Potential role of noninvasive biomarkers during liver fibrosis
2022-01-05NavneetKaurGitanjaliGoyalRavinderGargChaitanyaTapasviSoniaChawlaRajneetKaur
Navneet Kaur, Gitanjali Goyal, Ravinder Garg, Chaitanya Tapasvi, Sonia Chawla, Rajneet Kaur
Navneet Kaur, Gitanjali Goyal, Sonia Chawla, Rajneet Kaur, Department of Biochemistry, Guru Gobind Singh Medical College and Hospital, Baba Farid University of Health Sciences, Faridkot 151203, Punjab, India
Ravinder Garg, Department of Medicine, Guru Gobind Singh Medical College and Hospital, Baba Farid University of Health Sciences, Faridkot 151203, Punjab, India
Chaitanya Tapasvi, Department of Radiodiagnosis, Guru Gobind Singh Medical College and Hospital, Baba Farid University of Health Sciences, Faridkot 151203, Punjab, India
Abstract Various types of liver disease exist, such as hepatitis and alcoholic liver disease.These liver diseases can result in scarring of liver tissue, cirrhosis, and finally liver failure.During liver fibrosis, there is an excess and disorganized accumulation of extracellular matrix (ECM) components which cause the loss of normal liver cell functions.For patients with chronic liver disease, fibrosis prediction is an essential part of the assessment and management.To diagnose liver fibrosis, several invasive and noninvasive markers have been proposed.However, the adoption of invasive markers remains limited due to their inherent characteristics and poor patient acceptance rate.In contrast, noninvasive markers can expedite the clinical decision through informed judgment about disease stage and prognosis.These noninvasive markers are classified into two types: Imaging techniques and serum biomarkers.However, the diagnostic values of biomarkers associated with liver fibrosis have also been analyzed.For example, the serum levels of ECM proteins can react to either matrix accumulation or degradation.During virus-host interactions, several regulatory steps take place to control gene expression, such as the change in cellular microRNA expression profiles.MicroRNAs are a class of non-coding RNAs (18-20 long nucleotides) that function by post-transcriptional regulation of gene expression.Although various noninvasive markers have been suggested in recent years, certain limitations have restricted their clinical applications.Understanding the potential of non-invasive biomarkers as a therapeutic option to treat liver fibrosis is still in progress.
Key Words: Liver fibrosis; Non-invasive biomarkers; Viral hepatitis; MicroRNA; Cirrhosis; Fibroscan
INTRODUCTION
The liver is the main organ of our body.The functions of the liver include synthetic functions, metabolic functions, and most importantly the detoxification and excretion of toxic substances.The synthetic functions include the synthesis of cholesterol, triglycerides, plasma proteins, and lipoproteins.The metabolic functions include the metabolism of carbohydrates, lipids, and proteins.Ammonia is converted to urea in the liver.Any injury to liver cells will lead to the alteration in these functions.Various types of liver disease exist, such as acute and chronic hepatitis, alcoholic liver disease, and non-alcoholic fatty liver disease (NAFLD).Hepatitis is essentially the inflammation of the liver, a condition that can be self-limiting, although it can progress to other adverse situations, including fibrosis, cirrhosis, or even liver cancer.There are various causes of this condition, and the most implicated ones include infections, certain drugs, toxic substances, and autoimmune diseases.Mainly, there are five different types of hepatitis, namely, A, B, C, D, and E.Alcoholic liver disease occurs due to excessive consumption of alcohol.All these diseases lead to injury of the liver parenchyma which is studied based on their stages.The stage and degree of liver disease are fundamental in the diagnosis, prognosis, treatment, as well as follow-up of all hepatic diseases.
STAGES OF LIVER DISEASE
The progression of liver disease passes through various stages, as depicted in Figure 1.The figure also shows the factors promoting liver cell injury and thereafter the progression of the disease.The stages of liver disease are discussed below.

Figure 1 Factors promoting liver cell injury leading to fibrosis, cirrhosis, and carcinoma.
Inflammation stage
There are many types of liver failure, but despite the type, the progression towards full-blown disease is the same.The first stage is associated with inflammation and typically denotes the immune system's reaction to the offending agents like toxins.In this case, the hepatitis C virus (HCV) would be responsible[1].In the process of inflammation, the liver becomes tender and greatly enlarged.Before inflammation, massive viral infection leads to an increase in the production of inflammatory cytokines, and chemokine levels are also shown to increase (they are the inflammatory biomarkers).
Fibrosis
The second stage is associated with fibrosis, which is stimulated by chronic inflammation.Fibrosis usually occurs as a result of the liver's healing process, and it happens continuously with the regeneration of the liver's damaged areas.Fibrosis is a way that wound healing takes place with a balance between fibrogenesis and fibrinolysis[2].The process of inflammation causes quiescent hepatic stellate cells (HSCs) to be activated, which then differentiate and form myofibroblasts[3].
Myofibroblasts are important in fibrogenesis and are responsible for producing several components of the extracellular matrix (ECM), which then replace the damaged tissues.When the ECM is deposited excessively, it leads to scar formation, which can be altered by fibrolysis[4].The process of fibrosis is dynamic, and it is bound to be reversed upon the resolution of the HCV infection[5].The chronic damage that stimulates fibrogenesis and insufficient fibrolysis is linked to a reduction of the reversibility potential.
Cirrhosis stage
Cirrhosis is the point where the liver is completely scarred and is beyond the selfhealing ability.The development of cirrhosis is long due and could even take decades, meaning that interventions can be started in the initial stages before getting to this point.After several injurious exposure or inflammatory responses by the different mediators, HSCs undergo a transition from the quiescent to the activated state.The damaged hepatocytes lead to the release of reactive oxygen species, and apoptosis could occur[6].
Cirrhosis occurs in two stages: Compensated cirrhosis and decompensated cirrhosis (end-stage liver disease).During the compensated cirrhosis, there is liver damage, but it is not severe enough to hinder some of the cells' functioning.At this stage, one can be asymptomatic, although portal hypertension may be present[7].The chronicity of the infection could induce G1 arrest and then impair the functioning of hepatic cells, limiting regeneration.
Recent studies have determined that shortening of the liver's telomeres and their senescence results in fibrotic tissue formation in the cirrhosis stage of liver disease.During the cirrhosis stage, some clinical features become apparent: Increased propensity to bleeding, possible development of insulin resistance, sensitivity to some medications, skin itch, and water build-up leading to edema.It is also possible for the build-up of toxins in the brain, affecting memory and other mental functions.
End-stage liver disease (decompensated cirrhosis)
This is the stage where the liver has completely failed, and neither can the cells heal; it can be both acute and chronic[8].In HCV infection, it is a chronic occurrence.This is also called decompensated cirrhosis, and it follows inflammation of the hepatocytes, which leads to fibrosis and then disruption of the liver structure and function.During this stage, there is the development of complications like jaundice, variceal bleeding, ascites, and hepatic encephalopathy.
Clinical evidence has revealed that the median survival age for decompensated cirrhosis is about 2 years, and it is a common predictor of death in patients with cirrhosis.It has also been shown that decompensation can improve once the offending agent has been eliminated[8].Failure to remove the offending agent, therefore, means that liver transplant is the only remaining solution.
ASSESSMENT OF LIVER FIBROSIS
For assessment of liver fibrosis, various methods have been proposed, including both invasive and non-invasive methods (Figure 2).However, in clinical practice, finding the most effective and the best method for evaluating liver impairment in patients remains a major challenge.This is mainly because the prognosis and effective treatment are dependent on the assessment of liver damage as well as the extent of liver fibrosis in patients.Historically, all these parameters were provided through liver biopsy.Liver biopsy is among the oldest, effective, and most accurate assessment methods of evaluating liver histology and the progression of liver damage.The comparison of the main features of both invasive and non-invasive methods is shown in Table 1.
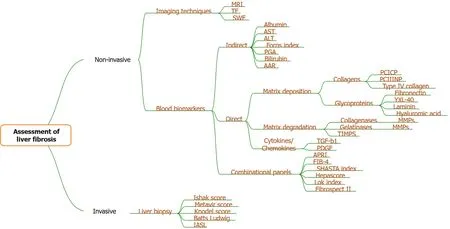
Figure 2 Various methods for assessment of liver fibrosis.
INVASIVE METHOD (LIVER BIOPSY)
As discussed by Shrivastavaet al[9], liver biopsy is a process that is considered by many experts in determining the best therapeutic approaches for patients.This is also the best approach in dealing with hepatitis C especially when it comes to chronic hepatitis.It is an invasive procedure for liver assessment[10].Consequently, liver biopsy as an assessment method of liver damage in hepatitis C patients brings forth several risks as well as sampling errors.Sampling errors in liver biopsy occur due to suboptimal biopsy size.Due to the increased risks of liver biopsy and sampling errors among other pitfalls of this assessment method, different markers have been developed.Research shows that during the pathological progression of liver fibrosis, especially in patients with hepatitis C, there is an excessive buildup of the matrix.The serum levels of different biomarkers tend to change[9].According to the authors, there are physical and biological non-invasive approaches that are based on serum biomarkers that have been proposed.
Scoring system for liver fibrosis
The scoring system of liver fibrosis assessment based on three methods,i.e., International Association of Study of Liver (IASL), Batts-Ludwig, and METAVIR scores are depicted in Table 2[11].
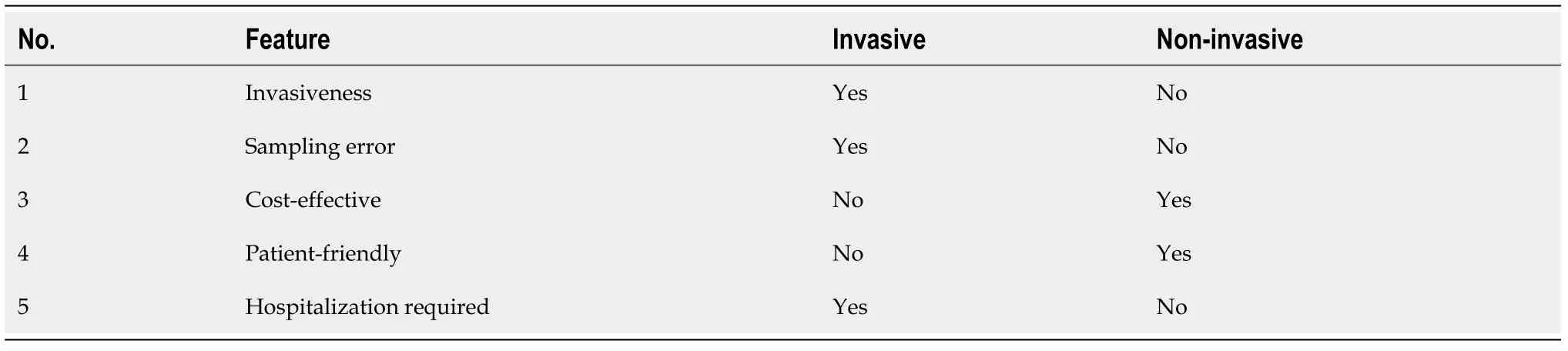
Table 1 Comparison of characteristics of invasive and non-invasive methods
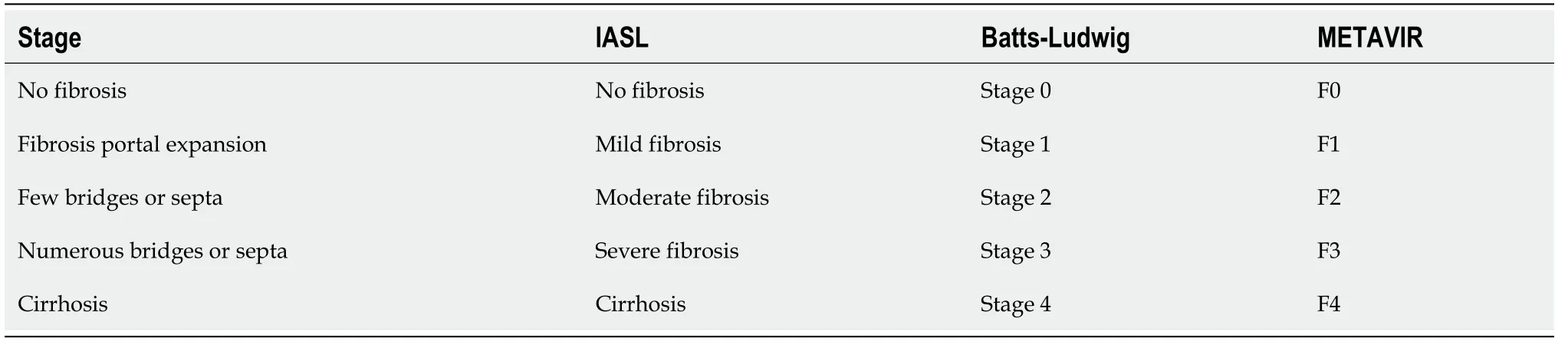
Table 2 Scoring systems for liver fibrosis
Limitations of liver biopsy
There are several limitations of liver biopsy that have led to the development and replacement of the assessment method with non-invasive biomarkers as an assessment method of liver damage and liver fibrosis in patients with hepatitis.One of the limitations of liver biopsy is that this method does not efficiently reflect the different fibrotic changes that may be occurring in the entire liver.This is mainly because any optimally sized liver biopsy contains a small number of complete portal tracks that reflect a small volume of the liver[12].Besides, the process of hepatic fibrosis is not liners.As a result, to cover hepatic fibrosis in the entire liver, biopsies have to be conducted on different areas of the liver.Besides, research shows that liver biopsies may miss cirrhosis in patients with hepatitis C.This is mainly because liver biopsy cannot differentiate between early and progressed cirrhosis.Consequently, liver biopsy cannot be relied upon as an ideal and accurate prognostic predictor[12].
Research shows that there are several risks of complications that tend to arise from liver biopsy[13].Most of these complications, however, carry symptoms such as injury to the biliary system, mild abdominal pain, and severe hemorrhage.The occurrence of such complications as a result of liver biopsy may increase hospitalization.There is variability in the interpretation of pathologists which is yet another limitation of liver biopsy.Research shows that biopsy cannot be conducted in hepatitis patients with diabetes, ascites, metabolic syndrome, and coagulopathy.Although liver biopsy has been considered as a keystone for the diagnosis of liver damage in patients with liver diseases such as hepatitis C, the invasive procedure has significant limitations mainly due to surgical complications and sampling heterogeneity.
NON-INVASIVE TECHNIQUES FOR LIVER DAMAGE ASSESSMENT
There are various methods in which non-invasive biomarkers are used to assess the damages in the liver.A conclusion reveals that through these assessments, experts canunderstand more about liver disease and analyze the various approaches which can be relied upon in managing the condition of the patient[13].These methods are distinctively classified into two, the natural or physical approach and the biological approach.The physical approach is majorly used with various imaging techniques while the biological method is based on the popular serum biomarkers[14].The two methods are quite distinct in the way that the conditions are valued and assessed but they are both based on conceptions and rationales that are quite different.
PHYSICAL APPROACH
There are many types of physical approaches that experts rely on in assessing liver conditions.These physical approaches include Doppler analysis, computed tomography, acoustic radiation force impulse imaging, transient elastography (TE), ultrasonography, magnetic resonance imaging, and real-time elastography.Menessyet al[13] also discuss that most of these methods are based on scanning and imaging techniques by which the experts analyze the liver and the condition of the systematic process.There are some of these methods that are widely considered more than others.There are the ones that are quite fast enough for experts while there are the slow ones.Some provide a distinct value of images or scans that can be relied on comfortably.
Transient elastography
TE is the most appropriate approach due to its speed.Fallatah[15] discusses that on top of that, the approach is quite reproducible and at the same time does not depend on operators.The approach is also quite common among many hepatitis experts since it provides and measures the stiffness of the liver and compares the same stiffness and its elasticity.With such considerations, it is quite easy to analyze the conditions of hepatitis and also conduct the corresponding analysis of its physical properties, which is highly genuine.The technique is also considered for its ability to predict the issues around severe fibrosis and also its accuracy in identifying cases of liver cirrhosis that are underlying the hepatitis condition.There are, however, issues of the method’s examination of fibrosis which are mostly associated with this disease.In some cases, the approach is unable to provide information that is quite sufficient for experts to diagnose cases of significant fibrosis especially with the main consideration being the hepatitis C condition.This means that the technique does not provide distinct stages and processes for the analysis of the condition, and that there should be experts to analyze and interpret the information provided through the technique despite the results from the basic approach being straightforward.This means that an expert, who has been aware of and dealt with the clinical background of the patient, especially with his or her case of hepatitis C, should be at the center of measurements and results[15].
When compared with the METAVIR score of liver biopsy, the sensitivity and specificity of the cut-off value of TE are shown in Table 3[16].

Table 3 Correlation of transient elastography cutoffs with METAVIRscore
Shear wave elastography
This has been a recently developed method for measuring liver elasticity.It has been considered that it is a reliable non-invasive tool for monitoring liver stiffness in HCV patients with an accuracy of 97.6%.It is a novel, rapid, and noninvasive method for measuring liver stiffness.It determines liver stiffness by estimating the velocity of shear waves emitted in the liver tissue.Moreover, the velocity of this shear wave (i.e., lateral wave) is calculated.The benefit of this mode of assessment is that the real-time images are seen with the help of a normal B-mode ultrasound probe[17].
The area under the receiver operating characteristic curve (AUROC) for F > 2 and F4 were found to be 0.87 and 0.93, respectively[18].Shear wave elastography was 85% specific and 79% sensitive when compared with the METAVIR score by taking a cutoff value of 1.34 for the F2 stage of fibrosis[19,20].
BIOLOGICAL APPROACH
Many developments have been realized across all industries.Among these industries are the medicine and clinical areas.A new era of biotechnology and biomedicine has taken a central part in developing our clinical and medical worlds.Stasi and Milani[21] make consideration that over the years, the world of medicine has seen major developments with tremendous strides having been realized in both the biotechnology and biomedical world[13].This has brought up a new generation of medical approaches that are characterized by rapid, novel, and non-invasive approaches.These approaches have brought up some challenging ideas of the previous settings of medicine with major changes being recognized in the invasive diagnostic and therapeutic approaches.Some characteristics need to be fulfilled by the non-invasive methods, with most of these being the factors of accessibility, simplicity, high accuracy, and being liver-specific, satisfactorily validated, and easily interpretable[14].
Class I biomarkers (direct) to assess liver fibrosis are the remnants of liver matrix components.These are formed by HSCs during ECM remodeling.These markersdirectly reflect either deposition or removal of ECM[22].
Whereas indirect (class II) markers include routine investigations such as alanine aminotransferase (ALT), aspartate aminotransferase (AST), serum bilirubin, gammaglutamyltransferase (GGT), haptoglobin, and α2-macroglobulin.These markers are not specific for assessing intermediate stages of fibrosis[23].
Combinational panels by computing indirect markers have also been studied.These include fibrosis-4 (FIB-4), APRI (AST to platelet count ratio), SHASTA index, Fibroscore, Hepascore, and Lok index.
Class I biomarkers (direct)
Over the years, there have been major demands to understand the pathophysiology of the liver better.This has prompted and enabled many scientists and experts in this field to establish major research while investigating the major developments in the area.Class 1 biomarkers are therefore types of non-invasive biomarkers that mimic the liver metabolism and its ECM.It has been considered that though majorly associated with the fibrosis stages, these biomarkers are also associated with the fibrogenic cells and the changes that are majorly seen in the same[10].It has been discussed that besides measuring and assessing the conditions of the liver concerning the hepatitis C condition, these biomarkers have another clinical usefulness in which they assess the rate at which other underlying issues progress besides staging the liver fibrosis[24].As revealed by Stasi and Milani[21] with such assessments done by the biomarkers, the same data and measurements from the assessment are turned or else translated into prognostic information that is quite effective.This is then made as a tool in which responses are evaluated.In the long run, they also help in monitoring the efficiency of the associated ant fibrotic drugs.This is where the data that is provided in these circumstances gets to be used as variables for the performance and availability measurements.The direct markers are classified as below.
Direct markers linked with matrix deposition: Collagens and glycoproteins
Collagens:These direct markers are found in the connective tissues and have three types.Pro-collagen is the precursor of the collagen which is cleaved by two different enzymes at amino (type 3) and carboxyl (type1) terminal ends to form collagens[25].The collagens formed are procollagen type 1 (PCICP) and procollagen type 3 (PCIIINP).PCICP is the main component of connective tissue[25].The upper limit of normal values is 202 and 170 µg in males and females, respectively[26-28].It is increased in cirrhosis progression.PCIINP is increased with fibrotic stage and correlates well with bilirubin levels in cirrhosis cases[29-31].The only drawback of this marker is that it increases in other medical conditions also.Also, the efficacy is decreased as compared to hyaluronic acid (HA)[27,31].Type IV collagen is the third collagen serving as a direct marker.It acts as a surrogate marker to assess liver fibrosis[32].Its levels are manifold increased in liver diseases and correlate well with fibrosis[33,34].An area under the curve (AUC) of 0.82 with a negative predictive value (NPV) of 83.6% was found with a cut-off value of greater than 5.0 ng/mL in NAFLD[34].
Glycoproteins:HA is an example of a direct serum marker used in the diagnosis of liver damage in patients[35].It is integrated and dispersed all over the extracellular space.This process is done by the HSCs.The damaged liver tends to provide HA in high quantities.As a result, this marker is used to predict the level of liver damage based on elevated serum levels.This is because the levels of HA correlate with liver fibrosis[36].Research shows that the HA serum direct marker is more accurate than most non-invasive indices.However, this method of diagnosis works best when combined with other liver markers.NPV was 98%-100% in cirrhosis[35-38].Also, HA levels start decreasing with the treatment of liver disease[39-41].Laminin is a glycoprotein that is non-collagenous and is formed by the HSCs[10].In a patient with liver fibrosis, elevated levels of laminin correlate well with the degree of the fibrosis.However, its diagnostic value is not of much significance when compared with HA.The cut-off value of 1.45 was proposed by Sebastiani[32] for detecting fibrosis and cirrhosis.It is 77% accurate for detecting fibrosis in HCV cases.YKL-40 is another diagnostic tool used to assess liver damage in patients with hepatitis C.It is a mammalian homologue of bacterial chitinases which are involved in the remodeling or degradation of ECM[21].The levels of YKL-40 correlate with the severity of fibrosis.Fibronectin (FN) is a high molecular weight glycoprotein of the ECM which binds to integrins (receptor proteins).It is synthesized by various cells but mainly by hepatocytes.In blood, FN exists in two major forms,i.e., cellular FN (cFN) and plasma FN (pFN)[42].
Direct markers that are associated with matrix degradation: Collagenases, gelatinases, and tissue inhibitors of matrix metallo proteinases
Collagenases:Metalloproteinase-1 (MMP-1) is found to be inversely correlated with necrosis as well as fibrosis[43].
Gelatinases:Two matrix metalloproteinases MMP-2 and MMP-9 have been found.They are also known as gelatinases,i.e., gelatinase A and B, respectively.Previously, MMP-2 was found to have no significant association with liver fibrosis stage[44,45].But later Boekeret al[44] found an accuracy of 92% for detecting cirrhosis in HCV patients.It is increased by 2.4 folds in HCV patients as compared to controls.MMP-9 is inversely correlated with histological severity in hepatitis.Its levels start decreasing as cirrhosis progresses[46,47].
Tissue inhibitors of matrix metallo proteinases:They interact with MMP functioning and further lead to ECM degeneration inhibition.It shows a positive correlation with fibrosis stage[45-48].
Cytokines/chemokines in liver fibrosis
These include transforming growth factor (TGF)-β1, TGF-α, and platelet growth factor (PDGF).TGF-β1 correlates well with fibrosis in HCV-infected patients.The value of < 75 ng/mL is considered to be normal[49,50].TGF-α is found to be more correlated with fibrotic stage in hepatocellular carcinoma (HCC)[51].PDGF levels are associated with liver fibrosis and a cut-off value of 40.50 ng/L is an indicator for inflammation and fibrosis[52].
Class II biomarkers (indirect)
Back in the day, the first approach that majorly assessed the conditions of the liver and issues like hepatitis C and liver fibrosis included hematological tests and routine biochemical tests which are classified as non-invasive biomarkers.Class II biomarkers are also referred to as indirect biomarkers.They are mostly based on common functional alterations in the liver and the evaluations that are attached to the same[13].These alterations, however, do not reflect the turnover and changes associated with the fibrogenic cells.For the class II biomarkers, the basis of the measurements and evaluation is algorithmic and single elaboration.These are mainly based on the alterations that have been observed in the liver and its functions.
AST/ALT ratio: The AST/ALT ratio (AAR) index is an example of an indirect serum marker used in the diagnosis of liver damage in patients with hepatitis C.However, it is important to note that when the stages of fibrosis are not advanced, the performance of the AAR index is low[13].Haukelandet al[53] validated this test in different liver diseases.The ratio of more than 1 predicts liver cirrhosis[54,55].
APRI:It provides a quick estimate for predicting severe fibrosis or cirrhosis[56].This is among the most validated noninvasive biomarkers[13].APRI was calculated as [AST level/AST (upper limit of normal)]/[platelet count (109/L)] × 100.It was originally developed by Waiet al[57] in 2003.The AUC was 0.8 and 0.89 for fibrosis and cirrhosis, respectively.Loaeza-del-Castilloet al[56] found that it is not a diagnostic marker in autoimmune hepatitis.
BARD score:This is the combination of AAR and body mass index (BMI) and other measures of diabetic patients.NPVs of 96% and 81.3% were found[58].
ALT: Due to its high sensitivity as well as specificity, it is used as a better indicator of liver disease[59].
Forns index: It involves parameters like age, platelet count, cholesterol, and GGT[60].Forns index was calculated as [7.811 - 3.131 × ln(platelet count)] + [0.781 × ln(GGT in IU/L)] + [3.467 × ln(age) - 0.014 × cholesterol in mg%].It differentiates mild fibrosis from severe fibrosis.
PGA and PGAA index:PGA is used to assess fibrosis in alcoholics[61].A combination of prothrombin index, GGT, and apolipoprotein A is used in calculating PGA.It is considered 65% accurate in detecting liver fibrosis.Furthermore, a2 macroglobulin was added and PGAA was invented.It has a 70% accuracy in detecting fibrosis[62].
FIB-4:It is a simple, fast, and cheap test that gives immediate results[23].It is a validated test used for detecting hepatitis B and C.The AUC of 0.85 and 0.81 for detecting severe fibrosis was found in HCV and HBV, respectively[63,64].IB-4 was calculated as [Age (years) × AST (U/L)]/[Platelet count × √ALT (U/L)]
Fibroindex:It is a simple scoring system[65].It showed an AUC of 0.83 for fibrosis detection.Also, a cutoff value of 2.25 was strongly associated with F2-F3 fibrosis stage with an NPV of 90%[65].Fibroindex was calculated as [1.738 - 0.064 × platelet count (104/mm3)] + [0.005 × AST (U/L)] + [0.463 × gamma globulin (g/dL)].
Fibrotest:It includes certain parameters like age, gender, haptoglobin, a2 macroglobulins, apolipoprotein A1, GGT, and serum bilirubin[66,67].This is considered as a most validated marker for detecting liver fibrosis[68,69].
Acti test:A simple addition of ALT in Fibrotest was made which reflects liver fibrosis as well as necro-inflammatory activity[70,71].Acti test is a parameter that was initially validated for patients with chronic hepatitis B and C.It was used in collaboration with the Fibrotest as an alternative to liver biopsy.The Acti test combines five components of the Fibrotest and ALT.The assessment is crucial for treatment prescription especially in patients with moderate or severe necro-inflammatory activity as well as cirrhotic patients.
Tests for NAFLD:Initially, the simplest test was developed by using age, BMI, platelet count, ALT: AST ratio, serum albumin, and glycemic status[72].AUC was calculated as 0.88 with an NPV of 93%.Steato test was later proposed by combining fibrotest and Acti test[73].A cut-off value was fixed at 0.7 with a 90% specificity.
MICRORNAS AND THEIR BIOSYNTHESIS
MicroRNAs (miRNAs) are also nowadays considered potential biomarkers in assessing liver fibrosis.They are small non-coding strands of RNA, responsible for the regulation of the expression of genes after the transcription process.They usually target and regulate the biological processes and then influence the complex programs of the expression of genes in several cellular processes[74].Notably, miRNAs are deemed principal regulators that control main cell functions in several physiological and pathophysiological processes.
The biogenesis of miRNAs is made up of two cleavage pathways; after forming the mature miRNA, there is one nuclear and one cytoplasmic.The miRNA precursors are sorted into different pathways.However, the process is unclear but appears to be determined by the site where the miRNA originates, the sequence, and even the thermodynamic stability[75].Regulatory functions of miRNAs occur through the silencing complex induced by RNA, specific for a particular miRNA.
MiRNAs are usually transcribed from the introns and exons of the genes responsible for protein-coding or the intergenic areas.The transcription of the miRNA genes is the basis of primary transcripts, which contain the hairpin structure that consists of a terminal loop and a double-stranded stem.Later, there is then cleavage of the stem-loop structure with the help of the RNase III-like enzymes that are known as Drosha and the binding partner DGCR8[76].The result is the formation of the precursor miRNA (pre-miRNA).
There is then the transfer of pre-miRNA from the nucleus into the cytoplasm, and this is helped by exportin-5 and the accompanying co-factor Ran-GTP.The GTP is bound to the Ras-related nuclear protein.The cofactor is then processed into a structure that is duplex by the RNA polymerase II dicer.When an miRNA binds to its target, it leads to the degradation of the target mRNA or the suppression of the mRNA translation[76].Figure 3 depicts the entire process of miRNA biogenesis.

Figure 3 Process of microRNA biogenesis.
More than 1500 miRNAs have been determined in the human genome, which are involved in the cell processes, including the development, differentiation, and proliferation of cells, the process of death, the pathology, and defense against viruses.
MiRNAs are essential in the process of the pathogenesis of HCV infection through the control of the signaling pathway.In this regard, they play a role in the response of both the innate and adaptive immune systems.MiR-122 has been determined to be the most abundant miRNA in the normal liver parenchyma, and it accounts for more than 70% of the miRNAs found in the hepatocytes[77].The miR-21 gene is located on chromosome 17, and it is highly conserved.Inside the cell, miRNA-21 is found in the cytosol and the extracellular exosome.At the organ level, miRNA is located in the bone marrow, lungs, kidney, peripheral blood, colon, intestines, and thyroid.
When miR-122 binds to a 5’-untranslated region (5’-UTR) of the genomic constituent of HCV RNA, which is critical for the replication of the virus, it then stimulates translation of the viral protein and then protects HCV RNA that is uncapped from the process of degradation.Over time, the upregulation of the miR-21 leads to the feedback of inhibition of type I interferon, which is mediated by the antiviral response.This then promotes viral replication[78].Moreover, miR-21 is detected in the oncogenic miRNA and controls the process of cell cycle and tumorigenesis.
As indicated above, miR-21 is a contributor to the development of fibrogenesis in the muscles and various organs, including the liver.Clinical data has demonstrated that miR-21 is always upregulated in the liver of patients who have biliary atresiainduced liver fibrosis.MiR-21 can induce fibrosis through activation of HSCs and then collagen synthesis.The overexpression of miR-21 leads to the promotion of oxidation, and this then increases the production of collagen, which in return, activates angiotensin.MiR-21 can affect the expression of several proteins by binding to the 3’-UTR of specific mRNAs.This results in a complex interaction network as a result of downstream effects of the signaling pathways[76].Various signaling pathways have been identified to be the basis of the pathophysiological fibrosis process, including the phosphoinositide 3-kinase, TGF-β/Smads, and the extracellular signal-regulated kinase (ERK)/mitogen-activated protein kinase pathways[79].
Activation of angiotensin occurs through several pathways: Spry1/ERK/NF-κB, PTEN/Akt, programmed cell death 4/AP-1, and Smad7/Smad2/3/NADPH oxidase 4.In recent findings, research has been able to elucidate that a moiety that is deficient in the methionine choline diet of NASH is linked to liver damage[79].MiR-21 then results in a decrease of steatosis, lipo-apoptosis, and inflammation with impairment of fibrosis.Recent findings have shown that antisense inhibition or the deletion of genes of miR-21 does not alter the HSC activation or fibrosis.MiR-21 is frequently upregulated in human beings with solid malignancies like breast, colon, pancreas, lung, and liver tumors[79].MiR-21 has also been shown to be a survival factor in the course of liver injury and the development of HCC.
MiR-449a is found to be dysregulated in hepatitis C infection only.Its significance is not found in alcoholics and NAFLD.It regulates YKL-40 by targeting the NOTCH signaling pathway in HCV infection[80].Also, the expression of miR-155 was significantly increased, which further led to tumorigenesis by modulating the Wnt signaling pathway[81].
NOVEL FINDINGS SUPPORTING IMPORTANCE OF NONINVASIVE MARKERS
According to Menessyet al[13], noninvasive markers are crucial.This is mainly because these procedures are effective in the evaluation of the stage of liver fibrosis in patients with hepatitis C whereby there are no clear indications for liver biopsy.Liver biopsy is not ideal for frequent development.Given the rapid development of new medications for the treatment of hepatitis C, there is an increased need for frequent evaluations of liver damage and liver fibrosis.Consequently, the use of non-invasive assessment methods for liver fibrosis in patients with hepatitis C is crucial.
For HCV infection, there are high chances of developing liver cirrhosis and liver fibrosis in some patients.This means that physicians examining a patient should be keen to verify the infections that are underlying in cases of the main condition which is hepatitis C.The presence of non-invasive biomarkers makes all these possible by establishing a process in which the necrotic processes and the inflammatory activities are considerably detected and analyzed.These biomarkers help in establishing a clear process of detecting the major changes in the liver as the patient deals with hepatitis C.The non-invasive biomarkers generally help in forecasting the main course that the HCV takes[13].
Similarly, Stasi and Milani[21] assert that non-invasive assessment methods for liver fibrosis tend to be readily available, simple, reliable, safe, inexpensive, and wellvalidated.As a result, they are effective in evaluating the progression of liver disease.Non-invasive biomarkers offer numerous advantages over liver biopsies.Some of these advantages include the absence of adverse effects and reduced risks of sampling errors.These bring about objectiveness when it comes to the interpretation of the results.Noninvasive biomarkers lack any reported ceiling effect hence effective as compared to liver biopsy Noninvasive assessment methods are appropriate as they allow for repeated assessment.
Various researchers argue that by definition, noninvasive biomarkers, however, cannot outperform liver biopsy even though they tend to be more accurate in the assessment of liver fibrosis.This is because of the method as well as its limitations.Some of its limitations are unreliability and feasibility especially in obese patients or under limited operator experience.The procedure is also contradicted during ascites, pregnancy, and implanted cardiac pacemaker patients.Besides, the knowledge of noninvasive biomarkers is still incomplete.This poses a challenge to clinical practice since it greatly hinders the development of accurate treatment and noninvasive diagnostic means with adequate sensitivity for liver fibrosis[24].
Similarly, Oksuzet al[82] affirm that for the assessment of necroinflammatory histological activity, few biomarkers have been proposed.Fallatah[15] argues that improving the accuracy of noninvasive biomarkers is essential for a correct diagnosis of liver damage in patients.This can be done using serum-based algorithms as sequential and simultaneous procedures.In a study, the comparison of TE to liver fibrosis was done[83].The authors found that TE performed better in predicting all stages of fibrosis as well as severe fibrosis.Fibroscan values showed a good correlation with the levels of fibrosis markers.Also, the Fibroscan value of 15KpA was a significant separation limit for differentiating advanced fibrosis stages (F3 and F4).They suggested that these Fibroscan values are clinically useful to predict fibrosis stages in chronic hepatitis patients[84].Other researchers correlated Fibroscan with fibrosis degree in liver biopsy and stated that it can be used as a noninvasive tool to diagnose moderate fibrosis[85].Recently, there has been increased interest in detecting liver fibrosis through the application of non-invasive techniques.The APRI is the most useful score to predict fibrosis[56].Attallahet al[86] found that FN discriminant scores based on FN, APRI, and albumin can be used to predict liver fibrosis (Table 4).

Table 4 Sensitivity and specificity of non-invasive biomarkers in liver fibrosis
PROS AND CONS OF NON-INVASIVE BIOMARKERS
Various authors had made the remarks that non-invasive biomarkers can be used instead of liver biopsy because its acceptance has faced some key resistance from different sectors[14].Some of the factors that bring the cases of resistance are attached to the paucity of well-designed studies and literature that discuss the non-invasive methods extensively giving a view of both sides.There are also issues with the validation of some of the non-invasive biomarkers and proposals for some of them in terms of the lack of validated data.With the ones that their proposals have been provided, some changes in terms of assessing the severity and the growth rate have not been discussed and analyzed extensively[12].As per Menessyet al[13] for others, there has not been enough time to validate them in terms of testing and analysis in their use when it comes to the cases of hepatitis C[9].What is needed in most of these cases is the specific etiology validation, especially for most of these non-invasive biomarkers.In these cases, each etiology should be considered to deal with the issues of the specific pathogenesis, associated comorbidities, and natural history.
In the clinical practice related to the hepatitis condition, there should be a careful evaluation of all risk factors that are attached to failure and errors that can be associated with the specific non-invasive tools or biomarkers.A careful evaluation is needed to interpret the result and measurements adequately[21].For the liver biopsy, a key concern for most experts is to note the role that these non-invasive biomarkers play in achieving the right clinical practice.With these biomarkers, most of these experts can create a cost-effective and attractive approach that is quite better and advantageous than the liver biopsy.
It has been revealed that the biomarkers are substantially less invasive, which provides a different experience for the clinical experts[9].Besides the same advantage, other significant factors make them better than the biopsy.First, they practically have no or fewer sampling errors which enable a sufficient and efficient approach in the analysis and assessments.On the other hand, they also have very few complications that are related to health and clinical advancements.Shrivastavaet al[9] make a point that the observer-related variability is also very small, which explains the high considerations from different experts.Lastly, the measurements and assessments may be performed and considered repeatedly even from different labs, and the instruments and the equipment for this process do not need to be complicated.This means that they can allow for the dynamic monitoring of the health condition and other issues related to liver damage.This underlines the huge role that biomarkers play in assessing and proposing the conditions of the liver which is the main body part affected by the disease.
CONCLUSION
We agree with the above discussions that the use of two or more noninvasive biomarker methods will increase the accuracy of an individual to be assessed for fibrosis.In such case, the choice of the algorithm to be used in the combination in clinical practice should be based on some specific considerations.Considerations that must be made include what is locally available, what is not related to the patient’s comorbidities, what is recently validated, and the method that the physician feels comfortable to use.We have found that a combinational panel of noninvasive biomarkers is cheap and simple as compared to the use of individual biomarkers and liver biopsy.Finally, we would suggest that one or more direct biomarkers along with one imaging technique can be used for the assessment of liver fibrosis.
杂志排行
World Journal of Hepatology的其它文章
- Non-alcoholic fatty liver disease in irritable bowel syndrome: More than a coincidence?
- Liver-side of inflammatory bowel diseases: Hepatobiliary and druginduced disorders
- Gastrointestinal and hepatic side effects of potential treatment for COVID-19 and vaccination in patients with chronic liver diseases
- Genotype E: The neglected genotype of hepatitis B virus
- One stop shop approach for the diagnosis of liver hemangioma
- Liver function in COVID-19 infection
