Evaluation of Depression and Quality of Life in Patients With Psoriasis
2022-04-15SravaniSriramojuShivaDundeVenkateshwarluEggadiManasaSowmyaKoppoluSharavanaBhavaBandaruSeshagiri
Sravani Sriramoju, Shiva Dunde, Venkateshwarlu Eggadi, Manasa Sowmya Koppolu,Sharavana Bhava Bandaru Seshagiri,∗
1Department of Clinical Pharmacy & Pharm. D., MGM Hospital, Vaagdevi College of Pharmacy, Hanamkonda, Warangal,Telangana 506007, India; 2Neuropsychiatric Consultant, Manisha Neuropsychiatry Clinic and Counselling Centre, Hanamkonda,Warangal, Telangana 506007, India.
Abstract
Keywords:depression,dermatology life quality index 10,patient health questionnaire 9,psoriasis,psoriasis area and severity index score
Introduction
Psoriasis is a chronic inflammatory dermatological condition characterized by skin lesions covered with white or silver scales,1-2with a strong genetic susceptibility, and complex autoimmune pathogenesis.3Based on the lesion characteristics,psoriasis is mainly classified into two types;non-pustular psoriasis includes psoriasis vulgaris, guttate psoriasis, erythrodermic psoriasis, inverse psoriasis, and psoriatic arthritis, while pustular psoriasis includes Von Zumbusch psoriasis, impetigo herpetiformis, and acrodermatitis continua of Hallopeau.4-6As psoriasis is a disorder with visible skin changes, it results in physical,emotional, and social burdens on the patient.7Patients with psoriasis often experience a significant decrease in their emotional wellbeing and social functioning,adversely affecting their quality of life.8-9As a result,patients with psoriasis have a high prevalence of psychiatric morbidities,including sleep disorders, anxiety, and most commonly depression.10A depressed state of mind has a negative impact on a patient’s health by decreasing the adherence to self-care and medication, which consequently leads to a poor disease prognosis.11-12In addition, the onset and course of depression in patients with psoriasis shows a strong association with systemic inflammation,13-14as there is a negative bidirectional relationship between depression and inflammation in patients with psoriasis.15-16The ongoing inflammation causes physiologic and biochemical changes that drive an increase in the levels of inflammatory cytokines,17including tumor necrosis factor, interleukin(IL)-1β,IL-6,18and C-reactive protein.19In the brain,these cytokines initiate biochemical signaling to deplete neurotransmitters such as serotonin,dopamine,and norepinephrine, which are directly involved in the pathogenesis of major depression.20-21Conversely,depression favors stress responses and increases inflammation, which in turn exacerbates psoriasis.15The present study aimed to assess the impact of psoriasis on mental health of patients by clarifying the relationship between the severity of psoriasis and prevalence of depression,as well as the effect on healthrelated quality of life.
Material and methods
This prospective observational study included patients treated at the Dermatology Department of Mahatma Gandhi Memorial Hospital, Warangal. The study protocol,data collection form,and informed consent document were approved by the Institutional Human Ethics Committee (approval number: IHEC/VCOP/PHARM-D/2019-20/NCT07). Verbal and written informed consent were obtained from all study participants.
Inclusion and Exclusion criteria
Inclusion criteria: Patients aged between 18 and 85years with a confirmed diagnosis of any type of psoriasis.Exclusion criteria: (1) Current treatment with psychotropic drugs,(2)severe comorbidities or chronic diseases,(3)a diagnosis of any psychiatric illness before the diagnosis of psoriasis,and(4)visual,hearing,language,or cognitive deficits or impairments.
Scales and questionnaires
The psoriasis area and severity index (PASI) was used to measure the severity of psoriasis. The PASI score ranges from 0 to 72 and is used to classify psoriasis as mild(1–5),moderate (6–12), severe (13–20), or very severe (>20).22The patient health questionnaire (PHQ 9) was used to assess the severity of depression in patients with psoriasis.The PHQ 9 is a self-administered questionnaire comprising nine elements to give a score ranging between 0 and 27;a score of 0 indicates no depression, while a score of 1–4 indicates minimal depression, 5–9 indicates mild depression, 10–14 indicates moderate depression, 15–19 indicates moderately severe depression, and 20–27 indicates severe depression.23-24The dermatology life quality index(DLQI 10) was used to evaluate the quality of life. The DLQI score ranges between 0 and 30, with higher scores indicating a greater effect of the disease on quality of life.25-26
Statistical analysis
All data collected through patient interviews and questionnaires were organized in a Microsoft Excel worksheet.All data were expressed as mean±standard deviation.The data analysis was conducted using Microsoft Excel 2019 and MedCalc statistical software,version 19.6.1.Pearson correlation coefficient“r”with a 95%confidence interval(CI) was evaluated to establish the association between two continuous variables. The Chi-squared test was used to compare variables between groups. A P value<0.05 was considered statistically significant.
Results
Baseline of the subjects
A total of 282 patients diagnosed with any type of psoriasis were screened, and 154 patients who met the eligibility criteria were included in the study. The study population comprised 90 men(58%)and 64 women(42%);the mean age was 49.59±13.39years(range 18–75years),and most patients were 56–65years old. The sex and age distributions are presented in Table 1.All patients were diagnosed with psoriasis at least 6months before the commencement of this study.Among the 154 patients,132(85.7%)had a diagnosis of plaque psoriasis, 14 (9.1%) had scalp psoriasis, three (1.9%) had guttate psoriasis, three(1.9%) had pustular psoriasis, and two (1.3%) had erythrodermic psoriasis (Table 2). The mean age at the onset of psoriasis was 45.48±13.53years (range 11–74 years) (Fig. 1).
Based on the PASI score, the psoriasis was classified as mild in 56 patients (36.36%), moderate in 40 (25.97%),severe in 50 (32.47%), and very severe in eight (5.20%).Based on the PHQ 9 scores, 139 of the 154 patients(90.3%) had depression. Of these 139 patients with depression, 72 (46.7%) had mild depression and four(2.6%) had severe depression. Only 15 of the total 154 patients(9.7%)had no signs of depression.The DLQI 10 showed that psoriasis had a moderate effect the quality of life of 57 patients (37.01%) and a very large effect on 52 patients (33.77%). Only 10 patients’ (6.49%) quality of life remained unaffected by the presence of psoriasis. The distributions based on the PASI, PHQ 9, and DLQI 10 scores are demonstrated in Tables 2 and 3, respectively.
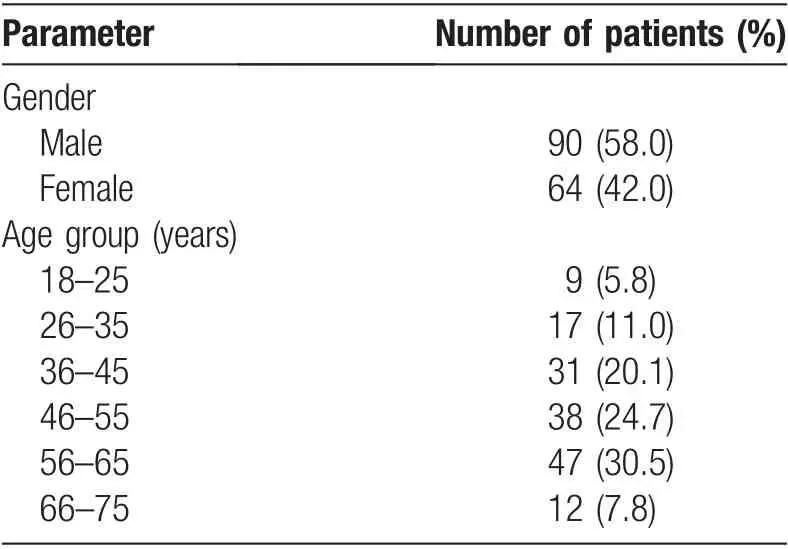
Table 1 Gender-wise and Age-wise distribution of the study participants.

Table 2 Distribution based on disease type and severity of psoriasis.
Sociodemographic factors and depression symptomology
To assess the factors associated with depression, the sociodemographic variables of patients with depression(mild and above) were compared with those without depression using the chi-squared test(Table 4).Of the 154 patients,102(66.2%)were classified as having depression.The variables that significantly differed between patients with versus without depression were age, marital status,educational status, working status, and severity of psoriasis. In the older-aged group (>59years old), 34 of 46 patients(73.9%)had depression.Depression was most prevalent in single/widowed patients(81.8%),uneducated patients (69.4%), daily wage earners (68.7%), and patients with severe and very severe forms of psoriasis(76% and 87.5%, respectively). The duration of disease(duration from the date of diagnosis to the date of study commencement)also affected the likelihood of depression.Patients who were recently diagnosed were more likely to have depression;74.4%of patients with a recent diagnosis of psoriasis had depression, while 60% of patients who had been living with psoriasis for more than 10years had depression.

Figure 1. Distribution of age onset of psoriasis in the study population.

Table 3 Distribution based on severity of depression(PHQ 9 score)and quality of life(DLQI 10 score).
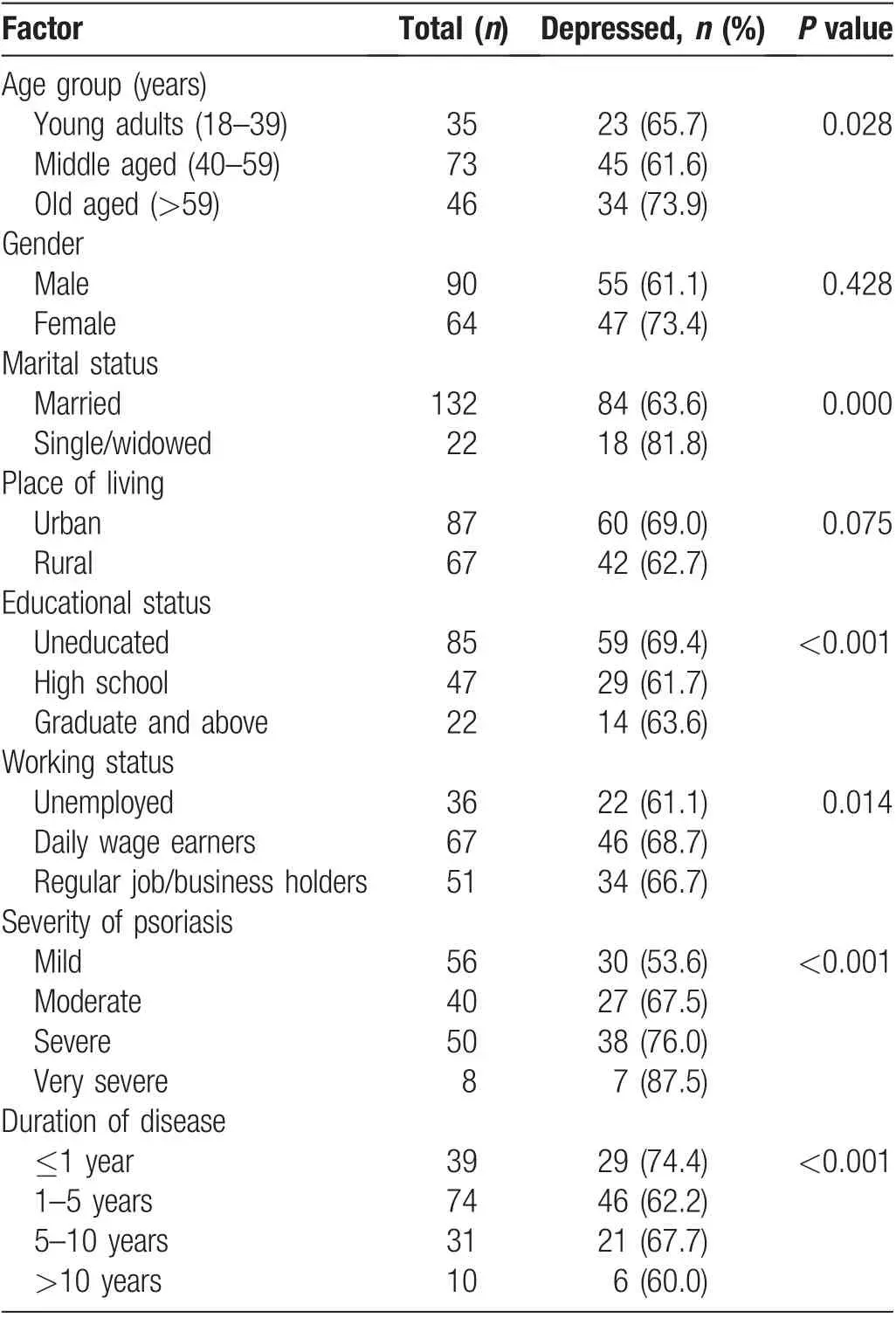
Table 4 Socio-demographic factors associated with likelihood of depression.
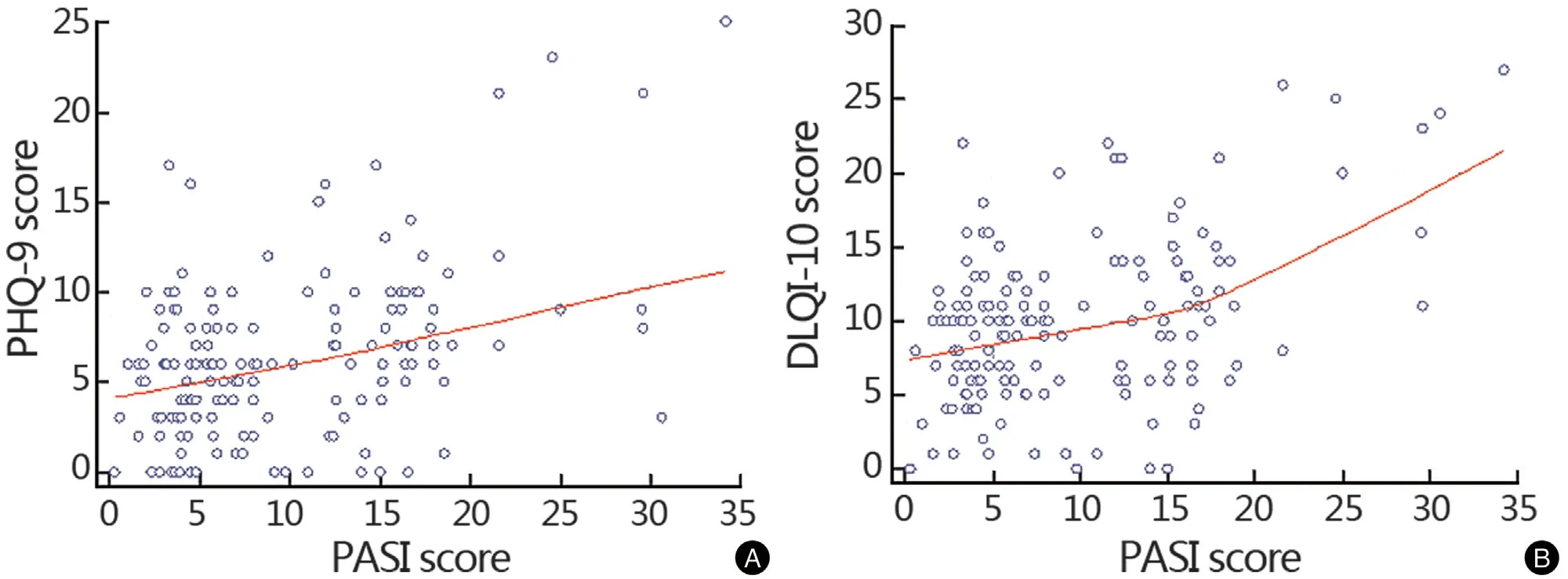
Figure 2. Correlation between severity of psoriasis and depression.(A)Scatter plot showing correlation between PASI and PHQ-9.(B)Scatter plot showing the correlation between PASI and DLQI 10. DLQI-10: dermatology life quality index 10;PASI: psoriasis area and severity index score; PHG-9: patient health questionnaire 9.
Correlation between PASI and PHQ 9/DLQI 10
Fig. 2A depicts the relationship between the PASI score and the PHQ 9 score, which reflects the association between the severity of psoriasis and the severity of depression. The PASI score and the PHQ 9 score were moderately positively correlated (r=0.42, P<0.0001,95% CI: 0.28–0.54); that is, the severity of depression increased with the increase in the severity of psoriasis.
Fig. 2B shows the relationship between the PASI score and the DLQI 10 score,which shows the effect of psoriasis severity on quality of life. The severity of psoriasis was positively correlated with the effect on quality of life (r=0.43,P<0.0001,95%CI:0.29–0.55).This means that as the severity of psoriasis increased,the effect of the disease on the quality of life increased.
Discussion
This study established the relationship between psoriasis and depression. Plaque psoriasis was the most common type of psoriasis (85.7%), while the other types each comprised <2% (Table 2). These findings are consistent with the literature that states that plaque psoriasis is the most frequently seen clinical form of psoriasis,constituting nearly 90% of all cases.27A recent study stated that psoriasis has two peaks of onset, with the first peak occurring at the age of 20–30years and the second peak at 50–60years.28In our study, the highest peak of onset occurred in the 40–49-year age group.This variation may be due to late diagnosis because of a low level of education,high level of poverty,and financial constraints.Data from various studies provide strong evidence for the validity of the PHQ 9 as a measure of the severity of depression.29-30Our analysis of the PHQ 9 scores complements the increasing use of the PHQ 9 as a measure of the severity of depression. At least 66% of the present study population had mild to severe symptoms of depression.Apart from the pathology of the disease,certain sociodemographic factors were found to be associated with depression.In the present study,young adults and older-aged patients with psoriasis tended to have a higher prevalence of depression than middle-aged patients, although this difference failed to achieve statistical significance (P=0.028). In addition,uneducated patients and patients whose earnings were based on daily wages were more likely to have depression compared with educated patients and patients who had a constant inflow of money through a regular job or business.The prevalence of depression was also higher in women than men, particularly for students and working women;a lack of knowledge about the disease and social stigma may add to the likelihood of depression in women who need to leave their homes on a regular basis. The health-related quality of life assessed with the DLQI 10 showed that the presence of psoriasis and psoriatic lesions affected the quality of life of most patients. Moreover,poor health-related quality of life was most frequently observed in psoriatic patients with scalp involvement.
When depression is diagnosed in a patient with psoriasis,the most common treatment approach is to treat both diseases simultaneously with drug therapy. However, the critical point of connection between psoriasis and depression is the systemic immune-mediated inflammation. Therefore, the treatment should mainly focus on diminishing the inflammatory immune response. Mrowietz et al.13suggested that psoriatic patients with depression benefit from pharmacological therapy with cytokine antagonists such as tumor necrosis factor inhibitors and IL-12 and IL-23 inhibitors along with lifestyle changes and adequate psychological support.
An important limitation of this study is that the outcomes of the ongoing treatment for psoriasis were not assessed. Therefore, there is a possibility that the association between psoriasis and depression is not directly related to the disease, but related to the medications used (oral retinoids or methotrexate). Moreover,the evaluation of depression was done using a patient response-based questionnaire. Although PHQ-9 has a good validity and reliability, a confirmatory diagnosis using the gold standard DSM-V criteria was not included in this study.
In conclusion, depression is a common comorbidity in patients with psoriasis.The severity of depression was mild in 46.7%of patients and severe in 2.6%.In addition to the pathogenesis of the disease, depression was associated with sociodemographic factors such as age,marital status,educational status, and working status. Psoriasis had a moderate effect on the quality of life of most patients.The severity of psoriasis was positively correlated with both the severity of depression and poor quality of life.
Acknowledgments
The authors are grateful to Dr. Ch. Devender Reddy(Secretary,Viswambhara Educational Society,Warangal)and Dr. Ch. Srinivas Reddy (Principal, Vaagdevi College of Pharmacy, Hanamkonda) for their support and providing the necessary facilities to carry out this study.
杂志排行
国际皮肤性病学杂志的其它文章
- Prevalence of Acne Inversa (Hidradenitis Suppurativa) in China: A Nationwide Cross-Sectional Epidemiological Study
- Cutaneous Manifestations of HIV/AIDS in the Era of Highly Active Antiretroviral Therapy:Evidence from Bangladesh
- Epidemiology of Pemphigus: A Single Center Experience in Morocco
- Nail Psoriasis: Treatment Options and Management Strategies in Special Patient Populations
- Concurrence of Merkel Cell Carcinoma and Squamous Cell Carcinoma in A Patient with Generalized Actinic Keratosis: A Case Report
- Bowen’s Disease on the Left Fifth Finger Successfully Treated with Photodynamic Therapy: A Case Report
