Prevalence and correlates of aggressive behavior in psychiatric inpatient populations
2022-04-01HunorGirasekVandaAdNagySzabolcsFeketeGaborUngvariborGazdag
Hunor Girasek,Vanda Adél Nagy,Szabolcs Fekete,Gabor S Ungvari,Gábor Gazdag
Hunor Girasek,Vanda Adél Nagy,Gábor Gazdag,Department of Psychiatry and Psychiatric Rehabilitation,Jahn Ferenc South Pest Hospital,Budapest 1204,Hungary
Szabolcs Fekete,Department of Psychiatry,National Institute of Forensic Psychiatry,Budapest 1108,Hungary
Szabolcs Fekete,School of PhD Studies,Semmelweis University,Budapest 1085,Hungary
Gabor S Ungvari,Division of Psychiatry,School of Medicine,University of Western Australia,Crawley 6009,Australia
Gabor S Ungvari,Section of Psychiatry,University of Notre Dame,Fremantle 6160,Australia
Gábor Gazdag,Department of Psychiatry and Psychotherapy,Faculty of Medicine,Semmelweis University,Budapest 1083,Hungary
Abstract Aggressive behavior in patients with psychiatric disorders is attracting increasing research interest.One reason for this is that psychiatric patients are generally considered more likely to be aggressive,which raises a related question of whether diagnoses of psychiatric disorders predict the prevalence of aggressive behavior.Predicting aggression in psychiatric wards is crucial,because aggressive behavior not only endangers the safety of both patients and staff,but it also extends the hospitalization times.Predictions of aggressive behavior also need careful attention to ensure effective treatment planning.This literature review explores the relationship between aggressive behavior and psychiatric disorders and syndromes (dementia,psychoactive substance use,acute psychotic disorder,schizophrenia,bipolar affective disorder,major depressive disorder,obsessivecompulsive disorder,personality disorders and intellectual disability).The prevalence of aggressive behavior and its underlying risk factors,such as sex,age,comorbid psychiatric disorders,socioeconomic status,and history of aggressive behavior are discussed as these are the components that mostly contribute to the increased risk of aggressive behavior.Measurement tools commonly used to predict and detect aggressive behavior and to differentiate between different forms of aggressive behavior in both research and clinical practice are also reviewed.Successful aggression prevention programs can be developed based on the current findings of the correlates of aggressive behavior in psychiatric patients.
Key Words:Aggression;Mental disorders;Inpatients;Prevalence;Risk factors;Risk assessment
lNTRODUCTlON
The relationship between psychiatric disorders and aggressive behavior has always been a contentious issue,as it is difficult to determine whether psychiatric patients are more likely to be aggressive and whether psychiatric disorders predict aggressive behavior[1].
The authors of most recently published studies agree that there is an increased risk of aggressive behavior in certain psychiatric disorders[2-5].In a meta-analysis,the proportion of patients classified as aggressive during their acute psychiatric treatment ranged from 8% to 44%[2].Aggressive behavior and violence pose a serious challenge to psychiatric care providers as they threaten the safety of both the patients and staff[1,2,6].They also result in longer hospitalization times and the increased stigmatization of psychiatric patients[3].To predict and prevent violent events in inpatient units,it is crucial to recognize the relationships of the sociodemographic and clinical characteristics of inpatients with the risk of aggression[2].
The aims of this paper are to review the risks of aggressive behavior associated with different psychiatric disorders and assess the commonly used measurement tools to measure various aspects of aggressive behavior.
DEFlNlTlON OF AGGRESSlON
There are several definitions of aggression,a rather broad term used with different emphases in criminology,political and social science,and psychiatry.For the purpose of this review,aggression is defined as a human behavior manifesting as verbal or physical acts that target other human beings,animals,or objects with the aim of causing harm.The aggressors are not always aware of the implications of their actions and the damage caused.If the harm is coincidental or a secondary consequence,the act is not considered as aggressive[7,8].
Instrumental or proactive aggression involves intentionally harming an individual to achieve a desired goal.In contrast,impulsive aggression is often referred to as hostile or reactive aggression that has no identifiable goal.In impulsive aggression,the perpetrator is driven by anger,and the act is an inconsiderate and unplanned response to perceived provocation[7,9,10].In line with most definitions,in this paper,violence is referred to as an extreme form of aggressive behavior with the purpose of physically harming others,irrespective of the consequences[7].
METHODS OF THE REVlEW
This narrative review began with a search of the PubMed,PsychINFO,Google Scholar databases using the key words such as (psychiat* or mental*) and (aggress* or violen*or hostil*) and measure*.The publication was chosen if it included any of the following categories of psychiatric disorders and syndromes:dementia,psychoactive substance use,acute psychotic disorder,schizophrenia,bipolar affective disorder,major depressive disorder,obsessive-compulsive disorder,personality disorders (PDs)and intellectual disability.The papers included were peer-reviewed journal articles and books that were published mainly in English.Further articles were reached by following up references.We tried to review the most recent research data to present the current findings of the prevalence and correlates of aggressive behavior in psychiatric inpatient populations.
AGGRESSlON lN DlFFERENT PSYCHlATRlC DlSORDERS
Dementia
Alzheimer’s disease (AD) and mild cognitive impairment (MCI) increase the risk of agitation and aggressive behavior[11-14].Aggressive behavior is one of the most common and disturbing complications of cognitive impairment,such as dementia;it contributes to early hospital admission and increases the burdens of caregivers and hospital staff[11],as patients with dementia can harm themselves and other patients[12,13].The extent of functional deficits and cognitive impairment in dementia is correlated with behavioral and psychiatric symptoms,including apathy,irritability,agitation,aggression,delusions,depressive mood,and anxiety[12].
The main neuropathological finding related to progressive changes in behavior and aggression[15-17] is prefrontal cortical atrophy,which is also associated with dementia[18].In frontotemporal dementia,anger and other confrontational/critical and emotionally charged ideas and behaviors underpin the development of interpersonal aggression and social isolation[19].Further brain areas significantly associated with aggression in dementia include the dorsomedial prefrontal and orbitofrontal cortices and the amygdala[20-22].
In a meta-analysis,the prevalence of aggressive behavior in patients with AD and MCI was reported to be 27.8% and 7.4%,respectively[11].However in another study aggression was found to be the major cause of hospitalization - in 34.2% of all cases -particularly in patients with moderate/severe dementia[23].Place of residence was also correlated with aggression.For example,agitation and aggressive behavior were observed in 20% of outpatients living in the community,but in 40%-60% of patients living in nursing homes[24].In a meta-analysis,no significant difference was observed in the risk of physical aggression between patients with different types of dementia with the exception of patients with frontotemporal dementia,among whom the prevalence of criminal behavior was 37%,as opposed to only 8% in patients with AD[11].In contrast,studies of verbal aggression in AD showed significantly higher rates ranging from 28% to 67%[14].However,no significant correlation was reported between verbal aggression and the severity of dementia measured by the Mini Mental State Examination,although verbal aggression was found to be related to the presence of delusions[14].
Aggressive behavior in AD is associated with depression,loss of family contact,a poor caregiver-patient relationship,and chronic pain[11,25-27].Objectively assessing the level of pain in dementia patients can be challenging,although reducing pain could decrease agitation and aggressive behavior[13].
A systematic review confirmed the clinical impression that compared with women,men have higher rates of aggression and other behavioral problems,such as wandering,abuse of others,and social incompetence[28].
Psychoactive substance use
Substance use disorders are among the most prevalent psychiatric disorders,but only a minority of such patients seeks treatment.The relationship between drug use and aggressive behavior is a constantly growing concern[29,30].It is universally accepted that alcohol and certain drugs significantly increase the incidence of aggressive behavior[2,29-33].In a forensic psychiatric sample,28% of patients with previous offences committed crime under the influence of a psychoactive substance[34].Aggressive behavior occurs at any stage of drug use:in acute intoxication,in connection with drug-seeking behavior,in withdrawal,or in episodes of drug-induced psychosis[31].Drugs and violence are related directly when the drug pharmacologically induces violence or indirectly when the violence serves as a method of obtaining the drug[32].Overall,the relationship between drugs and aggression is complex and is driven by a combination of factors related to both transient and permanent physiological,psychological,environmental,and individual differences[30].
Alcohol:Alcohol is the substance most commonly associated with aggressive and violent behavior[31].The link between acute alcohol consumption and aggressive behavior is well-known[35].Even moderate amounts of alcohol increase the likelihood of aggressive behavior[32].Alcohol consumption has been associated with increased frequency and severity of physical aggression toward acquaintances and strangers[36,37],increased verbal aggression[38],domestic and marital violence[39,40],sexual harassment[41-43],and suicide[44].There is preliminary evidence that alcohol is more closely associated with murder,rape,and abuse than any other substance[31].
Alcohol increases aggression in both men and women,but this effect is stronger in men[35];men intoxicated with alcohol are prone to physical aggression,whereas women are prone to verbal aggression[45].However,a recent study[46] found no intersex difference in the effect of alcohol on aggressive behavior.Alcohol consumed by women at home increases their physical aggression toward their male partners,and the amount of alcohol consumed is positively correlated with physical aggression[47-49].
Chronic alcohol dependence can lead to changes in personality structure;the person increasingly blames others for his/her condition,and frequent interpersonal conflicts develop,often leading to physical or verbal aggression.Furthermore,irritability and agitation increase during periods of withdrawal,triggering the onset of aggression[31].
Because of the high individual variability in the effects of alcohol on aggressive behavior,most authors emphasize the interplay between several factors[32].Alcohol impairs frontal lobe functions,affecting the handling of threatening situations[50-53],reduces inhibitions[51],and influences neurochemical systems that mediate aggressive behavior[54-56].It is well-established that heavy alcohol consumption affects prefrontal cortex thereby contributing to the development of aggressive behavior[57-59].Even a small amount of alcohol can reduce the activity of the medial prefrontal cortex[60] resulting in the impairment of prefrontal executive functions,which may lead to careless,inappropriate,or aggressive behavior[61,62].Alcohol consumption frequently provides false justification for the variety of antisocial behaviors displayed by the intoxicated person[63].
Heroin:There is compelling evidence that heroin increases aggressive behavior,including physical aggression against others,impulsivity,and suicidality[30,64-66].An analysis of the history of 527 heroin users found that almost 43% of them had attempted suicide[67].The symptoms of opioid withdrawal can be so severe and painful that opioid users may unintentionally become violent when trying to obtain opioid drugs to seek relief from the withdrawal symptoms[31].Research data support the view that the elevated level of aggression among heroin users is driven by individual differences in aggressive behavior and other risk factors,such as childhood abuse,family history of aggression and psychiatric illness,and living in a poor neighborhood,rather than the direct effect of heroin itself[30,68].
Cannabis:Cannabis is commonly regarded as a relatively harmless substance,but there is strong evidence that cannabis withdrawal can cause anger and lead to hostile behavior[30,69,70].Compared with non-users,regular cannabis users were almost twice as likely to show aggressive behavior towards their partner,were 1.2 times more likely to be victims of aggression by their partners and were 2.4 times more likely to be both perpetrators and victims of aggressive behavior[71].These findings remained true even after controlling for the effects of alcohol and other drugs[71].
Stimulants:Both cocaine[22,59] and methamphetamine use can trigger hostile behavior[31,72-74].3,4-methylenedioxy-N-methamphetamine has been found to reduce aggression during its acute use[30,75,76],followed by a flare-up of aggression in the following days and a return to baseline after approximately one week[77].A meta-analysis found that among illicit drugs,cocaine has the strongest link to physical,sexual,and psychological aggression[78].Tomlinsonet al[30] highlighted that the relationship between cocaine use and aggressive behavior may be enhanced by personality traits,such as poor impulse control and antisocial traits.
Hallucinogens:The use of most hallucinogens has been negatively correlated with aggression,i.e.,positively associated with a lowered risk of aggressive behavior and elevated mood[30,79].Both psilocybin[80] and lysergic acid diethylamide[30,31]decrease interpersonal conflicts and subsequent aggressive behavior[81].
Acute psychotic disorder
More than 50% of all violent incidents in the context of psychiatric illness occur during psychiatric care[82-85].Psychotic symptoms have traditionally been considered as a major contributing factor to aggression[83,86-88].
Several studies have shown that first-episode psychoses carry a high risk of aggressive behavior[89-91]:approximately one-third of patients with first-episode psychosis exhibit hostility and verbal and/or physical aggression during hospitalization,and the severity of their violence frequently poses risk to others[92].In one study,16% of patients with first-episode psychosis were reported to be aggressive in the week before admission,7% were aggressive in the week after admission,and 10%were aggressive in both periods[92].In another study,aggressive behavior was observed in more than half of the patients with first-episode psychosis,with verbal aggression being the most common aggressive behavior in inpatient wards[88,93].In a similar study,nearly 70% of participants with first-episode psychosis were reported to have committed at least one act of physical and/or verbal abuse in the year prior to admission,and 43% and 61.5% showed physical and verbal aggression,respectively[85].
A study reported that most of the violent acts by patients with first-episode psychosis targeted themselves or property,whereas only 7% of the violent acts were committed against another person,and only 2.5% of these caused actual injuries,such as bruises and scratches[92].Furthermore,46% of patients had conflicts with the law,of whom 42.9% were arrested and 35.1% spent at least one night in prison[85].Approximately one-fifth of patients reported some form of suicidal ideation and behavior,including suicide attempts,during the first episode of psychosis[88].A recent meta-analysis found that 18.4% of patients attempted suicide during their first episode of psychosis prior to seeking treatment[94].
Several sociodemographic and illness-related factors can contribute to the development of aggressive behavior[95,96].Risk factors for aggression during firstepisode psychosis include younger age,male sex,lower socioeconomic status,a longer duration of untreated psychosis,a manic state,drug use,antisocial personality traits,childhood emotional/physical/sexual abuse,and impulsivity[85,88,90,97-99].
Schizophrenia
Patients with schizophrenia tend to exhibit hostile behavior,particularly during an acute psychotic episode.These patients face an almost four times greater risk of aggressive behavior than people with no psychiatric problems[82,100,101].The degree of aggression is significantly related to psychopathology[101-103].Violent behavior is more commonly displayed by patients who have psychotic symptoms,such as command hallucinations that encourage them to act violently[104].Impulsivity in schizophrenia is also closely related to aggression and suicidal behavior[3,105-107];in a study of risk factors for suicide in schizophrenia,11.6% of the patients attempted suicide right after the violent behavior[108].Patients with schizophrenia,particularly those in the acute phase,frequently exhibit hostility,anger,and agitation that can lead to verbal or even physical aggression[109-111].Both hostility and aggressive behavior are associated with longer and more frequent hospitalization[100,112-115].Aggression also occurs frequently after discharge from hospital:a meta-analysis revealed that 10%of patients with schizophrenia,compared with only 2% of the general population,exhibited aggressive behavior in the community[116].
The prevalence of threatening and aggressive behavior is common in hospitalized schizophrenia patients,ranging from 10% to 45%[1,110,117-121],but a recent metaanalysis found higher rates of 15.3%-53.2%[122].Although different forms of aggression are common,with verbal aggression occurring in up to 75% of the cases,serious physical injury is rare[1,93,123-125].
The prevalence of auto- and hetero-aggression in schizophrenia has been reported to show considerable intersex differences.For example,in a previous study,75% of the male patients and 53% of the female patients demonstrated some form of aggressive behavior during their first hospitalization and in the following two years,while 17% of the male patients and 26% of the female patients attempted suicide[100].Demographic factors that predict aggression include younger age,male sex,and single marital status[1,3].
Co-morbid psychiatric disorders,primarily substance use disorders,significantly contribute to aggressive and violent behavior in patients with schizophrenia[100,116,126,127].It is estimated that 20%-65% of patients with schizophrenia use illicit drugs,compared with 16.7% of the general population[101].In addition to substance use disorders,other common comorbidities,such as antisocial personality disorder,can also increase the risk of aggressive behavior in patients with schizophrenia[2,3].
Bipolar affective disorder
Bipolar disorder is associated with an increased risk of aggressive behavior[128-131].A high risk of aggressive behavior has also been demonstrated in bipolar patients in remission[110,132-134].The lifetime prevalence of aggression was 12.2% in a mixed group of bipolar patients[135] and 25.3% in patients with bipolar I disorder[136].
Aggressive or violent behavior in bipolar patients usually appears during acute manic episodes[137-139] and is a common cause of hospitalization in this population[130,140-142].Involuntary hospitalization for acute mania is significantly associated with higher rates of aggression/violence and lower rates of insight[109,143].A clear association was found between the presence and severity of aggression during a manic episode and psychotic symptoms[130,144].Patients with mood-incongruent psychotic symptoms are more prone to agitation or aggression[145-149].Agitation — a common symptom in acute bipolar mania — is characterized by motor restlessness and increased responsiveness that can lead to physical aggression[110,150].No association has been found between aggressive and suicidal behaviors in bipolar illness[130] or between male sex and aggressive behavior[141,151].
Serotonergic hypoactivation has been hypothesized to play a role in the neurobiological basis of aggression in bipolar illness[131].The association between prefrontal cortical dysfunction and aggressive behavior in bipolar patients has been repeatedly confirmed[152-154].Damage to the prefrontal cortex results in disruption of executive functions,leading to dysfunctional patterns of behavior in the social realms including emotional outbursts,increased risk-taking and aggression as well as disorganized behavior[61,155].Executive dysfunction is common in bipolar disorder,schizophrenia and acute psychoses[156,157],where impaired impulse control and dysregulated behavior manifest in aggression[158].
A further possible explanatory factor for aggression in mania may be a lack of insight.Aggressiveness during acute manic episodes depends on the severity of the episode and the degree of insight[130,159].Possible predictors of aggressive or violent behavior in mania include past aggressive or violent behavior,criminal history,childhood sexual abuse,being a victim of previous violence,comorbid PDs,and alcohol and/or drug abuse[110].
Major depressive disorder
Depression is a risk factor for aggressive behavior,mostly in the form of autoaggression[160].Factors associated with aggressive behavior in depression include impulsivity[160-163],alcohol use[160,164-168],and the risk of suicidal behavior[169-173].High impulsivity scores were found in a sample of patients diagnosed with major depressive disorder who had previously attempted suicide[163].Suicide attempters are more aggressive than non-attempters[174-177].
Associations have also been found between attachment anxiety and suicide attempts[178,179] and between the expression,proneness,and attributions of anger and adult attachment styles[179].Adults with a preoccupied attachment style,which is characterized by the person having a negative image of him/herself and a positive image of others,are more likely to display high-risk behaviors and even suicidal gestures due to their dysregulated emotional and behavioral control[178].Insecurity is associated with signs of dysfunctional anger,such as hostility.An anxious-ambivalent attachment style is characterized by inward-directed anger and displaced aggression,whereas a secure attachment style is characterized by the appropriate,functional expression of anger[173,178,179].
Symptoms of depression and anger have been associated with attachment style and auto-aggression in depressed inpatients[173].It was hypothesized that the aggressive behavior of patients with elevated attachment anxiety is self-directed,resulting in nonsuicidal self-harm or suicide attempts.This theory is supported by the fact that depressive symptoms are strongly associated with suicide attempts,suggesting that depression is a partial mediator to the relationship between attachment anxiety and self-directed aggression[173].
Increased alcohol consumption is also a mediator to the relationship between depression and aggression.In one study,the prevalence of alcohol use disorder was estimated at 32.3% in a sample of people who reported a depressive episode in the previous year,as opposed to only 9.5% in the non-depressed sample[180].
It was hypothesized that in the anxiety/aggression-driven subtype of depression,depressive episodes are triggered by increased anxiety and/or unregulated,outwardly directed aggression,such as irritability or outbursts of anger.Consequently,in this subtype of depression,the symptoms of dysregulated aggression and/or anxiety mask the depressive mood[181].Assessment of depression should include a search for evidence of comorbidity with alcoholism and personality traits such as aggression and impulsivity to better understand the link between depression and suicidal behavior and to identify patients at a higher risk of suicidal behavior[166].
Obsessive-compulsive disorder
The relationship between obsessive-compulsive disorder (OCD) and aggression has been explored in relatively few studies.Increased aggression and hostility in OCD are positively correlated with symptoms of hoarding[182,183],the inhibition of avoidant behavior or rituals[184],and the severity of OCD symptoms[183,185,186].
In OCD,indirect aggression is more common and direct aggression is relatively infrequent[187].The relationship between latent aggression (hostility/aggression toward other individuals,which is not openly expressed but manifested in fantasies or disguised forms that are not always conscious to the individual) and OCD has been explored[188-190] but not extensively studied.Explanations offered for this association include the psychodynamic theory of OCD[189,190] and the role of anxiety,which may prevent OCD patients from expressing their anger because they are worried about how others will react to an openly aggressive behavior[183,191].
Increased anger[192,193],hostile behavior[183,194],and frequent interpersonal conflicts have been reported in studies on OCD[183,189,190,195].In one study,more than half of the OCD patients reported interpersonal conflicts,with one in two patients admitting that they were aggressive with their partner[195].Family members who refuse to participate in the rituals of an OCD patient may be targets of aggressive behavior[190,195].Another source of interpersonal conflict in OCD is when patients take excessive precautions to maintain the safety of others (e.g.,forced control of locks)who do not take these precautions as seriously[196],which induces anger and hostile behavior in OCD patients[197].Patients find it harder to alleviate their anxiety when experiencing high levels of hostility,which predicts poor treatment outcomes[183,191,198].Hostility and high levels of anxiety are linked to suicide in OCD patients;in a recent study,27% of the OCD patients had suicidal ideation during their lifetime and 33% had attempted suicide[198].
Personality disorders
PDs are associated with an increased risk of developing aggressive and violent behavior[199-201].The relationship between PDs and aggression is complex,because PDs differ in terms of the type,severity of frequency of aggressive behavior[202,203].Among the 10 PDs described in the Diagnostic and Statistical Manual of Mental Disorders,Fourth edition,aggression is typically associated with Cluster B PDs(antisocial,borderline,histrionic,and narcissistic PDs) and paranoid PD among Cluster A PDs[204-208].Patients with Cluster B PDs are 10 times more likely to have a criminal conviction and eight times more likely to be in prison than patients with other PDs[209].Violent crime is most frequently exhibited by individuals with antisocial PD but is also common among criminals with borderline,narcissistic,and paranoid PDs[210].
Patients with antisocial and borderline PDs have the greatest risk of hostile behavior[208],being four times more likely to be hostile in a psychiatric ward than patients with other PDs[121].Patients with antisocial PD are 12.8 times more likely to commit a violent act,compared with the general population[211].Up to 73% of patients with borderline PD have been found to behave aggressively during a one-year period[212],58% participated in “occasional or frequent” fights,and 25% used a gun against others at some point in their lives[213].Crimes committed by patients with borderline PD are impulsive,explosive episodes of physical violence,whereas those committed by patients with antisocial PD are driven by instrumental aggression[214,215].
Borderline personality disorder:The hostile behavior of patients with borderline PD is predicted by several possible factors,including interpersonal dysfunction,negative interpersonal events[216,217],hypersensitivity to social rejection[218],and increased sensitivity to threat[208,219].One study reported that patients with borderline PD experienced significantly more fear than did healthy controls when presented with neutral faces[220,221].These results suggest that patients with borderline PD do not properly recognize facial emotional expressions,which increases their feelings of threat or provocation and may ultimately lead to reactive aggression[219].Factors underlying hostility in borderline PD include comorbid psychiatric disorders and/or substance use,affective lability,and childhood abuse[222,223].Affective dysregulation and impulsive aggression in these patients require special attention,as they are risk factors for suicidal behavior,self-harm,and interpersonal aggression and influence the choice of psycho- and pharmacotherapy[223].Most studies have found no significant intersex difference in the aggressive behavior of patients with borderline PD,but one study reported more self-aggressive behavior among female patients than among their male counterparts[224].
Antisocial personality disorder:While the aggressive behavior of patients with borderline PD is generated primarily from intense anger and instability[225],patients with antisocial PD usually perceive their environment as hostile,and therefore,their aggressive behavior stems from their perceived need to fight for their own safety and survival[226].These patients use hostility to gain personal benefits[227-229].They are scarcely able to delay gratification and thus use aggressive behavior when their demands are not met[226].
Narcissistic personality disorder:Narcissism has been reported to be a significant predictor of violent behavior in clinical and forensic psychiatric samples,with odds ratios ranging from 1.21 to 11.46[230].A systematic review found that both low selfesteem[231] and unstable self-esteem[230] in patients with narcissistic PD are associated with violent behavior and hostility.Individuals with high but unstable self-esteem are most likely to report anger and hostility,whereas high but stable self-esteem prevents anger and aggression[225].
Intellectual disability
Aggressive behavior by people with intellectual disability is the main reason for their referral to healthcare services[232-235].A hostile attitude can have serious negative consequences for people with intellectual disabilities,as it can damage their personal development and social relationships and their quality of life[236-238].In addition,the aggressive behavior of patients with intellectual disabilities often imposes a heavy burden on their relatives and caregivers and thereby negatively impacts their quality of life[235,237].
Patients with intellectual disabilities exhibit different forms of aggression,including physical and verbal aggression,destructive behavior toward the physical environment,self-harm behavior,and sexually aggressive behavior[232,235],and the prevalence of these different forms also differs significantly among patients[239].The prevalence of physical aggression ranges from 2.1%[240] to 24.4%[232],while that of verbal aggression ranges from 5.9%[241] to 37.6%[232].Verbal aggression is the most common form of aggressive behavior in this population[232,234,242].A study reported that the incidence of any form of aggressive behavior in these patients assessed in a one-year period was 51%,whereas that of all forms of hostile behavior was less than 6%[232].
The extent of hostility and its behavioral manifestations are linked with psychosocial and sociodemographic factors,the severity of intellectual disability,and the presence of comorbid psychiatric disorders.For example,aggressive behavior is more common in men with intellectual disability than in women[243].Sexually aggressive behavior is associated with the severity of intellectual disability[235] and with the frequency of rage and objectionable personal habits[244].Physical aggression is associated with more severe intellectual disability and younger age[234].Hostile behavior is more common in cases wherein intellectual disability is associated with autism,psychotic disorder,paranoia,depression,and/or a PD[245].Self-harm behavior is more common in cases with comorbid autism[232,246].
The incidence of auto-aggression,destructive behavior,and hostility against others is higher in health care facilities than at home[247].van den Akkeret al[235]emphasized that hostility is also determined by factors such as the quality of care and the quality and frequency of interpersonal interactions with caregivers.Among patients with intellectual disability,aggressive behavior is frequently used to attract the attention of caregivers thereby increasing the frequency of social interactions[235,248].Therefore,understanding the background of hostile behavior for each individual is essential to find an effective treatment[235].
MEASUREMENT TOOLS FOR AGGRESSlON
Predicting and preventing aggression and violence are key issues faced by psychiatrists and forensic physicians[249].Several methods are used to measure aggression,namely interviews,observation,laboratory tests,and projective and self-reported questionnaires[250].However,all of these methods have limitations,such as social desirability,the effect of cognitive functioning on an individual’s self-perception,or the observer’s effect on observational methods[250,251].Interpretation of risk factors should involve the patients and their family members to better understand the triggering factors,such as impulsive behavior and substance use[5].Self-administered questionnaires correctly predict aggressive acts only if the patients admit to committing violent acts[252].Patients who deny their symptoms and aggressive behavior,particularly physical aggression,have lower scores in self-administered questionnaires (e.g.,in AQ)[252].Structured,systematic assessment tools for predicting direct aggression are a relatively new addition to clinicians’ armamentarium to report,predict,and assess the risk of violence in psychiatric populations[249,253].In a study by Ogloffet al[254],the accuracy of predicting impending aggression was significantly increased by using a dynamic,structured risk assessment tool for nurses in an acute psychiatric hospital.The main limitations of structured risk assessment tools are the time and resources required to administer them and the difficulties in translating the results into clinical practice[255] (Table 1).
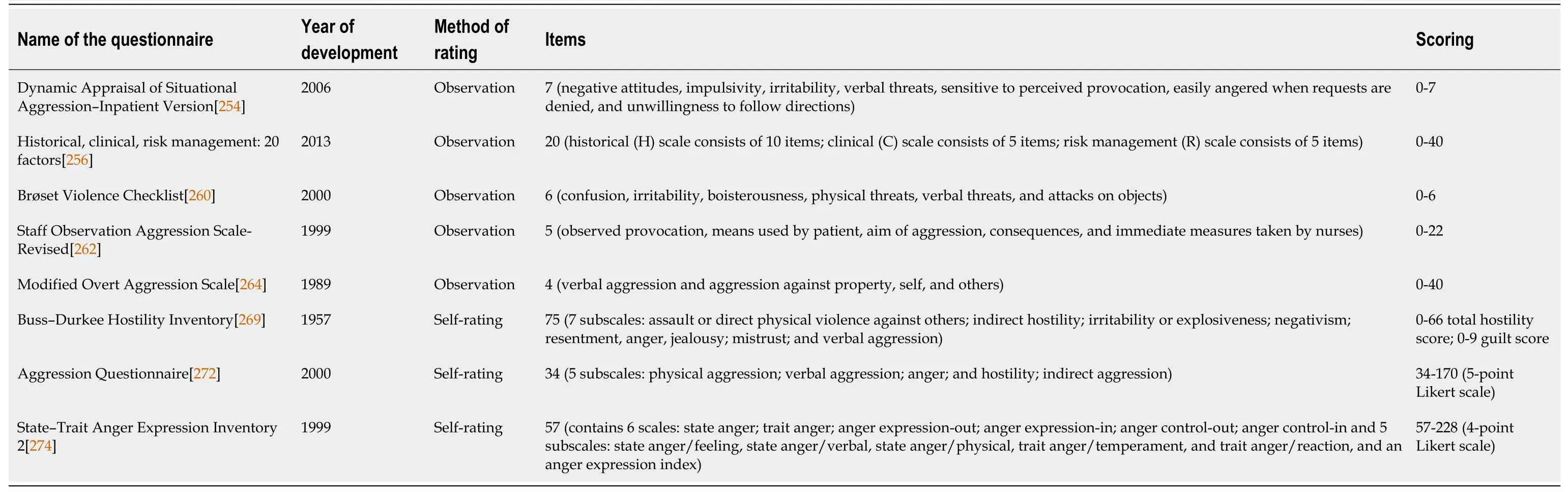
Table 1 Measurement tools for agression
Measurement tools based on observation
Dynamic Appraisal of Situational Aggression-Inpatient Version (DASA-IV[254]):The DASA-IV is a 7-item (negative attitudes,impulsivity,irritability,verbal threats,sensitive to perceived provocation,easily angered when requests are denied,and unwillingness to follow directions) structured risk assessment tool used to evaluate inpatient aggression.Each of the seven items is evaluated dichotomically,based on its presence or absence in the last 24 h.It takes less than 5 min to complete the scale.Scores of 0,1 to 3,and 4 or higher indicate very low,medium,and high risks of aggression,respectively,while a score of 6 or 7 indicates a risk of immediate aggression warranting preventive measures[254].The DASA-IV has moderate or good power for predicting aggressive events[249,253,255].
Historical,clinical,risk management:20 factors (HCR-20V3[256]):The HCR-20V3is a 20-item assessment tool that predicts the risk of interpersonal violence.The historical (H)scale consists of 10 items related to violence,and their presence is not expected to decrease with time or treatment even if the relevance of these factors may change over time.The clinical (C) scale consists of five items that are dynamic in nature and can change over time or during treatment.The risk management (R) scale also consists of five items that are dynamic and appraise concerns about the future.The items of the HCR-20V3are similar to those in the second version of the HCR-20,although some have been revised or classified under other items in the third version[257].Although relatively few validation studies have been performed on the third version[258],good inter-rater reliability was found for both the whole scale and its sub-scales (between 0.90 and 0.93) when scores were based on interviews and clinical documentation.The HCR-20V3has good predictive value for violence occurring over a 6- to 12-mo followup period[259].
Brøset Violence Checklist (BVC[260]):The BVC is a 6-item violence risk assessment checklist that evaluates six behavioral changes (confusion,irritability,boisterousness,physical threats,verbal threats,and attacks on objects) that often trigger aggression among inpatients[260].The BVC can be assessed quickly and easily (“1” denotes the presence of the behavior and “0” its absence) and is intended to predict the risk of inpatient violence occurring within 24 h.The total score is derived from the sum of the scores for each item.A score of 1 or 2 indicates a moderate risk of violence that requires preventive action,whereas a score of 3 or higher indicates a high risk of violence that requires immediate preventive action and activation of attack management plans[253,260,261].
Staff Observation Aggression Scale-Revised (SOAS-R[262]):The SOAS-R consists of five items measuring different aspects of aggression:observed provocation,means used by patient,aim of aggression,consequences,and immediate measures taken by nurses.The total score is calculated by summing the scores for each item;scores range from 0 (no aggression) to 22 (most severe form of aggression).A score of 9 or higher indicates severe aggression[262].The good psychometric properties of this scale have been confirmed by validation studies[249,262,263].
Modified Overt Aggression Scale (MOAS[264]):Adapted from the Overt Aggression Scale[265],the MOAS is used to measure aggression.Although the scale was developed to evaluate the hostile behavior of adult psychiatric inpatients,it has also been used in older patients with dementia[250].The MOAS consists of four subscales(verbal aggression and aggression against property,self,and others).The items are rated on a 5-point Likert scale,and each category is weighted:the severity of verbal aggression is given the lowest weight,whereas that of physical aggression is given the highest weight.The sum of the scores for the four subscales indicates the severity of overall aggressive behavior.The total weighted score ranges from 0 to 40.Psychometric studies of the MOAS have demonstrated good reliability and validity[266-268].
Self-report measurement scales
Buss-Durkee Hostility Inventory (BDHI[269]):The BDHI consists of 75 dichotomous(true or false) items and is divided into seven subscales:assault or direct physical violence against others;indirect hostility through gossiping,joking,slamming doors,or breaking things;irritability or explosiveness and annoyance at the smallest stimulus;negativism as either active rebellion or passive obedience to rules and authority;resentment,anger,jealousy,and/or hate of others due to real or supposed maltreatment;mistrust and the belief that others are damaging and diminishing the patient;and verbal aggression in style or content.Scores are added up to obtain a total hostility score based on 66 of the 75 items,after omitting the guilt items,which form a separate guilt scale to examine the influence of guilt on aggressive behavior.In a metaanalysis,the subscale score reliability for the BDHI was found to be less than desirable,as the Cronbach’s alpha coefficients were generally between 0.50 and 0.69[270].Nevertheless,the BDHI is one of the most widely used aggression measurement questionnaires both in clinical practice and research[271].
Aggression Questionnaire (AQ[272]):The AQ was developed to measure aggression[272],following the widespread and most commonly used BDHI[248].The AQ contains 29 items rated on a 5-point Likert scale and has four subscales:physical aggression (9 items),verbal aggression (5 items),anger (7 items),and hostility (8 items).Buss and Warren[273] revised the AQ and developed a 34-item version in which a fifth subscale—indirect aggression—was added.A higher score indicates an elevated predisposition to aggression.For the 29-item AQ,the Cronbach’s alpha scores for the subscales ranged from 0.72 (verbal aggression) to 0.85 (physical aggression),and with a score of 0.89 for the overall scale.The internal consistency of the 34-item AQ is acceptable,with Cronbach’s alpha scores for the subscales ranging from 0.71(indirect aggression) to 0.88 (physical aggression) and an overall reliability score of 0.94[271,273].
State-Trait Anger Expression Inventory 2 (STAXI-2[274]):The 57-item STAXI-2 consists of six scales that evaluate the experience,expression,and control of anger[274].The State Anger subscale assesses the intensity of anger at a particular time,whereas the Trait Anger scale measures the intensity of anger over time.The Anger Expression and Anger Control scales assess four mostly independent traits:expression of anger toward objects or others (Anger Expression-Out),holding in or suppressing angry feelings (Anger Expression-In),controlling angry feelings by preventing their expression toward objects or others (Anger Control-Out),and controlling suppressed anger by calming down or cooling off (Anger Control-In).The psychometric indicators of the STAXI-2 suggest adequate reliability and factorial,criterion,and construct validity[275-278].
CONCLUSlON
The aim of this review was to provide an overview of the aggressive behavior exhibited by patients with various psychiatric disorders.It discussed the manifestations and frequencies of aggression and the most commonly used measurement tools for aggression.Our review reveals that certain psychiatric disorders may carry an increased risk of aggressive behavior,which may be influenced by several other factors in addition to the presence of the psychiatric disorder.Examples of such factors include sex,age,socioeconomic status,comorbid disorders,and pre-existing aggressive behavior.Quantitative measurement tools,of which we have presented the most frequently used options,can help with the appropriate assessment of aggression.Successful aggression prevention programs can be developed based on the results of aggression risk evaluation.Note that the present review does not intend to increase the degree of stigmatization of psychiatric patients.Rather,it aims to draw attention to the risk factors for aggressive behavior,the importance of risk assessment and prevention of aggression,and the different possible interventions to manage aggression.
杂志排行
World Journal of Psychiatry的其它文章
- Resilience to the effects of social stress on vulnerability to developing drug addiction
- Depression among caregivers of patients with dementia:Associative factors and management approaches
- Brain-derived neurotrophic factor and inflammation in depression:Pathogenic partners in crime?
- Molecular typing of familial temporal lobe epilepsy
- Emergence of bariatric psychiatry as a new subspecialty
- Mental health promotion for elderly populations in World Health Organization South-East Asia Region:Needs and resource gaps
