement described above was determined by binary logistic regression [odds ratio (OR)].A univariate analysis was performed for each individual technique.Those with a significant association were entered into the multivariate analysis.The overall diagnostic accuracy for malignancy detection was determined for each diagnostic procedure which shown significance on multivariate analysis,considering a 24-mo follow-up as gold standard.Overall diagnostic accuracy comprehended calculation of sensitivity,specificity,positive predictive value (PPV),negative predictive value (NPV),positive likelihood ratio,negative likelihood ratio,and observed agreement.For multivariate analysis discrimination,we estimated the corresponding area under the receiver operating characteristics (AUROC) curves and contrasting using the DeLong’s test for two ROC curves.The IOA of the EUS criteria was performed using Fleiss’ kappa score (κ) calculation and interpreted based on Landis and Koch criteria.
RESULTS
Patient selection
A total of 2812 patients were referred to our unit for diagnostic EUS along study period.Of these,856 had pancreatic lesions,of which 129 patients with PCLs were included for analysis (
=129) (Figure 2).

Baseline characteristics
The median age of the 129 patients with PCLs was 69 years,and 69.8% patients were female.The most frequent pancreatic cyst location was the head of the pancreas (35.7%).Younger patients were significantly evaluated with EUS and an additional novel technique (mFB and/or nCLE) in comparison to those evaluated with EUS alone,EUS-FNA,CE-EUS or cystoscopy (
0.001).Cysts size above 30 mm were reported among patients evaluated with EUS and an additional novel technique (46.3%) compared with general cohort (27.1%;
<0.001).There were no statistically significant differences when comparing gender and PCLs location between patients evaluated with EUS alone and those evaluated with EUS plus additional diagnostic techniques (Table 1).
1. A widow: A widow often inspires sympathy, perhaps even pity, in fairy tales, except for when she is a stepmother, too. Here the woman is not a stepmother, but she quickly loses the audience s sympathy with her abusive behavior.Return to place in story.
But the whole shop, from the till down to the shavings, from that night changed their opinion of the tub, and they looked up to it, and had such faith in it that they were under the impression that when the grocer read the art and drama critiques out of the paper in the evenings, it all came from the tub

EUS was performed with an additional diagnostic technique in 82/129 patients:EUS-FNA [21/82 (25.6%)],CE-EUS [20/82 (24.4%)],cystoscopy [27/82 (32.9%)],mFB [36/82 (43.9%)],and nCLE [44/82 (53.7%)].More than one diagnostic technique was performed in a sample proportion (Figure 3).A 100% technical success was reached,with no documented adverse events for any of the performed procedures.

According to the PCLs EUS findings and guided biopsy when available (
=53),potentially malignant PCLs were detected in 81/129 (62.8%) patients,and the most frequent lesion among this group was IPMN [70/129 (54.3%)].In the nonmalignant group [48/129 (37.2%)],46 cases were serous cystadenomas (Table 1).Observed agreement between EUS malignancy detection and malignancy after 24 -mo follow-up was higher in patients evaluated with EUS plus at least one additional novel technique (mFB and/or nCLE),followed by EUS-FNA,CE-EUS and or cystoscopy;than in patients evaluated with EUS alone [42/55 (80.0%)
18/27 (66.7%)
8/47 (17%),respectively;OR 4.35,95%CI:2.70-7.37;
0.001].
Univariable and multivariable analysis
Cloudy fluid and a smooth cyst wall identify MCN,while finger-like projections and a mucin cloud are perceived with IPMN through single-operator cholangioscopy (SOC)[11,14].
Through multivariate analysis,we confirmed that malignancy detection was significantly more accurate with nCLE [OR 8.441 (2.698-33.081;
0.001)] and mFB [OR 3.425 (1.104-11.682;
0.038)] than cystoscopy [OR 0.622 (0.125-2.813;
0.541)] (Table 2).

Diagnostic accuracy for determining malignancy
EUS alone was performed in 47 cases and had a sensitivity,specificity,PPV,and NPV of 100%,3%,15%,and 100%,respectively.EUS-FNA,CE-EUS,and/or cystoscopy was performed in 28 cases and had a sensitivity,specificity,PPV,and NPV of 91%,47% 53% and 89%,respectively.EUS with nCLE and mFB yielded similar results for sensitivity (89%
88%),specificity (86%
82%),PPV (62%
58%) and NPV (97%
96%).When the three techniques were simultaneously performed (EUS with nCLE and mFB,
=26),the diagnostic accuracy analysis showed that the sensitivity,specificity,PPV,and NPV were 100%,89%,78%,and 100%,respectively.MCC identified a good correlation between EUS malignancy detection and malignancy after the 24-mo follow-up through different techniques.Nonetheless,EUS paired with nCLE and mFB showed the highest agreement (MCC=0.83) (Table 3).

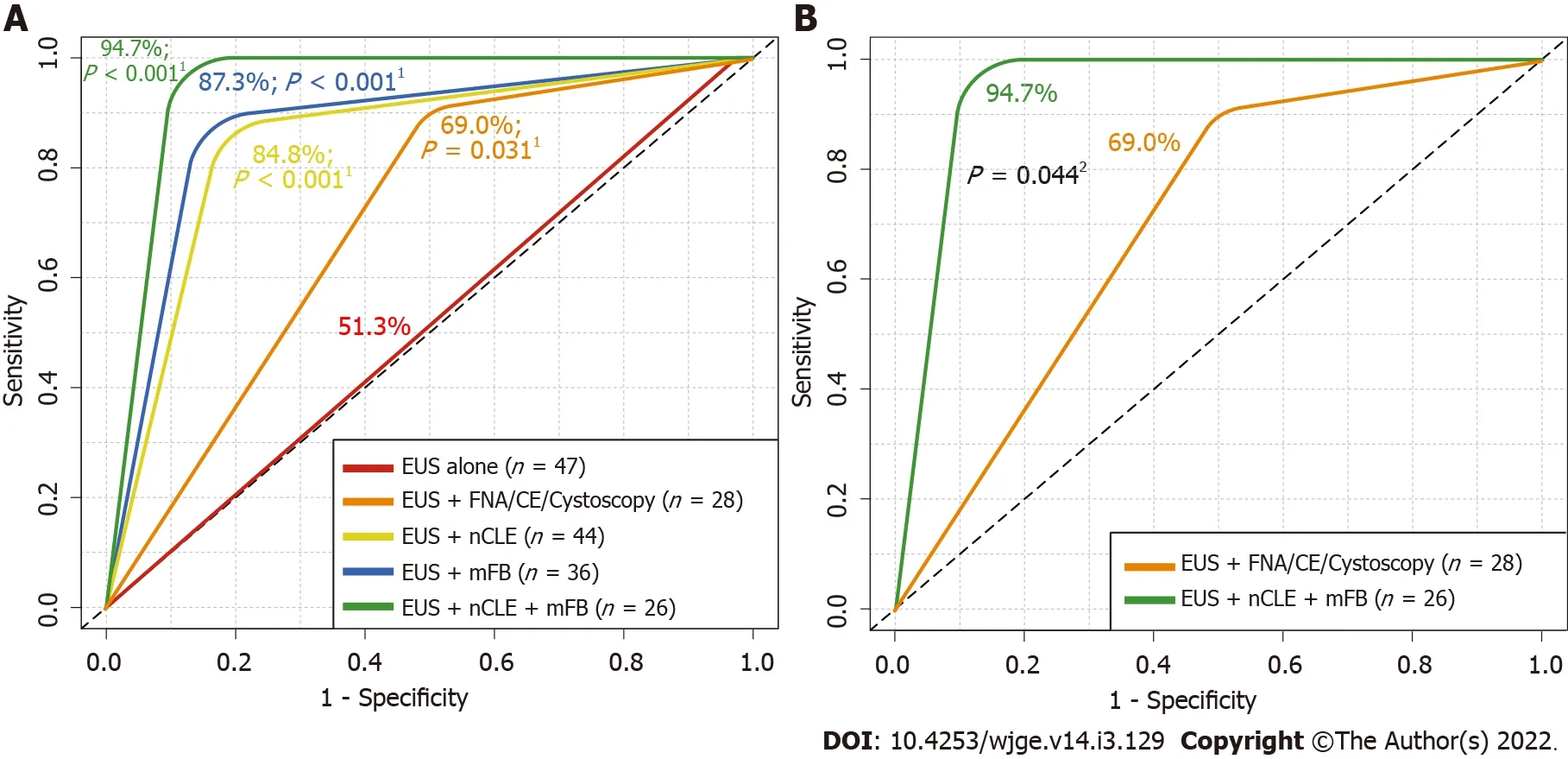
Detection of potentially malignant PCLs using EUS alone reached a 51.3% AUROC (
0.3599;moderate agreement).Meanwhile,EUS-guided mFB,nCLE or/and mFB reached an 87.3% AUROC (
0.001),84.8% (
0.001) and 94.7% (
0.001),respectively.In addition,nCLE reached a greater AUROC in comparison to EUS alone (
0.001) (Figure 4A).Moreover,a significantly higher AUROC was described for combined EUS-guided nCLE and mFB in comparison to EUS-FNA/CEEUS/cystoscopy (94.7%
69%,
=0.044) (Figure 4B).
Interobserver agreement
In the secondary IOA performed by three experienced endoscopists,the κ values in EUS borders,lobularity,wall,microcyst component,diagnosis,and level of confidence were as follows:0.12 (poor agreement),0.08 (poor agreement),0.04 (poor agreement),0.29 (fair agreement),0.21 (fair agreement),and 0.06 (poor agreement) respectively.
He jumped out of the car, grabbed some kid and pushed him up against a parked car, shouting, What was that all about and who are you? Just what the heck are you doing? Building up a head of steam, he went on That s a new car and that brick you threw is gonna cost a lot of money. Why did you do it?
DlSCUSSlON
Various clinically-available advanced EUS-guided diagnostic techniques have improved the accuracy of malignancy detection among PCLs;however,these techniques are not referenced in current guidelines,with unsatisfactory diagnostic accuracy in the risk stratification of potentially malignant PCLs[4].
To provide guidance on the relative accuracy and effectiveness of these new EUS-related techniques,we compared various additional endoscopic techniques during the EUS evaluation of PCLs.We evaluated the accuracy of EUS alone with more recent EUS-related techniques,namely EUS-FNA,cystoscopy,nCLE,mFB,and CE-EUS and found that the highest level of malignancy detection can be achieved when EUS is combined with both nCLE and direct intracystic mFB.
An increasing number of PCLs have been identified due to the growing use of complementary diagnostic techniques,such as CT and MRI;moreover,the malignancy potential of PCLs vary,and current diagnostic techniques cannot characterize the lesions with precision by their self[18-20].Due to the malignancy potential,patients with pancreatic neoplasms are recommended to undergo resection therapy;however,for patients with a high risk of postsurgical complications,preoperative determination of malignancy is critical for management guidance.
Either ending serves another great purpose: reminding people to be charitable and help the poor during the holidays, and hopefully year round, to keep young children from suffering with poverty and death.Return to place in story.
After a few years, the guy finally graduated and decided3 to further his studies overseas. Before leaving, he proposed4 to the girl, I m not very good with words. But all I know is that I love you. If you allow me, I will take care of you for the rest of my life. As for your family, I ll try my best to talk them round. Will you marry me?
In our study,EUS alone had a low agreement in comparison to the 24-mo follow-up.Also,in an offline interobserver agreement between three endosonographers,endoscopic criteria showed low agreement between operators,as previously described.Therefore,EUS itself should be complemented with additional endoscopic techniques for a more accurate detection of malignancy in PCLs.
Wang
[21] demonstrated that EUS-FNA can accurately confirm the presence of malignancy but does not perform well at excluding malignant or premalignant pancreatic lesions.This procedure achieved a pooled sensitivity and specificity of 51%,94%,respectively,for differentiating malignant lesions.In our study,which included 21/129 patients with pancreatic lesions for whom FNA was performed,we found that EUS-FNA did not achieve statistical significance in detecting malignancy with a modest agreement with the 24-mo follow-up;however,this may be due a limited number of cases in our cohort.
The good-natured fiddler bent13 down to pick it up, but in the twinkling of an eye the little man had jumped on to his back, and beat him till he was black and blue all over his head and body
The DETECT trial revealed that a combination of through-the-needle cystoscopy and nCLE for PCLs under EUS was feasible,with a sensitivity of 90% for cystoscopy in the clinical diagnosis of MCNs
an 80%sensitivity for nCLE,and a 100% sensitivity for the combination of both[11].In our study,we analyzed both techniques (separately and then combined) and obtained similar results - we obtained a sensitivity of 89% for EUS-guided-nCLE and 88% for EUS-guided through-the-needle cystoscopy;however,the sensitivity of EUS-guided nCLE combined with mFB was 78%.Additionally,in our cohort,we had more heterogenic lesions than in the DETECT trial,which was limited to mucinous lesions.
A little while before, Leip had been in the arms of a pretty greengrocers daughter nicknamed Lili. He was dreamily thinking about her when out of the lamp-lit haze8 came Marleen, a coquettish beauty with sea-green eyes whom Leip had met at an art gallery. For him it was love at first sight.
Haghighi
[8] compared the diagnostic accuracy of nCLE and EUS-FNA,where nCLE was found to have a higher accuracy (87.5%),sensitivity (91.7%),and NPV (93.3%).In our cohort,44/129 patients underwent nCLE,obtaining similar results (an 86.0% accuracy,an 89% sensitivity,and an NPV of 96%).Konda
[22] reviewed 31 PCLs that were examined using nCLE,and showed a high specificity (100%) and PPV (100%);and an overall accuracy of 71%.In our study,we obtained a higher sensitivity (89%),NPV (96%) and accuracy (86%) probably owing to a higher number of cases.
EUS-nCLE and mFB exhibited an 86.4% and an 83.3% agreement for PCLs malignancy detection,probably due to a better
cyst component evaluation and guided tissue acquisition.EUS combined with nCLE and mFB reached the highest AUROC (94.7%),in comparison to independent nCLE (87.3%) and mFB (84.8%).We propose that these techniques should be considered for the diagnostic workup of PCLs.
Then the old troll-hag flew into such a rage that she burst,62 and the Princess with the long nose and all the little trolls must have burst too, for they have never been heard of since. The Prince and his bride set free all the Christian folk who were imprisoned28 there, and took away with them all the gold and silver that they could carry,63 and moved far away from the castle which lay east of the sun and west of the moon.
The main limitation of our study lies in its retrospective design and in establishing an agreement of different endoscopic techniques for determining potential malignancy among different types of PCLs.This resulted in a difficulty in the recovery of different size cysts,where the smaller the cyst,the fewer the diagnostic methods at our disposal for use.On the other hand,larger cysts (specially over 30 mm),allowed us to perform a wider array of diagnostic procedures,including novel techniques.Moreover,these novel endoscopic techniques (
nCLE),are costly,limiting their widespread use.Furthermore,these tools require training,which increase the procedure’s startup cost.Despite these limitations,we compared these endoscopic techniques in terms of their ability to detect potential malignancy in patients with PCLs,and not only pancreatic lesions,as with other studies.Finally,as this study was designed in the context of PCLs assessment with EUS,to estimate EUS (and eventual used related techniques) diagnosability of malignancy considering a 24-mo follow-up as gold standard,a prospective diagnostic trial to re-analyse histopathological samples of PCLs after discarding malignancy during follow-up may be warranted to further asses the accuracy in diagnosing high-grade dysplasia/adenocarcinoma in non-malignant PCLs (MCN,IPMN) using the studied endoscopic techniques.
CONCLUSlON
To define formal diagnostic and therapeutical guidelines,we encourage researchers to conduct longterm follow-up randomized multicenter and cost-benefit studies,comparing newly available endoscopic techniques for the assessment of PCLs.
ARTlCLE HlGHLlGHTS
Research background
Pancreatic cystic lesions (PCLs) incidence is rising mainly in elderly patients.Accurate diagnosing and appropriate management of patients with malignant PCLs,have a positive impact in regards of healthcare expenses and in patients’ quality of life.
Research motivation
Currently,there is insufficient data about the accuracy in the diagnosing of PCLs,especially with novel endoscopic techniques.Furthermore,the early detection of potentially malignant PCLs,increases the possibility of a curative approach in said patients.
Research objectives
Given the poor prognosis of malignant PCLs,attaining early detection,an accurate diagnosis,and determining the best diagnostic approach with newly available endoscopic techniques,was essential to this study.
Research methods
This was a retrospective,single-center study.Patients were allocated to three evaluation cohorts:(1)Endoscopic ultrasound (EUS) alone;(2) EUS- fine needle aspiration,contrast-enhanced-EUS and/or EUS-guided fiberoptic probe cystoscopy (cystoscopy);and (3) EUS-guided direct intracystic microforceps biopsy (mFB) and EUS-guided needle-based confocal laser-endomicroscopy (nCLE);and compared the accuracy of these techniques for the detection of potentially malignant PCLs.
Research results
Now, continued the wolf, I am going to turn myself into a boat full of the most beautiful silken merchandise, and you must jump boldly into the boat, and steer28 with my tail in your hand right out into the open sea
Research conclusions
In our study,EUS-guided mFB combined with nCLE,improve malignancy detection in patients with PCLs.
Research perspectives
In conclusion,new EUS technologies such as through-the-needle techniques (direct intracystic mFB combined with nCLE),improve malignancy detection in patients with PCLs.However,multicenter,and cost-benefit studies are recommended to validate these findings.
And all this while his sister was pacing up and down the palace, hardly letting the knife out of her hand, and dreading18 what she knew she would see, and what she did see
Robles-Medranda C contributed to study conception,design,drafting;Olmos JI,Del Valle Zavala R,Nebel JA,Calle Loffredo D and Pitanga-Lukashok H contributed to study design,acquisition of data;Puga-Tejada M and Oleas R contributed to study design;Baquerizo-Burgos J,Puga-Tejada M and Oleas R contributed to study drafting,acquisition/analysis of data;Arevalo-Mora M did final database study consolidation and encryption,data acquisition;Robles-Medranda C,Olmos JI,Del Valle Zavala R,Nebel JA,Calle Loffredo D,Pitanga-Lukashok H,Puga-Tejada M,Oleas R and Arevalo-Mora M contributed to critical revision of important intellectual content;all authors did final approval of the version to be published.
“The bright warm sun shone on a little court, on the first warm day of spring. His bright beams rested on the white walls of the neighboring house; and close by bloomed the first yellow flower of the season, glittering like gold in the sun’s warm ray. An old woman sat in her arm chair at the house door, and her granddaughter, a poor and pretty servant-maid came to see her for a short visit. When she kissed her grandmother there was gold everywhere: the gold of the heart in that holy kiss; it was a golden morning; there was gold in the beaming sunlight, gold in the leaves of the lowly flower, and on the lips of the maiden. There, that is my story,” said the buttercup.
The study was approved by the Institutional Review Board of Instituto Ecuatoriano de Enfermedades Digestivas.
All study participants,and their legal guardians,provided informed written consent prior to study enrolment.
Fifty years ago there lived a king who was very anxious to get married; but, as he was quite determined1 that his wife should be as beautiful as the sun, the thing was not so easy as it seemed, for no maiden2 came up to his standard
Robles-Medranda C reports other from Pentax Medical,other from Boston Scientific,other from Steris,other from Medtronic,other from Motus,other from Micro-tech,other from G-Tech Medical Supply,other from CREO Medical,other from Mdconsgroup,outside the submitted work;The other authors declare no conflicts of interest.
The data that support the findings of this study are openly available by contacting the corresponding author.
The authors have read the STROBE Statement-checklist of items,and the manuscript was prepared and revised according to the STROBE Statement-checklist of items.
This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See:https://creativecommons.org/Licenses/by-nc/4.0/
Ecuador
Carlos Robles-Medranda 0000-0003-2434-3369;Juan I Olmos 0000-0002-8705-4233;Miguel Puga-Tejada 0000-0001-8853-0847;Roberto Oleas 0000-0001-9810-4745;Jorge Baquerizo-Burgos 0000-0002-6741-4211;Martha Arevalo-Mora 0000-0003-2561-8512;Raquel Del Valle Zavala 0000-0002-4862-7350;Joao Autran Nebel 0000-0002-0994-5161;Daniel Calle Loffredo 0000-0002-2230-0130;Hannah Pitanga-Lukashok 0000-0002-4364-1321.
Zhang H
A
Zhang H
1 Müssle B,Distler M,Wolk S,Shrikhande SV,Aust DE,Arlt A,Weitz J,Hackert T,Welsch T.Management of patients with pancreatic cystic lesions:A case-based survey.
2017;17:431-437 [PMID:28456590 DOI:10.1016/j.pan.2017.04.004]
2 Elta GH,Enestvedt BK,Sauer BG,Lennon AM.ACG Clinical Guideline:Diagnosis and Management of Pancreatic Cysts.
2018;113:464-479 [PMID:29485131 DOI:10.1038/ajg.2018.14]
3 Tanaka M,Fernández-del Castillo C,Adsay V,Chari S,Falconi M,Jang JY,Kimura W,Levy P,Pitman MB,Schmidt CM,Shimizu M,Wolfgang CL,Yamaguchi K,Yamao K;International Association of Pancreatology.International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas.
2012;12:183-197[PMID:22687371 DOI:10.1016/j.pan.2012.04.004]
4 Wu J,Wang Y,Li Z,Miao H.Accuracy of Fukuoka and American Gastroenterological Association Guidelines for Predicting Advanced Neoplasia in Pancreatic Cyst Neoplasm:A Meta-Analysis.
2019;26:4522-4536[PMID:31617119 DOI:10.1245/s10434-019-07921-8]
5 Krishna SG,Brugge WR,Dewitt JM,Kongkam P,Napoleon B,Robles-Medranda C,Tan D,El-Dika S,McCarthy S,Walker J,Dillhoff ME,Manilchuk A,Schmidt C,Swanson B,Shah ZK,Hart PA,Conwell DL.Needle-based confocal laser endomicroscopy for the diagnosis of pancreatic cystic lesions:an international external interobserver and intraobserver study (with videos).
2017;86:644-654 [PMID:28286093 DOI:10.1016/j.gie.2017.03.002]
6 Jang DK,Song BJ,Ryu JK,Chung KH,Lee BS,Park JK,Lee SH,Kim YT,Lee JY.Preoperative Diagnosis of Pancreatic Cystic Lesions:The Accuracy of Endoscopic Ultrasound and Cross-Sectional Imaging.
2015;44:1329-1333[PMID:26465956 DOI:10.1097/MPA.0000000000000396]
7 Lu X,Zhang S,Ma C,Peng C,Lv Y,Zou X.The diagnostic value of EUS in pancreatic cystic neoplasms compared with CT and MRI.
2015;4:324-329 [PMID:26643701 DOI:10.4103/2303-9027.170425]
8 Haghighi M,Sethi A,Tavassoly I,Gonda TA,Poneros JM,McBride RB.Diagnosis of Pancreatic Cystic Lesions by Virtual Slicing:Comparison of Diagnostic Potential of Needle-Based Confocal Laser Endomicroscopy versus Endoscopic Ultrasound-Guided Fine-Needle Aspiration.
2019;10:34 [PMID:31799020 DOI:10.4103/jpi.jpi_32_19]
9 Durkin C,Krishna SG.Advanced diagnostics for pancreatic cysts:Confocal endomicroscopy and molecular analysis.
2019;25:2734-2742 [PMID:31235996 DOI:10.3748/wjg.v25.i22.2734]
10 Sarno A,Tedesco G,De Robertis R,Marchegiani G,Salvia R,D'Onofrio M.Pancreatic cystic neoplasm diagnosis:Role of imaging.
2018;7:297-300 [PMID:30323156 DOI:10.4103/eus.eus_38_18]
11 Nakai Y,Iwashita T,Park DH,Samarasena JB,Lee JG,Chang KJ.Diagnosis of pancreatic cysts:EUS-guided,throughthe-needle confocal laser-induced endomicroscopy and cystoscopy trial:DETECT study.
2015;81:1204-1214 [PMID:25634486 DOI:10.1016/j.gie.2014.10.025]
12 Chen AL,Misdraji J,Brugge WR,Ferrone CR,Pitman MB.Acinar cell cystadenoma:A challenging cytology diagnosis,facilitated by moray
micro-forceps biopsy.
2017;45:557-560 [PMID:28236434 DOI:10.1002/dc.23693]
13 Napoleon B,Palazzo M,Lemaistre AI,Caillol F,Palazzo L,Aubert A,Buscail L,Maire F,Morellon BM,Pujol B,Giovannini M.Needle-based confocal laser endomicroscopy of pancreatic cystic lesions:a prospective multicenter validation study in patients with definite diagnosis.
2019;51:825-835 [PMID:30347425 DOI:10.1055/a-0732-5356]
14 Abdelkader A,Hunt B,Hartley CP,Panarelli NC,Giorgadze T.Cystic Lesions of the Pancreas:Differential Diagnosis and Cytologic-Histologic Correlation.
2020;144:47-61 [PMID:31538798 DOI:10.5858/arpa.2019-0308-RA]
15 Napoleon B,Krishna SG,Marco B,Carr-Locke D,Chang KJ,Ginès À,Gress FG,Larghi A,Oppong KW,Palazzo L,Kongkam P,Robles-Medranda C,Sejpal D,Tan D,Brugge WR.Confocal endomicroscopy for evaluation of pancreatic cystic lesions:a systematic review and international Delphi consensus report.
2020;8:E1566-E1581[PMID:33140012 DOI:10.1055/a-1229-4156]
16 Yang D,Trindade AJ,Yachimski P,Benias P,Nieto J,Manvar A,Ho S,Esnakula A,Gamboa A,Sethi A,Gupte A,Khara HS,Diehl DL,El Chafic A,Shah J,Forsmark CE,Draganov PV.Histologic Analysis of Endoscopic Ultrasound-Guided Through the Needle Microforceps Biopsies Accurately Identifies Mucinous Pancreas Cysts.
2019;17:1587-1596 [PMID:30471456 DOI:10.1016/j.cgh.2018.11.027]
17 Ritchie ME,Phipson B,Wu D,Hu Y,Law CW,Shi W,Smyth GK.limma powers differential expression analyses for RNA-sequencing and microarray studies.Nucleic Acids Res 2015;43:e47 [PMID:25605792 DOI:10.1093/nar/gkv007]
18 Erratum for the Research Article:"Integrated molecular analysis of tumor biopsies on sequential CTLA-4 and PD-1 blockade reveals markers of response and resistance" by W.Roh,P.-L.Chen,A.Reuben,C.N.Spencer,P.A.Prieto,J.P.Miller,V.Gopalakrishnan,F.Wang,Z.A.Cooper,S.M.Reddy,C.Gumbs,L.Little,Q.Chang,W.-S.Chen,K.Wani,M.P.De Macedo,E.Chen,J.L.Austin-Breneman,H.Jiang,J.Roszik,M.T.Tetzlaff,M.A.Davies,J.E.Gershenwald,H.Tawbi,A.J.Lazar,P.Hwu,W.-J.Hwu,A.Diab,I.C.Glitza,S.P.Patel,S.E.Woodman,R.N.Amaria,V.G.Prieto,J.Hu,P.Sharma,J.P.Allison,L.Chin,J.Zhang,J.A.Wargo,P.A.Futreal.
2017;9 [PMID:28404861 DOI:10.1126/scitranslmed.aan3788]
19 Palazzo M,Sauvanet A,Gincul R,Borbath I,Vanbiervliet G,Bourdariat R,Lemaistre AI,Pujol B,Caillol F,Palazzo L,Aubert A,Maire F,Buscail L,Giovannini M,Marque S,Napoléon B.Impact of needle-based confocal laser endomicroscopy on the therapeutic management of single pancreatic cystic lesions.
2020;34:2532-2540[PMID:31410626 DOI:10.1007/s00464-019-07062-9]
20 Hashimoto R,Lee JG,Chang KJ,Chehade NEH,Samarasena JB.Endoscopic ultrasound-through-the-needle biopsy in pancreatic cystic lesions:A large single center experience.
2019;11:531-540 [PMID:31798774 DOI:10.4253/wjge.v11.i11.531]
21 Wang QX,Xiao J,Orange M,Zhang H,Zhu YQ.EUS-Guided FNA for Diagnosis of Pancreatic Cystic Lesions:a Meta-Analysis.
2015;36:1197-1209 [PMID:26138881 DOI:10.1159/000430290]
22 Konda VJ,Meining A,Jamil LH,Giovannini M,Hwang JH,Wallace MB,Chang KJ,Siddiqui UD,Hart J,Lo SK,Saunders MD,Aslanian HR,Wroblewski K,Waxman I.A pilot study of in vivo identification of pancreatic cystic neoplasms with needle-based confocal laser endomicroscopy under endosonographic guidance.
2013;45:1006-1013 [PMID:24163192 DOI:10.1055/s-0033-1344714]
杂志排行
World Journal of Gastrointestinal Endoscopy的其它文章
- Z-per-oral endoscopic myotomy as definitive prevention of a bleeding ulcer in Zenker’s diverticulum:A case report
- Mucosa-associated lymphoid tissue lymphoma in the terminal ileum:A case report
- Endoscopic management and outcome of non-variceal bleeding in patients with liver cirrhosis:A systematic review
- SARS-CoV-2 in inflammatory bowel disease population:Antibodies,disease and correlation with therapy
- Ergonomics of gastrointestinal endoscopies:Musculoskeletal injury among endoscopy physicians,nurses,and technicians
- Role of intraluminal brachytherapy in palliation of biliary obstruction in cholangiocarcinoma:A brief review
