Two approaches for newborns with critical congenital heart disease:a comparative study
2022-03-11XiWangKaiMaKGuunaJningPangXuWangLeiQiYangaYngFengQunMaoShouJunLi
Xi Wang · Kai Ma · KGuuna-Jni-ng Pang · Xu Wang · Lei Qi · Yang aYng · Feng-Qun Mao · Shou-Jun Li
Abstract
Keywords Critical congenital heart diseases · Newborn · Prenatal diagnosis, transposition of the great arteries
Introduction
Critical congenital heart disease (CCHD) often presents with cyanosis, anoxia, feeding difficulty, and recurrent heart failure after birth. When not treated on time, approximately 50% of the patients would die during the neonatal period,becoming the leading cause of neonatal death [ 1, 2]. A latest study confirmed that the prevalence of CCHD was 1.46 per 1000 live births in China, where at least 10,000 babies with CCHD were born every year, representing a significant clinical and public health challenge [ 3]. The effective treatment strategy is to detect and identify lesions as early as possible,so that management plans can be performed in a timely manner. Many studies have demonstrated that prenatal diagnosis reduces the risk of death prior to planned cardiac surgery[ 4 ]. The proportion of prenatally diagnosed CCHD cases was approximately 40.0%-88.3% in many developed countries [ 5,6], and most of the patients received surgical treatment during the neonatal period with a 30 day mortality of 9.1% [ 7].
With the promotion of prenatally diagnosed technology and improvement of government policy, the prenatal diagnosis rate of CCHD has increased during the past 2 decades in China, and there has been a high detection rate for major CHD in both low- and high-risk populations [ 8, 9]. Pediatrics and fetal cardiologists understand well the pathophysiology and natural history of congenital heart disease in the developed countries. However, China is a developing country, and the development of pediatrics is relatively backward, especially in the field of critical congenital heart disease. The diagnosis and treatment levels vary among medical units owing to the relative lack of understanding of congenital heart diseases (CHDs). “Prenatal diagnosis and planned peripartum care” remains an unexplored concept for the care of neonates with CCHD in China. To improve the efficacy and to obtain better results of neonatal CCHD surgery, Fuwai Hospital has collaborated with some maternity hospitals in Beijing and has started the ‘perinatal integrated diagnosis and treatment model’ in 2019. In addition, we enhanced the ability to receive newborns who were diagnosed in the postpartum period and to rapidly transfer the patients into the hospital using a green channel.
Based on the integrated model, the diagnosis of newborns with CCHD and the treatment effects were evaluated retrospectively. In addition to confirming the efficacy of the integrated model, the outcomes of the integrated patients were compared with those of newborns with CCHD who were diagnosed in the postnatal period and were rapidly admitted to our center from January 2019 to December 2020.
Methods
This study was conducted at the Department of Pediatric Cardiac Surgery, Fuwai Hospital, Beijing, China. A retrospective review of demographic characteristics, operative records, and outpatient clinical data was performed according to the approval of our institutional ethics committee (ethical number 2017-977, approved on November 30, 2019).The need for informed consent from individual patients was waived by the hospital's ethical committee.
Prenatal diagnosis and postnatal treatment integrated model
Senior pediatric surgeons and cardiologists provided scientific perinatal diagnosis and evaluation of fetuses diagnosed with CCHD by fetal echocardiography. If parents were willing to continue pregnancy after consultation, the fetus would be arranged to be delivered in our cooperative maternity hospitals and transferred to our center after birth. The clinical workflow for fetuses with CCHD was integrated with multidisciplinary participation, including related disciplines from the obstetrics and gynecology hospitals and children’s hospitals in Beijing or hospitals not far from Beijing. The echocardiographic results help to predict the delivery room risk, anticipated postnatal level of care, and final delivery planning. Fetuses with severe or critical CHD were arranged with planned and coordinated delivery with a specialized care team in the delivery room.Relevant treatments were carried out depending on the types of the cardiac diagnosis and on the anticipated complexity of the staffing needed for delivery room stabilization; sometimes an urgent intervention would be required.A cardiac surgeon was responsible for coordinating the project and ensuring that everything went smoothly. All patients in the integrated group were diagnosed in the prenatal period and were admitted to Fuwai Hospital in a planned way after delivery.
Non-integrated model
Traditionally, almost all the patients with CHD need to be diagnosed at outpatient clinics or in an emergency department before admitting to pediatric cardiac center, which may delay the life-saving medications or surgery. Early diagnosis and timely surgery or interventional treatment and active management of the complications are keys to improving the success rate of surgery and to reducing mortality. Hence, since 2019, we also have increased the capacity to receive newborns with CCHD from outpatient clinics or those transferred from other hospitals by ‘green channel’. In other words, most children could be hospitalized without going to outpatient clinics or the emergency department. Once diagnosed at other hospitals and contacted with us, the patients diagnosed in the postnatal period would be admitted to Fuwai Hospital rapidly.All patients diagnosed during the postpartum period were divided into the non-integrated group. Patients who were not delivered in our cooperative maternity hospitals and transferred to Fuwai hospital in a planned way, also would be divided into the non-integrated group although they were diagnosed prenatally.
From January 2019 to December 2020, 133 neonates were admitted to the pediatric cardiac center of Fuwai Hospital. Among them, seven patients abandoned treatments for poor prognosis or economic factors before surgery, and six patients were in a stable state after medical treatment, which was scheduled after the neonatal period.Then, 120 consecutive neonates (surgical age ≤ 28 days)underwent cardiac surgery at our institution. Four cases of simple CHDs were excluded, including three cases of ventricular septal defect and one case oflarge patent ductus arteriosus. Neonates whose surgical age was > 28 days also were excluded from the study. The patients were divided into a “prenatal diagnosis and postnatal treatment integrated group” (n
= 47) and “non-integrated group”(n
= 69).Therapeutic strategy
Echocardiography was performed to confirm the preoperative diagnosis and anatomy immediately after admission.Cardiac CT examination was required when necessary.Prostaglandin E1 was used to maintain hemodynamic stabilization for patients with duct-dependent CHD and severe hypoxia. For patients with critical conditions who were unresponsive to medical treatments, emergency surgery was scheduled. For newborns with relatively stable hemodynamics, sub-emergency or conventional surgeries were performed during a limited period.
All patients were followed up in the 1st, 3rd, 6th, and 12th months of the first year of surgery, and at least once every year thereafter. Follow-up data were obtained by re-evaluation at the hospital, telephone interview, or WeChat application with parents. Early mortality or in-hospital mortality was defined as both 30-day mortality and death at any time after the surgery but before discharge. Late mortality was defined as death after 30 days or after discharge if the length of hospital stay was more than 30 days. Perioperative and follow-up results were compared between the two groups.
Statistical analysis
Categorical variables were expressed as frequency and percentage and were compared between the two groups using theχ 2
statistics or Fisher’s exact test. Continuous variables were described using mean and standard deviation if the data were normally distributed or using median and interquartile range if not normally distributed. Differences in continuous variables were assessed using thet
test or by non-parametric testing using the Mann-WhitneyU
test for skewed outcomes. All statistical tests were two-tailed, and statistical significance was set atP
< 0.05. The Kaplan-Meier method was used to estimate the probability of freedom from allcause death at given time points, and GraphPad Prism software (version 8.0) was used to create the Kaplan-Meier curve. Statistical analysis was performed using the SPSS 25.0 software package.Results
Perioperative results
The distribution of anatomical types is shown in Table 1.Most lesions were ductal dependent. A significant difference was observed in the distribution of the main diagnosis between the two groups (P
= 0.017). There were also 23(48.9%) cases of transposition of the great arteries (TGA)in the integrated group and 16 (23.2%) cases of TGA in the non-integrated group (P
= 0.005). However, the proportionof total anomalous pulmonary venous connection was significantly lower in the integrated group (8.5 vs. 23.2%,P
= 0.047).Table 1 Disease distribution between the two groups
transposition of the great arteries, intact ventricular septum,ventricular septal defect, P pulmonary stenosis, total anomalous pulmonary venous connection, coarctation of the aorta, I interrupted aortic arch, pulmonary artery atresia, severe pulmonary stenosis, complete atrioventricular septal defect, severe aortic stenosis, anomalous origin of pulmonary artery from ascending aorta, three cases functional single ventricle
Variables Integrated group( n = 47)Non-integrated group ( n = 67)P value TGA 23 (48.9%) 16 (23.2%) 0.005 TGA/IVS 14 (29.8%) 10 (14.5%) 0.062 TGA/VSD 8 (17.0%) 6 (8.7%) 0.246 TGA/VSD/PS 1 (2.1%) 0 0.405 TAPVC 4 (8.5%) 16 (23.2%) 0.047 CoA 7 (14.9%) 7 (10.1%) 0.563 IAA 4 (8.5%) 3 (4.3%) 0.439 PAA/IVS 4 (8.5%) 10 (14.5%) 0.396 SPS/IVS 3 (6.4%) 6 (8.7%) 0.737 PAA/VSD 0 2 (2.9%) 0.514 Taussig-Bing malformation 1 (2.1%) 0 0.405 CAVSD 1 (2.1%) 0 0.405 AOPA 0 2 (2.9%) 0.514 SAS 0 4 (5.8%) 0.146 Others 0 3 (4.3%) 0.514
Perioperative data between the two groups are shown in Table 2. The time of admission to the hospital and age at surgery were lower in the integrated group than in the non-integrated group (5.2 ± 7.2 days vs. 11.8 ± 8.0 days,P
< 0.001;11.9 ± 7.0 days vs. 16.5 ± 7.7 days,P
= 0.001). The weight at surgery also was lower in the integrated group than in the non-integrated group (3.3 ± 0.4 kg vs. 3.6 ± 0.6 kg,P
= 0.010). Early admission to the hospital allowed enough time to complete the examination and to confirm the preoperative diagnosis. Moreover, appropriate medical treatments and neonatal nursing were applied to keep the patients under a stable state. Therefore, the preoperative endotracheal intubation rate was 6.4% and 10.1% for the integrated and non-integrated groups, respectively (P
= 0.738). There was a low incidence of emergency surgery in the integrated group,but no significant difference was observed between the two groups (12.8 vs. 26.1%,P
= 0.104).The Aristotle score [ 10] is a complexity-adjusted method based on the complexity of the surgical procedures that was developed by an international group of experts.The complexity is based on two steps: the first establishes the basic score, which is adjusted only for the complexityof the procedures, and the second is used to develop the comprehensive Aristotle score, which further adjusts the complexity according to the specific patient characteristics. The complexity levels were graded according to the basic score as follows: level 1 (basic score 1.5-5.9);level 2 (basic score 6.0-7.9); level 3 (8.0-9.9); and level 4(10.0-15.0). The basic Aristotle score and its corresponding complexity level were used to compare the complexity of the major surgical procedures between the two groups in our study. The patients in the integrated group had a higher basic Aristotle score than those in the non-integrated group(8.8 ± 2.2 vs. 8.1 ± 2.0,P
= 0.050). The resulting complexity levels were as follows: level 1 (14.9% vs. 23.2%), level 2 (17.0% vs. 15.9%), level 3 (10.6% vs. 33.3%), and level 4 (57.4% vs. 27.5%) (P
= 0.004). The average Aristotle complexity level was 3.1 ± 1.2 vs. 2.7 ± 1.1 (P
= 0.037).Most of the patients completed primary repair, but palliative surgery was needed in 2.0% of the patients in the integrated group and 8.7% of the patients in the non-integrated group (P
= 0.238). The proportion of off-pump surgery was 17.0% vs. 30.4% (P
= 0.128).Table 2 Perioperative data between the two groups
Variables Integrated group( n = 47)Non-integrated group( n = 69)P value Premature infant, n (%) 3 (6.4%) 5 (7.2%) 1.000 Gestational age, wk 38.6 ± 1.5 38.7 ± 2.1 0.647 39-40 wk, n (%) 24 (51.1%) 43 (62.3%) 0.255 One of the twins, n (%) 3 (6.4%) 1 (1.5%) 0.303 Admission age, d 5.2 ± 7.2 11.8 ± 8.0 0.000 Surgery age, d 11.9 ± 7.0 16.5 ± 7.7 0.001 Weight, kg 3.3 ± 0.4 3.6 ± 0.6 0.010 Aristotle score 8.8 ± 2.2 8.1 ± 2.0 0.050 Aristotle level 0.004 Level 1, n (%) 7 (14.9%) 16 (23.2%)Level 2, n (%) 8 (17.0%) 11 (15.9%)Level 3, n (%) 5 (10.6%) 23 (33.3%)Level 4, n (%) 27 (57.4%) 19 (27.5%)Ventilation before surgery 3 (6.4%) 7 (10.1%) 0.738 Emergency operation, n (%) 6 (12.8%) 18 (26.1%) 0.104 CPB time, min 129.1 ± 24.6 132.0 ± 74.8 0.796 ACC time, min 80.0 ± 18.6 80.6 ± 46.4 0.932 Delayed sternal closure, n (%) 9 (19.1%) 5 (7.2%) 0.080 ECMO support, n (%) 0 3 (4.3%) 0.271 Major complications Respiratory tract infection, n (%) 15 (31.9%) 16 (23.2%) 0.393 Peritoneal dialysis, n (%) 7 (14.7%) 10 (14.5%) 1.000 Cardiac insufficiency, n (%) 3 (6.4%) 7 (10.1%) 0.738 Capillary leakage syndrome, n (%) 5 (10.6%) 3 (4.3%) 0.266 Secondary intubation, n (%) 1 (2.1%) 3 (4.3%) 0.646 Mechanical ventilation time, h 97 (51-259) 69 (29-169) 0.030 Early extubation (≤ 24 h) 4 (8.5%) 13 (18.8%) 0.181 Postoperative ICU stays, d 13.0 (8.0-21.0) 9.0 (4.5-16.0) 0.048 Postoperative stay, d 21.0 (16.0-28.0) 15.0 (21.0-24.0) 0.020 Early deaths, n (%) 0 5 (7.2%) 0.080 Follow-up time, mon 11.0 (3.0-13.0) 12.0 (8.0-14.0) 1.000 Late deaths, n (%) 1 (2.1%) 1 (1.4%) 1.000 Total mortality, n (%) 1 (2.1%) 6 (8.7%) 0.396
Longer recovery time was needed after surgery in the integrated group, and the median mechanical ventilation time was 97 h (interquartile range 51-259 h) vs. 69 h (29-168 h)(P
= 0.030); the postoperative intensive care unit time was 13.0 days (8.0-21.0 days) vs. 9.0 days (4.5-16.0 days)(P
= 0.048); the postoperative hospital stay was 21.0 days(16.0-28.0 days) vs. 15.0 days (12.0-24.0 days) (P
= 0.020).The in-hospital mortality rate was 0% in the integrated group and 7.2% in the non-integrated group (P
= 0.080).In the non-integrated group, three TGA patients were under poor state with ventilator assistance and severe infection before surgery. Although two of them received ECMO support, early death occurred 1 day, 24 days, and 36 days,respectively, after the emergency surgery. One newborn with total anomalous pulmonary venous connection (TAPVC)recovered well and was expected to be discharged but died from asphyxiation caused by feeding errors in the hospital.One severe aortic valve stenosis with severe aortic coarctation died owing to low cardiac output syndrome and severe coagulation disorders after emergency surgery, as well as ECMO support.
Follow-up results
During the follow-up period (13.8 ± 6.2 months vs.13.4 ± 8.2 months), late deaths occurred in 2.1 vs. 1.4% of both groups (P
= 1.000). There was also no significant difference in the all-cause mortality between the two groups(2.1 vs. 8.7%,P
= 0.238) (Kaplan-Meier curve in Fig. 1).Comparison of TGA between the two groups
The time of admission to the hospital and the age at surgery were lower in the integrated group. There was no significant difference in the cardiopulmonary bypass time (135.9 ± 22.5 min vs. 180.6 ± 106.8 min,P
= 0.119)and in the aortic cross-clamp time (84.4 ± 15.5 min vs.113.6 ± 59.6 min,P
= 0.073). There was also no significant difference in the postoperative recovery time, including the mechanical ventilation time (184.3 ± 269.1 h vs. 180.0 ± 268.0 h,P
= 0.119), intensive care unit time(15.3 ± 14.7 days vs. 12.9 ± 11.1 days,P
= 0.073), and postoperative hospital stay time (23.1 ± 14.2 days vs.19.1 ± 10.9 days,P
= 0.354). TGA had the highest early mortality rate, which was as high as 7.7% (3/39) in all cohorts; the integrated group was significantly lower than the non-integrated group (0 vs. 18.8%, log rankP
= 0.032)(Kaplan-Meier curve in Fig. 2). No late death occurred in either group.Discussion
The concept of prenatal diagnosis of CCHDs and planned perinatal care has been well established in most developed countries [ 4]. The proportion of neonatal surgery for CCHDs was 21.8% in the Society of Thoracic Surgeons Congenital Heart Surgery database and 19.5% in the European Association for Cardiothoracic Surgery database [ 11]. However,many facilities for congenital heart surgery in China have limited specialist capacity [ 12], resulting in delayed diagnosis, delayed life-saving medications, and suboptimal transport. Neonatal surgery accounted for 1.7% of all CHD patients in 2019 and 1.3% in 2020, according to the data from the Fuwai Hospital. The proportion of neonatal surgery for CCHDs was less than 5% at most of the pediatric cardiac centers, and most of the newborns with CCHDs did not receive timely treatment in China.
With the rapid development of prenatal diagnosis techniques, especially fetal echocardiography, most CHDs can be diagnosed before delivery. A study from China showed that fetal echocardiography had a high sensitivity and specificity for detecting major CHDs and had satisfactory positive and negative likelihood ratios in both the low-risk (88.2%and 100%, respectively) and high-risk (100% and 99.9%,respectively) populations [ 8]. However, 74.4%-88.9% of the prenatally diagnosed CHD cases were terminated [ 8, 9]. To reduce the high abortion rate and to improve the therapeutic outcomes of CCHD, we started the “prenatal diagnosis andpostnatal treatment integrated model” and transferred green channel by cooperating with obstetricians and neonatologists of maternity hospitals since January 2019. In our experience, the preoperative status of the newborn may be the main factor for early death after surgery. CCHD was almost duct-dependent, and prostaglandin E1 would be applied if they presented with severe hypoxia or acidosis owing to the tendency of closure of patent ductus arteriosus. As other studies have shown, prenatal diagnosis and planned peripartum care could significantly shorten the diagnosis and hospitalization interval of the newborns, and surgical intervention could be performed with good preoperative status and lower in-hospital death, especially for the transposition of TGA [ 13, 14]. The fetuses with CCHD would be transferred into the pediatric cardiac center after delivery and would receive timely neonatal nursing during the early neonatal period. The improved preoperative condition resulted in an earlier age of surgical repair and a relatively low proportion of emergency surgeries in the integrated group. Although there was no statistically significant difference, the in-hospital mortality was slightly higher in the postnatal diagnosis group.
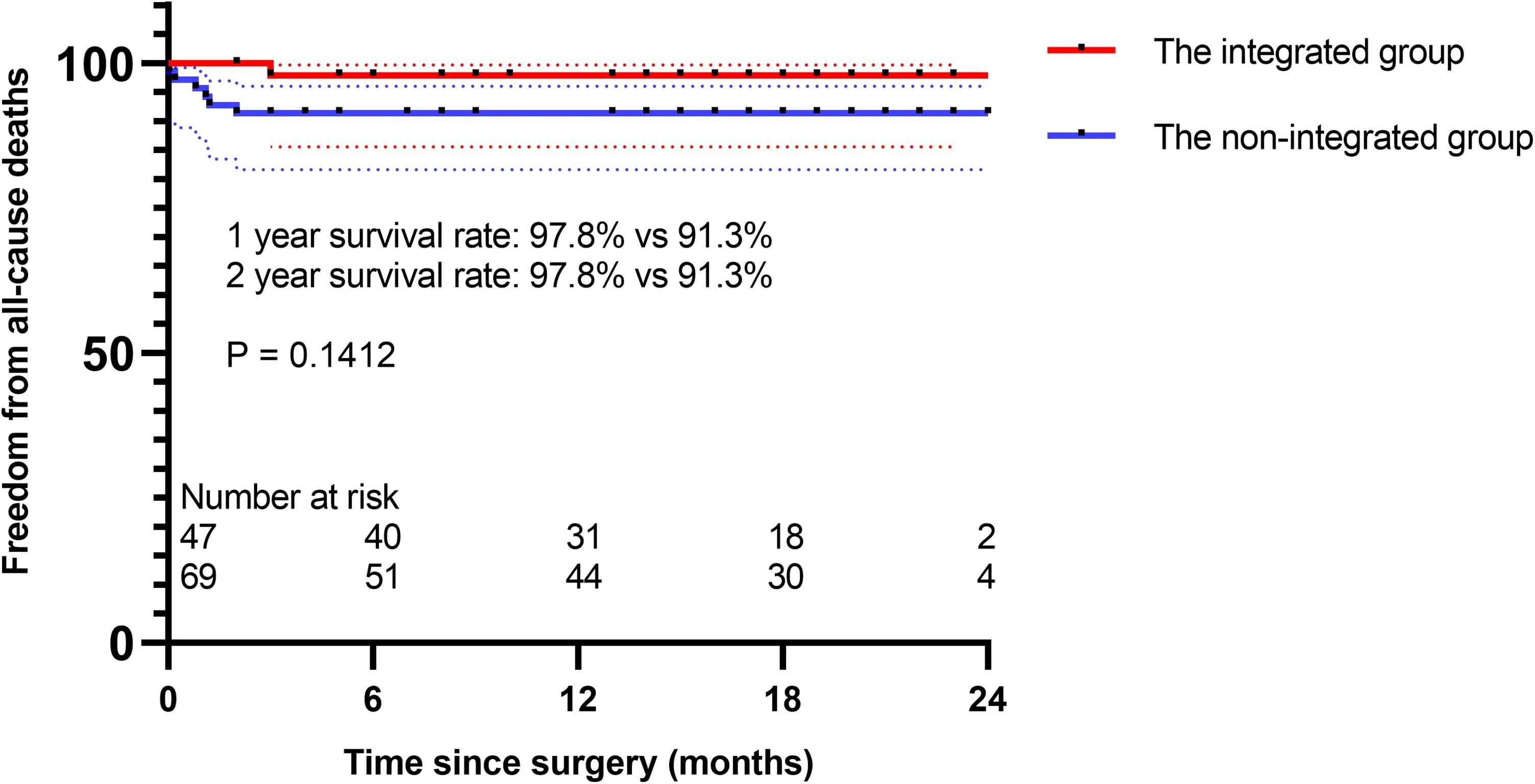
Fig. 1 Freedom from all-cause death between the two groups
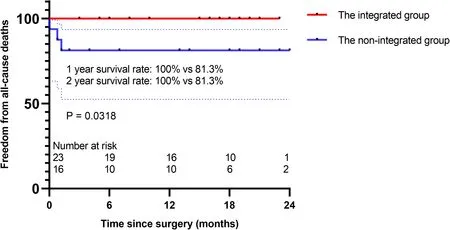
Fig. 2 Freedom from all-cause death of TGA between the two groups
For parents who were willing to continue the pregnancy,it was convincing that birth during the early term period of 37-38 weeks of gestation age was associated with worse outcomes after neonatal cardiac surgery, and 39-40 weeks of gestational age was associated with the lowest incidence of complications, shortest postoperative length of stay, and lowest in-hospital mortality [ 6]. However, only half of the fetuses in our cohort delivered at the optimal gestational age,suggesting the need for more cooperation and communication with obstetricians.
The distribution of the main diagnosis for neonatal surgery was different from that in Western countries. The European Association for Cardiothoracic Surgery Congenital Database analyzed 14,843 neonatal congenital heart surgical results between January 1999 and May 2008 and showed that hypoplastic left heart syndrome accounted for 8.2% of the newborns, but with the highest mortality rate(36.2%) [ 7]. However, there was a very low birth rate of hypoplastic left heart syndrome due to recommended abortion, and only a few cases of Norwood operation have been reported in China. TGA was the most common disease in the integrated group, and parents were willing to continue the pregnancy and to undertake the risk of surgery after birth owing to good prognosis. In terms of mortality,7.7% (3/39) of TGA patients died early in all cohorts, but all deaths occurred in the non-integrated group. Prenatal diagnosis significantly shortened the time interval from birth to neonatal care and surgery and was associated with improved survival [ 13]. Prenatal diagnosis reduced mortality and morbidity in TGA and strongly recommended in utero transfer of fetuses with prenatal diagnosis of TGA in an appropriate maternity hospital [ 15].
In addition to TGA, TAPVC was the most common disease in the non-integrated group. Many prenatally diagnosed fetuses were induced for possible long-term complications [ 16]. TAPVC with severe preoperative pulmonary venous obstruction also remained as one of the few indications for emergent cardiac surgical intervention in the newborn, but prenatal detection of TAPVC was consistently the lowest (28%) according to an international retrospective cohort study [ 5], and it was difficult to identify whether the fetuses were combined with pulmonary venous obstruction [ 17, 18]. Yang reported that 50% of the prenatally diagnosed cases combined with pulmonary venous obstruction, but none of them was diagnosed during the prenatal period [ 18]. Three of the four TAPVC cases in the integrated group were diagnosed with pulmonary venous obstruction after birth, and emergency surgeries were scheduled after hospitalization. Fetal vertical vein Doppler peak velocity > 0.74 m/s may help to predict pulmonary venous obstruction (93% sensitivity; 83% specificity) [ 17]. Further studies were needed to improve prenatal diagnosis, lower preoperative morbidity, and improve postoperative outcomes.
Although tremendous progress has been made in the surgical treatment of CHD, surgical trauma and cardiopulmonary bypass still greatly affect the prognosis of young patients. Low body weight, high serum lactate level, postoperative extracorporeal membrane oxygenation support, and prolonged cardiopulmonary bypass time were independent risk factors for early mortality in neonatal cardiac surgery[ 19]. For newborns who need extracorporeal circulation, it was important to increase the power of the pediatric surgery team and reduce the extracorporeal circulation time and aortic cross-clamp time. Since 2004, our center proposed a one-stop intraoperative hybrid procedure that combines surgical and interventional approaches simultaneously [ 20, 21].The technique was applied to treat pulmonary atresia with intact ventricular septum or severe pulmonary stenosis with intact ventricular septum, with nearly zero in-hospital death in recent years with experience accumulation. For patients with hypoplastic right ventricle, a modified B-T shunt may be placed or a bidirectional Glenn procedure could be performed simultaneously to prevent the occurrence of hypoxemia [ 20, 21]. This procedure could also be performed in infants with congenital aortic valve stenosis with a good prognosis [ 22].
Many children with CCHD cannot be recognized early enough to avoid adverse cardiovascular events. In our cohort,more than half of newborns with CCHD were diagnosed during the postpartum period. The effective treatment strategy was to detect and identify the lesion as early as possible, so that management plans can be performed in a timely manner. Thus, an increasing number of countries have introduced CHD screening as a routine practice. In asymptomatic newborn babies, the sensitivity of pulse oximetry plus clinical assessment was 93.2% for CCHD and 90.2% for major diseases [ 23]. Our government also recognized the importance of neonatal screening and required pulse oximetry recorded as a basic routine in Chinese maternity hospitals.
There were some limitations to our study. This was a retrospective single-institution study, and there were only 116 patients with various types of CHD in our cohort. Confounding factors also may affect the survival rate, including gestational week, age and weight at surgery, and preoperative status. It was unclear that whether the differences in clinical conditions were related to differences in the type of treatment received between the two groups or to differences in occurrences of TGA and/or TAPVC. In other words, the study design cannot eliminate the possibility of confounding between these alternative explanations. The potential for confounding has implications for the interpretation of results. Alternatively, a more complex statistical analysis would be tried to address the confounding. Moreover, there remained a gap between China and other developed countries. To obtain better neonatal surgical results, improvement of prenatally diagnosed ratio and planned postnatal treatment are needed in the future in China.
In conclusion, “Perinatal integrated diagnosis and treatment model” could significantly shorten the diagnosis and hospitalization interval of newborns, and surgical intervention could be performed with a lower risk of death, especially for the TGA. In addition, it is necessary to screen for CHD in the early neonatal period, and the prognosis is favorable if they are diagnosed and treated appropriately.
Acknowledgements
We gratefully acknowledged the doctors and nurses who were involved in the study.Author contributions
GXW collected and analyzed the data and drafted the manuscript. GXW, KM, KJP, XW, and SJL designed the study. KM, LQ, YY, and FQM contributed to the critical revision of the manuscript for important intellectual content, and SJL approved the final version of the manuscript. SJL obtained fundings. All the authors have read and approved the final manuscript.Funding
This work was supported by National Key R & D Program of China (2017YFC1308100) and Beijing Municipal Science & Technology Commission (Z201100005520001).Data availability
The datasets generated and/or analyzed during the current study were available from the corresponding author on reasonable request.Declarations
Ethical approval
This retrospective study was conducted at department of pediatric cardiac surgery, Fuwai Hospital in Beijing, China. It was approved by our institutional ethics committee. The specific ethical number was 2017-977 and it was approved on November 30, 2019. The need for individual patient informed consent was waived.Conflict of interest
No financial or nonfinancial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.杂志排行
World Journal of Pediatrics的其它文章
- Developmental hemostasis in the neonatal period
- Can pediatric vasovagal syncope be individually managed?
- Journal’s responsibility in maintaining scientific integrity
- Physicians’ perspectives on adverse drug reactions in pediatric routine care: a survey
- Evaluation of the Quick Wee method ofinducing faster clean catch urine collection in pre-continent infants: a randomized controlled trial
- Chest CT features of children infected by B.1.617.2 (Delta) variant of COVID-19
