Fundamentals of percutaneous coronary bifurcation interventions
2022-03-30Tamerrat
Tamer Kırat
Tamer Kırat,Department of Cardiology,Yücelen Hospital,Muğla 48000,Turkey
Abstract Coronary bifurcation lesions (CBLs) account for 15%-20% of all percutaneous coronary interventions.The complex nature of these lesions is responsible for poorer procedural,early and late outcomes.This complex lesion subset has received great attention in the interventional cardiac community,and multiple stenting techniques have been developed.Of these,the provisional stenting technique is most often the default strategy;however,the elective double stenting (EDS) technique is preferred in certain subsets of complex CBLs.The double kissing crush technique may be the preferred EDS technique because of its efficacy and safety in comparative trials;however,this technique consists of many steps and requires training.Many new methods have recently been added to the EDS techniques to provide better stent scaffolding and to reduce early and late adverse outcomes.Intravascular imaging is necessary to determine the interventional strategy and postinterventional results.This review discusses the basic concepts,contemporary percutaneous interventional technical approaches,new methods,and controversial treatment issues of CBLs.
Key Words:Percutaneous coronary intervention;Coronary artery disease;Drug-eluting stents;Bifurcation lesion;Stenting technique;Left main intervention
INTRODUCTION
Percutaneous interventions of coronary bifurcation lesions (CBLs) are not only technically challenging,with lower procedural success and higher complication rates,but also have higher thrombosis and restenosis rates than nonbifurcation lesions[1-3].The broad anatomical (i.e.,bifurcation site and angle,and vessel diameters) and pathological (i.e.,severity,locations and lengths of the atherosclerotic plaques) spectrum of CBL,as well as dynamic changes (carina,plaque shift and dissection) during intervention are responsible for the complexity of these lesions[3,4].Many stenting and other interventional techniques have been developed and are used to provide optimum stent scaffolding,resulting in fewer clinical adverse outcomes.Operators should be familiar with these techniques and the basic aspects of CBLs.
BASIC ASPECTS
Anatomy
In epicardial coronary arteries,bifurcations show a fractal geometry[5] (a fractal is a geometric shape in which every smaller structure is similar to the whole part).This geometry provides minimum energy consumption and the optimum amount of blood required for the underlying myocardium[6].A coronary bifurcation consists of a flow divider (carina) and three vessel segments:The proximal main vessel (PMV),the distal main vessel (DMV) and the side branch (SB) (Figure 1).There is a constant relationship between these three vessels that was identified by Murray’s law 95 years ago[7] as:
(Diameter of PMV)3=(Diameter of DMV)3+ (Diameter of SB)3
Nearly a decade ago,this law was modified in human coronary arteries by the Huo-Kassab law[8] as:
(Diameter of PMV)7/3=(Diameter of DMV)7/3+ (Diameter of SB)7/3
Nearly at the same time,Finet’s formula was created by IVUS measurements in normal human coronary arteries[9] as:
(Diameter of PMV)=0.678 (i.e.,approximately 2/3) × (Diameter of DMV + Diameter of SB)
Huoet al[10] compared these 2 Laws and Finet’s formula in the epicardial coronary bifurcations of patients and swine in a later study.They found that Huo-Kassab law accurately predicts all size diameters of the epicardial coronary bifurcation vessels whereas Murray’s law and Finet’s formula can only do so in certain size subsets[10].However,due to its simplicity,Finet’s formula is the most commonly used in clinical practice in most angiography units.
The polygon of confluence (POC) is an independent area between the PMV,DMV and SB whose boundaries are formed by the lines drawn vertically in the ostium of branches and at the end of the PMV (Figure 1)[11,12].Finally,the bifurcation angle (carinal angle) is important in accessing the SB and in the decision of the stent treatment strategy.
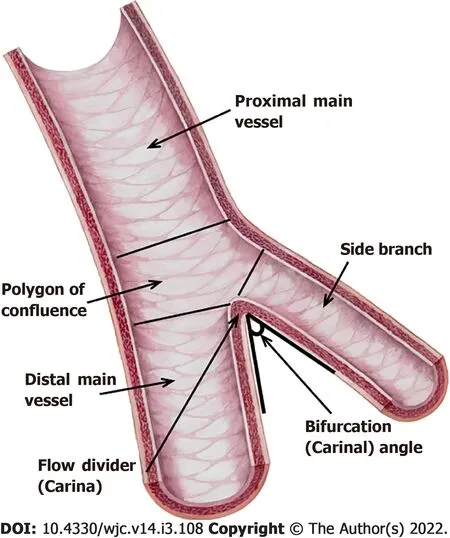
Figure 1 Coronary bifurcation anatomy.
Definition
A bifurcation lesion is a major epicardial coronary artery stenosis next to and/or including the ostium of a significant side branch[13,14].A significant SB is a branch whose severe narrowing or acute occlusion before or during intervention can cause considerable ischemia or a new infarction area that will worsen the clinical course of a particular patient.To determine the significance of the SB,not only the diameter,length,location and collateral function of the SB but also the symptoms,left ventricular function and viability of the supplied myocardium should be evaluated[13,14].
Pathophysiology of atherosclerosis in CBL
Bifurcations are among the sites most affected by atherosclerotic processes in the coronary tree.In vitroand recentin vivostudies on the anatomy and flow patterns of coronary bifurcations have shown that local flow disturbances and thus endothelial shear stress (ESS) play the most important role in the localization and progression of atherosclerotic plaques[15].ESS is the tangential force caused by the friction of the flowing blood on the endothelial surface[16].The major determinants of ESS are the blood viscosity and the spatial gradient of the blood velocity.Endothelial mechanoreceptors sense ESS;and in response to high ESS,these receptors induce many intracellular signaling pathways resulting in the expression of many atheroprotective genes and suppression of many proatherogenic genes.Conversely,in the case of low or oscillatory ESS,atheroprotective genes are suppressed and proatherogenic genes that promote atherosclerosis are upregulated[15-17].Indeed,in IVUS and autopsy studies of bifurcation lesions,atherosclerosis was most frequently demonstrated in the lateral walls of MVs and side branches where ESS was low and oscillatory and uncommon in the carina where ESS was high[18].Moreover,the carinal angle was found to affect the severity of atherosclerosis as larger angles have been correlated with increased plaque burden[19].This is again explained by the role of ESS since larger angles produce lower and more oscillatory ESS in the lateral walls of the bifurcation vessels.Finally,in addition to its most important role in plaque initiation and progression,low ESS has also been found to be associated with rupture-prone atherosclerotic plaque formation[19].Thus,CBLs have an increased tendency for plaque rupture,platelet aggregation and atherothrombosis[20].
Classification
Various angiographic classifications of CBL have been proposed[21].Because of its simplicity,the easiest to remember and most prevalently used is the Medina classification[22].This classification is established on the presence (“1”) or absence (“0”) of significant stenosis (≥50%) in the proximal main vessel (MV),distal MV and SB in CBLs,respectively (Figure 2).According to this classification,two different types are described:“true” and “non-true “ CBLs.Significant stenosis (≥50%) in both vessels (proximal MV and/or distal MV and SB),i.e.,Medina 1,1,1/1,0,1 and 0,1,1 classes are defined as “true”,while all others are defined as “non-true“ CBLs.“True” bifurcation lesions are more complex and more difficult to treat with poorer outcomes than “non-true“ types[23].However,in true bifurcation lesions,Medina 1,1,1 and 0,1,1 lesions were found to have a higher risk of cardiac death,myocardial infarction (MI),and more SB occlusion than Medina 1,0,1 lesions[23];and only these two classes have been taken as the criterion or one of the criteria of complex true lesions in many bifurcation (especially left main) trials.

Figure 2 Medina classification.
Finally,the Medina classification does not consider other important information that may direct treatment strategies,such as lesion size and length,calcification and bifurcation angles.Therefore,additional modalities such as multislice computed tomography (MSCT),intravascular ultrasound (IVUS),optical coherence tomography (OCT) and fractional flow reserve (FFR) or other functional tests may be necessary to clarify the true classification of a bifurcation lesion and to determine the treatment strategy[24].
PERCUTANEOUS CORONARY INTERVENTION (PCI) TECHNIQUES
Classification
Many stenting techniques have been developed and published.For simplicity,these techniques were classified by the European Bifurcation Club (EBC) as “MADS” in 2008.However,some techniques have been abandoned due to adverse outcomes or lack of effectivity.Therefore,an updated new classification called “MADS-2” was created by the EBC in 2020[25].This classification is based on the location of the first stent implanted (as Main vessel,Across side branch,Double lumen in proximal MV or Side branch).Balloon applications and dedicated bifurcation stent types are added to the original form in this new classification[25].
Although MADS-2 involves many stenting techniques,the most widely used major bifurcation stenting techniques recommended by the EBC are as follows[25]:(1) One-stent techniques:The provisional stenting technique (PST) and inverted provisional stenting technique;and (2) Two-stent techniques (Elective,or bail-out in PST):(a) T/T and protrusion (TAP) stenting;(b) Culotte/inverted culotte stenting techniques;and (c) Double kissing (DK)-crush technique.
Vascular access and guiding catheter selection
In one-stent techniques,most CBLs can be treated transradially or transfemorally using a 6 Fr guiding catheter (GC).However,if a rotablator with a burr size ≥ 2 mm is used or more than two balloons are used simultaneously in the GC,a 7 Fr or larger GC is required[26].Although transfemoral is the most preferred route in this situation,an increasing number of operators prefer the transradial route using slender sheaths or sheathless guiding catheters.
Two-stent techniques can also be performed using 6 Fr GC except when there are two stents in the GC at the same time,such as mini-crush,V or simultaneous kissing stenting techniques[27].
Due to the challenging interventional nature of CBLs,guiding catheters with strong support (such as extra back-up guiding catheters for the left coronary artery and AL 0.75,AL1 or AR2 for the right coronary artery (RCA)) should be preferred[28].
Optimal views for bifurcation lesions[28,29]:(1) Left main coronary artery (LMCA) bifurcation:(a) Working view:RAO caudal (0-30°,25-30°);and (b) Side branch ostium visualization:LAO caudal (30-60°,25-30°),AP caudal (0,45-55°);(2) LAD-first diagonal bifurcation:(a) Working view:RAO cranial (10°,40°);and (b) Side branch ostium visualization:AP/LAO cranial (0-45°,25-70°);(3) For early diagonals:LAO caudal (45-55°,25-30°);(4) LCx-first marginal:(a) Working view:RAO caudal (0-15°,25°);(b) Side branch ostium visualization:AP caudal (0,25°-40°),LAO caudal (45-55°,25-30°);and (5) RCA-PDA/PL:(a) Working view:LAO 35-50°;and (b) Side branch ostium visualization:AP/LAO cranial (0-55°,30-40°).
Which technique should be selected? The PST or the elective double stenting technique?
Most of the randomized comparative trials prior to the mid-2010s showed no difference in major adverse cardiovascular events (MACE) between the PST and elective double stenting (EDS) techniques[26,30,31].Even,lower mortality rates were found for the PST compared to EDS in two recent metaanalyses[32,33].As a result,the provisional stenting technique has been recommended as the default strategy for CBLs in the guidelines and consensus statements for more than 15 years.However,it should be noted that the EDS techniques in these trials and meta-analyses were the culotte,T,and crush techniques.After the introduction of the DK-crush technique,in 2011,Chenet al[34] showed that there was a significant reduction in target lesion revascularization (TLR) and target vascular revascularization (TVR) rates in favor of the DK-crush techniquevsthe PST with no MACE differences in complex true bifurcation lesions in the DKCRUSH II trial.Later,the DKCRUSH III trial showed that the culotte stenting technique was worse than the DK-crush technique in terms of MACE in patients with unprotected left main (LMCA) bifurcation lesions[35].Moreover,the DKCRUSH V study presented in 2017 found a lower rate of target lesion failure (TLF) at 1 year with the DK-crush technique than with the PST in complex true LMCA bifurcation lesions[36].
Recently,the 3-year outcomes of the DKCRUSH V trial were published and confirmed the one-year results and additionally showed a reduction in the stent thrombosis rate in favor of the DK-crush technique[37].Crimiet al[38] found that the DK-crush technique lowered device-oriented clinical events (defined as a composite of cardiac death,target-vessel MI,stent thrombosis and TLR or TVR)vsthe PST and other EDS techniques in their recent meta-analysis.In another concurrent network meta-analysis,Di Gioiaet al[39] showed that TLR was significantly lower with the DK-crush technique than with the PST and other EDS techniques with no differences in cardiac death,MI or stent thrombosis rates.In addition,in this meta-analysis,a clinical benefit was observed with EDS techniques over PST in CBL with SB lesion lengths ≥ 10 mm.In the recently published DEFINITION II trial,complex bifurcation lesions were defined by the sum of various criteria,as shown in Table 1.In this trial,the EDS technique (DK-crush 77.8%,culotte 17.9%,and other 4.3%) provided a significant reduction in TLF (mainly driven by target vessel MI and clinically driven TLR) compared to the PST in the defined complex bifurcation lesions at one year[40].
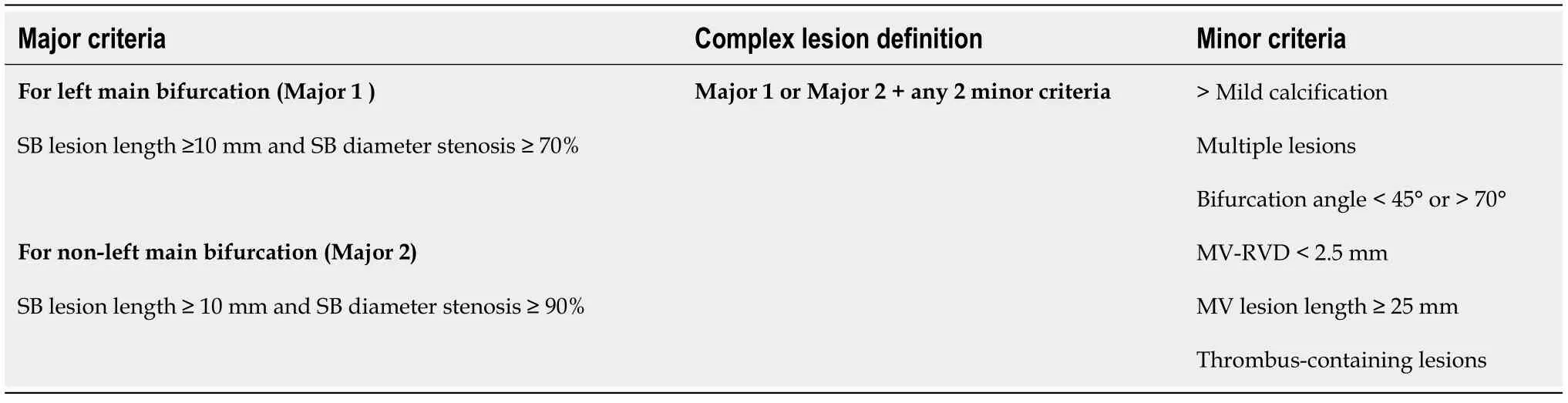
Table 1 DEFINITION criteria for a complex coronary bifurcation lesion[40]
Despite the favorable results of the DK-crush technique in randomized studies and two metaanalyses,the recent guidelines still recommend the PST as the default strategy for complex CBLs and a class IIb indication for the DK-crush technique over the PST in true LMCA bifurcations[25,41-43].The reason for this may be some reservations that have been described[30]:(1) The DK-crush technique has multiple steps and is a challenging technique;(2) The DKCRUSH trials mostly come from the same group of interventional experts who have performed this procedure for many years;and (3) The PST results in these trials were worse than previously published ones,which might be associated with a high SB stenting rate (29%-47%) due to the high rate of long SB lesions (mean 15-17 mm).
When deciding between the PST and EDS,the high risk of SB occlusion should also be considered,as SB occlusion may result in serious adverse clinical outcomes[44].SB occlusion predictors by angiography,IVUS and OCT have been described recently[44,45].Angiographically,plaque on the same side of the SB,SB stenosis > 50%,POC stenosis > 50%,bifurcation angle > 70%,MV/SB diameter ratio (diameter of PMV+DMV/2×diameter of SB) > 1 and a low MV TIMI flow grade were found to be predictors of SB occlusion after MV stenting.A risk score was described based on these predictors[44].According to this risk score,higher stenosis rates,larger bifurcation angles,larger MV/SB diameter ratios,a lower TIMI flow grade,and more predictors result in higher SB occlusion rates[44].
The recently published EBC-MAIN study,which compared the PST and EDS techniques in LMCA bifurcation lesions,showed that there were fewer MACE in the PST than EDS,although the difference was statistically insignificant.The authors consequently recommended the PST as the default strategy for LMCA bifurcation lesions.However,it should be noted that the DK-crush technique was used in only 5% of the EDS patients in this trial.In addition,the mean lesion lengths of the side vessels were not long:5.8 cm and 7.9 cm in the PST and EDS patients,respectively[46].
Consequently,for non-true CBL,the default strategy is the PST[47].In true complex CBL (Medina 1,1,1 or 0,1,1),if the SB is ≥ 2.5 mm and the SB lesion length ≥ 10 mm or the likelihood of SB occlusion is high or SB wiring is difficult,it is better to choose EDS;otherwise,the PST is preferred[38,39,41,45,48].In true non-complex CBL (Medina 1,0,1),the inverted PST may be an appropriate treatment if there is no large difference between the SB and the PMV diameter[42];otherwise,and in the case of the above risks,EDS may be preferred[39,45,48,49].A proposed algorithm for choosing between the PST/inverted PST and the EDS technique is shown in Figure 3.
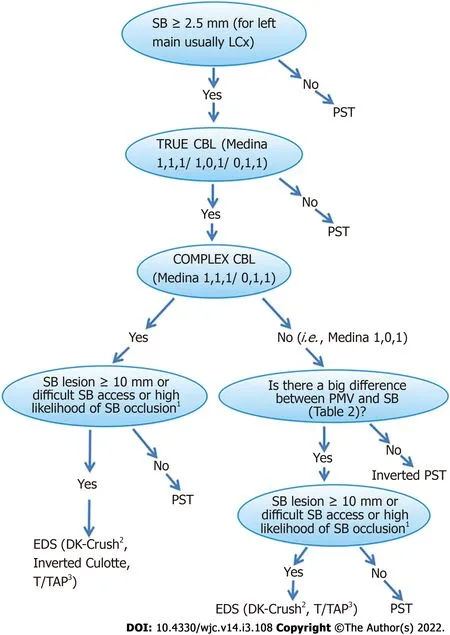
Figure 3 Proposed algorithm for selecting an optimum percutaneous coronary intervention strategy in both left main coronary artery and non-left main coronary artery bifurcation lesions.
The ongoing BBK3 trial will provide more data on the outcomes of the PST or EDS techniques in non-LMCA bifurcation lesions[50].
The choice between the different EDS techniques depends partially on the bifurcation angle.The T technique can only be applied at bifurcation angles very close to 900[25].The TAP technique can be performed at bifurcation angles from 70°-90°.Culotte/inverted culotte stenting and the DK-crush techniques (unlike the crush technique) can be implemented regardless of the bifurcation angle[51,52];however,applying the culotte technique at < 70°angles gives better results[35].If the bifurcation angle is from 70°-90°,due to simplicity and familiarity,an increasing number of operators are using the T/TAP technique not only when a second stent is required in the PST[53] but also in the EDS technique as the first-line therapy and perform the culotte/inverted culotte or DK-crush techniques if the angle is < 70°[41,54].
In conclusion,in view of recent data,the DK-crush technique may be preferred over the other twostent techniques regardless of the bifurcation angle;however,it is a complex procedure with many steps,and the operator’s familiarity with a particular technique is an important factor in the choice of which EDS technique to perform and in obtaining the best result[45].
PST
The step-by-step PST is shown in Figure 4.
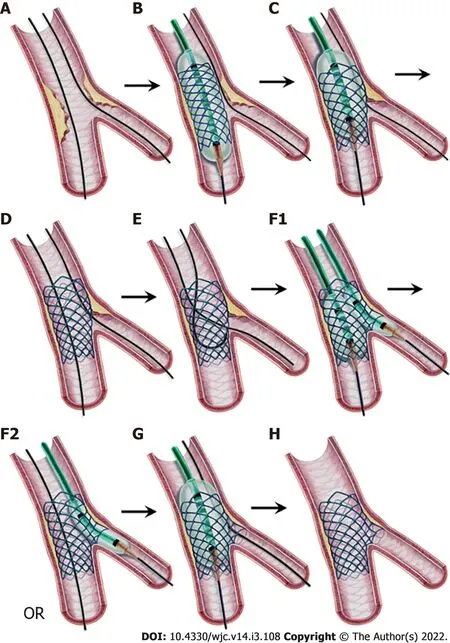
Figure 4 Provisional stenting technique,step-by-step.
Wiring the vessels
In addition to the MV,the SB should also be wired in all CBLs.This wire helps to prevent SB occlusion after MV stenting,serves as a marker in case of SB occlusion,widens the angle between the PMV and SB for easier access,enhances support of the guiding catheter,and finally can be used as a rescue balloon guidewire that will be described later.To prevent the two wires from wrapping,the more difficult vessel (mostly the SB) should be wired first,and the second wire should be inserted without much manipulation.
Wire types and shaping
The types of wires are left to the operator’s preference.Any type of wire (hydrophilic with or without polymer coating and hydrophobic) can be used[55,56].One necessary point is not to jail the radiopaque tip part of the wire in the SB ostium during MV stenting.
Both wires should be ready for the exchange technique if needed after MV stenting.To accomplish this,the MV guidewire tip should be angled so that its length will be longer than the proximal MV reference diameter to reach the SB ostium.A 1-1.5 mm secondary bend can also be added to the tip to hook the struts of the MV stent[57].The SB wire should be prepared as a sharp angled short tip that will make it easier to create a “U” shape to pass through the MV stent during wire exchange[58].The MV wire should not be pushed too distally in order to maintain the shape of the tip for exchange and to reduce the risk of distal perforation or dissection that can occur during many maneuvers.
Troubleshooting SB wiring problems
SB wiring may be difficult in the following circumstances:a bifurcation angle greater than 70°-90°,severe ostial SB stenosis,MV stenosis or severe calcifications in the proximal MV and/or ostial SB.In addition,tortuosity before or at the SB take-off may flatten or change the angle of the wire,resulting in difficult SB wiring[58].
Possible solutions for solving the SB wiring problem are the following[52,58]:(1) If the problem is wide angulation,a wide smooth bend or double bend shape given to the tip can help;(2) The workhorse wire can be replaced with a stiffer or hydrophilic polymer-coated wire.Stiffer wires are preferred first because hydrophilic wires can easily go subintimally and cause dissection or perforation;(3) Pull-back wire technique:A wide smooth bent or double bent wire is advanced into the DMV and pulled back to intubate the SB ostium.After intubating,a gentle counterclockwise rotation allows the wire to advance in the SB;(4) Reverse wire technique:When the SB has an excessively angled take-off (greater than 90°),a polymer-jacket wire with a 3-5 cm tip bent 180°,like a hairpin,is used in this technique (Figure 5).The wire is advanced in the DMV and pulled back to the bifurcation,and an attempt is made to enter the SB ostium.After intubation,the wire is gently withdrawn and gently rotated counterclockwise to allow the wire to advance in the SB;(5) A dual lumen microcatheter,a steerable-tip microcatheter (Venture,Teleflex,Wayne,PA,United States) or an angled microcatheter (SuperCross 45-90-120°-XT,Teleflex) can be used to direct the wire to the SB;(6) When there is a large plaque burden that prevents wiring the SB,debulking techniques such as rotational/orbital atherectomy or laser may be used;(7) Balloon dilatation of the MV to modify the plaque is performed by many operators as a last effort.However,it can cause plaque and/or carina shift,resulting in SB occlusion;and (8) Finally,if the SB cannot be wired,the decision to abandon the procedure can be made based on the patient’s clinicopathological condition.
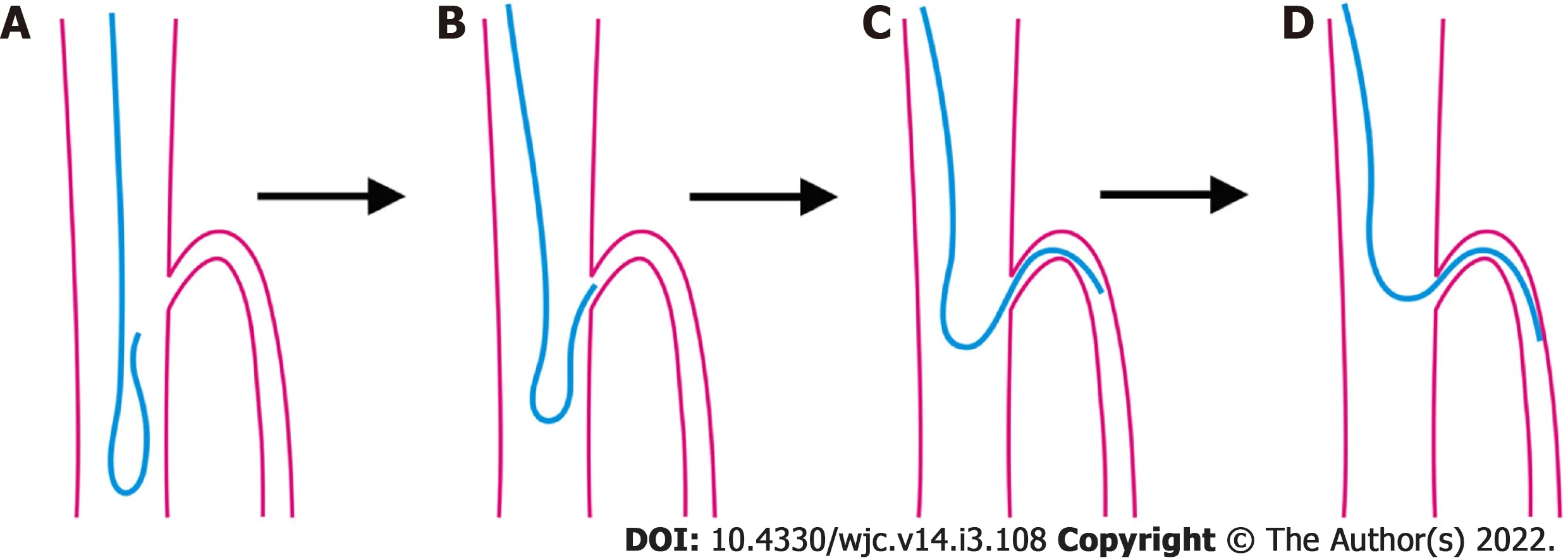
Figure 5 Reverse wire technique.
Predilation of the MV and the SB
Optimal preparation of the MV is necessary before stenting.Therefore,the operator can decide to predilate the MV and/or perform any debulking procedure according to the MV lesion properties.
Routine predilation of the SB has been a controversial issue in the PST.Predilation aims to prevent SB closure after MV stenting;however,it can cause dissection that may prevent guidewire advancement during wire exchange or may require an extra stent in the SB.A prospective randomized study showed that SB predilation resulted in improved flow with less need to treat the SB[59].However,another double-blind smaller randomized study and a recent meta-analysis of eight trials demonstrated the opposite:SB predilation increased SB intervention rates and made no difference in procedural angiographic and long-term major cardiovascular outcomes[60,61].Consequently,it seems that routine predilation of the SB cannot be recommended currently.Conditions that favor SB predilation with an undersized non-compliant balloon are severe ostial SB narrowing,extensive SB calcification,difficult SB access or decreased flow after MB predilation and/or debulking[14,49].
When the SB is predilated,the angiographic result should be carefully evaluated before MV stenting.In situations where the SB is compromised,such as dissection or difficult SB access,the operator should be ready to change the stenting strategy to another strategy,such as the inverted PST or the DK-crush technique[49].
Newer side branch protection techniques
To prevent side branch occlusion during the PST,various novel techniques have been developed recently:the pre-kissing technique,jailed balloon,jailed semi-inflated balloon and modified jailed balloon techniques.The pre-kissing technique involves the simultaneous dilation of two undersized balloons (one in the MV and the other in the SB) whose proximal parts are aligned in the proximal MV before MV stenting.The aim of this technique is to sustain the central position of the carina while moving the atherosclerotic plaques away.Using first-generation drug eluting stents (DESs),this technique was shown to reduce SB-related complications in a small retrospective study[62].
The jailed balloon technique (JBT) and the jailed semi-inflated balloon technique (JSBT) involve implanting an MV stent while a semi-compliant balloon is in the SB protruding to the MV.The proximal marker of the SB balloon is positioned to align or 1-2 mm proximal to the marker of the MV stent (Figure 6).The SB balloon is uninflated (JBT) or inflated to low or moderate pressure (< 3 to 7 atm) (JSBT) during MV stent balloon inflation at nominal pressure.After MV stent implantation,if the SB flow is not compromised (i.e.,TIMI-3 flow),the uninflated SB balloon is inflated at low (< 3 atm) pressure in the JBT (not shown in Figure 6).If less than TIMI-3 flow in the SB is observed,the SB balloon is inflated at nominal pressure.After the balloons are removed,the proximal optimization technique (POT) is performed in the PMV[63,64].
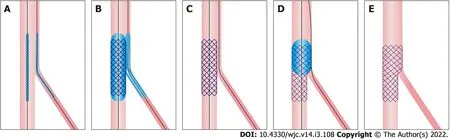
Figure 6 Jailed balloon technique and jailed semi-inflated balloon technique.
In the modified jailed balloon technique (M-JBT),the MV stent is positioned across the SB,and a balloon is placed in the SB with its proximal end touching the MB stent (Figure 7).Both the MV stent and SB balloon are inflated at the same nominal pressure (e.g.,12 atm) simultaneously.After deflation and removal of the balloons,the POT is performed in the PMV[65].
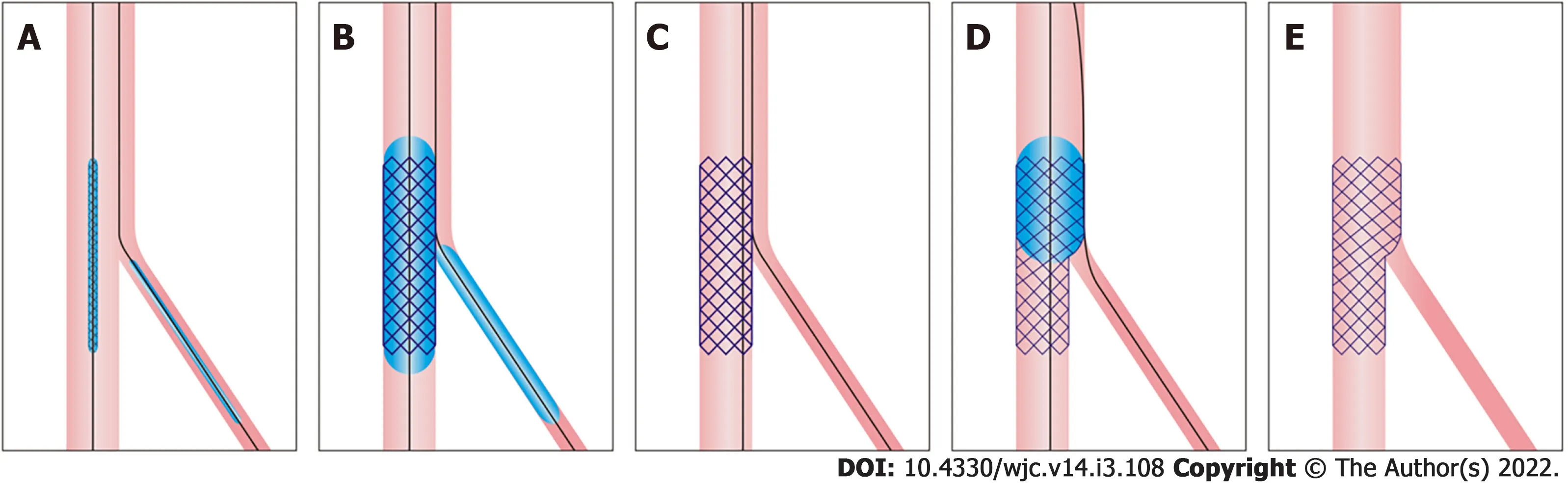
Figure 7 Modified jailed balloon technique.
All three JBTs,the jailed semi-inflated balloon technique and the M-JBT were investigated in smallsized trials and found to have low SB loss,SB dissection and MACE rates[66,67];however,larger randomized controlled trials are required for the routine use of these new techniques in the PST.
MV stenting
The preferred type of stent is new-generation DESs which reduce the risk of restenosis and repeat interventions compared to bare metal stents and early-generation DESs[68,69].The diameter of the MV stent should be chosen at a 1:1 ratio according to the reference distal MV size (Figure 4B).The implantation of a larger stent can cause distal dissection and carinal shift,which can result in severe narrowing or even occlusion of the SB.The length of the stent should be selected so that its PMV part will be equal to or longer than the shortest balloon available (usually 6-8 mm) for the subsequent POT[25,48].The stent should be implanted at nominal pressures,avoiding overexpansion,which is called the “distal optimization technique” (called “DOT” in the literature)[53].
POT
Since the diameter of the MV stent is chosen according to the diameter of the DMV,a semi-compliant or non-compliant balloon sized to the PMV diameter should be inflated in the PMV stent part to correct malapposition[25] (Figures 4B and 4C).The distal shoulder of the balloon (the point where balloon parallelism ends) should be aligned to the level of the carina so as to avoid stent underexpansion at the polygon of confluence (occurs when placed more proximally) and carinal shift (occurs when placed more distally)[70].Many operators use the distal balloon marker as the distal shoulder;however,as the location of this marker varies between manufacturers,the operator should be familiar with the design of the balloon used to avoid misplacement[49,71].The POT corrects the malapposition of the stent in the PMV,prevents understrut passing of subsequent wires,provides strut protrusion into the SB and widens the distance between struts in the SB ostium which facilitates subsequent wire and balloon passing into the SB.
When the POT balloon is shorter than the PMV stent part,the POT must be applied to the entire PMV stent part.Furthermore,the POT balloon should not be longer than the PMV part of the stent;otherwise,it can cause proximal stent edge dissection.
Finally,the overexpansion capacity of the available stent types should be known to select the correct stent in order to provide natural fractal anatomy of the coronary bifurcation with the POT [72] (Table 2).
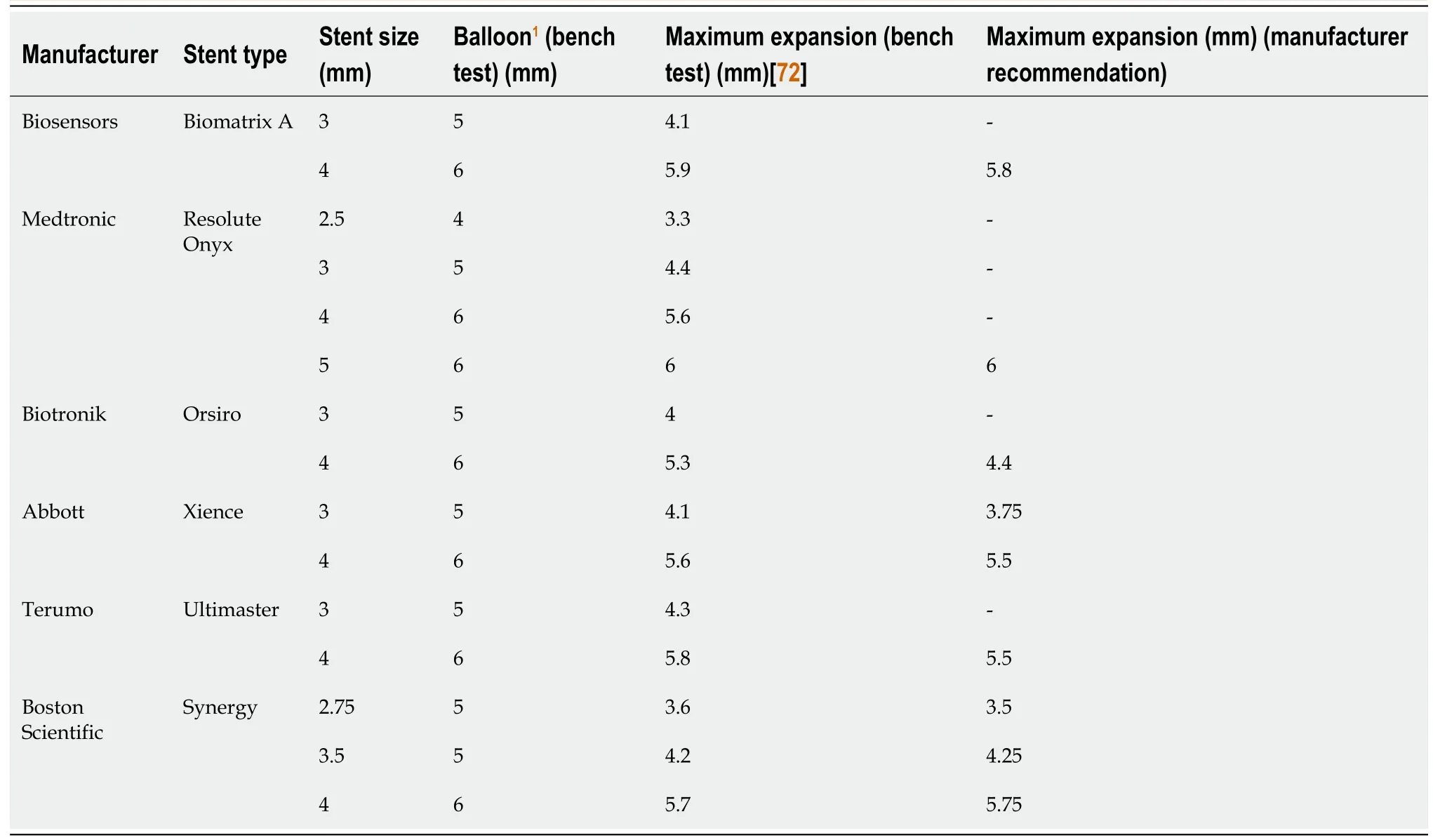
Table 2 Maximum-expansion capacity of stents
Is routine kissing balloon inflation or POT-side-POT technique necessary after the first POT?
KBI involves the inflation of two non-compliant balloons (one in the MV and the other in the SB) whose proximal parts are aligned in the proximal MV.The aim of this procedure after MV stenting is to remove the stent struts at the SB ostium,to eliminate the stenosis in the SB,and to maintain the carina in its central position.
In a recent meta-analysis,routine final KBI resulted in a significant reduction in SB restenosis,but an increase in MV restenosis rates with no significant differences in clinical outcomes[73].Another recent larger meta-analysis of final KBIvsno-final KBI in PST trials also showed similar results in that there was no difference in terms of MACEs and other outcomes[74].
SB dilatation to open the struts at the ostium of the SB after MV stent implantation was shown to cause stent distortion with malapposition of struts at the opposite side of the SB ostium in bench studies[75,76].Therefore,the POT or KBI should be performed to correct this distortion[71,75,76].POT-side-POT is a new technique that involves initial POT + SB balloon dilatation + final POT (or re-POT) and will be described later.
Presently,there are no convincing data for KBI and insufficient data for the POT-side-POT technique to recommend either of them for routine use after the first POT in PST.
When should we treat the SB after the POT?
After the POT,if the SB flow is TIMI-3 and there is < 75% stenosis in the ostium,or no dissection,then the operation is completed.
After MV stenting,the MV plaque and/or carina shift can create an angiographic image of SB ostial narrowing.However,angiography is unreliable with regard to the functional significance of SB stenosis in this situation.It was shown in a study that none of the < 75% and only 27% of the SB stenoses ≥ 75% were found to be significant with the FFR[77].This situation can be explained by the oval shape of the SB ostium (the narrower the carinal angle,the more oval the ostium) (Figure 8),the edge effect originating from angiography[57] and the recently shown elliptical stretch of the SB ostium after MV stenting[78].
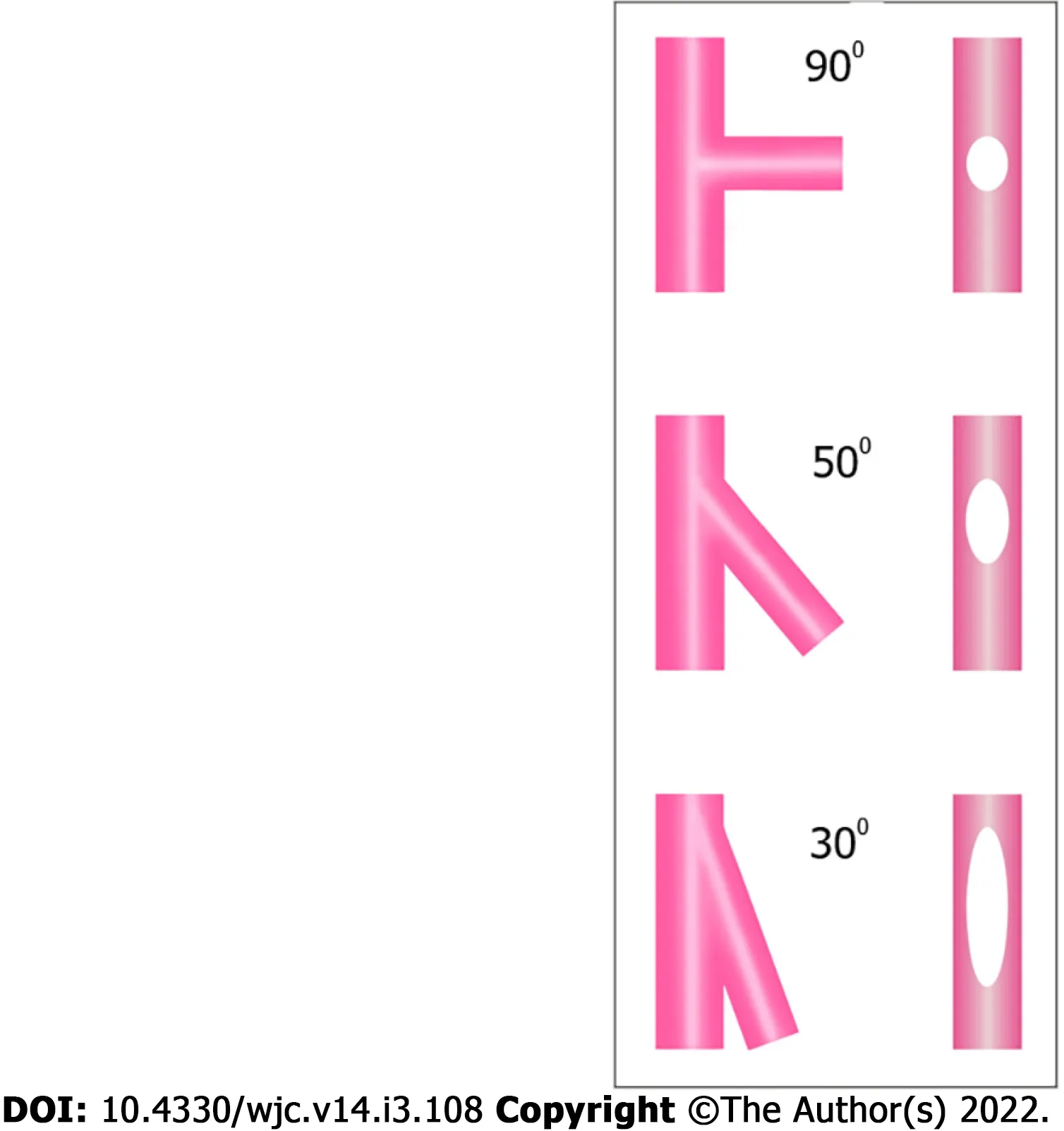
Figure 8 Effect of bifurcation angle on side branch ostium ellipticity.
Consequently,severe stenosis (≥ 75%) in the SB ostium,FFR ≤ 0.8,less than TIMI-3 flow or dissection in the SB requires SB intervention.
Technical steps of SB intervention after the POT
If the SB requires intervention after MV stenting and the POT,the sequential techniques and technical steps are as follows:
Guidewire exchange technique:The MV wire tip is pulled to the level of the carina and tried to pass into the SB through the most distal cell of the MV stent (carinal cell) at the SB ostium (Figure 4E).The passing of the wire through the distal cell is very important in the PST as subsequent balloon inflation will direct the struts to the non-carinal ostial segment of the SB,providing better scaffolding[26].The jailed SB wire should not be retracted until the MV wire passes into the SB,since this wire indicates the SB ostium location and can be used when a rescue balloon is required as described next.
If the wire cannot be passed through the stent struts into the SB,the following options are available:(1) It can be reshaped;(2) The POT with a larger balloon can be performed again to open the cells and remove the struts at the SB ostium;(3) A hydrophilic polymer-coated or a stiffer wire can be used;(4) A steerable-tip microcatheter (Venture,Teleflex),an angled microcatheter (SuperCross,Teleflex) or a dual lumen microcatheter can be used;and (5) Finally,a small balloon (1-1.5 mm) can be passed through the jailed wire under the stent struts and dilated at the ostium of the SB,which not only rescues the SB in case of occlusion but also allows the MV wire to enter the SB[26].In extreme cases,the inverted crush technique can be implemented as a last effort to rescue the occluded SB.
After the MV wire is inserted in the SB,the jailed SB wire is withdrawn until it comes out under the stent struts and is then pushed forward into the stent.At this time,the tip should be formed into a “U” shape to easily cross the MV stent,avoiding passing under the struts (Figure 4E).While the jailed SB wire is being retracted,the guiding catheter may intubate deeply into the vessel,which can cause dissection and longitudinal stent deformation in the case of LMCA stenting[26].Therefore,the guiding catheter tip should be withdrawn a few mm into the aorta beforehand;and while retracting the wire with right hand,the operator should control the guiding catheter with left hand while closely monitoring its tip[26].
Rarely,the jailed wire cannot be easily removed under the struts.In this case,a small balloon passed over the jailed wire with or without inflation at the jailed site may help.
Instead of the wire exchange technique,a third wire can be used to pass into the SB while the jailed wire is in place.The third wire is advanced into the DMV and then retracted back,and an attempt is made to enter through the most distal cell.
Kissing balloon inflation technique:After exchanging the wires,a non-compliant balloon sized to the SB diameter is inserted into the SB,and another non-compliant balloon sized to the DMV diameter is inserted into the MV.The balloons should be sufficiently short to prevent inflation outside the MV stent and disease-free regions in the SB.Moreover,minimal balloon overlap is recommended to keep elliptical stent deformation in the PMV to a minimum (Figure 4F1)[25,79].First,the SB balloon is inflated at a high pressure to open the struts and eliminate the stenosis;and after deflation,the MV balloon is inflated to a high pressure.Subsequently,to maintain the carina in its central position,simultaneous inflation and deflation of both balloons is conducted using moderate pressures (at approximately 8-10 atm) as high pressures cause more oval distortion in the PMV segment of the stent[25].
A modified kissing balloon inflation (KBI) technique investigated in a bench test study was described by Mortieret al[80].In this technique,the SB balloon is inflated to 12 atm and deflated to 4 atm.Then,the MB balloon is inflated to 12 atm;and finally,both balloons are deflated simultaneously.This technique was found to cause less elliptical stent deformation of the PMV segment with optimization of SB access compared to KBI with 12 atm inflation and deflation of both balloons simultaneously.
After KBI,to correct the oval (elliptical) stent deformation in the PMV segment,the POT should be performed again,which is termed the re-POT or final POT.In a recent bench test study,the position of the re-POT balloon was found to be an important factor in the alteration of the SB cell area size of the MV stent.The distal shoulder of the balloon positioned across the SB takeoff caused a reduction in the SB cell area whereas the distal shoulder positioned proximal to the SB takeoff did not[71].The results of futurein vivotests and clinical studies of this approach are needed.
Balloon crossing problem to the SB:If the balloon does not cross to the SB through the stent struts,the following steps are performed[26,51]:(1) The first step is to check the position of the guiding catheter to determine whether it is at the ostium and coaxial to the vessel;(2) The second step is to use a smaller or the smallest balloon (1-1.5 mm) available;(3) It is suspected that the two wires are wrapped if the balloon cannot be forwarded to the SB ostium or if the MV wire is observed coming back while pushing the balloon.In this case,the MV wire is withdrawn back to the GC and inserted again into the DMV;(4) The next step is to inflate a balloon in the DMV stent part to increase the support of the GC (the anchorballoon technique);(5) Performing the re-POT with a larger balloon to open the cells at the ostium of the SB is another choice;(6) Some operators advance a small balloon until it stops at the SB ostium,inflate it at high pressure with the objective of opening the struts,and then try to advance the balloon while deflating it[81];and (7) As a last effort,the SB can be rewired from a different stent cell.
POT-Side-POT technique:After the first POT and exchanging wires,instead of the KBI,the POT-Side-(re)POT technique was proposed as an alternative and is increasingly used[82-84].Technically,after the first POT,a balloon sized to the SB diameter is dilated in the SB to eliminate stenosis and remove the struts at the ostium,followed by the re-POT (Figures 4F2 and 4G).Because only one balloon is inserted and inflated at a time,this technique can be performed with 5 Fr guiding catheters,requires only one indeflator,and permits more proper balloon positioning.In a small recent clinical prospective registry using optical coherence tomography (OCT),the global strut malapposition,ellipticity index and SB occlusion rates were significantly reduced with a good sixth-month safety outcome[83].
Inverted PST
In Medina 0,0,1 bifurcation lesions with a very large SB (for ex.,ostial circumflex or ostial diagonal lesion),a stent from the PMV to the SB may be implanted.This is called the “inverted PST”[25].In addition,if there is no large difference between the PMV and the SB,this technique can also be performed in Medina 1,0,1 Lesions (Figure 3).The technical steps are the same as for the PST.The only difference is that the DMV is considered the SB and the SB is considered the DMV.
SIDE BRANCH STENTING FOLLOWING THE PST
After KBI or POT-side-POT techniques,if there is dissection,TIMI flow grade < 3 or FFR ≤ 0.8 in the SB,a second stent is required.Since there is a poor correlation between angiography and FFR measurements,when there is a suspicion of severe stenosis in the SB ostium after PST,it is better to use FFR to decide on SB stent implantation[14].
T/TAP stenting techniques
These stenting techniques are the simplest methods of second stent implantation in the PST.If the bifurcation angle is very close to 90°,then implanting a second stent in the SB as a “T form” is suitable.Technically,optimal angiographic views of the SB ostium should be obtained and stent augmentation tools should be used for successful T stenting[25].
Bench test studies and clinical practice have demonstrated that the bifurcation angle is usually not 90°;thus,the second stent may not completely cover the SB ostium with the T stenting technique,resulting in increased restenosis rates[25].Therefore,the TAP stenting technique was developed.The TAP technique allows complete coverage of the SB ostium at the cost of creating a metallic neocarina.The length of the metallic neocarina depends on the bifurcation angle;the narrower the bifurcation angle is,the longer the length of the neocarina.For this reason,the TAP technique is generally not recommended at bifurcation angles < 70°.
The technical steps of the TAP technique in the PST are as follows[25] (Figure 9):(1) After the MV stenting and exchanging wires,the SB ostium is dilated with a balloon;(2) A DES of the SB diameter and appropriate length is positioned in the SB;(3) A balloon sized to DMV diameter is placed uninflated in the MV for use in subsequent KBI;(4) The SB stent is implanted with great care so that the non-carinal ostium is completely covered with minimal protrusion in the carinal segment (Figure 9B);(5) After the implantation of the SB stent,the stent balloon is slightly withdrawn and inflated at high pressure to provide optimum stent expansion in the SB ostium and postdilation of the stent (Figure 9C);(6) The uninflated,parked MV balloon and SB stent balloon are aligned in the PMV.Simultaneous KBI at moderate pressure and deflation are implemented to hold the neocarina in a central position;and (7) As a last step,the re-POT is performed to correct the oval shape if KBI has been implemented in a long segment in the PMV;otherwise,this step is not mandatory.It is of upmost importance that the re-POT balloon should not reach the metallic neocarina (Figure 9E).If this happens,the neocarina can bend to the SB side,which can result in rejailing and reduction in the SB ostial cell area[71].
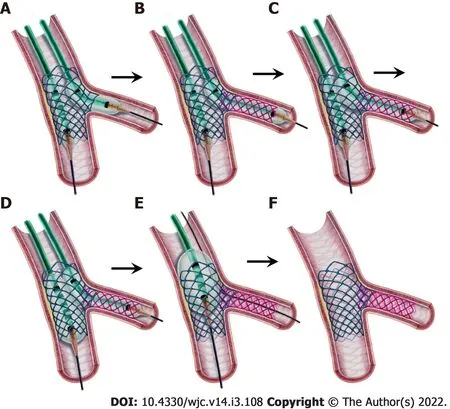
Figure 9 Step-by-step T and protrusion technique.
Culotte stenting technique in the PST (classical culotte technique)
TAP is the most often used technique in the PST due to its simplicity;however,when the bifurcation angle is less than 70°,some operators prefer to use the culotte technique first introduced by Chevalieret al[85].The culotte technique provides full coverage of the bifurcation;however,two layers of struts in the PMV are the disadvantage of this technique.Furthermore,before deciding to perform this technique,the overexpansion capacity of the available stent types should be known (Table 2)[72].If the maximum expanded diameter of the available SB stent is less than the diameter of the PMV according to the table,then the culotte technique cannot be performed.This is especially the case when there is a large difference between the PMV and SB diameters.
The technical steps of culotte stenting in PST are the following[25] (Figure 10):(1) After the stages of the PST are completed (Figures 10A-C),wire exchange and balloon dilatation of the SB ostium is performed (Figures 10D and E);(2) A DES with the same diameter as the SB and an appropriate length that extends from the SB to overlap the proximal part of the MV stent is implanted while the MV wire is in place.The overlap part is long in the classical culotte technique but is kept at 1-3 mm in the “miniculotte” technique (Figure 10F);(3) A new POT is performed through the SB wire with a non-compliant balloon sized to the PMV.The balloon distal shoulder should be aligned to the carinal level (Figure 10G);(4) Wire exchange should be performed for the second time.It should be noted that the SB wire must be passed from the cell closest to the carina into the DMV (Figure 10H).This allows the deployed SB stent struts to move to the lateral walls of the MV rather than the carina and the SB ostium during the next balloon inflation.The MV wire is retracted under the SB stent and advanced into the SB as a “U” shape;(5) A non-compliant balloon sized to the DMV and another non-compliant balloon sized to the SB are advanced into the relevant vessels,and the proximal balloon markers are aligned in the PMV.Each balloon is inflated at high pressure and deflated sequentially,followed by KBI at moderate pressures (Figure 10I);and (6) A last POT should be performed for correcting the oval shape created by previous KBI (Figure 10J).
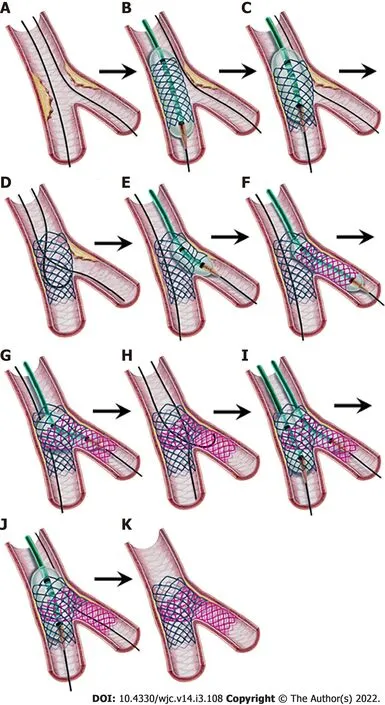
Figure 10 Step-by-step classical (provisional) culotte stenting.
ELECTIVE DOUBLE STENTING TECHNIQUES
Inverted culotte stenting technique
To maintain access to the SB during the procedure,the culotte stenting technique was modified to the “inverted culotte stenting technique” in elective double-stent implantation.Similar to the culotte technique,the inverted culotte technique provides full coverage of the bifurcation at the expense of two layers of struts in the PMV,and it cannot be performed when there is a large difference between the PMV and SB diameters.
The technical steps of inverted culotte stenting are as follows (Figure 11):(1) Both branches are wired,and MV predilation and/or debulking is performed with predilation of the SB;(2) A stent sized 1:1 to the SB diameter is deployed in the SB protruding into the PMV.The length of the stent is selected so that the PMV part is sufficiently long enough for the subsequent POT.In the “mini-culotte technique“ introduced a decade ago,the PMV part of the SB stent is kept as short as 1-3 mm to reduce the length of the two stent layers[86,87] (Figure 11B).This technique was found to be associated with high procedural success and very good 9-month outcomes in a pilot study[88].Randomized,controlled,larger comparative studies are needed to confirm the favorable outcomes of this method;(3) The PMV part of the stent is dilated with a non-compliant or semicompliant balloon sized to 1:1 to the PMV diameter.This is the first POT (Figure 11C);(4) Wire exchange (or a third wire advancement) should then be performed.The DMV should be wired from the closest cell to the carina for the reasons described above (Figure 11D);(5) Stent struts are opened by a DMV balloon.Instead,KBI,which is part of the recently introduced “DK-culotte technique”,can be performed[89,90] (Figure 11E).This technique was found to achieve better morphological properties than classical culotte stenting in a bench test study[89],and it reduced the total procedural time with better strut apposition than the culotte and even the DK-crush techniques in another study[90];(6) An MV stent sized 1:1 to the DMV diameter is advanced and implanted.The length of the PMV part should be sufficient to cover the PMV part of the SB and be at least equal to the shortest POT balloon (Figure 11F);(7) A second POT is performed in the PMV (Figure 11G);(8) A second wire exchange is performed by passing the MV wire through the closest cell to the carina into the SB and the U-shaped SB wire into the DMV (Figure 11H);(9) KBI is performed with short non-compliant balloons sized 1:1 to the branches.Before KBI,sequential balloon inflation is recommended.The SB balloon is first inflated to a high pressure;and after deflation,the MV balloon is inflated to a high pressure.Then,both balloons are inflated at moderate pressures (at approximately 8-10 atm) and deflated simultaneously (Figure 11I).A recent mini-KBI in culotte stenting was described in a bench test study[91].In this technique,the SB balloon only protrudes into the MV at the upper edge of the SB,and the KBI is performed.Compared to classical KBI,this modification significantly prevented stent deformation and overexpansion in the MV stent and provided better apposition of the MV stent and better expansion of the SB stent[91];and (10) A final POT is performed in the PMV (Figure 11J).
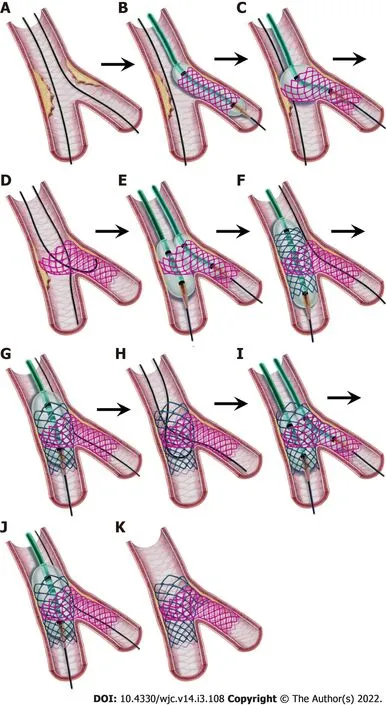
Figure 11 Step-by-step inverted culotte stenting.
Double-kissing crush technique
The crush technique was first introduced by Colomboet al[92].The aim of this technique was to provide full coverage of the ostium to lessen SB restenosis with immediate patency of both branches.However,in clinical practice and in trials,the rate of achievable KBI was found to be low,leading to suboptimal long-term outcomes.Thus,this technique is no longer recommended[49].Some modifications of this technique,such as “mini-crush”[93],“step-crush”[94],and “double-kissing (DK) crush”[95] were described.As described before,the DK crush technique has received great attention due to its high final KBI success rate and its efficacy with long-term safety in complex bifurcation lesions in a series of trials[25,34-36,96].Nonetheless,this technique is complex with many steps that require proper training and experience.
The technical steps of the contemporary DK-crush technique are as follows[25] (Figure 12):(1) After wiring the two branches,optimal preparation of the MV with balloon inflation and/or debulking with predilatation of the SB is performed;(2) A DES,sized to the SB diameter and with a length to ensure full coverage of the SB lesion,is advanced into the SB.The stent is positioned protruding 2-3 mm into the PMV (Figure 12A);(3) A balloon sized to the PMV is positioned in the MV to crush the stent later.This balloon will be kept uninflated until the crushing procedure (Figure 12A);(4) After the SB stent is implanted,a new method called the “proximal side optimization” described by Lavarra[97,98] and considered useful by the EBC[25] may be performed.In this method,the stent balloon is slightly withdrawn and inflated at 4-6 atm higher than the nominal pressure (Figure 12B);and after removing this balloon,a new NC balloon (0.25-0.5 mm larger than the SB stent) is again inflated in the protruding part of the stent and the SB ostium (Figure 12C).The purpose of this method is to achieve adequate expansion and apposition of the SB stent in the ostium and to provide a larger stent cell area for rewiring;(5) After the SB balloon is removed,angiography should be performed to evaluate the results of SB stent implantation,such as the stent expansion,flow pattern,distal dissection or new lesion development.If an additional stent is required,it should be implanted at this time as the SB wire will be removed in the next step and rewiring and stent advancement may be challenging in later steps[99];(6) The SB wire is removed (some operators leave it in),and the pending uninflated MV balloon is positioned with its distal shoulder aligned to the carina.High-pressure inflation (POT) is performed to crush the protruding part of the SB stent,which is called “balloon crushing”[25].It was demonstrated in bench tests that the POT is required to achieve total crushing.(Figure 12D);(7) The SB is rewired through anon-distalcell of the crushed stent (Figure 12E).Non-distal cell rewiring,the opposite of distal rewiring in the PST,is important because more frequent suboptimal KBI results and higher SB stent restenosis were found with distal wiring[100].The mechanism of this is explained by the fact that the KBI in the distal cell pushes the stent struts to the proximal side,causing incomplete coverage of the distal 1/3 of the SB ostium[100].How to overcome wiring problems is explained in the relevant section of the PST;(8) An SB balloon sized 1:1 to the SB diameter and an MV balloon sized 1:1 to the DMV diameter are advanced.To perform the first KBI,the SB balloon is inflated at high pressure to open the struts;and after deflation,the MV balloon is inflated at high pressure.Eventually,simultaneous inflation and deflation of both balloons with moderate pressures (at approximately 8-10 atm) is conducted (Figure 12F).How to overcome balloon crossing problems is explained in the relevant section of the PST;(9) The two balloons and the SB wire are removed.A DES sized 1:1 to the DMV diameter is positioned across the SB covering all the distal and proximal MV lesions and deployed (Figure 12G).The PMV part of the DES should be at least equal to the shortest POT balloon;(10) After removing the stent balloon,a repeat POT with a balloon sized 1:1 to the PMV diameter should be performed
(Figure 12H);(11) The SB is rewired again through a non-distal cell (Figure 12I);(12) A second KBI is performed (Figure 12J);(13) A final POT is performed to correct the oval shape of the PMV created by the previous KBI (Figure 12K).
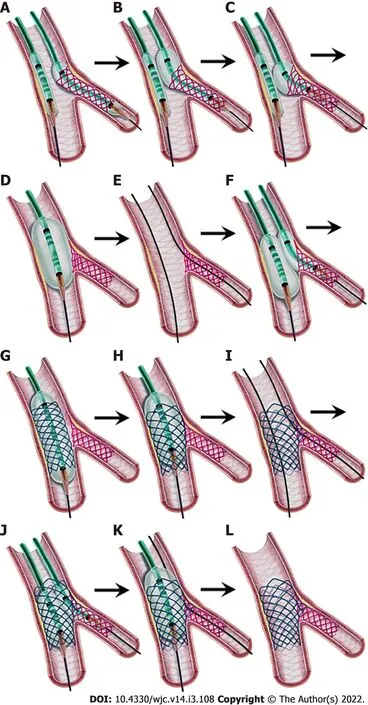
Figure 12 Step-by-step double kissing-crush technique.
Nano-crush technique
The “nano-crush” technique was first presented by Rayet al[101,102] at the 12th EBC meeting in 2016.Later,in 2017,Rigatelliet al[103] published a bench test and clinical outcome study of a technique with the same name.Although both procedures use a tiny SB stent part for crushing,the techniques are somewhat different from each other.Rigatelliet al[104] recently changed the name of their technique to the "nano inverted T stenting technique".
In the nano-crush technique described by Rayet al[105],the SB stent is positioned uninflated in the SB,and a non-compliant MV balloon is positioned across the carina and then inflated at a nominal pressure.While the MV balloon is inflated,the SB stent is pulled back until a small part protrudes into the MV and is deployed.However,in the nano-crush technique described by Rigatelliet al[103,104],0.5-1 mm protrusion of the proximal part of the SB stent for crushing is adjusted visually by angiography.Moreover,the KBI numbers and techniques are also different.Where Rayet al[102] perform double “classical” KBI at high pressures without a final POT,Rigatelliet al[103-105] perform only one “snuggle” KBI,then a final POT.The other steps are similar to the DK-crush stenting technique described before.Finally,Rigatelliet al[103-105] use only ultrathin strut stents in their technique.
Both techniques provided complete coverage of the SB ostium with a tiny amount of metal at the carina in bench tests[106,107].In a clinical study with a small number of patients,Rayet al[102] demonstrated short procedural times and no procedural complications with acceptable clinical outcomes with their technique.Rigatelliet al[104,108] showed a low incidence of TLF,no stent thrombosis and a good survival rate in left main bifurcation lesions in a small registry study and less contrast use and less procedural and radiation exposure time in comparison to the culotte technique in left main bifurcation lesions in an observational study.
Further controlled,randomized,larger studies are needed to confirm the favorable procedural and long-term clinical outcomes of these techniques in left main and non-left main bifurcation lesions.
OTHER DOUBLE STENTING TECHNIQUES
Mini-crush and step-crush techniques
The mini-crush technique is a version of the crush technique in which the crushed part of the SB stent is 1-2 mm instead of 3-4 mm.The main advantage of the crush and mini-crush techniques is that instant patency of both branches is secured[52].However,the main disadvantage of these techniques is that a 7 Fr guiding catheter is required because two stents are positioned in the coronary arteries at the same time.After the SB stent is deployed,the stent balloon and wire are withdrawn,and the prepositioned MV stent is inflated while the SB stent is crushed.The SB is rewired followed by balloon dilatation of the ostial struts,KBI and a final POT,sequentially.Rewiring the SB and balloon passing can be challenging due to three layers of stent struts,which is the reason for the low KBI rate in classical crush trials resulting in more adverse outcomes.
The step-crush technique is the same as the DK-crush technique except that the first KBI is not implemented in this technique.
Reverse (internal) crush technique
When a second stent is required in the PST,some operators use the reverse (internal) crush technique[48].A stent is positioned in the SB,and a balloon is placed in the MV.The stent is pulled back prolapsing 2-3 mm into the MV and implanted.After the stent balloon and wire is removed,the MV balloon is inflated at a high pressure to crush the SB stent.After rewiring,KBI and the POT are subsequently performed.In this technique,the crushed SB part is on the MV stent facing the lumen,unlike the other crushing techniques where it is under the stent and adheres to the vessel wall.There is no large study investigating the safety and efficacy of this technique.
Inverted DK-crush technique
When the SB is larger than the DMV,the inverted DK-crush technique may be performed.The technical steps are the same as those of the DK-crush technique with the only difference being that the DMV is considered the SB and the SB is considered the DMV.
In addition,in very rare PST cases,when the SB is occluded after MV stenting and cannot be rewired,this technique can be used to rescue the SB.The PMV stent part is crushed with a balloon passed through the jailed wire,followed by the DK-crush technique steps.
V and simultaneous kissing stent techniques
The V and simultaneous kissing stent (SKS) techniques consist of the simultaneous implantation of the MV and SB stents.The two stents are positioned so their proximal parts overlap in the PMV to form a neocarina.If the neocarina is ≤ 2 mm,the technique is called “V stenting“;however,if it is ≥ 3 mm,it is called “SKS”[28,109].Due to the simultaneous implantation of two stents,at least a 7 Fr guiding catheter is required.The main advantage of these two techniques is that access to both branches is maintained throughout the procedure without the need to rewire any branches.Therefore,these techniques are easy and fast and may be preferable to the more complex double stenting procedures in emergencies such as acute LMCA occlusion.
There are also disadvantages of these techniques[52]:(1) The possibility of PMV dissection is relatively higher because of barotrauma during two-stent implantation or postdilation;(2) If a proximal dissection occurs during the procedure or proximal restenosis develops on follow-up,a stent cannot be implanted simply proximal to the stents since a gap between the new stent and the others is inevitable.In this situation,one of the branch stents (mostly the SB) should be crushed by the new stent,but this results in four strut layers in the ostium of the branch causing difficulty for rewiring;(3) If restenosis or lesions occur distal to the stents during follow-up,wiring can be difficult as the wire can pass under or between the struts in the neocarina;and (4) Finally,SKS causes a long neocarina that has been shown to transform into a thin diaphragmatic membranous structure over time;however,the long-term adverse outcomes of this structure are unknown.
The main application of the V stenting technique is Medina 0,1,1 Lesions where the PMV is free of disease and the carinal angle is < 90°.Although many authors recommend this technique in this situation[28,48,52],there is no large study investigating the acute and long-term clinical outcomes of this technique.Due to the long carina and the above disadvantages,the SKS technique is not approved by the interventional community for use in nonemergent bifurcation interventions[48,51].
PROCEDURAL COMPLICATIONS AND OUTCOMES OF CBL INTERVENTIONS
The PCI of CBLs has more procedural risks and higher rates of adverse outcomes and restenosis than non-CBLs[99,110].In addition to classical PCI risks such as dissection,no-reflow and perforation,the procedural risks specific to CBL interventions include acute side branch closure (2.8%-5.2%),the fracture of a jailed wire,and SB stent embolism while passing or withdrawing it through the implanted MV stent[99,110].Early (< 30 d) (especially more in the EDS techniques) and late stent thrombosis rates are higher than those for non-CBLs[111-113].This may be due to higher rates of stent underexpansion and malapposition and more metallic and polymer burdens,which may provide stimuli for hypersensitivity and acute thrombogenicity reactions[99,111].
Long-term MACEs are also higher after successful DES implantation for CBLs compared to non-CBLs.Finally,distal LMCA interventions compared to non-LMCA bifurcations are associated with higher MACE (death and TVR) rates[2,99].
INTRAVASCULAR IMAGING IN CBLs
Since coronary angiography is two-dimensional lumenography,it has some limitations in evaluating lesion characteristics and post-intervention results.The intravascular imaging techniques IVUS and OCT provide accurate tomographic images and essential information that guides planning and optimizing PCI treatment[114,115].OCT provides much higher resolution images of the luminal surface,calcifications,wire positions and SB ostium than IVUS[43].On the other hand,IVUS has been used more,needs no extra contrast or vessel flushing and is better in evaluating the plaque burden[43].
Compared to angiography,better visualization of the location and extension of plaques using these imaging techniques before PCI can assist in selecting an appropriate stenting strategy and avoid unnecessary two-stent implantation[26].In addition,proximal and distal vessel sizes and plaque locations can be determined more accurately to determine the stent size,and calcifications that require debulking before stenting can also be identified[47].In patients without ostial side branch involvement (i.e.,Medina 1,1,0/1,0,0/0,1,0),the “eyebrow” sign identified by IVUS was found to be a strong predictor of SB narrowing or occlusion after MV stent implantation[116],in which case the intervention strategy can be changed.After stenting,OCT can help rewire through the distal cell,which is required for optimal stent scaffolding by subsequent balloon or KBI[115].Stent expansion and apposition status,distal or proximal stent edge dissection,or residual stenosis can be well identified by both IVUS and OCT[43].
The MAIN-COMPARE registry trial,comparing the use of IVUS in LMCA bifurcation lesions to angiography alone,showed a lower 3-year mortality rate;and the other registry trial SCAAR showed a significantly lower primary endpoint (all-cause mortality,restenosis,or definitive stent thrombosis)[117,118].In addition,a recently published analysis of the British Cardiovascular Intervention Society Database has shown lower in-hospital MACE and lower 1-year death rates with the use of IVUS in LMCA interventions[119].Finally,the results were found to be similar in two recent meta-analyses[120,121].In view of these data,IVUS is recommended as the gold standard for PCI of LMCA bifurcation lesions;and although there are no large data,it has been reported that OCT is feasible in LMCA bifurcation lesions in recent guidelines[41,47].
In non-LMCA lesions,an observational PCI study found a lower 7-year cardiac death,MI and MACE rates in the IVUS guided compared to angiography alone in true bifurcation lesions[122].There are no randomized trials confirming the clinical benefits of routine IVUS use in non-LMCA bifurcation lesions,but the EBC emphasizes the benefit of intravascular imaging in all CBLs in the latest guidelines[20,47].
Although OCT provides superior images compared to IVUS,there are limited clinical data that only come from observational trials with a small number of bifurcation patients[115].The results of ongoing large randomized trials OCTOBER (comparing two-year MACE between OCT guided or angiography alone interventions in CBLs) and OPTIMUM (comparing 3D OCT guidedvsangiography alone provisional stenting in terms of malapposed struts in bifurcation lesions) will shed more light on the benefits of OCT use in CBL interventions[123,124].
LEFT MAIN BIFURCATION LESIONS
LMCA stenosis is detected in 5-8% of patients undergoing diagnostic angiography[125],and left main bifurcation lesions (LM-BLs) account for approximately 80% of LMCA lesions[125,126].The LMCA with its bifurcation has specific properties and requires some different technical approaches[26,42,43,126]:(1) The LMCA supplies > 75% of the blood of the myocardium in a right dominant coronary system,so any complication may result in catastrophic outcomes;(2) The LMCA diameter is between 3.5-6.5 mm with a mean of 4.75-5 mm,so the overexpansion capacity of the stent to be used should be known (Table 2);(3) The left circumflex artery (LCx) is usually the side branch and supplies > 10% of the blood of the myocardium in > 95% of cases,so its loss during PCI is unacceptable;(4) The bifurcation angle is wider than the other bifurcations with a mean value of 70°-80°,so LCx rewiring may be more difficult,and it should be noted that worse outcomes were found with culotte stenting than with the DK-crush technique in patients with bifurcation angles > 70°in LM-BLs[35];(5) The guiding catheter is close to the LMCA stent,so wires can go behind the struts.In addition,during the withdrawal of jailed wires or balloons,the guiding catheter can enter the LMCA and cause longitudinal compression of the LMCA stent,which is associated with adverse outcomes if untreated[26,57,127];(6) Diffuse LMCA disease can be overlooked when using angiography due to the lack of a reference segment.Due to the physical laws of coronary bifurcation,LMCA diffuse disease should be considered when the LMCA reference diameter is similar to that of the LAD;and (7) A total of 10%-15% of patients have trifurcation with the addition of an intermediate (ramus) branch,so the complexity of PCI increases,and larger guides are required for triple kissing inflations.
CABG is the gold standard treatment for LMCA lesions according to both recent European Society of Cardiology/European Association for Cardio-Thoracic Surgery (ESC/EACTS) and American Heart Association/American College of Cardiology (AHA/ACC) guidelines[41,128].However,there are some differences in PCI implementation between these guidelines.The ESC/EACTS recommends PCI as a Class I indication for LMCA patients with SYNTAX scores < 22 (low risk),Class IIa with SYNTAX scores between 23-32 (intermediate risk),and Class III with higher scores.On the other hand,the AHA/ACC classifies LMCA lesions as ostial,trunk and bifurcation.LMCA bifurcation lesions with an increased risk of surgical outcomes (Society of Thoracic Surgeons (STS) score > 2) are Class IIb indications whereas ostial and trunk lesions with a very high risk of surgical outcomes (STS score ≥ 5) are recommended as Class IIa indications for PCI.After these guidelines,5-year results of two important EXCEL and NOBLE trials have been published,which have caused intense debate about the treatment of LMCA disease with PCIvsCABG[129,130].Repeat revascularization rates were higher in the PCI arms of both trials.Although mortality rates were similar between the CABG and PCI arms,PCI was inferior in terms of the nonprocedural MI in the NOBLE trial.On the other hand,no significant difference between CABG and PCI was found in the primary outcome (composite of death,stroke or MI) in the EXCEL trial.However,the primary outcome definition that does not include repeat revascularization and the MI definition that differs from the second or third universal definition of MI have been criticized[131].Moreover,although the cardiac death rates were not different,a higher total mortality rate in the PCI arm was noted[47].A meta-analysis of five randomized trials involving EXCEL and NOBLE was recently published and found that individual total mortality,cardiac death,stroke and MI rates were not different between the CABG and PCI arms,and unplanned revascularization rates were significantly higher in the PCI arm,as expected[132].Finally,the multidisciplinary heart team approach,which considers the anatomical and clinicopathological status of each patient and the experience of the operators,is required in the LMCA treatment decision[45,47].
LM-BLs that involves only one branch (i.e.,Medina 1,1,0 or 1,0,1) are considered non-complex lesions,and the default strategy is the PST[42].Two-branch involvement (i.e.,Medina 1,1,1 or 0,1,1) in LM-BLs is a complex true lesion.The EBC still recommends the PST for the vast majority of these complex lesions[42],and recommends the EDS techniques in the case of long SB (usually LCx) lesions (≥ 10 mm) or difficult SB access[49].Furthermore,EDS is preferred in cases where there is a high risk of SB occlusion[48].Finally,as described before,preferring the DK-crush technique over the PST in complex-true LMCA lesions is a Class IIb indication in the 2018 ESC/EACTS myocardial revascularization guidelines[40].
As described before,the EBC-MAIN trial was recently published and showed that there was no statistically significant difference between the PST and EDS techniques in LM-BL interventions in short SB lesions.The DK-crush technique was used in only 5% of EDS patients in this trial[46].
In light of the latest data and expert opinions,the PST is most often the default strategy[37-39,46,48].However,it is better to prefer EDS if the SB (usually LCx) is ≥ 2.5 mm and the lesion length is ≥ 10 mm or the likelihood of SB occlusion is high or SB wiring is difficult in complex-true (Medina 1,1,1;0,1,1) LM-BLs;furthermore,if the operator is familiar with the technique,the DK-crush technique may be preferred over other EDS techniques (Figure 3).
Angiographical LMCA stenosis > 50% is considered significant;however,there are many cases of ambiguous lesions.FFR and/or IVUS should be used to decide on revascularization for these lesions.Collected data showed that if FFR > 0.8,then it is safe to defer revascularization;and if FFR ≤ 0.8,then revascularization of the LMCA is indicated[42,133].On the other hand,an IVUS-derived minimum lumen area (MLA) of 6 mm2is usually considered to be the cut-off value of significant LMCA lesions[42];however,this value was determined in Western populations who typically have larger body and vessel sizes,and an IVUS-derived MLA of 4.5 mm2was found to be the cut-off value in an Asian population study[134].Consequently,in LMCA lesions,it is recommended to defer revascularization if the MLA > 6 mm2,to revascularize if the MLA < 4.5 mm2and to evaluate with FFR measurement if the MLA is between 4.5 and 6 mm2[135].There is no defined cut-off value for OCT yet[42].
After LMCA stenting,IVUS-derived minimum stent area cut-off values for predicting angiographic restenosis were 5 mm2for the ostial LCx,6.3 mm2for the ostial left anterior descending artery (LAD),7.2 mm2for the polygon of confluence,and 8.2 mm2for the LMCA above the polygon of confluence (the socalled 5-6-7-8 rule) in a study[136].However,this trial was conducted in Asian patients and it appears that larger LMCA cut-off values should be targeted in other populations and large body size patients[127].Indeed,in an IVUS substudy of the EXCEL trial,the minimum LMCA stent area cut-off value for predicting angiographic restenosis was 9.8 mm2;and in the NOBLE trial substudy,this value was found to be 13.4 mm2[137,138].
After crossover stenting in the LMCA during the PST,whether the nonobstructed SB (usually LCx) ostium should be opened is a matter of debate[47].A recent large registry,however,showed that there was no significant difference between the KBI and non-KBI arms in terms of TLR in patients with crossover stenting from the LMCA to the LAD[139].
The optimal PCI strategy for isolated ostial LAD lesions and ostial LCx lesions (Medina 0,1,0 and 0,0,1) is uncertain[25].The extension of LMCA bifurcation plaques may not be detected by angiography,so IVUS/OCT is preferred for isolated ostial LAD or LCx lesions.Indeed,angiographic assessment was found to underestimate the extension and severity of lesions.Distal LMCA atherosclerotic plaques extended 90% to the LAD,66% to the LCx,and 62% to both whereas isolated ostial plaque involvement of the LAD and LCx was only 9% and 17%,respectively,in an IVUS study[140].In conclusion,if the anatomy is appropriate according to IVUS/OCT (the carinal angle is approximately 90°,the LMCA is free of plaque and there is certain visualization of the ostium of the other branch),then ostial stenting may be preferred to avoid LMCA stenting.Otherwise,the PST (from LMCA to LAD stenting) for isolated ostial LAD and the inverted PST (from LMCA to LCx stenting) for isolated ostial LCx seem to be the preferred options[25,47].
Finally,after successful LMCA stenting,late (3-12 mo) control angiography may be considered regardless of symptoms according to recent guidelines (Class IIb,level of evidence C)[41].
DRUG–COATED BALLOONS IN CBLs
Drug-coated balloons (DCBs) are a new technology intended for the prevention of restenosis as an alternative option to DESs[26].The use of DCBs in CBL is attractive due to the high rate of restenosis after CBL intervention.Observational studies using a DES in the MB and a DCB in the SB showed good SB results[141].The PEPCAD-BIF trial showed that DCBs provided very acceptable late lumen loss in SB lesions without both major dissections and significant early vessel recoil[142].In the BABILON trial,a DCB in the SB plus a bare metal stent in the MV was found to be worse than the provisional DES strategy in terms of MACE and TLR[26].It should be noted that these and all the other studies to date on the use of DCBs in de novo CBLs are heterogeneous and include a small number of patients[47].A recent meta-analysis that included four studies with 349 patients treated with DCBsvsstandard balloon angioplasty,showed that the DCB reduced the SB late lumen loss,but the SB binary restenosis rates and the clinical outcomes (MACE and TLR) were not different[143].Consequently,there still is insufficient conclusive data on the use of DCBs in de novo CBLs[48].A new “POT-side DCB-POT” method was recently described in a case report[144],and more research is expected on the clinical consequences of this technique.
DCBs have been tested in in-stent restenosis (especially after two-stent implantation) and have been found to provide a good clinical outcome without requiring extra stent implantation[145].Therefore,the method was reported as “feasible” in this case in the latest EBC guidelines[47].
DEDICATED BIFURCATION STENTS
The difficulties in accessing the SB after MV stenting,or vice versa,resulted in the development of dedicated bifurcation stents (DBSs).Although many types are available,4 DBSs were studied in randomized trials:BiOSS Expert and BiOSS LIM (Balton,Warsaw,Poland),the Tryton stent (Tryton Medical,Durham,North Carolina) and the Axxess bifurcation stent (Biosensors International,Singapore).
The BiOSS Expert is a paclitaxel-eluting balloon-expandable dedicated bifurcation stent that is implanted in the MV and has an open side to the ostium of the SB.In the Polbos I trial,the BiOSS Expert was compared with many types of DESs using the PST.Although the MACE rates were similar,the TLR rate was higher in the BiOSS Expert group[146].The BiOSS LIM is a sirolimus-eluting balloonexpandable dedicated stent.In the Polbos II trial,no difference was found between the BiOSS LIM and provisional DES techniques in terms of the MACE and TLR rates[147].
The Tryton stent is a balloon expandable dedicated cobalt chromium non-DES.This stent is implanted in the SB,and a DES is implanted in the MV through the open struts of this dedicated stent.A pooled analysis of the Tryton pivotal randomized controlled trial and post-approval confirmatory study comparing this stent with the PST with a DES showed that the Tryton stent was clinically noninferior to the PST with good angiographic outcomes at 1 year[148].
The Axxess stent is a self-expandable biolimus-eluting dedicated stent that is designed for EDS.It is implanted in the proximal MV with its distal end aligned to the carina,allowing easy access to both the distal MV and the SB[149].In the COBRA study,Axxess with two biolimus-eluting stents (in the distal MV and the SB) was compared to the culotte stenting technique with two everolimus-eluting stents and found no difference in stent coverage at 9 mo and similar favorable clinical outcomes at 5 years[150].
Consequently,DBSs have not yet been found to be superior to conventional bifurcation stenting strategies for routine use in CBLs[151].
ANTITHROMBOTIC THERAPY
Since the periprocedural and long-term risk of stent thrombosis (ST) of coronary bifurcation PCI is high[112],antithrombotic therapy is an important part of CBL treatment.The anatomical properties of bifurcations lead to a relatively high rate of strut malapposition,stent underexpansion and isolated strut noncoverage,resulting in thrombosis[113].EDS,except for the DK-crush technique,has been found to cause higher ST risk than one-stent implantation.In addition,the ST rate of “bail-out” second stent implantation in the PST was shown to be higher than that in EDS[152].Therefore,careful preselection of the stenting strategy is required.ST most often occurs acutely or in the first 30 d postprocedure rather than later[20].
Unfractioned heparin is the standard anticoagulant agent for every PCI procedure.Given the complex and time-consuming nature of bifurcation intervention,close monitoring of ACT values is required.In order to prevent ST in the acute and early phases,IV cangrelor may be preferred in P2Y12inhibitor-naïve patients (ESC Class IIb,LOE A recommendation)[40].
Dual antiplatelet therapy (DAPT) with P2Y12inhibitors and aspirin is the standard treatment after every coronary stent implantation.In acute coronary syndrome (ACS),the potent P2Y12inhibitors prasugrel and ticagrelor are preferred over clopidogrel.Due to the results of the recent ISAR-REACT 5 trial,prasugrel is preferred over ticagrelor in the latest ESC guidelines (Class IIa)[153].In stable coronary artery disease (CAD),although they have not been documented to be more efficient than clopidogrel,the potent P2Y12inhibitors prasugrel or ticagrelor may be considered in high ST risk situations,such as LMCA interventions,according to the ESC guidelines (Class IIb,LOE C recommendation)[41].
The duration of DAPT depends on the clinical presentation (stable CAD or ACS) and the ST and bleeding risk.In both stable CAD and ACS interventions,high ST risk patients such as bifurcation PCI ≥ 2 stents and LMCA PCI,the duration of DAPT may be prolonged beyond 12 mo if the bleeding risk is not high (Class IIb indication for stable CAD and class IIa indication for ACS)[41,154].However,in the case of high bleeding risk (e.g.,PRECISE-DAPT score ≥ 25),DAPT duration may be considered as 3 mo for stable CAD and 3-6 mo for ACS patients with the cessation of P2Y12inhibitor (Class IIa indication according t
o ESC and Class IIb indication according to the latest AHA/ACC guidelines,for both stable CAD and ACS)[41,154-156].Finally,after the recent publication of 5 large trials that also included CBLs,the AHA/ACC recommends a class Ⅱa indication for a shorter DAPT duration (1-3 months) followed by P2Y12inhibitor monotherapy to reduce the risk of bleeding events in selected patients [156].
CONCLUSION
Coronary bifurcation lesions are complex and require meticulous preplanning of the stenting strategy.The provisional stenting technique is the default strategy in most cases.However,two-stent techniques,especially the DK-crush technique,may be the upfront-stenting strategy in some patients with complex lesions.Multiple consecutive steps are required to perform a successful stenting procedure.During the procedure,intravascular imaging is an essential tool since it is not only helpful in the selection of the stenting technique but also necessary for optimization of the result.The results of ongoing and anticipated future trials are awaited to clarify various unresolved issues in percutaneous coronary bifurcation interventions.
ACKNOWLEDGEMENTS
I would like to thank the illustrator Coşkun Kuzgun for drawing clear and explanatory figures.
FOOTNOTES
Author contributions:The author reviewed the literature and related books,and wrote the article.
Conflict-of-interest statement:Author declares no conflict of interests for this article.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is noncommercial.See:https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Turkey
ORCID number:Tamer Kırat 0000-0002-7746-0844.
Corresponding Author's Membership in Professional Societies:European Society of Cardiology,No.169218;Turkish Society of Cardiology,No.1216.
S-Editor:Ma YJ
L-Editor:A
P-Editor:Yu HG
杂志排行
World Journal of Cardiology的其它文章
- Electrocardiographic alterations in patients with chronic obstructive pulmonary disease
- Risk profiles and outcomes of patients receiving antibacterial cardiovascular implantable electronic device envelopes:A retrospective analysis
- Predictors of persistence of functional mitral regurgitation after cardiac resynchronization therapy:Review of literature
- Climatic influences on cardiovascular diseases
- Arrhythmic risk stratification in ischemic,non-ischemic and hypertrophic cardiomyopathy:A two-step multifactorial,electrophysiology study inclusive approach
