Preoperative laser reduces silicone oil use in primary diabetic vitrectomy
2022-04-19WenBinZhengXiaoHuDingKunBeiLaiJiZhuLiYuQingWuYuanMaZiYeChenShiDaChenSaiNanXiaoBingQianLiuYingLinTaoLi
INTRODUCTION
Diabetic retinopathy (DR) is the leading ocular complication of diabetes which cause irreversible blindness in working-age adults worldwide
. Approximately 25% of vision loss in DR patients is a result of severe complications of advanced proliferative diabetic retinopathy(PDR)
. Due to the aging population and the increasing prevalence of diabetes, the number of people suffering visionthreatening PDR has significantly increased in recent years
.Pan-retinal photocoagulation (PRP), which prevents the disease progression and reduces the risk of severe visual impairment by 50%, has been the standard treatment of high-risk PDR for decades
. However, in our experience, several patients miss the best time for laser photocoagulation treatment for various reasons and progress to severe PDR-related complications that require vitrectomy surgery. It was reported that 5.6%of patients progress to severe PDR and require a vitrectomy despite having received adequate PRP
.
Vitrectomy has been established as the ultimate treatment of severe PDR-related complications and silicone oil has been used as an effective endotamponade agent that increases the success rate of complicated cases undergoing vitrectomy
.However, once silicone oil is used as intraocular tamponade agent, a subsequent surgery for removal is required. It also brings some disadvantages, such as the progression of nuclear cataracts, poor vision prognosis, increased economic burden and may lead to other postoperative complications
. Having a clearer understanding of the risk factors of silicone oil tamponade in vitrectomy for PDR-related complications might provide novel and more effective preventive strategies. Thus,it is critical to understand the predictive factors of silicone oil tamponade in vitrectomy for PDR-related complications.However, although clinically relevant, the related factors of using silicone oil as intraocular tamponade agent during diabetic vitrectomy still unknown.
Protocol of this cross-sectional, retrospective study was reviewed and approved by the Medical Ethics Committee at Zhongshan Ophthalmic Centre (ZOC) of Sun Yat-sen University (2021KYPJ094). As this was a retrospective study, patient informed consent was waived. The study adhered to the Helsinki Declaration (2008).
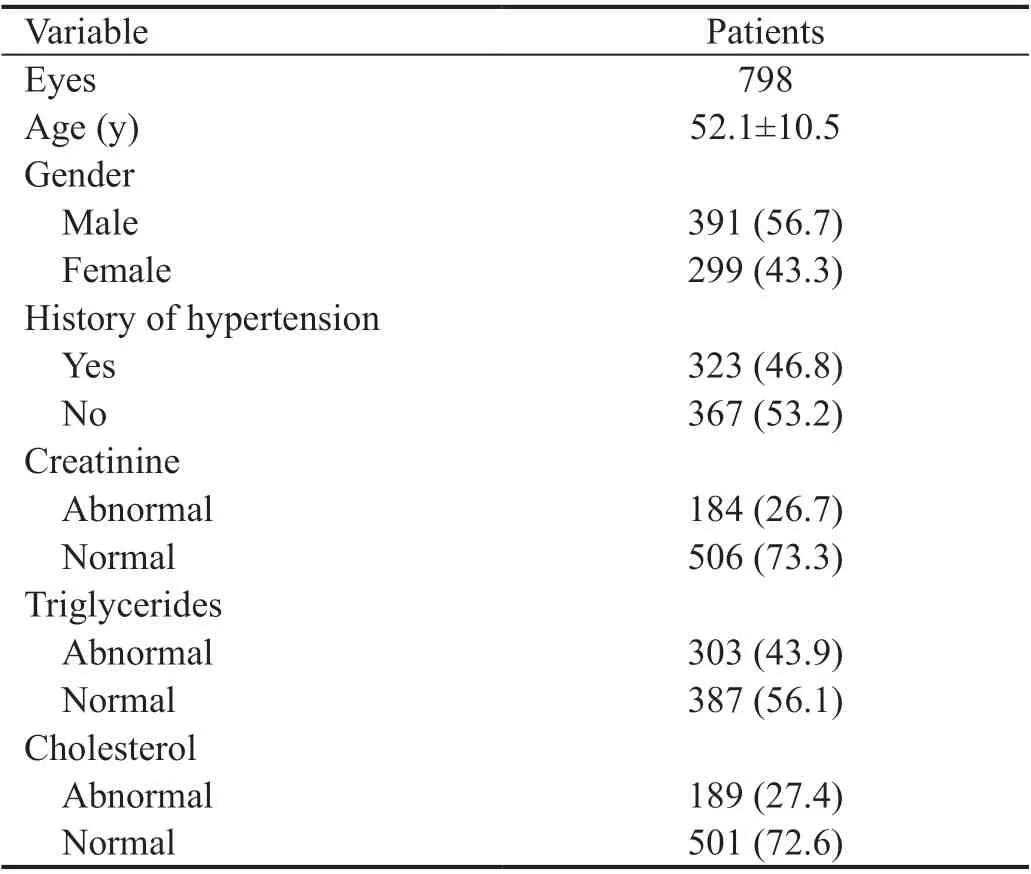
The mean patient age at surgery was 52.1±10.5y (range: 18-85y),79 patients (11.4%) were under 40y of age and 158 (20%) were at least 60 years old. Demographics and clinical characteristics of the patients were showed in Table 1.
SUBJECTS AND METHODS
60例自2015年1月—2017年1月收治的肝脏核磁共振检查患者作为分析样本,以护理路径为前提,分为两组。基础组30例,患者男女比18:12,年龄23~80岁,平均(51.52±10.36)岁,文化程度:初中10例,高中9例,大专以上11例。分析组30例,患者男女比19:11,年龄24~80,平均(52.07±10.39)岁,文化程度:初中11例,高中10例,大专以上9例。对比组间数据,不统计学价值。
(1)课程结束后,进行考核。理论考核根据教学大纲统一命题,统一试卷,统一评分标准;操作考核统一操作要求和评分标准,考核成绩采用百分制。
Preoperative anti-VEGF combined with PRP therapy was performed in 191 eyes (23.8%),preoperative anti-VEGF without prior PRP in 387 eyes(48.6%), preoperative PRP treatment alone in 62 eyes (7.8%)and 158 eyes (19.8%) received no adjuvant pretreatment. One hundred and forty-four out of the 798 eyes (18.1%) underwent at least three sessions of PRP.
很多时候,人们的一些过失行为会导致电力电缆的损坏。这是由于电缆在布置的过程中,有的工作人员由于粗心或者操作方法不当,导致其发生扭曲或者被折,造成了电缆线的损坏,随着使用时间的增长,将会影响电网的正常运行。
A standard three-port 23G or 25G parsplana vitrectomy (PPV) was peformed for non-clearing VH,traction retinal detachment (TRD), combined traction and rhegmatogenous retinal detachment (TRRD), or combined VH and RD with a wide-angle viewing system in all the patients.All surgeries were conducted by one of six experienced vitreoretinal specialists, each with more than five years of experience performing vitreoretinal surgery. Intravitreal anti-vascular endothelial growth factor (VEGF) drugs(ranibizumab, aflibercept or conbercept) were administrated 3-7d prior to surgery for active neovascularization (NV) or VH at the surgeon's discretion. The blood or opacified vitreous was cleared, vitreoretinal traction was released, and fibrovascular membrane were removed. Laser was applied for retinal breaks and PRP was used in patients who had not previously undergone laser photocoagulation or in patients in whom previous laser photocoagulation was insufficient. Combined phacomusification was performed as indicated. Whether the intraocular lens was implanted at the same time depends on the fundus status. Endotamponade was achieved using the balanced salt solution, air or silicone oil, mainly according to the status of the retina at the end of the surgery. However, the patient's general condition and visual acuity of the opposite eye were also taken into consideration as silicone oil filling indicators. Balanced salt solution was used as endotamponade in case of no retinal tears was observed. Air endotamponade was used in case of within two retinal tears in a superior location. Silicone oil (5000 mPa.s; RT SIL-OL 5000; Zeiss,Berlin, Germany) was used in case of inferior retinal tears,large and more than two retinal tears, or fibrovascular membrane that could not be cleaned completely. Silicone oil removal was performed at least three months postoperative.Cataract surgery was performed when the lens opacity affects the observation of the fundus.
The medical and surgical data of the patients were retrospectively collected
the electronic medical record system. The preoperative data included patient demographics, duration of symptoms, best-corrected visual acuity, fasting blood glucose, serum cholesterol, triglycerides,serum creatinine, blood urea nitrogen, history of hypertension,use of anti-VEGF agents prior to vitrectomy, and previous treatments for DR (including local laser, PRP and vitrectomy).The operative and postoperative data collected for this study included intraocular tamponade used at the end of the surgery and recurrence of VH or RD that required subsequent surgeries.
The
statistical analyses were performed with SPSS version 25 (IBM, North Castle, NY, USA).
<0.05 was considered statistical significant. Variables were calculated using basic descriptive statistics, normally distributed continuous variables were presented as mean±standard deviation; nonnormally distributed continuous variables were presented as the median. Categorical variables were presented as number and percentage. A binary Logistic regression test was performed to identify risk factors associated with the use of silicone oil tamponade at the end of vitrectomy.
RESULTS
The aim of the present study was to identify the predictive factors for silicone oil tamponade during primary diabetic vitrectomy. In addition, the clinical characteristics of patients who underwent PPV for PDR-related complications, preoperative treatments and duration of symptoms, were also assessed.
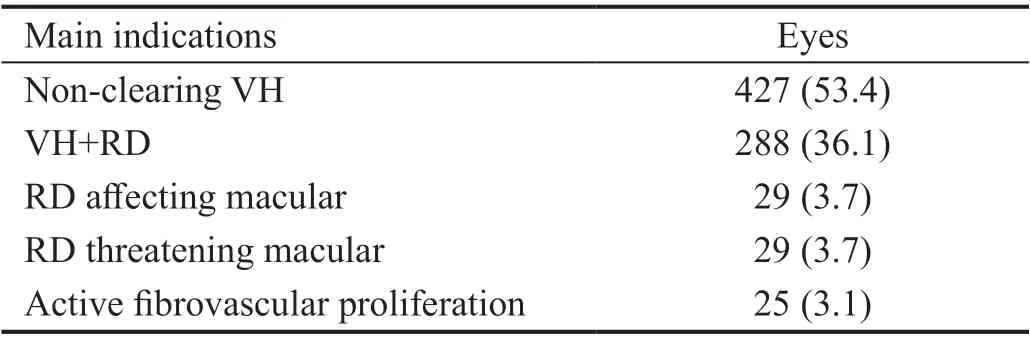
The main indication for primary diabetic vitrectomy surgery was non-clearing VH, followed by VH combined with RD, RD affecting macular, RD threatening macular, and active fibrovascular proliferation (Table 2).
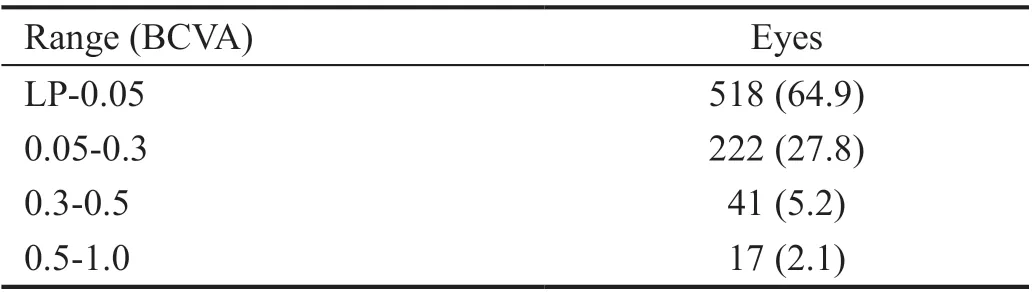
The preoperative corrected Snellen visual acuity of most patients undergoing surgery was <0.05,while 58 eyes (7.3%) had visual acuity >0.3 before surgery (Table 3).
“天脊化肥专营店”是天脊集团市场深耕终端发力的“桥头堡”。天脊集团以基层网络建设为重要抓手,把“给政策”扭转到“教技能”上来,积极推进重点门店向天脊化肥专营店发展升级。今年验收通过200家,在三年内至少建成1000家以上天脊化肥专营店,让其成为农民丰收交流、科学种田案例示范、增产增效成果分享、农民致富亲身体验的“新时代天脊助力乡村振兴喜悦舞台”。
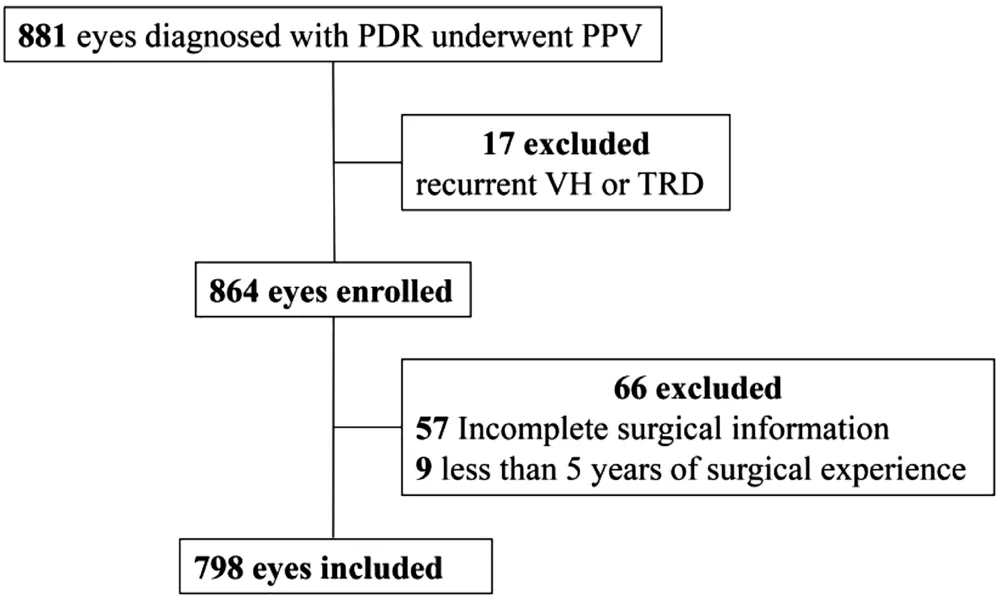
Medical and surgical records of all vitrectomy surgeries at the fundus surgery centre of ZOC from 1 January 2018 to 31 December 2018 were identified and reviewed in the electronic medical record system. A total of 881 consecutive cases of vitrectomy were identified.Patients who underwent primary vitrectomy for PDR-related complications were enrolled. Patients undergoing a secondary vitrectomy for recurrent vitreous haemorrhage (VH) or recurrent retinal detachment (RD), patients with incomplete medical or surgical records, and vitrectomies performed by surgeons with less than five years of experience were excluded from this analysis. The final analysis included 690 consecutive patients (798 eyes; Figure 1).
Nevertheless, Antoszyk
reported that anti-VEGF alone was not inferior to vitrectomy with PRP in the treatment of VH from PDR in the primary outcome of visual acuity over 6mo following initial treatment; however, vitrectomy surgery, which involves the removal of pathological vitreous and clearance of hemorrhage and scarring tissues relieving vitreoretinal traction,remains the cornerstone of treatment for late complications of PDR, even in patients with a history of optimal laser photocoagulation and other medical therapies
. The current surgical concept and techniques used in vitrectomies have dramatically advanced since the surgery reported by Diabetic Retinopathy Vitrectomy Study (DRVS)
, characterizing by the increased use of smaller gauge vitrectomy systems,application of wide-angle viewing system, injection of silicone oil to aid retinal reattachment in complicated cases, and widespread use of anti-VEGF adjuvant therapy for severe PDR-related complications
.
由表1可知,白泥的主要成分是SiO2和Al2O3,其含量分别高达68.46%和12.98%,二者通过碱液浸出获得可溶性硅源和铝源,能够替代传统分子筛合成过程中需要的化工原料。
相关研究表明,当地下水动力条件改变时,原来被堵塞的洞隙及其相连的下部排水通道复活,重新成为地下水集中活动的地段;地下水位上升,抗水性差的土强烈崩解,一部分顺喇叭口落入溶洞中,初步形成上覆土层的土洞;土洞进一步扩大,向地表发展,顶板渐薄,当顶板薄到不能支撑上部土层重量时,便突然发生塌落。
Vitrectomy was combined with phacoemulsification in 26 eyes (3.3%), and one eye (<1%) received combined sclera encircling surgery.The most frequent surgical complications during the oneyear follow up period were recurrent RD and recurrent VH.Twenty-nine eyes (3.6%) required reoperation, including 19(2.4%) for stubborn recurrent VH and 10 (1.2%) for recurrent RD. Six eyes (<1%) developed neovascular glaucoma (NVG)after vitrectomy and underwent shunting device implantation surgery. No patient experienced endophthalmitis and no serious systemic complications occurred after surgery.
During the one-year follow-up period, 201 out of the 313 silicone oil eyes (64.2%) underwent surgery to remove the silicone oil.Ninety-six eyes (30.7%) in the silicone oil tamponade group underwent cataract surgery compared to 19 out of 485 eyes(3.9%) in the non-silicone oil tamponade group (
<0.01).
DISCUSSION
The demographic and clinical characteristics of Chinese patients who underwent PPV for PDR-related complications were explored in this study. Silicone oil tamponade rate was high although anti-VEGF agents were widespread administrated prior to diabetic vitrectomy. Moreover, we identified that the lack of preoperative laser treatment was the main reason for the high silicone oil tamponade rate during primary diabetic vitrectomy. Thus, in the anti-VEGF era for DR management, PRP still plays an important role and should not be ignored.
This study reviewed a large number of Chinese patients who underwent PPV for severe PDR-related complications. As digital data collection is increasing, the use of database studies to document clinical outcomes in real-world settings is also increasing
. The data used in this study were collected from the electronic medical record system, which represented the patients encountered daily by physicians. Although the results of randomised controlled studies are considered as the highest level of clinical evidence, real-world research results are valuable and applicable.
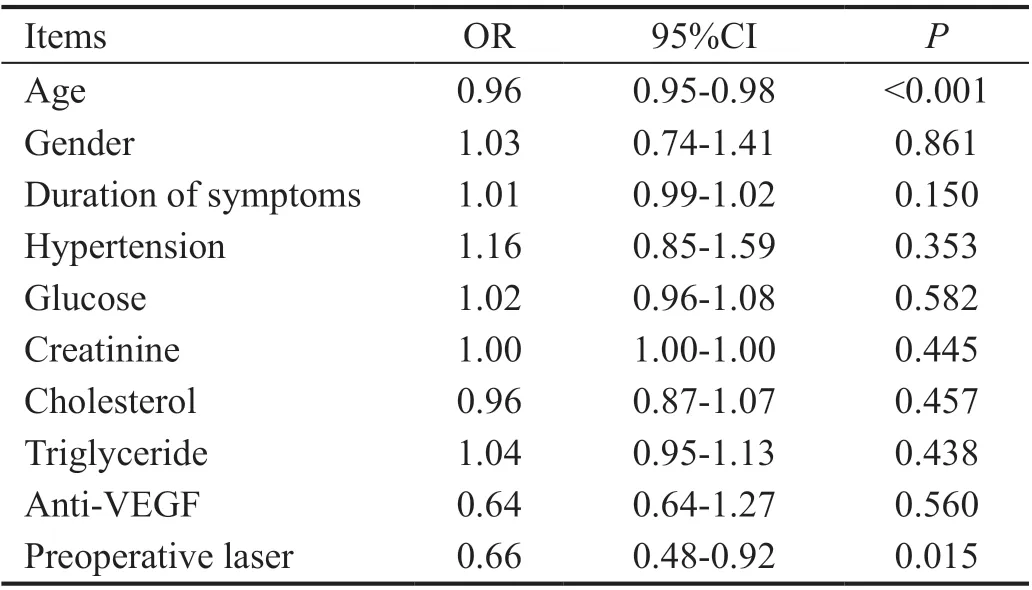
Silicone oil was used as an intraocular tamponade agent in 313 eyes(39.2%). The silicone oil tamponade ratio of the RD group was 69.4% (240/346); the non-RD group was 16.1% (73/452),and by preforming Chi-square test,
<0.001. Preoperative photocoagulation treatment [odds ratio (OR)=0.66, 95%confidence interval (CI)=0.48-0.92,
=0.015] and younger age [OR=0.96, 95%CI=0.95-0.98,
<0.001) were identified as protective factors against the use of silicone oil tamponade during primary vitrectomy for PDR-related complications,while preoperative anti-VEGF therapy did not affect the choice of silicone oil as endotamponade agent (OR=0.64;95%CI=0.64-1.27;
=0.560; Table 4).
Few studies reported the baseline characteristics and trends of preoperative treatments in Chinese patients undergoing diabetic vitrectomy. In our study, the mean age of the patients at surgery was 52y and the most frequent indication for diabetic vitrectomy was non-clearing VH. In one of the largest previously-published studies with a series of 890 consecutive patients regarding vitrectomy for PDR-associated complications, the mean age was 51.9y and the most common indications for vitrectomy were TRD (36.6%) and persistent VH (35.4%)
. Our results are also consistent with those of the Early Treatment Diabetic Retinopathy Study (ETDRS)
.Few studies regarding the preoperative visual acuity of patients with PDR undergoing vitrectomy have been reported. One previous study reported that 11.9% of eyes had visual acuity≥0.1 at baseline
, while 24.8% of eyes in our study had a preoperative visual acuity >0.1, including 7.3% of eyes with a preoperative visual acuity >0.3. The threshold for performing vitrectomy for patients with PDR has decreased as a result of the advancement of the modern PPV technique, the application of adjuvant therapies, and advances in the management of these patients.
姜夔词素以清空峭拔称名,其中《点绛唇·燕雁无心》更是白石词风的代表杰作,抒发了词人对身世的感慨嗟叹。在《点绛唇》中,关于首句“燕雁无心”一直有不同的释义:《全宋词》中,注释“燕雁”为“自北方飞来之雁”;《唐宋词鉴赏辞典》中,释“燕雁”为“北来之雁”;《唐宋词选释》中,俞平伯先生注:“‘燕雁’有两说:一.‘燕’指玄鸟。仄声。二.燕为地名,幽燕之燕,平声”……在当下学术论文中,也有两种释义的偏倚。那么到底是“北地之雁”?还是“燕与大雁”?究其原词,我们或可得解。
Preoperative anti-VEGF and PRP treatments are common for patients with PDR, which are closely related to the postoperative prognosis
. The adjuvant intravitreal injection of anti-VEGF drugs was first reported in 2006 for the preoperative treatment of patients with PDR with active proliferation
,which made the procedure significantly less challenging,diminished intraoperative iatrogenic complications, and reduced intra- and postoperative bleeding
. In our study, 72%of the eyes received preoperative anti-VEGF treatment and 2.1% of the eyes underwent re-vitrectomy due to recurrent VH within the first postoperative year. The re-vitrectomy rate in our study is significantly lower than previously reported rates of 10.4%-23%
. These differences may be due to a relatively higher rate of preoperative anti-VEGF treatment in our study compared with other studies, which ranged from 17%-53.8%
.
Previous studies have reported that preoperative laser treatment improves visual prognosis and reduces the risk of recurrent bleeding after surgery
. It seems to be the common sense for vitreoretinal surgeons that preoperative laser treatment helps avoid intraoperative complications and reduce the use of silicone oil at the end of the surgery. However, our results provide exact data reference for this conclusion. In this study,only 30% of the eyes underwent PRP treatment prior to surgery, which is significantly less than previously reported PRP rates of 56.8%-83%
. These differences may be due to the poor accessibility to or awareness of regular DR screening and timely laser treatment in Chinese patients with diabetes
. Ophthalmologists and public health policymakers in China should be made aware of these results as China has the largest diabetes mellitus and DR population in the world
.Silicone oil infusion significantly improves the surgical success rate and postoperative visual acuity in complicated cases
; however, its use will inevitably increase the number of operations and postoperative complications, especially postoperative nuclear cataracts
. Iatrogenic injuries should be avoided during DR surgery to reduce the use of silicone oil. The silicone oil tamponade rate was 40% in our study,which was significantly higher than previously reported rates of 5.2%-24.4%
. The higher rate may be attributed to the large number of more serious cases included in this study.The lack of preoperative laser photocoagulation treatment and older age were identified as independent risk factors for the use of silicone oil as endotamponade in this study. The lack of prior PRP treatment may increase the risks of proliferative reticulum and intraoperative iatrogenic holes
. In our study,the preoperative laser treatment ratio was only 30%, which may explain the high ratio of patients who underwent silicone oil infusion.
Several original studies and Meta-analysis have showed that anti-VEGF pretreatment could shorten operation duration,easy the procedure, reduce intraoperative and postoperative complications and even spare the need for postoperative retinal photocoagulation sometimes
. However, controversies regarding the impact of preoperative anti-VEGF drugs on the risk of TRD in eyes with PDR and the use of silicone oil as intraocular tamponade agent in primary diabetic vitrectomy still exist. According to a recent review, the progression to TRD following intravitreal anti-VEGF therapy was noted from 1.5% to 18.4% in different studies, especially common in patients with increased severity of DR with fibrosis
. On the contrary, another study showed that anti-VEGF therapy for PDR does not increase the risk of TRD in eyes with PDR similar to those enrolled in the DRCR.net protocols for which prompt vitrectomy was not planned
. Moreover, Uzel
reported that preoperative anti-VEGF can reduce the use of silicone oil tamponade at the end of surgery in patients undergoing PPV for diabetic TRD. Recently, Chen
evaluated the effects of preoperative ranibizumab intravitreal injection on vitrectomy in patients aged less than 40 years old with PDR-related complications, the results showed that the use of silicone oil tamponade were not affected by preoperative anti-VEGF treatment but affected by the severity of DR. A Meta-analysis also revealed that no significant difference existed between sham control group and preoperative anti-VEGF injection group in reducing the rate of silicone oil tamponade
. In this study, the use of preoperative anti-VEGF was not associated with the choice of using silicone oil as intraocular tamponade agent, which may be attributed to the fact that most patients with aggressive conditions received injections and the treatment makes no significant difference in patients with mild conditions. Our results also support the concept that the incidence of use of silicone oil tamponade were not affected by preoperative anti-VEGF injection.
This study included a relatively large sample size and consecutive primary vitrectomy data from a single tertiary centre during a one-year period, reflecting the current management of PDR-related complications in China. Surgeries performed by inexperienced surgeons were excluded from this study to reduce external causes of variability. However, this study has some limitations. The retrospective nature of the study did not allow for the standardization of the measurements, and loss to long-term follow-up may have resulted in the underor overestimation of the reported outcomes. For example,patients with mild recurrence of VH after surgery that did not require reoperation were not recorded as having recurrent VH. Moreover, some important factors such as: the severity of PDR, the level of glycated haemoglobin, the duration of diabetes and the type of diabetes that may affect the choice of tamponade during the surgery was missing and failed to be evaluated in the present study. And even the patient's general condition and visual acuity of the opposite eye are relevant to the use of silicone oil. Those factors relevant to silicone oil use can be further evaluated.
错误分析理论的语言学基础是转换生成法体系,这一体系认为人脑天生具有语言习得机制与语言使用能力,从而使得人类具有了其他物种所无法拥有的完备的语言体系。而由于语言的使用往往存在一定的规则,并且主观影响较大,因此错误分析理论的心理学基础就是语言迁移理论。而语言迁移理论的核心观点则是母语的性质会使外语学习的某些方面变得容易或困难,即语言迁移有正负之分。由于受到汉语语义以及表达顺序的影响,在口译的过程中,许多学生往往来不及思考正确的英文语序,而是顺着汉语语序翻译所听到的句子,从而使句子的表达不符合英语语言习惯。例如:
In conclusion, the lack of preoperative laser treatment was identified as a significant predictive factor of silicone oil tamponade at the end of primary PDR vitrectomy. Although preoperative anti-VEGF therapy can reduce the time and difficulty of the diabetic vitrectomy procedure, it cannot reduce the rate of silicone oil tamponade. Thus, even in the anti-VEGF era, PRP should not be ignored for the treatment of PDR. The results could be served as a reference for the evaluation and management of patients with PDR.
The authors thank Chen Ning from the medical record statistics department of ZOC for her help in organizing the medical records.
Supported by the National Natural Science Foundation of China (No.82070972); the Natural Science Foundation of Guangdong Province (No.2019A1515011347);the grants from the Guangdong Province High-level Hospital Construction Program (No.303020103); the Key Science&Technology Project of Guangzhou (No.202103000045).
None;
None;
None;
None;
None;
None;
None;
None;
None;
None;
None;
None.
1 Cheung N, Mitchell P, Wong TY. Diabetic retinopathy.
2010;376(9735):124-136.
2 Yau JWY, Rogers SL, Kawasaki R,
. Meta-Analysis for Eye Disease(META-EYE) Study Group. Global prevalence and major risk factors of diabetic retinopathy.
2012;35(3):556-564.
3 Saeedi P, Petersohn I, Salpea P, Malanda B, Karuranga S, Unwin N,Colagiuri S, Guariguata L, Motala AA, Ogurtsova K, Shaw JE, Bright D, Williams R, Committee IDFDA. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045:results from the International Diabetes Federation Diabetes Atlas, 9
edition.
2019;157:107843.
4 Early photocoagulation for diabetic retinopathy. ETDRS report number 9. Early Treatment Diabetic Retinopathy Study Research Group.
1991;98(5 Suppl):766-785.
5 Flynn HW Jr, Chew EY, Simons BD, Barton FB, Remaley NA,Ferris FL 3rd. Pars plana vitrectomy in the Early Treatment Diabetic Retinopathy Study. ETDRS report number 17. The Early Treatment Diabetic Retinopathy Study Research Group.
1992;99(9):1351-1357.
6 Castellarin A, Grigorian R, Bhagat N, del Priore L, Zarbin MA.Vitrectomy with silicone oil infusion in severe diabetic retinopathy.
2003;87(3):318-321.
7 Aaberg TM. Pars plana vitrectomy for diabetic traction retinal detachment.
1981;88(7):639-642.
8 Flaxel CJ, Adelman RA, Bailey ST, Fawzi A, Lim JI, Vemulakonda GA, Ying GS. Diabetic retinopathy preferred practice pattern
.
2020;127(1):P66-P145.
9 Parikh HA, Kalbag NS, Zarbin MA, Bhagat N. Characteristics,demographics, outcomes, and complications of diabetic traction retinal detachments treated with silicone oil tamponade.
2016;26(5):497-502.
10 Jabbour E, Azar G, Antoun J, Kourie HR, Abdelmassih Y, Jalkh A. Incidence and risk factors of ocular hypertension following pars plana vitrectomy and silicone oil injection.
2018;240(3):129-134.
11 Morphis G, Irigoyen C, Eleuteri A, Stappler T, Pearce I, Heimann H.Retrospective review of 50 eyes with long-term silicone oil tamponade for more than 12 months.
2012;250(5):645-652.
12 Kohanim S, Sternberg P Jr. Ophthalmic patient data registries: defining and improving quality and outcomes.
2014;121(3):619-621.
13 Antoszyk AN, Glassman AR, Beaulieu WT, Jampol LM, Jhaveri CD, Punjabi OS, Salehi-Had H, Wells JA 3rd, 3rd M, Stockdale CR, Martin DF, Sun JK, Network DRCRR. Effect of intravitreous aflibercept
vitrectomy with panretinal photocoagulation on visual acuity in patients with vitreous hemorrhage from proliferative diabetic retinopathy: a randomized clinical trial.
2020;324(23):2383-2395.
14 Iyer SSR, Regan KA, Burnham JM, Chen CJ. Surgical management of diabetic tractional retinal detachments.
2019;64(6):780-809.
15 Early vitrectomy for severe vitreous hemorrhage in diabetic retinopathy.Two-year results of a randomized trial. Diabetic Retinopathy Vitrectomy Study report 2. The Diabetic Retinopathy Vitrectomy Study Research Group.
1985;103(11):1644-1652.
16 Stewart MW, Browning DJ, Landers MB. Current management of diabetic tractional retinal detachments.
2018;66(12):1751-1762.
17 Choovuthayakorn J, Khunsongkiet P, Patikulsila D, Watanachai N, Kunavisarut P, Chaikitmongkol V, Ittipunkul N. Characteristics and outcomes of pars plana vitrectomy for proliferative diabetic retinopathy patients in a limited resource tertiary center over an eightyear period.
2019;2019:9481902.
18 Ramezani A, Ahmadieh H, Rozegar A, Soheilian M, Entezari M,Moradian S, Dehghan MH, Nikkhah H, Yaseri M. Predictors and outcomes of vitrectomy and silicone oil injection in advanced diabetic retinopathy.
2017;31(3):217-229.
19 Zhao XY, Xia S, Chen YX. Antivascular endothelial growth factor agents pretreatment before vitrectomy for complicated proliferative diabetic retinopathy: a meta-analysis of randomised controlled trials.
2018;102(8):1077-1085.
20 Chen E, Park CH. Use of intravitreal bevacizumab as a preoperative adjunct for tractional retinal detachment repair in severe proliferative diabetic retinopathy.
2006;26(6):699-700.
21 Khuthaila MK, Hsu J, Chiang A, DeCroos FC, Milder EA, Setlur V,Garg SJ, Spirn MJ. Postoperative vitreous hemorrhage after diabetic 23-gauge pars plana vitrectomy.
2013;155(4):757-763.e1-e2.
22 Kaidonis G, Hassall MM, Phillips R, Raymond G, Saha N, Wong GH, Gilhotra JS, Liu E, Burdon KP, Henderson T, Newland H, Lake SR, Craig JE. Visual outcomes following vitrectomy for diabetic retinopathy amongst Indigenous and non-Indigenous Australians in South Australia and the Northern Territory.
2018;46(4):417-423.
23 Schreur V, Brouwers J, van Huet RAC, Smeets S, Phan M, Hoyng CB,de Jong EK, Klevering BJ. Long-term outcomes of vitrectomy for proliferative diabetic retinopathy.
2021;99(1):83-89.
24 Chen TT, Jin L, Zhu WH, Wang CY, Zhang GS, Wang XQ, Wang J,Yang K, Cochrane GM, Lamoureux EL, Friedman DS, Gilbert S,Lansingh VC, Resnikoff S, Zhao JL, Xiao BX, He MG, Congdon N. Knowledge, attitudes and eye health-seeking behaviours in a population-based sample of people with diabetes in rural China.
2021;105(6):806-811.
25 Xu Y, Wang LM, He J, Bi YF, Li M, Wang TG, Wang LH, Jiang Y,Dai M, Lu JL, Xu M, Li YC, Hu N, Li JH, Mi SQ, Chen CS, Li GW,Mu YM, Zhao JJ, Kong LZ, Chen JL, Lai SH, Wang WQ, Zhao WH, Ning G, China Noncommunicable Disease Surveillance Group 2010. Prevalence and control of diabetes in Chinese adults.
2013;310(9):948-959.
26 Ostri C, Lux A, Lund-Andersen H, la Cour M. Long-term results,prognostic factors and cataract surgery after diabetic vitrectomy: a 10-year follow-up study.
2014;92(6):571-576.
27 Gupta B, Wong R, Sivaprasad S, Williamson TH. Surgical and visual outcome following 20-gauge vitrectomy in proliferative diabetic retinopathy over a 10-year period, evidence for change in practice.
(
) 2012;26(4):576-582.
28 Uzel MM, Citirik M, Ilhan C, Inanc M. The effect of bevacizumab pretreatment on the choice of endotamponade in diabetic tractional retinal detachment.
2016;47(10):924-929.
29 Tan YR, Fukutomi A, Sun MT, Durkin S, Gilhotra J, Chan WO. Anti-VEGF crunch syndrome in proliferative diabetic retinopathy: a review.
2021;66(6):926-932.
30 Bressler NM, Beaulieu WT, Bressler SB, Glassman AR, Melia BM,Jampol LM, Jhaveri CD, Salehi-Had H, Velez G, Sun JK, Network DRCRR. Anti-vascular endothelial growth factor therapy and risk of traction retinal detachment in eyes with proliferative diabetic retinopathy: pooled analysis of five drcr retina network randomized clinical trials.
2020;40(6):1021-1028.
31 Chen HJ, Wang CG, Dou HL, Feng XF, Xu YM, Ma ZZ. Effect of intravitreal ranibizumab pretreatment on vitrectomy in young patients with proliferative diabetic retinopathy.
2020;9(1):82-89.
32 Wang DY, Zhao XY, Zhang WF, Meng LH, Chen YX. Perioperative anti-vascular endothelial growth factor agents treatment in patients undergoing vitrectomy for complicated proliferative diabetic retinopathy: a network meta-analysis.
2020;10(1):18880.
猜你喜欢
杂志排行
International Journal of Ophthalmology的其它文章
- Leptin activates the JAK/STAT pathway to promote angiogenesis in RF/6A cells in vitro
- CCPG1 involved in corneal Aspergillus fumigatus infection
- Anti-scarring effect of sodium hyaluronate at filtration pathway after filtering surgery in rabbits
- Five-in-one: a novel, cost-effective yet simple use of micro needle holder
- CO2 laser-assisted sclerectomy surgery and trabeculectomy combination therapy in Peters’ anomalyrelated glaucoma: a case report
- Congenital fibrovascular pupillary membranes: case series with pathological correlation and surgical treatment
