Assessing the accuracy of arthroscopic and open measurements of the size of rotator cuff tears: A simulation-based study
2021-12-28DimitriosKitridisDimosthenisAlaseirlisNikolaosMalliaropoulosByronChalidisPatrickMcMahonRichardDebskiPanagiotisGivissis
Dimitrios Kitridis, Dimosthenis Alaseirlis, Nikolaos Malliaropoulos, Byron Chalidis, Patrick McMahon, Richard Debski, Panagiotis Givissis
Dimitrios Kitridis, Dimosthenis Alaseirlis, Byron Chalidis, Panagiotis Givissis, 1st Orthopaedic Department, Aristotle University of Thessaloniki, School of Medicine, Thessaloniki 54124, Greece
Nikolaos Malliaropoulos, William Harvey Research Institute, Centre for Sports and Exercise, Barts and The London School of Medicine and Dentistry, Queen Mary, University of London, London EC1M 6BQ, United Kingdom
Patrick McMahon, McMahon Orthopedics and Rehabilitation, University of Pittsburgh, Pittsburgh, PA 15203, United States
Richard Debski, Department of Bioengineering, Swanson School of Engineering, University of Pittsburgh, Pittsburgh, PA 15219, United States
Abstract BACKGROUND Arthroscopic procedures are commonly performed for rotator cuff pathology. Repair of rotator cuff tears is a commonly performed procedure. The intraoperative evaluation of the tear size and pattern contributes to the choice and completion of the technique and the prognosis of the repair.AIM To compare the arthroscopic and open measurements with the real dimensions of three different patterns of simulated rotator cuff tears of known size using a plastic shoulder model.METHODS We created three sizes and patterns of simulated supraspinatus tears on a plastic shoulder model (small and large U-shaped, oval-shaped). Six orthopaedic surgeons with three levels of experience measured the dimensions of the tears arthroscopically, using a 5 mm probe, repeating the procedure three times, and then using a ruler (open technique). Arthroscopic, open and computerized measurements were compared.RESULTS A constant underestimation of specific dimensions of the tears was found when measured with an arthroscope, compared to both the open and computerized measurements (mean differences up to -7.5 ± 5.8 mm, P < 0.001). No differences were observed between the open and computerized measurements (mean difference -0.4 ± 1.6 mm). The accuracy of arthroscopic and open measurements was 90.5% and 98.5%, respectively. When comparing between levels of experience, senior residents reported smaller tear dimensions when compared both to staff surgeons and fellows.CONCLUSION This study suggests that arthroscopic measurements of full-thickness rotator cuff tears constantly underestimate the dimensions of the tears. Development of more precise arthroscopic techniques or tools for the evaluation of the size and type of rotator cuff tears are necessary.
Key Words: Shoulder; Arthroscopy; Simulation model; Rotator cuff tear; Supraspinatus tear; Cuff tear size
INTRODUCTION
Rotator cuff (RC) tears are the most common tendon injury in adults, often resulting in debilitating symptoms related to both daily and sports activities[1-3]. After the failure of conservative regimens, these patients are usually treated with surgical repair of the tear[1]. Arthroscopy is the preferred surgical option for rotator cuff repair, giving a better intraoperative evaluation of the dynamic shoulder anatomy, preserves the muscle integrity, is associated with lower postoperative morbidity, and provides equal or better results compared to open techniques[4,5].
Repair techniques are based on many factors including patient characteristics, muscle quality, mobility of the tendons, and intraoperative evaluation of the size of the tear[4,6-9]. Therefore, accurate intraoperative measurement of the size of the rotator cuff tear is crucial. Especially in certain techniques such as superior capsule reconstruction, precise measurements of the tears’ dimensions are crucial for the correct sizing of the graft[10-12]. Previous studies have compared magnetic resonance imaging (MRI) measurements with arthroscopic evaluation, and focused on the MRIs ability to detect shoulder pathology in general, and not on the arthroscopic accuracy to evaluate the dimensions of different types of rotator cuff tears[13-15].
Our purpose was to compare the arthroscopic and open measurements with the real dimensions of three different patterns of simulated rotator cuff tears of known size using a plastic shoulder model. We utilized surgeons of three different levels of experience and compared the accuracy between them. The hypothesis of our study was that the size of a rotator cuff tear can be estimated accurately and equally with both arthroscopic and open techniques. To our knowledge, there is currently no research implementing this study design.
MATERIALS AND METHODS
The study took place at the Musculoskeletal Research Center in Pittsburgh, PA, USA. A plastic shoulder model (ALEX shoulder model, Sawbones Inc, Vashon, WA, Figure 1), a 30-degree arthroscope (Linvatec, Largo, FL) through the posterior portal, and a high-definition video system were utilized. Three sizes and patterns of fullthickness rotator cuff tears (a small U-shaped, a larger U-shaped, and a crescent-type, Figure 2) were created using computer software. Dimensions close to the cut-off point of medium and large tears (3 cm) were chosen, according to the DeOrio and Cofield classification system (Table 1)[16]. The simulated tear patterns were printed on paper with adhesive backing and placed in the location of the soft tissue element of the model simulating the supraspinatus tears location. The simulated tears with these computerized measurements had a precision of 0.1 mm.
Six orthopaedic surgeons were enrolled in the study and they were blinded to the computerized measurements: two senior residents with fellowship training, two fellows and two senior staff surgeons, all of the Sports Injuries and Shoulder Surgery Department. We asked them to measure the dimensions of the tears arthroscopically, repeating the procedure three times at weekly intervals. Viewing was from the lateral portal and measuring from the lateral portal, constantly. We used a probe calibrated in 5mm intervals and with a 5 mm tip, reflecting the usual practice. During all arthroscopic measurements, the shoulder model was completely covered, so the observers could not have direct vision of the simulated tears (Figure 1B). When all arthroscopic measurements were completed, the shoulder model was uncovered and the plastic cover was also removed. Each surgeon used a surgical ruler for a single measurement to simulate the open technique.

Figure 1 The ALEX plastic shoulder model.
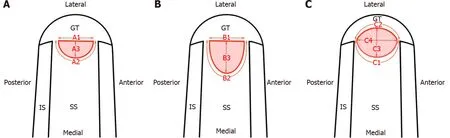
Figure 2 Three pattern of supraspinatus tears were created using computer software and were printed on paper with adhesive backing.
Statistical analysis
The mean differences between the arthroscopic measurements of the tears compared to the open and computerized measurements were calculated. Comparisons between the overall mean differences between the groups in pairs, using Wilcoxon signed ranks test, with< 0.016 as the level of significance using the Bonferroni correction were then performed.
Subsequently, the subgroups of the separate dimensions’ measurements were evaluated, using Wilcoxon signed ranks test, with< 0.05 as the level of significance. Finally, the measurements between the surgeons with the different levels of experience were compared using Wilcoxon signed ranks test, with< 0.016 as the level of significance using the Bonferroni correction.
The mean value of the three consecutive arthroscopic measurements were used for the analyses that was then performed with the Statistical Package for Social Sciences (SPSS, IBM) software version 24.
RESULTS
Arthroscopic vs computerized measurements
A statistically significant underestimation of the dimensions of the tears when measured arthroscopically was observed (< 0.001) (Table 2). The largest mean differences of the separate measurements were -7.6 ± 5.8 mm in the contour length of the small U-shape tear, -4.5 ± 3.1 mm in the anterior to posterior height of the crescenttype tear, and -3.1 ± 3.1 mm in the contour length of the large U-shaped tear (Table 3). All mean differences were negative (Table 3), showing the constant underestimation of the dimensions. The accuracy of the arthroscopic measurements was 90.5%.
Arthroscopic vs open measurements
The overall mean difference between arthroscopic and open measurements confirmed the trend of underestimation of the dimensions, when measured arthroscopically (< 0.001) (Table 2). The differences between separate measurements were all negative, and some of them were statistically significant (Table 3).
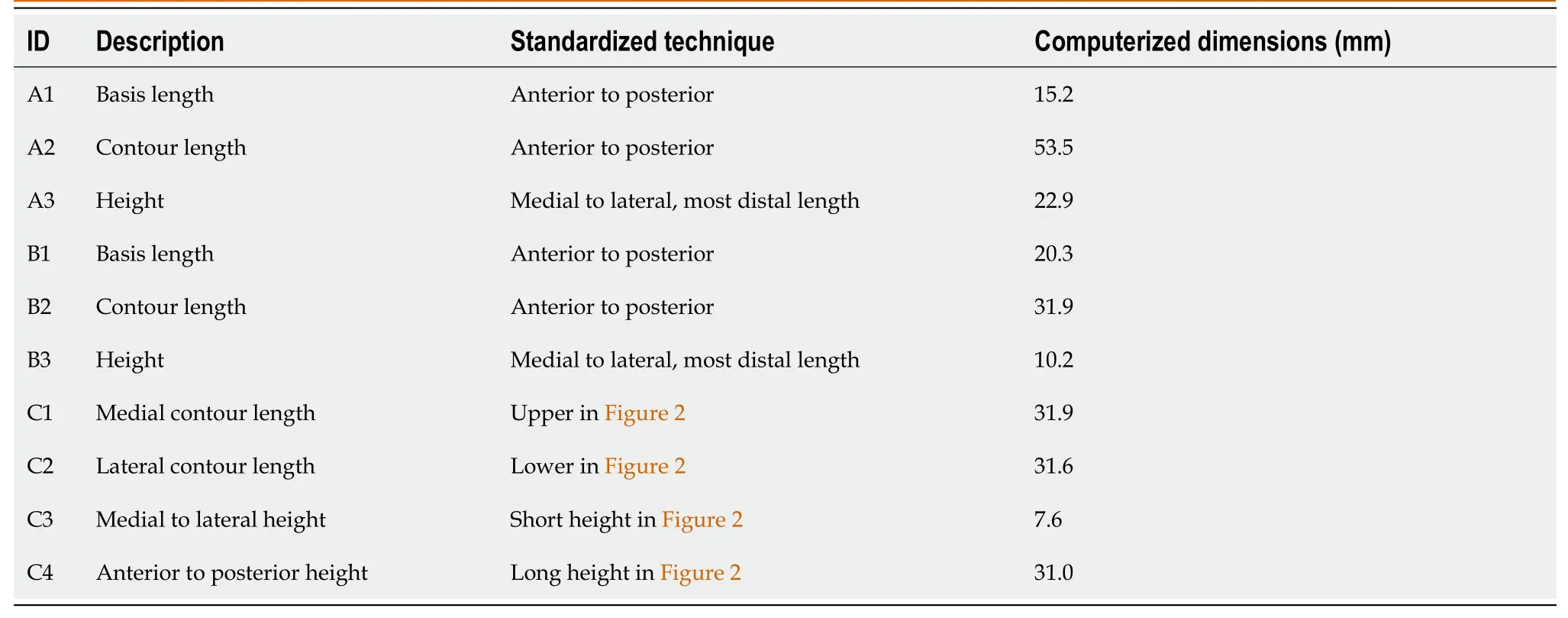
Table 1 The dimensions of the simulated tears measured by the surgeons (Layouts in Figure 2)
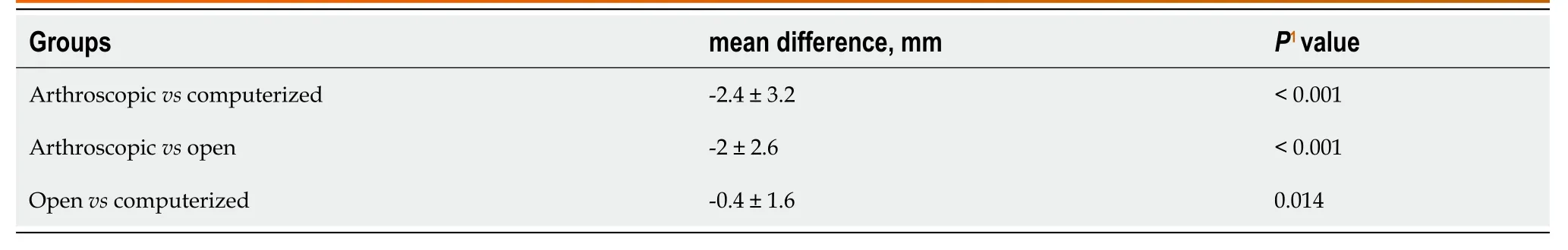
Table 2 Overall mean difference between the groups of measurements
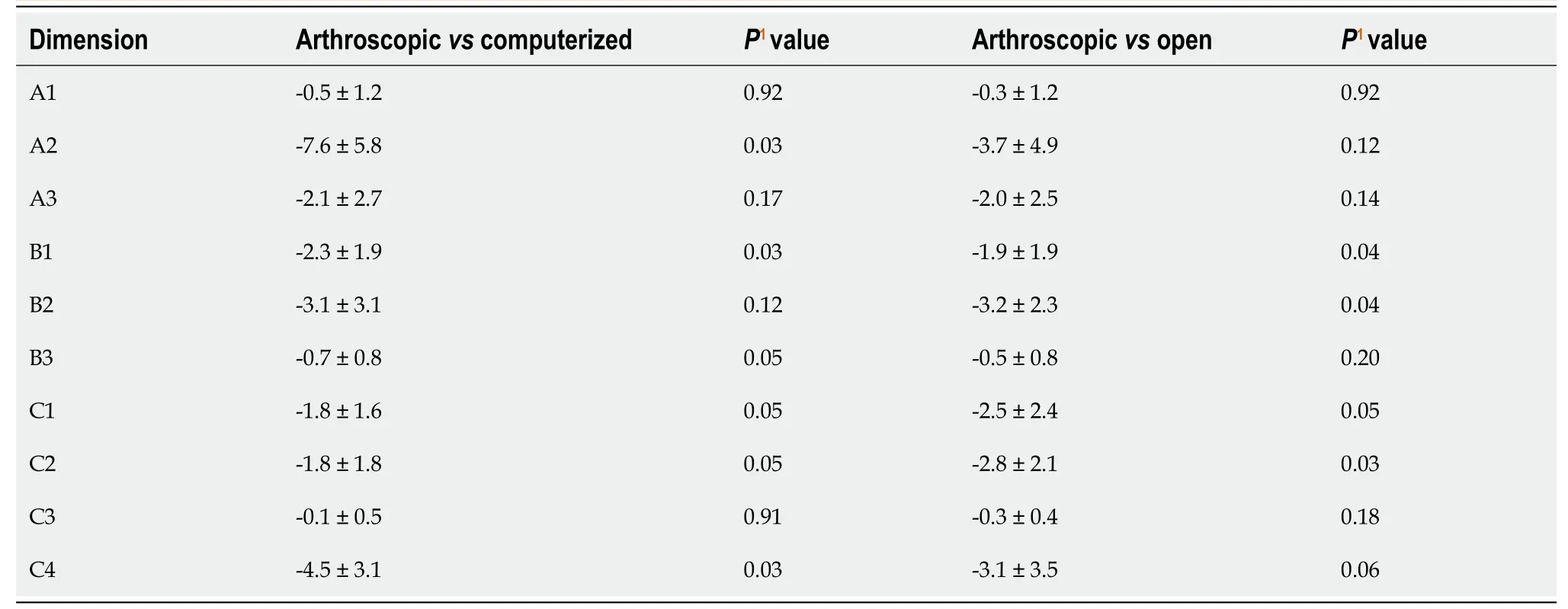
Table 3 Comparison of mean differences between arthroscopic versus computerized, and arthroscopic and open measurements in millimeters (mean ± SD)
Open vs computerized measurements
The overall mean difference between open and computerized differences was smaller than between arthroscopic and computerized; -0.4 ± 1.6 mm-2.4 ± 3.2 mm. The difference was statistically significant for the corrected level of significance between the groups (< 0.016), but we considered the mean value of 0.4 mm clinically insigni-ficant for the surgical decision-making. The accuracy of the open measurements was 98.5%.
Precision between surgeons with different levels of experience
No significant differences were observed between the senior staff surgeons and the fellows (= 0.07). On the contrary, the senior residents reported smaller tear dimensions when compared both to the staff surgeons and the fellows (< 0.001 for both comparisons). Measurements with the open technique were precise among all surgeons (= 0.96), showing excellent inter-observer reliability.
DISCUSSION
Surgeons of three different levels of experience were found to constantly underestimate given dimensions of simulated rotator cuff tears with the arthroscopic technique. We utilized three common patterns of rotator tears (a small U-shaped, a larger U-shaped, and a crescent-type). We observed a constant underestimation of the dimensions of the tears when measured with a standard 5 mm probe arthroscopically.
We observed mean differences up to 7.5 mm when comparing the separate measurements of the tears’ dimensions compared to the computerized measurements. The accuracy of the arthroscopic and open measurements was 90.5% and 98.5%, respectively. When comparing the different levels of experience, the senior residents reported smaller tear dimensions when compared both to the staff surgeons and the fellows. It seems that more experienced surgeons tend to be more accurate, although the underestimation is constant to all levels of experience, implicating that the instrumentation used is not suitable for precise measurements. Measurements with an open technique were both accurate and precise.
There are numerous studies considering the intraoperative evaluation of the size of the tear as a factor influencing the choice of the most indicated repair technique and the outcomes of the repair. Park[4] reported that large-to-massive tears (> 3 cm) repaired with double-row fixation had significantly improved outcomes in terms of functional outcomes in comparison with those repaired with single-row fixation. Duquin[7] analyzed data from 23 studies and found re-tearrates significantly lower for double-row repairs when compared with single-row, especially for tears greater than 5 cm. A summary of meta-analyses reported that six meta-analyses found double row repair to be superior for tears greater than 3 cm, and recent studies also report that larger tears size increases re-tear risk[9,17-19]. Of course, several other factors influence the surgeon’s decision-making of the appropriate surgical technique, including patient characteristics, muscle quality, and mobility of the tendons, as mentioned before[4,6-9]. However, recent research has shown that the rotator cuff tear size at the time of surgery significantly affects supraspinatus integrity in the long-term, thus greatly influences the prognosis of clinical and functional outcomes and patient satisfaction[20]. Moreover, in certain techniques such as superior capsule reconstruction for irreparable rotator cuff tears or reinforcement of cuff repair, precise measurements of the tears’ dimensions are crucial for the technique per se[10,11].
In the current study, we observed a constant underestimation of the tears’ dimensions with mean differences up to 7.5 mm, when measured arthroscopically. These differences could lead to inappropriate selection of procedures during surgery and affect the patients’ outcomes and prognosis. Our results agree with Bryant[21], who reported arthroscopic measurements to have a 12% underestimation of the tear size compared to measurements with an open technique.
Previous studies have compared MRI measurements with the arthroscopic evaluation of rotator cuff tears and reported high sensitivity and specificity both for full and partial thickness tears[13,14]. However, Bryant[21] reported magnetic resonance imaging to underestimate the size of rotator cuff tears by 30%. Additionally, Eren[14] found significantly larger measurements during surgery when compared with MRI.
In our study, arthroscopic and open techniques were compared but the accuracy and precision were also determined. Combined with the three different levels of experience of the surgeons and the common clinical use of the 5 mm probe, our procedure is very close to daily routine surgical practice.
Limitations of the study
We used a relatively small sample size. The rationale for the sample selection was that separate measurements for ten specific tear dimensions provided a total of sixty observations in each group (arthroscopic, open, and computerized measurements), which were enough to draw conclusions. Secondly, the measurements were conducted in a plastic simulation shoulder model and not in real patients so that comparisons could be made to computerized measurements.
CONCLUSION
This study suggests that arthroscopic measurements of full-thickness rotator cuff tears constantly underestimate the dimensions of the tears. This underestimation, especially of specific dimensions (contour length of the small U-shape tear, anterior to posterior height of the crescent-type tear, and contour length of the large U-shaped tear), could lead to false documentation during surgery, unreliable prognostic suggestions, and even postoperative failures. Measurements with an open technique were accurate and precise. These observations raise the need for the development of better arthroscopic tools and techniques for the evaluation of the size of the rotator cuff tears.
ARTICLE HIGHLIGHTS
Research background
Arthroscopic procedures are commonly performed for rotator cuff pathology. The intraoperative evaluation of the tear size and pattern contributes to the choice and completion of the technique and the prognosis of the repair.
Research motivation
The accuracy of common arthroscopic instruments to evaluate the dimensions of different types of rotator cuff tears is not yet evaluated.
Research objectives
The purpose of the current study was to compare the arthroscopic and open measurements with the real dimensions of three different patterns of simulated rotator cuff tears of known size using a plastic shoulder model.
Research methods
Three sizes and patterns of simulated supraspinatus tears on a plastic shoulder model(small and large U-shaped, oval-shaped) were created. Six orthopaedic surgeons with three levels of experience measured the dimensions of the tears arthroscopically, using a 5 mm probe, repeating the procedure three times, and then using a ruler (open technique). Arthroscopic, open and computerized measurements were compared.
Research results
A constant underestimation of specific dimensions of the tears was found when measured with an arthroscope, compared to both the open and computerized measurements. No differences were observed between the open and computerized measurements. The accuracy of arthroscopic and open measurements was 90.5% and 98.5%, respectively. When comparing between levels of experience, senior residents reported smaller tear dimensions when compared both to staff surgeons and fellows.
Research conclusions
This study suggests that arthroscopic measurements of full-thickness rotator cuff tears constantly underestimate the dimensions of the tears. This underestimation could lead to false documentation during surgery, unreliable prognostic suggestions, and even postoperative failures.
Research perspectives
Development of more precise arthroscopic techniques or tools for the evaluation of the size and type of rotator cuff tears are necessary.
ACKNOWLEDGEMENTS
The support of the Musculoskeletal Research Center and the facilities of the Wet Lab in Southside Hospital of UPMC, Pittsburgh are greatly appreciated.
杂志排行
World Journal of Orthopedics的其它文章
- Far lateral lumbar disc herniation part 1: Imaging, neurophysiology and clinical features
- Total hip arthroplasty in fused hips with spine stiffness in ankylosing spondylitis
- Role of biomechanical assessment in rotator cuff tear repair:Arthroscopic vs mini-open approach
- Rates of readmission and reoperation after operative management of midshaft clavicle fractures in adolescents
- Surgical treatment outcome of painful traumatic neuroma of the infrapatellar branch of the saphenous nerve during total knee arthroplasty
- Decision aids can decrease decisional conflict in patients with hip or knee osteoarthritis: Randomized controlled trial
