Neutrophil-to-lymphocyte ratio or platelet-to-lymphocyte ratio is a predictive factor of pancreatic cancer patients with type 2 diabetes
2022-04-29BaoDongRongRongWu
Bao Dong, Rong-Rong Wu
The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, University of Science and Technology of China, Hefei 230031, China
TotheEditor:
Pancreatic cancer (PC) is one of the most deadly cancers due to the difficulty of its early diagnosis. Most patients have developed an unresectable PC when diagnosed [1] . According to GLOBOCAN 2018 estimates, PC ranked the 11th most common cancer in the world counting 458 918 new cases and causing 432 242 deaths (4.5% of all deaths caused by cancer) in 2018 [2] .
Type 2 diabetes (T2D) is one of the most common comorbidi- ties in cancer patients, particularly those with PC. Previous stud- ies showed that the survival rate of PC patients with short-term T2D was similar to that of non-diabetic patients, while PC pa- tients with long-term T2D had worse survival than non-diabetic patients [ 3 , 4 ]. Therefore, early detection and treatment are of crit- ical importance. Carbohydrate antigen 19-9 (CA19-9) is an estab- lished PC biomarker, but it is not sensitive enough to detect PC at the early stage [5] . Histology is confirmative diagnosis, but it is dif- ficult to obtain tumor tissue. In order to improve the prognosis of PC patients with T2D, it is urgent to develop new biomarkers that can detect early PC with T2D.
Recently, several studies have shown that inflammatory path- ways may play an important role in tumorigenesis and metasta- sis [ 6 , 7 ]. However, reports on the predictive value of neutrophil- to-lymphocyte ratio (NLR) or platelet-to-lymphocyte ratio (PLR) in PC with T2D are few [8] . As NLR and PLR are derived from rou- tine blood tests, they are easy to obtain and may play important roles in monitoring PC with T2D progression. Thus, we performed this study to evaluate the diagnostic value of NLR and PLR in PC patients with T2D.
In this study, all data were derived from the electronic medical records of the First Affiliated Hospital of USTC. The study popu- lation were divided into three groups: PC patients with T2D, pa- tients with T2D alone, and healthy controls. Demographic informa- tion and the results of laboratory examinations were collected be- fore the surgery, including sex, age, CA19-9 levels and blood cell counts (neutrophil, lymphocyte, and platelet counts).
The inclusion criteria were as follows: (i) PC patients with no chemotherapy or radiotherapy before the surgery; (ii) PC con- firmed by preoperative biopsy or postoperative pathology.
The exclusion criteria were: (i) patients with a previous history of cancer or an active infectious disease; (ii) patients had severe bleeding; (iii) aged<20 years, or with incomplete demographic information.
All statistical analyses were conducted using SPSS 23.0 (SPSS Inc., Chicago, IL, USA). Differences between groups were analyzed by Student’st-test or one-way analysis of variance (ANOVA) for continuous variables and Chi-square test for categorical variables. Moreover, areas under receiver operating characteristic (AUC) curves were determined for variables to identify the predictors of PC patients with T2D. Two-sidedPvalues less than 0.05 were con- sidered statistically significant.
The socio-demographic characteristics of study population were illustrated in Table 1 . Our study included 46 PC patients with T2D (18 females, 28 males), 50 patients (19 females, 31 males) with T2D alone, and 50 healthy controls (10 females, 40 males). The mean age of the PC patients with T2D, patients with T2D alone, and healthy controls was 61 ± 10, 60 ± 9 and 63 ± 6 years, respectively. There was no significant difference between the three groups concerning sex and age (P>0.05).
PC patients with T2D had significantly higher neutrophil counts, NLR and PLR compared to patients with T2D alone and healthy controls, but there were no significant differences in platelet counts between PC patients with T2D and patients with T2D alone, healthy controls. In addition, the lymphocyte counts were found to be significantly lower in the PC patients with T2D compared to pa- tients with T2D alone and healthy controls ( Table 1 ).
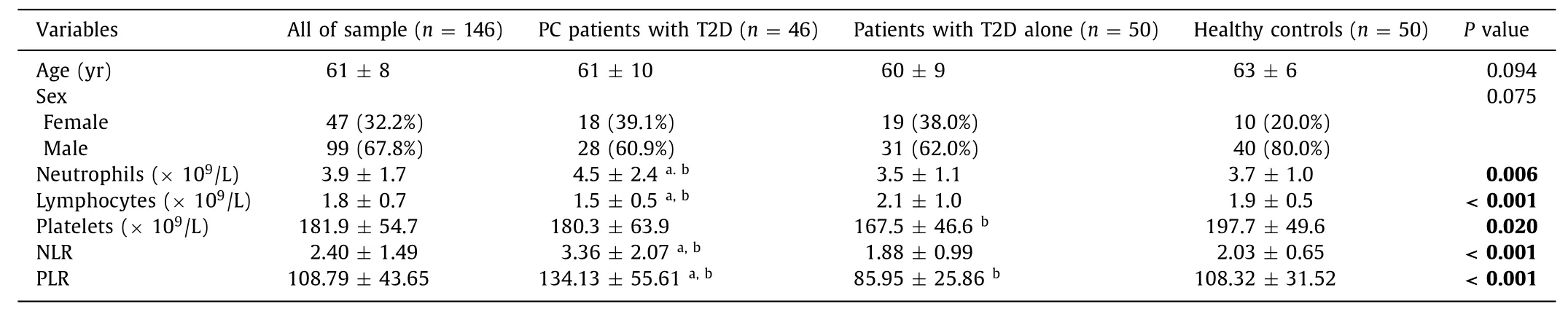
Table 1 Socio-demographic and clinical characteristics of PC patients with T2D.
According to the receiver operating characteristic (ROC) curve, with the cutoff value of 2.06, NLR showed the sensitivity and specificity of the test for PC patients with T2D as 84.8% and 71.0%, respectively (AUC: 0.788, 95% CI: 0.706–0.870,P<0.001); with the cutoff value of 126.42, PLR showed the sensitivity and specificity of the test for PC patients with T2D as 50.0% and 84.0%, respectively (AUC: 0.706, 95% CI: 0.612–0.800,P<0.001) ( Fig. 1 ).
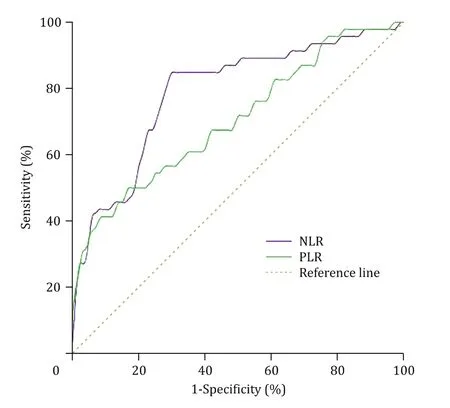
Fig. 1. Receiver operating characteristic curve analysis for PC with T2D according to the preoperative NLR and PLR. PC: pancreatic cancer; T2D: type 2 diabetes; NLR: neutrophil-to-lymphocyte ratio; PLR: platelet-to-lymphocyte ratio.
Systemic inflammation and immune response play key roles in cancer cell growth. NLR and PLR are inflammatory biomarkers. El- evated NLR and PLR have been associated with poor prognosis and poor response to chemotherapy in patients with multiple malig- nancies [9] . In this study, we found that NLR and PLR of PC patients with T2D were higher compared to patients with T2D alone and healthy controls. Details of the mechanisms underlying the pre- dictive value of NLR and PLR are not entirely understood. As an inflammatory cell, neutrophil plays an important role in the de- velopment of tumor by producing a variety of cytokines, such as oncostatin-M receptor, interleukin-6, hepatocyte growth factor, and tumor necrosis factor [10] . These factors can increase tumor cell invasion and metastasis and help the cells escape immune surveil- lance. In addition, platelets can be in direct contact with circulating tumor cells, which promotes the extravasation of tumor cells to the site of metastasis [11] . On the other hand, lymphocyte is an impor- tant factor in suppressing cancer progression and development by inducing cytotoxic cell death [12] .
In this study, NLR and PLR were predictive markers of PC pa- tients with T2D. A study showed that carcinoembryonic antigen level above 30 ng/mL in the pancreatic juice was an independent factor associated with malignancy [13]. However, sampling of fluid in pancreatic juice using routine endoscopic retrograde cholan- giopancreatography and endoscopic ultrasound-guided fine needle aspiration were more invasive with dissemination risk [14] . In ad- dition, the NLR and PLR are inexpensive, readily available and less invasive. Therefore, NLR and PLR should be considered, like com- mon tumor markers, before planning invasive examinations for PC patients with T2D.
Several limitations should been taken into consideration. First, the sample size was relatively small and the study objects came from the same hospital, which may affect the representativeness of the sample. Second, this was a retrospective study lacking lon- gitudinal observation.
In conclusion, results of this study suggested that PC patients with T2D had significantly higher NLR and PLR compared to pa- tients with T2D alone and healthy controls. Moreover, NLR and PLR are derived from routine blood tests, inexpensive, readily avail- able, and less invasive, suggesting that the preoperative NLR and PLR may be useful predictive biomarkers for evaluating PC patients with T2D.
Acknowledgments
None.
CRediTauthorshipcontributionstatement
BaoDong:Data curation, Formal analysis, Writing - original draft.Rong-RongWu:Conceptualization, Methodology, Writing - review & editing.
Funding
None.
Ethicalapproval
Not needed.
Competinginterest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the sub- ject of this article.
杂志排行
Hepatobiliary & Pancreatic Diseases International的其它文章
- Meetings and Courses
- Information for Readers
- NAFLD or MAFLD: That is the conundrum
- Relevant Content
- Nanosecond pulsed electric field interrupts the glycogen metabolism in hepatocellular carcinoma by modifying the osteopontin pathway
- Isolated pancreatic metastasis from a malignant pleural mesothelioma diagnosed using endoscopic ultrasonography-guided fine needle aspiration biopsy