Meta-analysis of the clinical efficacy of Chinese herbal decoction combined with arthroscopy in the treatment of gouty arthritis
2022-02-17XULuchunWANGJianjunYEChaoWANGYueLIHuanan
XU Lu-chun, WANG Jian-jun, YE Chao, WANG Yue, LI Hua-nan
1. The First Clinical Medical College of Beijing University of Chinese Medicine, Beijing 100000, China
2. The Third Department of Orthopedics and Traumatology, Affiliated Hospital of Jiangxi University of Traditional Chinese Medicine, Nanchang 330000, China
Keywords:
ABSTRACT Objective: To systematically evaluate the efficacy of traditional Chinese medicine decoction combined with arthroscopy in the treatment of gouty arthritis. Methods: A systematic search of CNKI, CBM, WanFang, VIP, PubMed, Cochrane Library, and EMBASE databases, and the receipt of the database until February 2021. Randomized controlled trials (RCTs) of traditional Chinese medicine (TCM) decoction combined with arthroscopy in the treatment of gouty arthritis. Two researchers independently read the title and abstract to screen and them read the full text to clarify whether it should be included. The method of Cochrane systematic review was used to evaluate the quality of the literature, and the RevMan 5.3 software was used to conduct meta-analysis of the data. Results: Nineteen RCTs were finally included. A total of 1 383 patients, 697 cases in the treatment group were treated with traditional Chinese medicine decoction combined with arthroscopy, and 686 cases in the control group were treated with arthroscopy alone or combined with western medicine. Meta-analysis results showed that the total clinical effective rate (P<0.000 01) of the treatment group was better than that of the control group. Visual analogue scoring (VAS) score (P=0.000 5, P<0.000 01, P=0.03) and erythrocyte sedimentation rate (ESR) level (P<0.000 01, P<0.000 01, P<0.000 01)reduction in each subgroup was better than that of the control group. The Lysholm score of the treatment group increased (P<0.000 01, P<0.000 01, P=0.19), while for blood uric acid (UA) level(P<0.000 01, P=0.18, P<0.000 1) and C-reactive protein (CRP) levels (P<0.000 1, P<0.000 01, P=0.23) two subgroups were better than the control group, but there was no significant difference in one subgroup. Conclusion: Traditional Chinese medicine decoction combined with arthroscopy is effective in treating gouty arthritis, which can relieve pain, improve joint function, and reduce body inflammation and uric acid levels. However, in the future, clinical studies with larger sample sizes, more reasonable designs, and higher quality are still needed to demonstrate this conclusion.
1. Introduction
Gouty arthritis is a kind of joint inflammation caused by the precipitation of monosodium urate crystals in the joints and surrounding tissues, which causes severe joint pain. In severe cases, it can cause joint stiffness and deformity in the later stage[1-3]. According to reports, the gout population accounts for 1-2%of the total population, but the prevalence is increasing year by year and the incidence tends to be younger [4,5]. Western medicine mainly controls gouty arthritis through anti-inflammatory and uric acid-lowering drugs, anti-IL-1b and other biological agents, and minimally invasive arthroscopy [6]. Arthroscopic surgery conducts a comprehensive observation and resection of the lesion through a small incision, which can quickly alleviate the symptoms, and the clinical efficacy has been widely recognized, but certain adjuvant drug treatments are required after surgery to relieve the cause and prevent recurrence [7].Traditional Chinese medicine believes that the cause of gout in the acute stage can be mainly classified as dampness, sputum, heat, cold,etc., and treatment should be beneficial, clearing, and warming; the chronic stage is mainly due to the weakness of the viscera, especially the liver, spleen, and kidney, and the treatment should be tonic[8-10]. In recent years, a large number of clinicians have achieved satisfactory results with traditional Chinese medicine decoction combined with arthroscopy, but further verification is still needed.Therefore, this study will conduct a systematic review to provide evidence-based medicine for the diagnosis and treatment of gouty arthritis.
2. Materials and methods
2.1 Literature inclusion criteria
2.1.1 Research type
Chinese medicine decoction combined with arthroscopy in the treatment of RCTs for gouty arthritis.
2.1.2 Research objects
Meet the Gout Standard of the American Academy of Rheumatology (2015) [11], and the Gout Standard of the European Federation of Rheumatism (2018) [12].
2.1.3 Intervention measures
Arthroscopy combined with Chinese medicine decoction VS arthroscopy, arthroscopy combined with Chinese medicine decoction VS arthroscopy + Western medicine, arthroscopy combined with Chinese medicine decoction + Western medicine VS arthroscopy +Western medicine.
2.1.4 Outcome indicatorsOne or more of the total clinical effective rate, Lysholm and VAS scores, UA, CRP, ESR, and adverse reactions.
2.2 Literature exclusion criteria
(1) Studies that do not meet the treatment of gouty arthritis (2)Studies with incomplete data (3) Studies with duplication of data or serious errors.
2.3 Search strategy
Search Chinese and English databases: CNKI, CBM, WanFang,VIP, PubMed, Cochrane Library and EMBASE databases. Chinese search terms are Chinese medicine, Chinese and Western medicine,Chinese medicine, Chinese herbal medicine, Chinese medicine decoction, arthroscopy, gout, acute gout, gouty arthritis, crystal arthritis, randomized, randomized controlled trials. English search terms are Chinese Medicine, Chinese and Western Medicine, herb,Chinese herbal medicine, decoction, Arthroscopic debridement,Gout, Acute gout, Gouty arthritis, Crystal arthritis, randomized controlled trial, controlled clinical trial, randomized.
2.4 Literature screening and data extraction
Two evaluators respectively clarify whether the study will be included after the introduction of duplication check. Use Excel to organize and extract data, such as disagreements, to discuss or consult professionals to determine the results.
2.5 Methodological quality evaluation
Both reviewers used the "bias risk assessment tool [13]" to evaluate the quality of the research.
2.6 Statistical analysis
The effect value is continuous variables such as Lysholm score using mean difference, and binary variables such as clinical effective rate use relative risk. The Q and I2methods were used for heterogeneity test, and the funnel chart analysis was used for publication bias.
3. results
3.1 Literature search results
A total of 618 studies were identified in the database, 264 were duplicates excluded, 319 did not match the content of the study,and 1 review, systematic review, and conference were included. 32 studies were initially included. After reading the full text, 13 non-RCT studies were excluded, and 19 RCTs were finally included.[14-32], the retrieval process is shown in Figure 1. Among the 19 studies included, there were 697 cases in the study group and 686 cases in the control group. Among them, 14 studies reported the total effective rate [14,17-20,24-32], and 11 studies reported the Lysholm score [14,16, 21-23,25,27-31], 8 studies reported VAS score [18,22-25,28-30], 11 studies reported UA level [14-16,21,24,25,27- 29,31,32], 9 studies reported CRP levels [16,21,23-25,27,29,31,32], 11 studies reported ESR levels [14,16,21,23-25, 27,29-32], 3 literature studies [25,28,32] reported adverse reactions, see Table 1.

Tab 1 Basic information of included literatures

Fig 1 Literature screening process
3.2 Quality evaluation of included studies
A total of 8 studies [14,18,19,25,27,28,30,32] used the random number table method, 1 [29] used the "coin toss method", and 3 [21-23] used"random sampling" Method", all rated as "low risk", the remaining 7 items [15-17,20,24,26,31] did not mention random schemes, rated as"uncertain risk"; neither allocation concealment nor blind method were mentioned And, rated as "uncertain risk"; data missing and selective reports were not found, rated as "low risk"; all research data have comparable baselines, all studies have reported the results of observation indicators, and no other biases have been found. The specific situation is shown in Figure 2.
3.3 Meta data analysis results
3.3.1 Total clinical effective rate
14 studies [14,17-20,24-32] reported the total clinical effective rate, and subgroup analysis was conducted according to different intervention measures.
The arthroscopy combined with traditional Chinese medicine VS arthroscopy treatment group included a total of 6 studies [14,17-20,24],with high homogeneity (P=0.98, I2=0%) using a fixed-effect model,as shown in Figure 3. The results show that the Chinese medicine combination group is better in improving the total clinical effective rate [RR=1.20, 95%CI=(1.11, 1.30), P<0.000 01]. The arthroscopy combined with traditional Chinese medicine VS arthroscopy +western medicine treatment group included a total of 5 studies [25-29], with high homogeneity (P=0.74, I2=0%) using a fixed-effect model, as shown in Figure 3. The results show that the Chinese medicine combination group is better in improving the total clinical effective rate [RR=1.23, 95%CI=(1.12, 1.35), P<0.000 1]. A total of 3 studies were included in the arthroscopy combined with Chinese medicine + Western medicine VS arthroscopy + Western medicine treatment group [30-32], with high homogeneity (P=0.48, I2=0%)using a fixed-effect model, as shown in Figure 3. The results show that the Chinese medicine combination group is better in improving the total clinical effective rate [RR=1.12, 95%CI=(1.03, 1.22),P<0.000 01].

Fig 2 Percentage of projects included in the study that produced a risk of bias

Fig 3 Forest plot effective rate between three groups
3.3.2 Lysholm score
11 studies [14,16,21-23,25,27-31] reported Lysholm score, according to different interventions to conduct subgroup analysis.
A total of 5 studies were included in the arthroscopy combined with Chinese medicine VS arthroscopy treatment group [14,16,21-23], with high heterogeneity (P<0.000 01, I2=94%). The sensitivity analysis speculated that the reason may be related to Wang [16] is related to the study, after the elimination found that the heterogeneity is reduced(P=0.20, I2=35%), the fixed effects model is used, as shown in Figure 4. The results showed that the Chinese medicine combination group was better in improving Lysholm score [MD=5.59, 95%CI=(4.06,7.11), P<0.000 01]. The arthroscopy combined with traditional Chinese medicine VS arthroscopy+Western medicine treatment group included a total of 4 studies [25,27-29], with high homogeneity(P=0.75, I2=0%) using a fixed-effect model, as shown in Figure 5.The results showed that the Chinese medicine combination group was better in improving Lysholm score [MD=10.50, 95%CI=(8.39,12.60), P<0.000 01]. Arthroscopy combined with Chinese medicine+ Western medicine VS arthroscopy + Western medicine group included a total of 2 studies [30,31], and found that the heterogeneity was high (P<0.000 01, I2=99%) and then used a random effects model, as shown in Figure 6. The results showed that there was no significant difference between the Chinese medicine combination group and the arthroscopy + western medicine group in improving the Lysholm score [MD=12.38, 95%CI=(-6.14, 30.90), P=0.19].
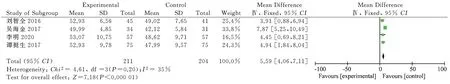
Fig 4 Forest plot of Lysholm score in arthroscopy + traditional Chinese medicine treatment vs arthroscopy treatment group
3.3.3 VAS score
8 studies [18,22-25,28-30] reported VAS score, and subgroup analysis was performed according to different interventions.
The arthroscopy combined with traditional Chinese medicine VS arthroscopy treatment group included 4 studies [18,22-24], with high homogeneity (P=0.68, I2=0%), using a fixed-effect model, as shown in Figure 7. The results showed that the Chinese medicine combination group was better in reducing the VAS score [MD=-0.60, 95%CI=(-0.94, -0.26), P=0.000 5]. Arthroscopy combined with traditional Chinese medicine VS arthroscopy + western medicine treatment group included a total of 3 studies [25,28,29],with homogeneity (P=0.28, I2=14%) using a fixed-effect model, as shown in Figure 8. The results showed that the Chinese medicine combination group was better in reducing the VAS score [MD=-0.74,95%CI=(-1.03, -0.45), P<0.000 01]. Arthroscopy combined with Chinese medicine + Western medicine VS arthroscopy + Western medicine treatment group was included in 1 study [30], 46 cases in the experimental group, 46 cases in the control group, see Figure 9.The results showed that the Chinese medicine combination group was better in reducing the VAS score [MD=-0.89, 95%CI=(-1.68,-0.10), P=0.03].

Fig 5 Forest plot of Lysholm score of arthroscopy + traditional Chinese medicine treatment vs arthroscopy + western medicine treatment group

Fig 6 Forest plot of Lysholm score of arthroscopy + traditional Chinese medicine + western medicine treatment vs arthroscopy + western medicine treatment group
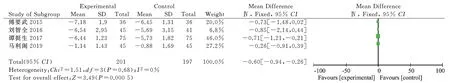
Fig 7 Forest plot of VAS score of arthroscopy + Chinese medicine treatment vs arthroscopy treatment group

Fig 8 Forest plot of VAS score in arthroscopy + traditional Chinese medicine treatment vs arthroscopy + western medicine treatment group

Fig 9 Forest plot of VAS score of arthroscopy+Chinese medicine+western medicine treatment vs. arthroscopy+Western medicine treatment group
3.3.4 Impact on UA
11 studies reported UA levels [14-16,21,24,25,27-29,31,32], and subgroup analysis was conducted according to different interventions.
The arthroscopy combined with traditional Chinese medicine VS arthroscopy treatment group included 5 studies [14-16,21,24], with homogeneity (P=0.17, I2=38%) using a fixed-effect model, as shown in Figure 10. The results showed that the Chinese medicine combination group was better in reducing UA [MD=-57.94,95%CI=(-74.20, -41.67), P<0.000 01]. A total of 4 studies were included in the arthroscopy combined with Chinese medicine VS arthroscopy + western medicine treatment group [25,27-29], with high heterogeneity (P=0.002, I2=80%) and the source of heterogeneity cannot be ruled out by sensitivity analysis. The random effects model is used, as shown in Figure 11. The results showed that there was no significant difference between the Chinese medicine combination group and the arthroscopy + western medicine group in reducing UA[MD=21.34, 95%CI=(-52.80, 10.02), P=0.18]. A total of 2 studies were included in the arthroscopy combined with Chinese medicine+ Western medicine VS arthroscopy + Western medicine treatment group [31,32], with high homogeneity (P=0.92, I2=0%) using a fixedeffect model, as shown in Figure 12. The results showed that the Chinese medicine combination group was better in reducing UA[MD=-41.19, 95%CI=(-59.70, -22.67), P<0.000 1].

Fig 10 Forest plot of UA level in arthroscopy + traditional Chinese medicine treatment vs arthroscopy treatment group
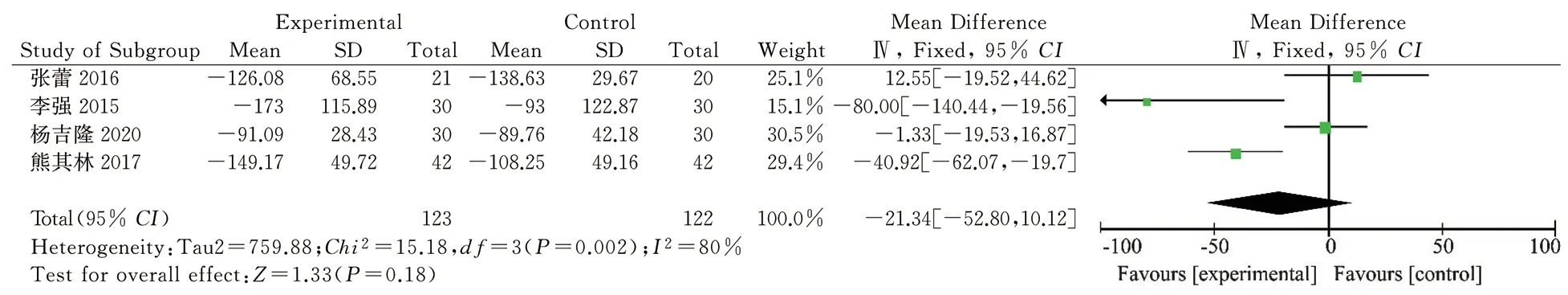
Fig 11 Forest plot of UA level of arthroscopy + traditional Chinese medicine treatment vs arthroscopy + western medicine treatment group

Fig 12 Forest plot of UA levels in arthroscopy + traditional Chinese medicine + western medicine treatment vs. arthroscopy + western medicine treatment group
3.3.5 Impact on CRP
Nine studies reported CRP levels [16,21,23-25,27,29,31,32],and subgroup analysis was performed according to different interventions.
The arthroscopy combined with traditional Chinese medicine VS arthroscopy treatment group included 4 studies [16,21,23,24], with high homogeneity (P=0.42, I2=0%) using a fixed-effect model, as shown in Figure 13. The results showed that the Chinese medicine combination group was better in reducing CRP [MD=-3.75,95%CI=(-5.44, -2.06), P<0.000 1]. The arthroscopy combined with traditional Chinese medicine VS arthroscopy+Western medicine treatment group included a total of 3 studies [25,27,29], with high homogeneity (P=0.73, I2=0%) using a fixed-effect model, as shown in Figure 14. The results showed that the Chinese medicine combination group was better in reducing CRP [MD=-6.30,95%CI=(-8.38, -4.22), P<0.000 01]. Arthroscopy combined with traditional Chinese medicine + Western medicine VS arthroscopy+ Western medicine group included a total of 2 studies [31,32],with high heterogeneity (P=0.04, I2=75%) using a random effects model, as shown in Figure 15. The results showed that there was no significant difference between the Chinese medicine combination group and the arthroscopy + western medicine group in reducing CRP [MD=-3.09, 95%CI=(-8.17, 2.00), P=0.23].
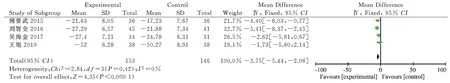
Fig 13 Forest plot of CRP level in arthroscopy + traditional Chinese medicine treatment vs arthroscopy treatment group

Fig 14 Forest plot of CRP level of arthroscopy + traditional Chinese medicine treatment vs arthroscopy + western medicine treatment group

Fig 15 Forest plot of CRP levels in arthroscopy + traditional Chinese medicine + western medicine treatment vs. arthroscopy + western medicine treatment group
3.3.6 Impact on ESR
11 studies reported ESR levels [14,16,21,23-25,27,29-32], and subgroup analysis was performed according to different interventions.
Arthroscopy combined with traditional Chinese medicine VS arthroscopy treatment group included a total of 5 studies[14,16,21,23,24], high heterogeneity (P=0.13, I2=44%) sensitivity analysis speculated that the cause may be related to the research of Wang [16] is related, after eliminating the heterogeneity found to be reduced (P=0.49, I2=0%), the fixed effects model is adopted, as shown in Figure 16. The results showed that the Chinese medicine combination group was better in reducing ESR [MD=-2.99,95%CI=(-4.30, -1.68), P<0.000 01]. Arthroscopy combined with traditional Chinese medicine VS arthroscopy + western medicine group included a total of 3 studies [25,27,29], with high heterogeneity(P=0.003, I2=83%). The sensitivity analysis speculated that the reason may be the same as that of Li Qiang 2015[29] Is related to the study, after the elimination found that the heterogeneity is reduced(P=0.38, I2=0%), the fixed-effects model is used, as shown in Figure 17. The results showed that the Chinese medicine combination group was better in reducing ESR [MD=-5.16, 95%CI=(-7.22,-3.09), P<0.000 01]. A total of 3 studies were included in the arthroscopy combined with Chinese medicine + Western medicine VS arthroscopy + Western medicine treatment group [30-32], with high homogeneity (P=0.51, I2=0%) using a fixed-effect model, as shown in Figure 18. The results showed that the Chinese medicine combination group was better in reducing ESR [MD=-4.44,95%CI=(-5.84, -3.04), P<0.000 01].
3.3.7 Adverse reactions
3 studies reported adverse reactions [25,28,32]. After statistics,it was found that 5 cases occurred in the experimental group,including 2 cases of mild abdominal pain and 3 cases of increased stool frequency; 6 cases in the control group , Including 2 cases of mild abnormal liver function, 2 cases of thinning stool, 1 case of drug eruption reaction and 1 case of gastrointestinal reaction.Meta-analysis of the adverse reaction rate found that the studies were homogeneous (P=0.35, I2=5%), so the fixed effects model was adopted, as shown in Figure 19. The results showed that the difference between the experimental group and the control group was not statistically significant [RR=0.81, 95%CI=(0.26, 2.58),P=0.72].
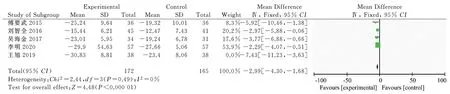
Fig 16 Forest plot of ESR level in arthroscopy + traditional Chinese medicine treatment vs arthroscopy treatment group

Fig 17 Forest plot of ESR level of arthroscopy + traditional Chinese medicine treatment vs arthroscopy + western medicine treatment group

Fig 18 Forest plot of ESR levels in arthroscopy + traditional Chinese medicine + western medicine treatment vs. arthroscopy + western medicine treatment group
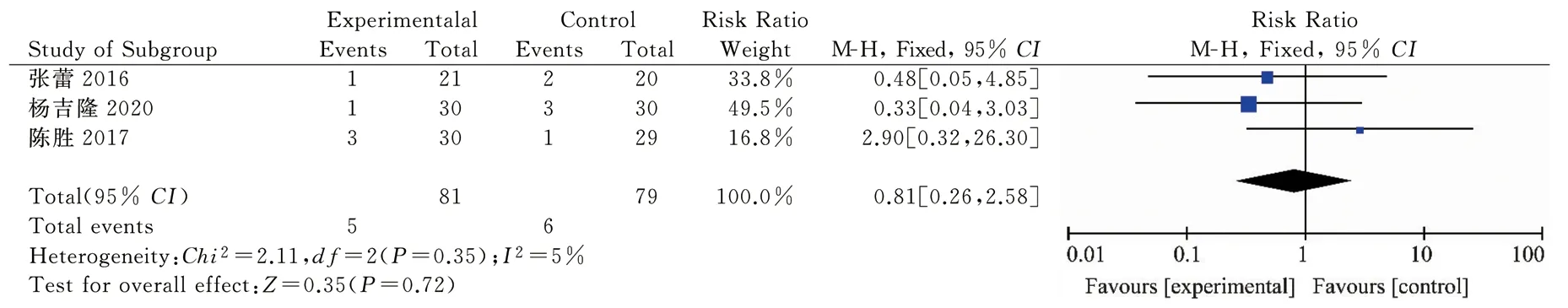
Fig 19 Forest plot for Meta-analysis of ADR rate between two groups
3.3.8 Publication biasTo draw a funnel chart for the clinical total effective rate, Lysholm score, UA and ESR, see Figure 20-23. The results show that most of the clinically effective data points are symmetrically distributed on both sides of the funnel chart's symmetry axis, and most of them are located in the middle and upper part of the funnel chart. Only one data point is scattered in the lower part of the funnel chart; Lysholm score data points are distributed in The funnel chart is mostly on the left side of the symmetry axis and some data points are scattered outside the funnel chart. It can be considered that the asymmetry is related to the heterogeneity between the studies. The UA data points are also mostly distributed on the left side of the symmetry axis of the funnel chart, and 4 data points are scattered outside the funnel chart, which is also related to the research heterogeneity. The ESR funnel chart is not completely symmetrical, and one data point is scattered outside, indicating that there may be a possibility of bias.All studies selected in this paper are positive results, and there may be methodological quality differences, which may cause publication bias.
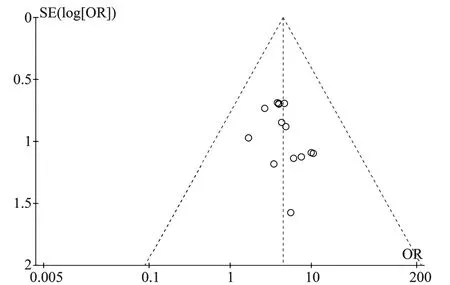
Fig 20 Funnel chart of total clinical effectiveness

Fig 21 Funnel chart of Lysholm score

Fig 22 Funnel chart of UA levels
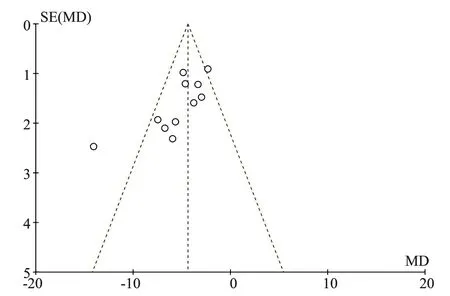
Fig 23 Funnel chart of ESR levels
4. Discussion
4.1 Commonly used Chinese medicines for gouty arthritis
Gout has long been discussed in Chinese medicine. The causes of gout in Zhu Danxi's "Gezhi Yulun" can be attributed to cold,dampness, and wind. Modern physicians also have their own opinions on gout. The causes of gout in the acute phase can be mainly classified as dampness, phlegm, heat, cold, etc., and the weakness of the viscera in the chronic phase. The most commonly used treatment drugs are heat-clearing, dampness, expectorant, and tonic drugs [33-36].
According to the collation and summary of the included 19 studies, it was found that Achyranthes bidentata, Phellodendron achyranthes, Coix seed, Atractylodes rhizome, Red peony root,Atractylodes lanceolata, Gentiana, Chuanxiong and other drugs are more commonly used in the treatment prescriptions. Cork is used most frequently. Achyranthes bidentata has the effects of drug introduction, nourishing liver and kidney, etc. Studies have shown that the total saponin in Achyranthes bidentata can inhibit NACHTLRR-PYD domain protein 3 (NALP3) and aspartate proteolytic enzyme 1 (Caspase- 1) The activation reduces the production of inflammatory factors and relieves the symptoms of gout; inhibits the chondrocyte apoptosis pathway PI3K/AKT to reduce chondrocyte apoptosis and protect the joints [37,38]. Atractylodes and Phellodendri are commonly used drug pairs for the treatment of damp-heat syndrome. Pharmacological studies have shown that baicalein and quercetin contained in the drug pairs can reduce blood uric acid levels in the body, and the compatibility can be used to supplement the single-use effect, and the ratio of anti-inflammatory The role is also different [39-41].
4.2 Evaluation of the efficacy and safety of Chinese herbal decoction combined with arthroscopy
Through the subgroup analysis of 19 studies, we found that compared with pure Western medicine and surgical treatment,the method of integrated Chinese and Western medicine can significantly improve the clinical efficacy of patients. After statistical analysis of all subgroups of each index, we found that the VAS score and For changes in ESR levels, analysis of all subgroups showed that the traditional Chinese medicine combination group was better than the single treatment group. The VAS score is a pain scale widely used in clinical practice, which can be used for sensitive and objective evaluation of pain efficacy [42]. ESR is one of the classic surrogate indicators of inflammation, and it is also a commonly used indicator to evaluate the activity status of gouty arthritis, which can reflect the inflammation control effect of gout [43]. Therefore, it can be speculated that the treatment of gout with integrated traditional Chinese and western medicine may play a good role in the control of pain and inflammation.
In addition, for the improvement of Lysholm score and the reduction of UA and CRP levels, although some subgroups have little difference, the results are statistically significant for the overall analysis. And from the point of view of adverse reactions, although traditional Chinese medicine irritates the gastrointestinal tract slightly, it does relatively little damage to liver function. Therefore, it can be explained that for the above-mentioned overall indicators, the improvement effect of taking traditional Chinese medicine decoction should be more obvious than pure arthroscopy and western medicine treatment.
4.3 Research limitations
This study still has some limitations and deficiencies: (1) The included studies have certain limitations, such as blinding, etc. are not used, which may have selection bias; (2) All studies selected in this paper are positive results, and There may be differences in methodological quality, which may cause publication bias; (3) Since this study analyzes all traditional Chinese medicine decoctions,the course of treatment is not the same, which may be the reason for the lack of homogeneity of the outcome indicators; (4) the total sample The amount is too small, only 1383 cases, and each study is a single-center trial, it is impossible to determine the influence of the researcher's subjective factors, and the stability of the conclusion may be affected.
On the whole, this study shows that for the treatment of gouty arthritis, Chinese medicine decoction combined with arthroscopy has a definite effect, which can more effectively relieve symptoms and increase the rate of good treatment. It can more quickly relieve pain and improve joint function. Reduce body inflammation and uric acid levels. However, in the future, clinical studies with larger sample sizes, more reasonable designs, and higher quality are still needed to demonstrate this conclusion.
Author's contribution degree description:
Xu Luchun, the first author, the design executive of this research,completed the literature screening, data collection and analysis,and the writing of the first draft of the paper; Li Huanan, the corresponding author of this article, overall guided the design of the research plan and criticized the content of the article; Wang Jianjun, The second author, reads the title and abstract for research screening, participates in plan design, data analysis and correction of the content of the paper. Ye Chao, the third author, participates in the process of data collection and analysis, and provides some support in statistical software; WANG Yue, the fourth author, participates in data collection and entry, participates in literature review and article content modification corrections.
杂志排行
Journal of Hainan Medical College的其它文章
- Research progress on pathogenesis of ulcerative colitis
- Advances in the application of optical coherence tomography in the assessment of ischemic stroke
- Study on syndrome distribution and medication characteristics of patients with rectal cancer in the real world
- Experimental study of TGF-β1/Smads pathway inhibition of macrophage polarization based on miR145-5P negative feedback regulation
- Exploring the key pathways of tetrandrine in the treatment of early silicosis based on bioinformatics and in vitro experiments
- Based on the theory of “Kidney-blood-bone” to explore the mechanism of GH/IGF-1 system in the prevention and treatment of osteoporosis in Qing 'e pill
