Role of early transjugular intrahepatic portosystemic stent-shunt in acute variceal bleeding: An update of the evidence and future directions
2021-12-06FaisalKhanDhirajTripathi
Faisal Khan, Dhiraj Tripathi
Abstract Variceal bleeding is a serious complication of cirrhosis and portal hypertension.Despite the improvement in management of acute variceal bleed (AVB), it still carries significant mortality. Portal pressure is the main driver of variceal bleeding and also a main predictor of decompensation. Reduction in portal pressure has been the mainstay of management of variceal bleeding. Transjugular intrahepatic porto-systemic stent shunt (TIPSS) is a very effective modality in reducing the portal hypertension and thereby, controlling portal hypertensive bleeding.However, its use in refractory bleeding (rescue/salvage TIPSS) is still associated with high mortality. “Early” use of TIPSS as a “pre-emptive strategy” in patients with AVB at high risk of failure of treatment has shown to be superior to standard treatment in several studies. While patients with Child C cirrhosis (up to 13 points) clearly benefit from early-TIPSS strategy, it’s role in less severe liver disease (Child B) and more severe disease (Child C > 13 points) remains less clear.Moreover, standard of care has improved in the last decade leading to improved 1 -year survival in high-risk patients with AVB as compared to earlier “early”TIPSS studies. Lastly in the real world, only a minority of patients with AVB fulfil the stringent criteria for early TIPSS. Therefore, there is unmet need to explore role of early TIPSS in management of AVB in well-designed prospective studies.In this review, we have appraised the role of early TIPSS, patient selection and discussed future directions in the management of patients with AVB.
Key Words: Transjugular intrahepatic portosystemic stent-shunt; Early transjugular intrahepatic portosystemic stent-shunt; Salvage transjugular intrahepatic portosystemic stent-shunt; Portal hypertension; Acute variceal bleed; Hepatic encephalopathy
INTRODUCTION
Acute variceal bleeding (AVB) is a severe complication of portal hypertension and occurs at a rate of around 10 %-15 % per year in patients with cirrhosis. The risk of variceal bleeding depends on the severity of liver disease, size of varices, and presence of red wale marks[1 ]. Six-week mortality following an episode of AVB (the endpoint identified as the key outcome in variceal bleeding) is reported to be between 15 % and 25 %[2 -4 ]. Early mortality was reported to be 50 % in the early eighties[5 ]. The presence of clinically significant portal hypertension is the main factor determining the risk of development of varices and other liver-related decompensations. Transjugular intrahepatic portosystemic stent-shunt (TIPSS) was initially used for management of refractory variceal bleeding only (salvage or rescue TIPSS), followed by prevention of rebleeding or as secondary prophylaxis. There has been recent interest in early or preemptive TIPSS (e-TIPSS) in selected patients at high risk of treatment failure and mortality. There remains considerable controversy in the utility of early TIPSS, and we aim to provide a summary of the current evidence and discuss unresolved issues and future directions.
IDENTIFYING PATIENTS AT RISK OF A POOR OUTCOME FOLLOWING AVB
Although the prognosis of AVB has significantly improved over the last decades due to better management of haemorrhage and its associated complications, mortality is still as high as 15 %-20 %[2 ].
Patients presenting with AVB do not benefit equally from standard treatment as not all patients have the same risk profile of treatment failure, re-bleeding and mortality.The risk of rebleeding (and subsequently death) is greatest in the first 48 -72 h after the initial episode and over 50 % of rebleeding episodes occur within the first 10 d[6 -8 ].Therefore, it is important to identify those patients who are at high risk of treatment failure and death in whom a more aggressive approach, like implantation of early or pre-emptive TIPSS (within 72 h of index bleeding) can be utilised.
Measurement of the hepatic venous pressure gradient (HVPG) is the gold standard method for evaluating portal hypertension[9 ]. Portal hypertension is defined as an increase of HVPG > 5 mmHg; and HVPG ≥ 10 mmHg is defined as clinically significant portal hypertension as above this threshold, varices usually appear and risk of developing overt clinical decompensation (variceal bleeding, ascites and hepatic encephalopathy) increases[9 ,10 ]. If varices remain untreated, rebleeding and death occur in approximately 60 % and 30 % of patients respectively, one to two years after the index bleeding[1 ].
HVPG measured within 24 h of the bleeding episode is shown to be a prognostic indicator for outcome following AVB. HVPG > 20 mmHg has been associated with up to 5 -fold increased risk of failure to control bleeding and one-year mortality[11 ,12 ].Decrease in portal pressure of ≥ 20 % from the baseline or to HVPG ≤ 12 mmHg is associated with significant reduction in risk of decompensation and with improved survival[13 ].
Recent data also show that decreasing HVPG by > 10 % from baseline, or to absolute values < 10 mmHg, reduces the risk of development of varices and AVB regardless of the presence of varices[14 ]. Therefore, lowering HVPG has been one of the treatment strategies in management of AVB.
Portal hypertension correlates strongly with severity of liver disease measured by Child-Pugh score[13 ]. The severity of liver disease remains the main determinant of prognosis in patients with AVB[15 ,16 ]; There is a strong relationship between the presence of HVPG > 20 mmHg and Child–Pugh class[11 ,17 ]. Therefore, Child-Pugh Class C is associated with poor outcome following AVB. Moreover, presence of ascites and bacterial infections are also associated with poor outcome[18 ].
Severity of bleeding (active bleeding on endoscopy and haematocrit level) as well as presence of portal vein thrombosis are also among the significant predictors of early treatment failure following AVB[19 ].
Recalibrated MELD score (−5 .312 + 0 .207 × MELD) has been developed to predict early mortality after an episode of AVB. MELD score of 19 or higher is associated with a higher mortality risk of 20 %[2 ]. The utility of recalibrated MELD in predicting outcome has recently been validated in 2 observational studies[20 ,21 ]. Similarly, Child-Pugh Class C is associated with higher mortality risk than in Child–Pugh class A and B cirrhosis, regardless of the presence of active bleeding[21 ].
In a recently published study acute-on-chronic liver failure (ACLF) at baseline is also found to be an independent risk factor for rebleeding and mortality in patients presenting with AVB. Presence of ACLF almost doubled the risk of rebleeding[22 ].
SALVAGE TIPSS
In the 1980 s, the prognosis in patients with refractory or uncontrolled variceal bleeding was poor with mortality of over 90 % in Child-Pugh B and C patients[23 ].Though rescue surgical treatments (oesophageal transection or surgical porto-systemic shunting) were effective in decreasing portal hypertension, these procedures were associated with high mortality, ranging from 50 % to 90 % in this situation[24 ,25 ].Moreover, subsequent liver transplantation may become technically more difficult to perform following porto-systemic shunt surgery[25 ].
The concept of percutaneous transjugular porto-systemic shunt in context of oesophageal variceal bleeding in humans was first introduced by Colapintoet al[26 ] in 1982 (in which intrahepatic portosystemic shunt was created by dilating the track with an angioplasty balloon). First (prospective) study evaluating the role of salvage TIPSS in patients with variceal haemorrhage refractory to (then) standard medical and endoscopic treatment was published in 1994 [27 ]. In that study though salvage TIPSS(with bare stent) was associated with immediate control of bleeding in all 20 patients,40 -d mortality was very high at 60 % mainly due to liver failure and sepsis[27 ].
Several (retrospective) studies were published afterwards, evaluating the role of salvage (rescue) TIPSS (using uncovered stents) in setting of refractory variceal bleeding[28 -30 ]. Salvage TIPSS was effective in controlling the variceal bleeding but early mortality rate remained high in these patients, approaching 48 % at 45 -d. Majority of the patients died due to multi-organ failure and sepsis. Child-Pugh (CP > 11 ),APACHE II and MELD scores (> 20 ) were associated with increased mortality[29 ,30 ].These studies were uncontrolled, mainly involved uncovered stents and sclerotherapy was the choice of endoscopic treatment.
Standard treatment of AVB has improved considerably in the recent decade and covered TIPSS has lower risk of stent dysfunction as compared to bare metal stents[31 ,32 ]. In subsequently reported retrospective studies of salvage TIPSS using both covered and uncovered stents, the use of covered stent did not culminate in survival advantage at both 6 wk and 1 -year[33 ,34 ]. However, use of bare metal stent was associated with increased rate of re-bleeding due to stent dysfunction and salvage TIPSS appeared to be futile in patients with Child-Pugh score of > 13 [34 ].
A recently published Chinese retrospective study of 58 patients, in which 55 patients had covered stents, showed better 6 -weeks and 1 -year transplant free survivals (87 .7 % and 81 .8 %, respectively) following salvage TIPSS[35 ]. Treatment failure at 6 wk was associated with bare stents and white cell count. It is important to note that 62 % patients had Child B disease and over 60 % had hepatitis B related disease. Only 30 % of patients had Child C disease. Median MELD score was 10 and mean Child score was 8 .7 , indicating that majority of patients had less severe disease(but with high portal pressure)[35 ]. Moreover, 82 % of patients had variceal embolization[35 ], an effective tool to prevent re-bleeding[36 ,37 ].
EARLY TIPSS
Randomised control trials in e-TIPSS
It is important to clarify the concept of e-TIPSS. e-TIPSS strategy refers to a preemptive placement of TIPSS in those at a high-risk of treatment failure before treatment failure or re-bleeding occurs. In this setting, TIPSS is usually placed within 24 –72 h of successful therapeutic endoscopy (with patients already on pharmacological therapy with vasoactive drugs and antibiotics). The rationale of this strategy is that reducing portal pressure early on, will prevent rebleeding, the associated liver failure and development of multi-organ failure with a lot worse outcome. This is in contrast to salvage TIPSS, where TIPSS is placed in patients with refractory variceal bleeding,not controlled with standard treatment; and this group of patients has very high mortality (as described above).
As stated earlier, reduction in portal hypertension is one of the mainstays of management of AVB. Utilising this evidence, Jalanet al[38 ] introduced the concept of preventive insertion of TIPSS (pre-emptive or early TIPSS placement, within 72 h) to lower portal pressure in cirrhotic patients with AVB in 1990 s. They published a randomised control trial (RCT) in 1997 including 58 patients and compared endoscopic band ligation (EBL) with e-TIPSS (with bare-metal stent) randomised within 24 h after controlling of first episode of AVB. Mean time to TIPSS in that study was 2 .2 d. e-TIPSS placement was superior to EBL in preventing rebleeding and was cost-effective in this setting. However, no survival difference was seen, although ITU requirement was significantly less with TIPSS. The Child-Pugh score of 9 was similar in the two groups, although there were some Child’s A patients included[38 ]. Patient selection was not as strict as for subsequent studies. This could explain the lack of difference of survival.
Since then, the role of e-TIPSS in the management of acute variceal bleeding in patients with cirrhosis has been evaluated in several studies. The safety and efficacy of e-TIPSS in high-risk cirrhotic patients has been evaluated in a few RCTs (Table 1 ).
Monescilloet al[12 ] performed the first study applying high-risk selection criteria by using measurements of HVPG. Fifty two patients with HVPG ≥ 20 mmHg measured with 24 h of bleeding episodes were randomised to either TIPSS group or standard therapy. Their study showed that “early” TIPSS placement was associated with a significantly lower rate of treatment failure (50 % vs 12 %) and lower 6 -wk mortality(38 % vs 19 %). 46 % of study population had Child C disease[12 ]. However, bare-metal stents were used in TIPSS patients and standard of care (SOC) in the non-TIPSS group did not reflect current practice (sclerotherapy rather than combination of endoscopic band ligation and non-selective beta-blocker therapy). Patients in non-TIPSS arm received only non-selective beta-blockers (NSBBs) to prevent rebleeding and EBL was used in whom NSBBs were not tolerated or were contraindicated.
Measurement of early HVPG for risk stratification and treatment assignment in AVB is not easily applicable in clinical practice nor readily available. Therefore, it is important to identify non-invasive predictors of treatment failure and early mortality in patients with AVB. In this regard, Abraldeset al[11 ] not only showed a strong relationship between the presence of HVPG > 20 mmHg and Child-Pugh class C but also showed that 6 -wk mortality is more strongly determined by the severity of underlying liver disease (assessed by Child- Pugh classification) than by HVPG > 20 mmHg. Therefore, subsequent studies used clinical criteria to define high-risk patients and used only covered stents. A schema of the study design of these trials is illustratedin Figure 1 and Figure 2 .
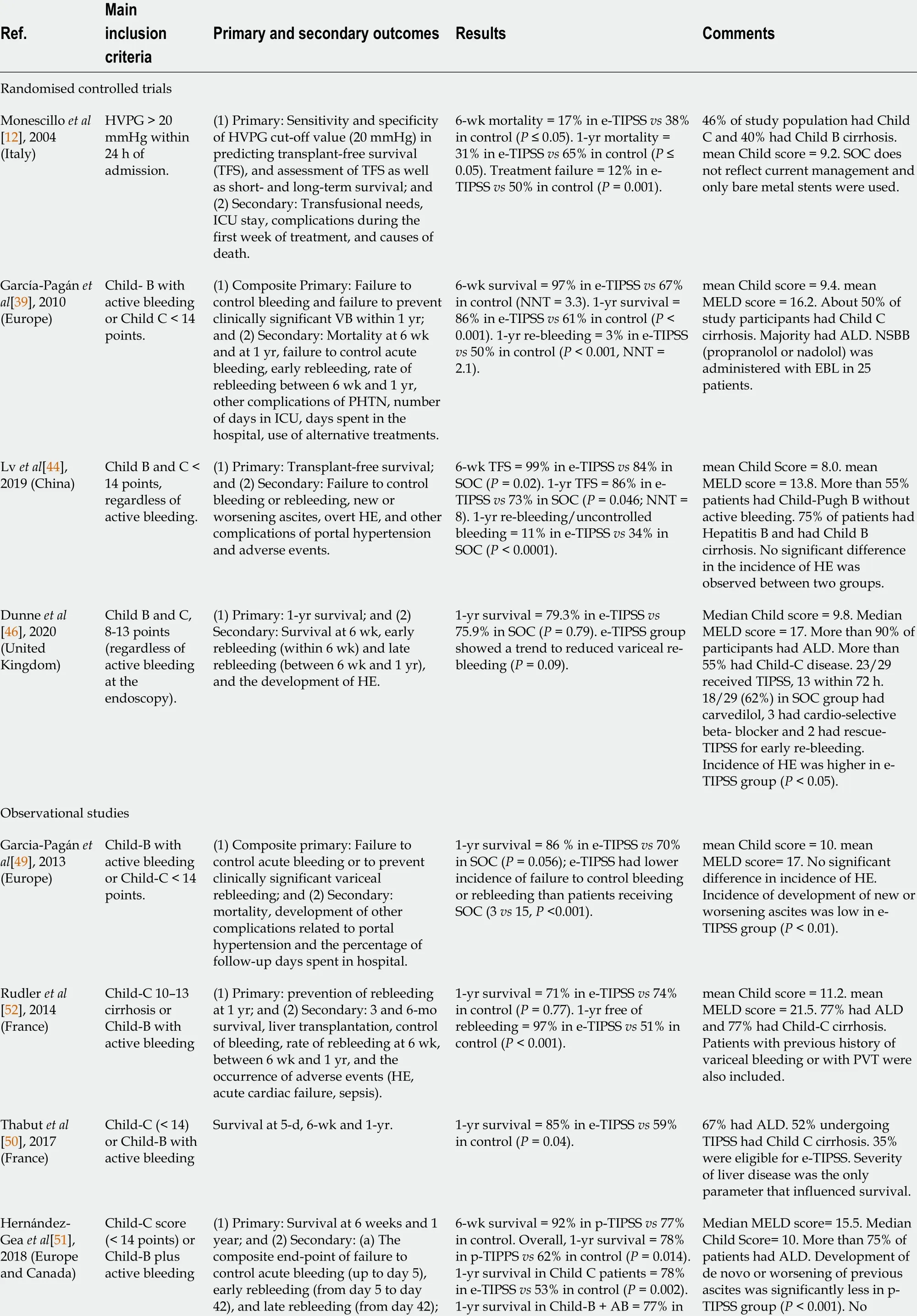
Table 1 Early transjugular intrahepatic portosystemic stent-shunt in acute variceal bleeding: Key studies

(b) onset or worsening of ascites; and(c) development of HE.p-TIPSS vs 75 % in control (P = 0 .935 ).difference in incidence of HE was observed in two groups.Lv et al[45 ],2018 (China)Any grade of cirrhosis (with Child score <14 ) and AVB.(1 ) Primary: All-cause mortality; and(2 ) Secondary: Failure to control acute bleeding or rebleeding, new or worsening ascites and development of overt HE.Overall 6 -wk mortality = 3 .6 % in e-TIPSS vs 10 .6 % in SOC (P = 0 .002 ).Overall 1 -yr mortality = 14 .1 % in e-TIPSS vs 17 .3 % in SOC (P = 0 .218 ). e-TIPSS group had significantly lower mortality in MELD ≥ 19 category.Patients with Child A cirrhosis were also included. Only small number (< 20 %) had Child C cirrhosis. Survival benefit was not seen in Child B patients without active bleeding. Incidence of HE was not significantly different between two groups.Trebicka et al[22 ], 2020 (Multicentre)Child-C, Child-B with active bleeding.(1 ) Primary: All-cause mortality or liver transplantation at 6 wk and 1 yr;and (2 ) Secondary: Rebleeding.6 -wk mortality = 13 .6 % in e-TIPSS vs 51 % in SOC group of patients with ACLF (P = 0 .002 ). 1 -yr mortality =22 .7 % in e-TIPSS vs 56 .5 % in SOC group with ACLF (P = 0 .002 ).Patients with ACLF had a higher rate of rebleeding compared to patients without ACLF (42 -d: P <0 .001 ; 1 -yr: 22 .9 % vs 17 .7 %, P =0 .024 ).e-TIPSS: Early transjugular intrahepatic portosystemic stent-shunt; RCT: Randomised controlled trial; HVPG: Hepatic venous pressure gradient; HCC:Hepatocellular carcinoma; PHTN: Portal hypertension; PVT: Portal vein thrombosis; TFS: Transplant-free survival; HIV: Human immunodeficiency virus;ICU: Intensive care unit; NSBB: Non-selective beta-blockers; EBL: Endoscopic band ligation; IGV: Isolated gastric varices; MELD: Model for end-stage liver disease; ALD: Alcohol-related liver disease; NNT: Number needed to treat; HE: Hepatic encephalopathy; SOC: Standard of care; ACLF: Acute on chronic liver failure.
In García-Pagánet al[39 ] landmark RCT published in 2010 , patients with Child-Pugh C < 14 or Child-Pugh B with active bleeding at index endoscopy were considered high-risk patients. While there is clear justification of including patients with Child C disease in this category[11 ], the selection of Child B patients (with active bleeding on endoscopy) was not very clear. The composite primary end point in their study was of failure to control acute bleeding or to prevent clinically significant variceal rebleeding within 1 year. Their trial of 63 patients showed that early covered TIPSS (placed within 72 h of index bleeding) not only reduced re-bleeding at 1 year (3 % vs 50 %, P < 0 .001 )but also improved 6 -wk [97 % vs 67 %; absolute risk reduction = 30 %; number needed to treat (NNT) = 3 .3 ]; and 1 -year survival rates (86 vs 61 %, P < 0 .001 ; NNT = 4 .0 ) in highrisk patients with cirrhosis when compared to standard of care (NSBB plus EBL). It is important to note that rates of treatment failure and death were higher in Child C patients than in those with Child-B disease, and mortality rates in Child B category did not appear to be significantly different statistically between SOC and TIPSS arms (2 /16vs1 /16 ). However, the trial was not powered enough to conduct appropriate subgroup analyses[39 ]. Patients with prognostic factors unlikely to benefit from TIPSS placement were excluded from this trial and the subsequent studies (Table 1 ).
In the light of emerging evidence, subsequent guidelines incorporated the use of pre-emptive or e- TIPSS, as a treatment option in patients with AVB at high risk of treatment failure[40 -43 ] (Table 2 ).
An RCT from China included 132 cirrhotic patients who were randomly assigned(2 :1 ) to receive pre-emptive TIPSS or standard of care (NSBB + EBL)[44 ]. This RCT showed better 1 -year transplantation-free survival (primary outcome) in e-TIPSS group than in the control group; with greatest benefit for those with a MELD score between 12 and 19 (P = 0 .04 , NNT = 8 )[44 ]. However, all patients with Child B and C(< 14 points) cirrhosis were included regardless of active bleeding at the index endoscopy. Secondly, the patient demographics were significantly different from other studies and most patients were Child-Pugh B without active bleeding (57 %). Over 75 %of patients had Hepatitis B related cirrhosis. Only 43 % of patients were high risk according to the previously described criteria[39 ], and considered to benefit from e-TIPSS intervention[45 ]. Therefore, absolute risk difference of 13 % for 1 -year(transplant-free) survival in e-TIPSS group appeared to be lower than in the previous RCTs (34 % and 25 %)[39 ]. There was no significant difference in incidence of hepatic encephalopathy between the two groups.
A recently published RCT from the UK included 58 patients with a Child-Pugh score of 8 -13 , without previous treatment for portal hypertension related bleeding,regardless of active bleeding on endoscopy[46 ]. Patients were randomised to receive e-TIPSS or standard of care (carvedilol + EBL). There was no difference in 1 -year survival rate (primary outcome) between the SOC and e-TIPSS groups (75 .9 % vs 79 .3 %respectively,P= 0 .79 ). More than 90 % of participants had alcohol related liver disease and majority (over 80 %) were actively consuming alcohol at inclusion reflecting real Western world population. Over 55 % had Child-C disease with median MELD score of 17 , comparable with Garcia-Pagan study[39 ]. In the e-TIPSS group, 23 /29 patients(79 %) actually underwent TIPSS and only 13 within 72 h, but all within 5 days. There was no difference in worsening or new ascites, with more encephalopathy (46 .1 %vs20 .7 %, P < 0 .05 ) and a trend towards lower variceal rebleeding in the e-TIPSS group (P= 0 .09 ). Notably, previous RCT[39 ] and recent individual data metanalysis[47 ] did not show significant difference in development of hepatic encephalopathy between the two groups. Though the study was not powered enough to reach valid conclusions, it demonstrated better survival in the SOC arm than the previous European RCT[39 ](76 % vs 61 %), although SOC survival rate is comparable to the Chinese RCT[44 ].

Table 2 Summary of current Guidelines regarding early transjugular intrahepatic portosystemic stent-shunt
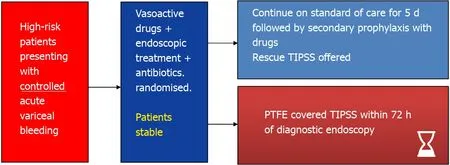
Figure 1 Early transjugular intrahepatic portosystemic stent-shunt – study design. High risk criteria: Child’s C or Child’s B + active bleeding, Child-Pugh score 8 -13 , Child’s B + C; Maximum threshold: CPS > 13 ; TIPSS: Transjugular intrahepatic portosystemic stent-shunt; PTFE: Polytetrafluoroethylene.
Better survival in SOC group could be explained by improved initial management of AVB (vasoactive drugs, antibiotics and endoscopic band ligation), with better access to intensive care. Furthermore, carvedilol was used to a greater extent. The improved SOC could be major factor in the lack of difference in survival between the two groups.In the SOC arm, 18 /29 patients received carvedilol (at a median dose of 6 .25 mg a day). Carvedilol with its additional alpha-1 antagonism profile, seems to have greater effect on reducing HVPG than other traditional NSBB (propranolol and nadolol) and may have a beneficial effect in SOC group but this needs further validation. This study has led to much debate in relation to patient selection[48 ].
Observational studies
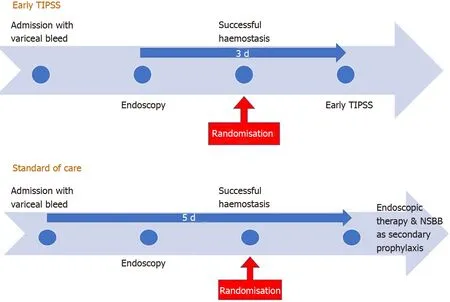
Figure 2 Design of early transjugular intrahepatic portosystemic stent-shunt and standard of care. TIPSS: Transjugular intrahepatic portosystemic stent-shunt.
The benefits of e-TIPSS have been shown by several (but not all) observational studies.Most of these studies used similar clinical high-risk and exclusion criteria as the study by Garcia-Pagan[49 ] (Table 1 ). It is important to note that in a French national audit and in large multicentre study, only a minority of patients eligible for e-TIPSS(according to defined criteria) actually received e-TIPSS (6 .7 % and 9 .8 % respectively)[50 ,51 ]. Survival benefit of e-TIPSS was only seen in those with Childs-Pugh C disease in a large multicentre study including 671 patients[51 ]. These large observational multicentre studies underscore the lack of adherence of physicians to concept of e-TIPSS and difficulty in arranging e-TIPSS (within limited timeframe) in a real-life practice. Most physicians did not believe in the role of e-TIPSS. Two European studies did not find a statistically significant increase in survival in e-TIPSS group[49 ,52 ]. One of these studies included patients with Child-Pugh score up to 15 points i-e, patients with significantly advanced liver disease[52 ].
A recent observational study from China included 1425 patients with cirrhosis and variceal bleed[45 ]. Most of the patients had cirrhosis due to viral hepatitis and e-TIPSS was also offered to Child-Pugh A patients and Child-Pugh B patients without active bleeding. Survival benefit was observed in patients fulling the high-risk criteria used in Garcia Pagan RCT[39 ] and with MELD score ≥ 19 but not in patients with Child-Pugh A or Child-Pugh B without active bleeding.
In a recently published retrospective study, e-TIPSS has also shown improved 6 -weeks and 1 -year survival (P < 0 .05 ) in patients with ACLF[22 ]. 671 patients were eligible for e-TIPSS and only 66 received e-TIPSS. 22 out of 66 e-TIPSS patients had ACLF. However, the findings need to be interpreted with caution due to the small sample size and require validation in larger prospective studies.
Systemic reviews and meta-analyses
A few metanalyses of studies looking at the role of early TIPSS in patients with AVB have been published in recent years. A well-designed meta-analysis of two earlier RCTs[39 ] and two observational studies[49 ,52 ] comparing e-TIPSS with standard of care showed that e-TIPSS is associated with reduced overall mortality (odds ratio =0 .38 , 95 %CI: 0 .17 -0 .83 , P = 0 .02 )[53 ] (Table 3 ). It is important to note that sensitivity analysis looking separately at Child B patients with active bleeding and those with Child C (< 14 score) showed that survival benefit was only observed in Child C (< 14 score) patients but not so in Child B patients. There was also significant reduction in rebleeding with e-TIPSS without significant difference in incidence of hepatic encephalopathy. Moderate heterogenicity was observed among the studies and the recent RCTs by Lvet al[44 ] and Dunne et al[46 ] were not included in this metanalysis. The authors concluded that further study was required to identify factors associated with poor outcome after e-TIPSS.
A recently published individual patient data meta-analysis assessed the efficacy of e-TIPSS in high-risk patients[47 ]. They included 7 studies: 3 randomized controlled trials[12 ,39 ,44 ] and 4 observational studies[45 ,49 ,51 ,52 ] comprising 1327 patients. As discussed previously, one of the RCTs[44 ] and one of the observational studies[45 ]included patients in all Child-Pugh categories, therefore only individual data of those patients fulfilling the current high-risk criteria (Child-Pugh B with active bleeding and Child- Pugh C up to 13 points) were included in this individual meta-analysis. Thismeta-analysis showed overall survival benefit of e-TIPSS over standard of care. Sixweek and 1 -year survival were significantly higher in the e-TIPSS group than in the SOC group (93 % vs 76 .8 % and 79 % vs 62 %, respectively P < 0 .001 ). Moreover, benefit of e-TIPSS was observed in both CP- B patients with active bleeding (P= 0 .008 ;) and in CP-C patients (P< 0 .001 ). Number of patients needed to treat to save one life was 4 .23 (95 %CI: 3 .57 –6 .94 ). Multivariate analysis showed that patients with a CP score > 7 points had a significantly worse survival than those with CP score of 7 points or less.e-TIPSS significantly reduced the risk of failure to control bleeding/preventing variceal rebleeding (P< 0 .001 ) in all patients. Moreover, risk of developing new or worsening ascites was significantly reduced by the e-TIPSS in the overall population (P< 0 .001 ). This meta-analysis showed no significant differences in the risk of developing hepatic encephalopathy in the overall population (P= 0 .553 ). However, a limitation of this meta-analysis is the inclusion of both prospective and observational studies, and the authors concluded that further prospective studies are necessary. The latest UK RCT[46 ] and the multicentre French audit[50 ] were not included in this meta-analysis, thus somewhat limiting its utility.

Table 3 Early transjugular intrahepatic portosystemic stent-shunt in acute variceal bleeding: Key meta-analyses
A recent meta-analysis of 152 patients in three prospective RCTs, including the latest UK RCT[39 ,44 ,46 ], concluded that e-TIPSS is more effective in preventing variceal rebleeding than standard of care (EBL and medical management) without increase in adverse events[54 ]. e-TIPSS with covered stents significantly reduced incidence of bleeding (RR = 0 .20 , 95 %CI: 0 .09 –0 .42 , P < 0 .001 ). This was associated an improvement in overall survival, but it did not quite reach statistical significance, at 1 and 2 years (RR = 0 .62 , 95 %CI: 0 .33 –1 .19 and RR = 0 .62 , P = 0 .1695 %CI: 0 .31 –1 .26 ,respectively). Incidence of hepatic encephalopathy was similar across the studies[54 ].
FUTURE DIRECTIONS
Patients with advanced liver disease i-e with Child-Pugh C score (up to 13 points) and MELD score ≥ 19 benefit from the e-TIPSS intervention in the described studies.However, benefit of this intervention in patients with less severe disease i-e with Child-Pugh B or MELD < 19 is not very robust and there is further need to define the high-risk category.
Though patients with child score > 13 points are considered too sick for early TIPSS intervention with high mortality, it is not very clear from the literature if there is a maximal threshold of severity of liver disease beyond which there is no benefit from e-TIPSS intervention. Indeed certain patients with ACLF may benefit from e-TIPSS following AVB. This concept needs further revalidation in a multi-centre trial collecting large numbers of patients.
Outcomes after an episode of variceal bleed have improved in the last decade with improved 1 -year survival in patients receiving standard care[44 ,46 ] as compared to the earlier landmark RCT[39 ], causing reluctancy to adopt e-TIPSS approach among the practicing physicians. Moreover, providing e-TIPSS (within 72 h of admission) is challenging in most healthcare systems, even in centres providing 24 /7 TIPSS service,and is a significant barrier to adoption of e-TIPSS. Indeed, recruitment in trials[39 ,46 ]was very slow and careful reading of the manuscripts suggests that the included patients may not be truly representative of the entire population of patients with severe cirrhosis and variceal bleeding. With such stringent inclusion criteria, the applicability of this therapeutic approach is questionable in a larger cohort of cirrhotic patients.
Even if TIPSS was performed outside the 72 h window, so called “late e-TIPSS”, it may not have a significant impact on the outcomes given the time frame for acute bleeding is 5 d as defined by the Baveno consensus[40 ]. Indeed, benefits of e-TIPSS placement following oesophageal variceal bleeding have been observed for up to 28 d after index endoscopy[55 ,56 ]. Therefore, a more pragmatic approach to the time window for e-TIPSS is an important consideration when designing future trials.
CONCLUSION
The role of e-TIPSS in acute variceal bleeding requires further prospective study with adequately powered trials. Studies should focus on careful patient selection,investigate optimal timing of TIPSS, and explore quality of life and health economics.
杂志排行
World Journal of Gastroenterology的其它文章
- Proton pump inhibitors and colorectal cancer: A systematic review
- Orexins: A promising target to digestive cancers, inflammation, obesity and metabolism dysfunctions
- Calycosin attenuates severe acute pancreatitis-associated acute lung injury by curtailing high mobility group box 1 - induced inflammation
- Prediction of genetic alterations from gastric cancer histopathology images using a fully automated deep learning approach
- Endoscopic management of difficult common bile duct stones: Where are we now? A comprehensive review
- COVID-19 : Effect on gastroenterology and hepatology service provision and training: Lessons learnt and planning for the future
