Comparison of intraocular pressure peak and fluctuations among Filipino patients with non-glaucomatous eyes and glaucoma suspects using water drinking test and diurnal intraocular pressure
2021-11-30AnelisaKohCynthiaVerzosa
Anelisa Koh, Cynthia Verzosa
Department of Ophthalmology, Jose R. Reyes Memorial Medical Center, Manila 1003, Philippines
Abstract
INTRODUCTION
Glaucoma is one of the leading causes of irreversible blindness worldwide, and by 2020, according to Waisbourdet al[1], an estimate of 79.6 million people would have been affected. The main pathophysiology behind glaucoma is thought to be secondary to an impaired aqueous drainage leading to an increase in intraocular pressure (IOP),subsequently causing damage to the optic nerve. Increase or fluctuation in IOP is considered a major risk factor in glaucomatous progression, hence, IOP control is the mainstay of treatment strategy for glaucoma.
As reported by Susannaet al[2], target IOP is the baseline pressure at which glaucoma occurred; and treatment response are mostly determined by single measurements done at office hours. Some studies showed continuous glaucomatous progression even with controlled target IOP. Aside from other probable risk factors involved, an undetected high IOP and high IOP fluctuation may be a probable cause for this progression, hence, recent studies are being undertaken to prove a relationship between peak IOP and glaucomatous progression[3-5].
Water drinking test (WDT) was initially used as a form of stress test in assessing patients with primary open angle glaucoma (POAG). However, due to low sensitivity and specificity of the procedure, it was considered unreliable[6].Nonetheless, in recent emerging studies, results showed that WDT can detect significant fluctuation of IOP among glaucoma patients and maybe used as a standard tool for detection of glaucomatous progression[3-5].
In a recent cohort study done by Medinaet al[7], results showed that among patient with POAG and normal individuals, mean baseline IOP, peak IOP, and IOP change during WDT were significantly higher among patients with POAG than normal individuals. Interestingly, low levels of similarity among WDT performed during different hours of the day were noted,suggesting a poor reproducibility of the results. In prospective analysis by Hatanakaet al[8], results showed peak IOP with significant reproducibility, whereas IOP fluctuation showed moderate reproducibility. In a 2017 prospective study by De Moraeset al[9], among patients with POAG, higher IOP peaks during the WDT were more predictive of visual field progression, whereas, in the mean and peak IOP during office hours over the same period were not significantly associated with visual field progression.
In the Philippines, glaucoma is the third common cause of blindness in the population[10-11]. Screening patients for glaucoma has been a proactive movement among ophthalmologists. Inspite of these recent evidences, WDT has not yet been considered as a standard tool for analysis of progression; but the results were promising. In our local setting, this method has not yet been fully applied to any institutions. And due to lack of local studies, initiation of such study may lead to a great impact in the care and management for our glaucoma patients.
As of writing, there is no study regarding WDTs used as a measuring tool for IOP peaks among Filipinos. It is currently getting popular among ophthalmologists specifically glaucoma specialist. Current standard used is by acquiring the mean diurnal IOP to determine the IOP peak and fluctuation which usually takes the whole day for a patient versus 2h when doing a WDT. This study aims to initiate the standard use of WDT as a screening tool in glaucoma.
SUBJECTS AND METHODS
Ethical ApprovalThe study underwent ethical approval by the Institutional Review Board. All information collected was made confidential. Participants were identified through code numbers. Data collected were property of Jose R. Reyes Memorial Medical Center. Informed consent was taken by the investigator prior to the start of the study. There were no expected risks during this study. Fundings were investigator initiated, hence all costs were shouldered by the investigator.Study subjects were randomly taken from the Out-patient Department last November 2019. Inclusion criteria were the following: 1) 18 years old above, 2) patients diagnosed as glaucoma suspects, 3) healthy individuals volunteered from relatives of glaucoma suspects. Criteria to be diagnosed as glaucoma suspect in this study are the following: 1) open angles on gonioscopy, 2) suspicious optic disc and/or retinal nerve fibre layer findings on visual field, 3) elevated IOP>21 mm Hg[12].Exclusion criteria are: 1) patients with heart conditions, 2)chronic renal diseases, 3) other concomitant eye condition, 4)patients, who are using any ophthalmic medications, 5) those who underwent past ocular surgeries.
Patients were free to withdraw from the study anytime they wish. The demographics of each participant were taken. All participants were given general ophthalmological evaluation including visual acuity, gonioscopy, and fundus examination of optic nerve head. Participants in both groups underwent WDT and mean peak diurnal IOP measurement.
WDT was performed by asking patients not to drink any fluids 2h prior to the test. IOP was taken using Goldmann applanation tonometry. IOP was then measured just before ingestion of water as their baseline IOP. After which, the participant was asked to drink 1 liter of water in 5min. The IOP value was determined with the mean of 3 consecutive measurement. Another IOP was taken if the IOP values were not within 2 mm Hg. WDT was performed on different times of the day within clinic hours from 8a.m.to 5p.m. IOP was then measured 5, 15, 30, 45, and 60min after fluid ingestion.Peak IOP, defined as the maximum IOP measured in WDT,was determined. On a separate visit, diurnal IOP measurement was done at a two-hour interval between 8a.m.and 4p.m.
Statistical AnalysisThis study had a sample size of at least 128 eyes with a 95%CI and 80% power. The required number of subjects was calculated using OpenEpi™ Version 7.1.0.6 Calculator.
Statistical analyses were performed using STATA Statistical Software, Version 13, College Station, TX: StataCorp LP. AP-value <0.05 was considered significant. Descriptive statistics such as mean, standard deviation, frequency, and percentage were used to summarize the respondent’s demographic characteristics, peak intra-ocular pressure, and time of peak IOP measurements. Comparative analysis was conducted using analysis of covariance (ANCOVA) to compare the mean peak IOP measurements between the WDT and mean diurnal IOP methods while controlling for identified confounders,particularly age.
RESULTS
The study included a total of 64 glaucoma suspect eyes and 64 normal control eyes. Table 1 illustrates the demographic profile of the respondents. It can be noted that the mean age of patients with normal eyes was 40.09y (SD=15.85), while for the glaucoma suspects was 53.41y (SD=12.14). Comparative analysis using independentt-test showed that these mean ages were statistically different (t=-3.77,P=0.0004), denoting that glaucoma suspects were older. On the other hand, gender distribution between males and females was equally dividedamong those with normal eyes; however, majority of glaucoma suspect eyes were male (65.63%), however, comparative analysis showed that these proportions were not statistically different (χ2=1.60,P=0.206).

Table 1 Demographic profile of the respondents n=64

Table 2 Frequency distribution of the time of peak IOP measurement using WDT among patients with normal and glaucoma suspect eyes n=128
Table 2 depicts the frequency distribution of the time for the peak IOP measurement using the WDT among patients with normal and glaucoma suspects. It can be noted that among patients with normal eyes, the peak IOP were measured at 15min, both for the right (40.63%) and left eyes (43.75%). On the other hand, the peak IOPs for the right and left eye of glaucoma suspects were measured at 15min (37.50%) and 5min (37.50%).The comparative analysis using ANCOVA of the peak IOP using the WDT and mean diurnal IOP methods among patients with normal eyes are presented in Table 3. It can be noted that the unadjusted mean IOP for the WDT and mean diurnal IOP of the right eye among normal patients were 18.78 (SD=2.85)and 17.22 (SD=3.50) mm Hg, respectively. After adjusting for the confounding effect of age, comparative analysis showed that the peak IOP measurements were statistically higher(F=4.45,P=0.039) for the WDT. Similarly, analysis showed that the peak IOP measurements of the left eye was statistically higher (F=4.06,P=0.048) in the WDT (18.64±0.53) than the mean diurnal IOP method (17.11±0.53).
The comparative analysis using ANCOVA of the peak IOP using the WDT and mean diurnal IOP methods among patients with glaucoma suspect eyes are presented in Table 4. It can be noted that the unadjusted mean IOP for the WDT and mean diurnal IOP of the right eye among glaucoma suspects were 17.94 (SD=3.51) and 16.00 (SD=3.49) mm Hg, respectively.After adjusting for the confounding effect of age, comparative analysis showed that the peak IOP measurements were statistically higher (F=4.84,P=0.032) for WDT. In the same vein, analysis showed that the peak IOP measurements of the left eye was statistically higher (F=4.85,P=0.031) in WDT(17.82±0.60) than the mean diurnal IOP method (15.93±0.60).The comparative analysis using independentt-test of the IOP fluctuation using the WDT and mean diurnal IOP methods among patients with normal eyes are presented in Table 5.It can be noted that for the right eye (3.91±2.08), the WDT had a statistically higher IOP fluctuation (t=-3.05,P=0.003)compared to the mean diurnal IOP method. Similarly, the WDT (3.28±2.28) had a statistically (t=-2.61,P=0.011) higher mean IOP fluctuation score than the mean diurnal IOP method for the left eye (1.78±2.32).
Table 6 shows the comparative analysis for the IOP fluctuation between the two methods for glaucoma suspect eyes. It can be noted that for the right eye (3.38±2.12), WDT had a statistically higher IOP fluctuation (t=-3.31,P=0.002)compared to the mean diurnal IOP method. Similarly, the WDT (3.06±2.21) had a statistically (t=-2.89,P=0.005) higher mean IOP fluctuation score than the mean diurnal IOP method for the left eye (1.19±2.92).
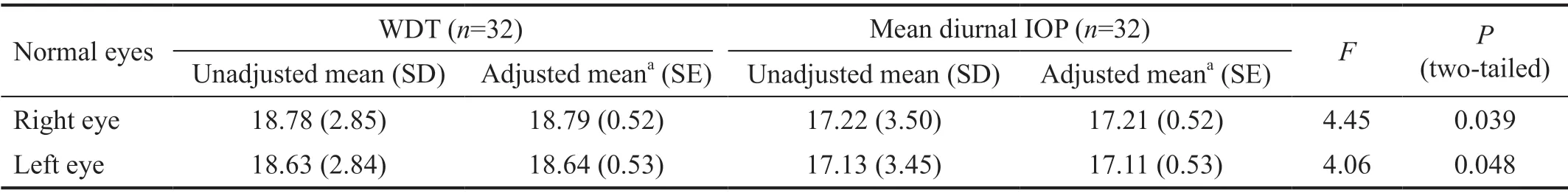
Table 3 Comparative analysis using ANCOVA of the peak IOP using WDT and mean diurnal IOP among patients with normal eyes n=64, mm Hg
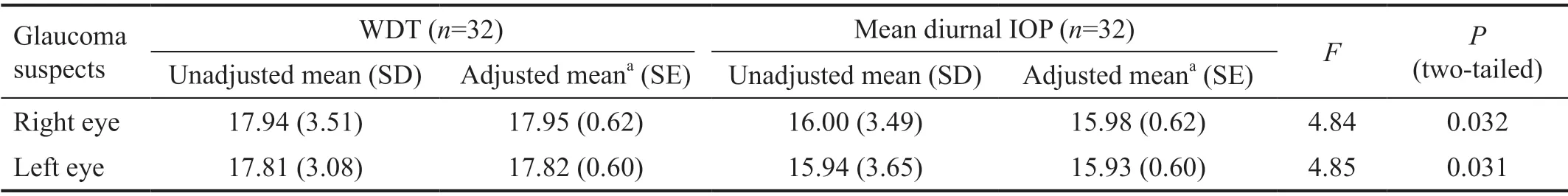
Table 4 Comparative analysis using ANCOVA of the peak IOP using WDT and mean diurnal IOP among glaucoma suspects n=64, mm Hg
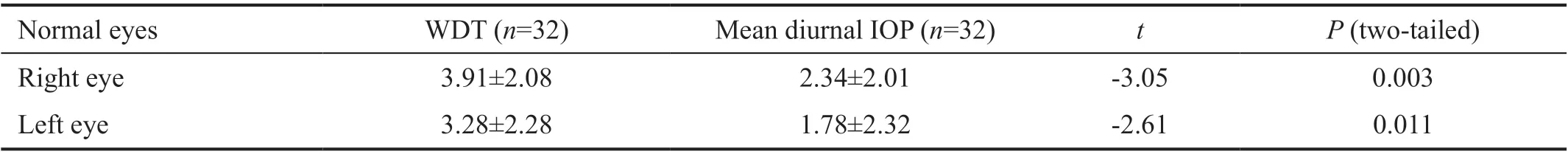
Table 5 Comparative analysis using independent t-test of the IOP fluctuation using WDT and mean diurnal IOP among patients with normal eyes n=64, mean±SD

Table 6 Comparative analysis using independent t-test of the IOP fluctuation using WDT and mean diurnal IOP among patients with glaucoma suspect eyes n=64, mean±SD
DISCUSSION
Progression of glaucoma is associated with large IOP fluctuations and worsening of visual field. Hence, diurnal IOP measurement has been a valuable tool used to determine disease progression of glaucoma[13]. However, this method requires at least 10 to 24h to complete depending on the ophthalmologist. The introduction of WDT enables faster IOP determination, significantly decreasing the time to determine IOP fluctuations to an hour. We found that in the two groups, the peak IOP and IOP fluctuation from WDT were statistically higher than the mean diurnal IOP. In the clinical setting, this may suggest that the ability to detect a wider IOP fluctuation or higher peak IOP may lead to adjustment of current management of the patient with respect to correlation of this data to other clinical and diagnostic methods such as the standard visual field and optical coherence tomography.
WDT is considered to be a precise and reproducible diagnostic examination for glaucoma in recent studies[5,8]. According to Babicet al[14], WDT peak pressures were highly reproducible,however, IOP fluctuation only showed moderate reproducibility and was not considered significant. De Moraeset al[9]suggested a good correlation between WDT and diurnal curves. IOP fluctuations in WDT are considered important independent risk factors in predicting glaucomatous vision loss[15]. In a study by Bhattiet al[16], significant IOP increase was noted in the first 15min of water intake, which lasted up to 45min. This was accompanied with a relative decrease in the heart rate and increase in blood pressure in healthy participants. Because of this, there was an observed increased falling rate in the entire optic nerve head and its surrounding tissue. The changes in IOP are also reflected in blood flow waveform parameters in the region of the optic nerve head. Further studies also showed that WDT may be used to indirectly measure ocular outflow facility in both healthy and glaucoma patients[17].
WDT has also been proposed to be able to evaluate the eye’s 1)aqueous humor outflow facility, 2) detect IOP variability, and 3)estimate the 24-hour peak IOP[9,18]. The mechanism by which WDT impacts IOP fluctuations remain unknown. However,studies have proposed several mechanisms by which aqueous influx and outflow occurs. According to a study by Chenet al[19], it was proposed that the rise in IOP in WDT was caused by 1) reducing aqueous fluid transfer across the trabecular meshwork, 2) increasing peripheral and central venous pressure, including episcleral venous pressure[15,17]. Another mechanism is caused by increased choroidal volume, causing ciliary body congestion and iris rotation. This reduces the pressure gradient throughout the trabecular meshwork, thereby decreasing trabecular outflow[8,17,19-20]. A compensatory IOP increase is then needed to maintain equilibrium in the aqueous flow, trabecular outflow, and uveoscleral outflow[17]. In a study by De Moraeset al[20], in the correlation with choroidal volume and WDT among patients with OAG, it was also observed that the peak IOP was acquired 15min after the choroidal expansion.
Despite its diagnostic advantages, WDT cannot be used in patients with cardiac, renal, prostatic, and respiratory diseases,for fear of exacerbating fluid overload status[21]. Furthermore,patients who underwent trabeculectomy and non-penetrating deep sclerectomy would impair WDT interpretation due to increased outflow facility[17].
As of writing, there is still limited literature regarding glaucoma diagnosis and treatment among Filipinos. This study shows that WDT can be a comparable, if not better, diagnostic exam in predicting IOP fluctuations than mean diurnal measurement.WDT may become a promising diagnostic procedure to attenuate glaucoma progression, hence, further studies of its mechanism is highly recommended including the relationship between effect of WDT on aqueous outflow resistance and rise in IOP. However, we acknowledge that this study has several limitations including being a prospective comparative study.Follow up studies comparing WDT with the gold standard diagnostic exam for other forms of glaucoma among Filipino patients are recommended. Moreover, a study correlating WDT results with visual loss and progression is recommended as well.
ACKNOWLEDGEMENTS
Conflicts of Interest: Koh A,None;Verzosa C,None.
杂志排行
International Journal of Ophthalmology的其它文章
- Toric implantable collamer lens for the management of pseudophakic anisometropia and astigmatism
- Efficacy of rhNGF-loaded amniotic membrane transplantation for rabbit corneal epithelial and nerve regeneration
- lncreased cGAS/STlNG signaling components in patients with Mooren’s ulcer
- lnhibition of corneal neovascularization by topical application of nintedanib in rabbit models
- TGF-β2-induced NEAT1 regulates lens epithelial cell proliferation, migration and EMT by the miR-26a-5p/FANCE axis
- Protective effect of human umbilical cord mesenchymal stem cell-derived exosomes on rat retinal neurons in hyperglycemia through the brain-derived neurotrophic factor/TrkB pathway
